Abstract
Objective:
Evaluate a dissonance-based group eating disorder treatment designed to be a cost-effective front-line transdiagnostic treatment that could be more widely implemented than extant treatments that are more intensive and expensive relative to a supportive mindfulness group treatment typical of that offered at colleges.
Method:
Young women with eating disorders (N = 84) were randomized to 8-week dissonance-based Body Project Treatment (BPT) or supportive mindfulness treatment, completing diagnostic interviews and questionnaires at pretest, posttest, and 6-month follow-up.
Results:
Regarding primary outcomes, by 6-month follow-up 77% of BPT participants no longer met diagnosis for an eating disorder versus 60% of supportive mindfulness participants (relative risk ratio = 2.22; 95% CI = 1.01–4.93), though groups did not differ on eating disorder symptom change. Regarding secondary outcomes, BPT versus supportive mindfulness participants showed significantly lower dissonance about affirming the thin ideal at posttest and 6-month follow-up (d = .38 & .32), body dissatisfaction at posttest and 6-month follow-up (d = .62 & .62), negative affect at posttest and 6-month follow-up (d = .49 & .48), and functional impairment (d = .36) at 6-month follow-up; differences in thin-ideal internalization and abstinence from binge eating and compensatory behaviors were not significant.
Conclusions:
Whereas both treatments appeared effective, BPT produced larger effects and significantly greater remission of eating disorder diagnoses than a credible alternative treatment, which is very rare for trials that have compared active eating disorder treatments. Results suggest it would be useful to refine BPT and conduct target engagement research and efficacy trials.
Keywords: eating disorder, treatment, group, efficacy trial, cognitive dissonance
Eating disorders affect 13–15% of women by young adulthood (Allen, Byrne, Oddy, & Crosby, 2013; Stice, Marti, & Rohde, 2013) and are marked by chronicity, relapse, distress, functional impairment, and risk for future obesity, depression, anxiety disorders, substance abuse, suicide attempts, and early morbidity (Crow et al., 2009; Swanson et al., 2011). Unfortunately, over 80% of individuals with an eating disorder do not receive treatment (Swanson et al., 2011), in part because it is difficult to locate clinicians who deliver evidence-based treatments (Zandberg & Wilson, 2013). In addition, eating disorder treatments are intensive, typically requiring 20 individual sessions delivered over 6 months (Wilson & Zandberg, 2012), and very expensive (Striegel-Moore et al., 2000). The fact that the most evidence-based treatments differ for the various eating disorders (cognitive-behavioral therapy for bulimia nervosa [BN; e.g., Spielmans et al., 2013] and binge eating disorder [BED; e.g., Grilo, Masheb, & Wilson, 2005] versus family therapy for anorexia nervosa [AN; e.g., Dare, Eisler, Russell, Treasure, & Dodge, 2001]) also complicates implementation. Further, even those who receive treatment typically do not receive evidence-based interventions (Lilienfeld et al., 2013). Another limitation of the extant treatments is that only 47% of individuals treated with evidence-based treatments achieve abstinence from binge eating and compensatory behaviors for at least a 1-month period (Hay, 2013). Finally, individuals often continue to report pursuit of the thin ideal and body dissatisfaction post-treatment, which increases the risk of relapse (Bardone-Cone et al., 2010), implying that a treatment that reduces these factors should reduce relapse.
The recognition that there would be utility in developing a transdiagnostic treatment for eating disorders prompted the development of enhanced cognitive behavioral therapy (CBT-E), which was designed for use with the full spectrum of eating disorders. One randomized controlled trial found that CBT-E did not produce significantly greater abstinence from binge eating and compensatory behaviors by 4-month follow-up relative to integrative cognitive-affective therapy (ICAT; 23% versus 33%; Wonderlich et al., 2014). A second randomized controlled trial likewise found that CBT-E did not produce significantly greater abstinence than interpersonal therapy (IPT) by 15-month follow-up (34% versus 35%; Fairburn et al., 2015). Moreover, the fact that CBT-E, like ICAT and IPT, is delivered in 20 individual sessions makes this an expensive option that would be difficult to broadly implement.
Accordingly, we developed a brief front-line treatment for the spectrum of eating disorders that could be easily, inexpensively, and widely implemented. We reasoned that if young women with eating disorders, who might not otherwise seek treatment, were recruited through outreach efforts, it could markedly increase the proportion who receive treatment. In this 8-session group treatment, referred to as Body Project Treatment (BPT), women with eating disorders complete verbal, written, and behavioral activities in which they discuss costs of pursuing the thin ideal and engaging in disordered eating behaviors. These activities putatively create dissonance that reduces valuation of the thin ideal and eating disorder behaviors, as people are motivated to align their attitudes with their publically displayed behavior. BPT is an extension of the Body Project (Stice, Marti, Spoor, Presnell, & Shaw, 2008), a dissonance-based eating disorder prevention program for young women at risk for eating disorders due to body dissatisfaction. Efficacy and effectiveness trials have found that the Body Project produces greater reductions in eating disorder risk factors and symptoms compared to both assessment-only controls and alternative interventions across independent labs (e.g., Becker, Smith, & Ciao, 2005; Green, Scott, Diyankova, Gasser, & Pederson, 2005; Halliwell & Diedrichs, 2014; Mitchell, Mazzeo, Rausch, & Cooke, 2007; Stice et al., 2008). The Body Project produced a 60% reduction in eating disorder onset relative to assessment-only controls over a 3-year follow-up (Stice et al., 2008), and a 74% reduction in future eating disorder onset relative to an Internet-based eating disorder prevention program over 7-month follow-up (Stice, Rohde, Shaw, & Gau, 2017). Critically, the Body Project produced larger pre-to-post symptom reductions for women with versus without an eating disorder at baseline (d = .71 and .18, respectively; Müller & Stice, 2013), supporting its use as the foundation for a new dissonance-based eating disorder treatment (note; we attempted to only exclude participants with AN or BN in the two selective prevention program trials analyzed in this report, not those with BED or subthreshold AN, BN, or BED).
In an initial trial, 72 women with any threshold or subthreshold eating disorder (M age = 23.7, SD = 7.3) (AN = 3, BN = 37, BED = 5, subthreshold BN = 21, subthreshold BED = 2, purging disorder [PD] = 4) were randomized to the 8-session BPT or a usual care comparison condition (any treatment participants usually received; Stice, Rohde, Butryn, Menke, & Marti, 2015). Participants in both conditions could seek ancillary treatment. BPT participants showed significantly greater reductions in outcomes over 2-month follow-up compared to usual care, with large effects for thin-ideal internalization (Cohen’s d = .79), body dissatisfaction (d = 1.14), and eating disorder symptoms (d = .95), medium effects for dissonance regarding perpetuating the thin ideal (d = .65) and negative affect (d = .55), but the two conditions did not differ on change in functional impairment (d = .04). Effects for thin-ideal internalization, dissonance regarding perpetuating the thin ideal, body dissatisfaction, and eating disorder symptoms were significantly larger for BPT participants who attended more sessions and completed more homework (e.g., the effect for symptoms was larger [d = 1.36] for those who attended > 50% of the sessions versus those who attended fewer sessions [d = .28]), providing evidence of a dose-response relation.
Although results from the first trial were encouraging, one limitation was that treatment in the usual care control condition was not standardized and varied from receiving no intervention to meeting regularly with a psychotherapist with a range of theoretical orientations, and treatment often focused on more general mental health/personal problems rather than eating disorders. Further, usual care consisted almost entirely of individual therapy and never consisted of a manualized group treatment. Thus, we decided to compare BPT to a standardized version of usual treatment that was matched on amount, duration, and format of care. After reviewing available options, we selected a supportive mindfulness group treatment that is similar to treatments provided at many universities. The particular usual care treatment we evaluated has been offered at the University of Texas at Austin (one of our study sites) for several years. We inquired about treatments offered at another 6 universities, finding that all offered a similar supportive group treatment, many of which had mindfulness elements, and none offered any evidence-based eating disorder treatments. Only one randomized controlled trial evaluated a mindfulness-based treatment for eating disorders. In that trial, 150 overweight/obese adults reporting binge eating and weight concerns (66% met BED criteria) were randomized to a 12-session mindfulness-based group treatment, focused on promoting awareness of hunger and satiety, sensory-specific satiety, and emotional triggers for overeating, a CBT group intervention, or wait-list control (Kristeller, Wolever, & Sheets, 2013). Participants in both group-based treatments showed significantly greater improvements in binge eating and depression at 4-months follow-up than controls, but showed no differences in BMI change. Of the subset with BED at baseline, 68% in the mindfulness treatment no longer met diagnostic criteria at 4-month follow-up, versus 46% of those in the CBT condition and 36% of wait-list participants, a statistically significant difference.
The present report tested the hypotheses that participants randomly assigned to BPT versus a matched comparison intervention of supportive mindfulness treatment would show significantly greater reductions in blinded interviewer-assessed eating disorder symptom composite and remission of eating disorder diagnoses (primary outcomes), as well as significantly greater reductions in thin-ideal internalization, dissonance regarding perpetuating the thin ideal, body dissatisfaction, and abstinence from binge eating and compensatory behaviors (secondary outcomes). In the first trial participants were only followed for 2-months after treatment termination, making it difficult to operationalize remission from eating disorder diagnoses. Accordingly, we extended the follow-up period to 6-months for the present trial. We tested for differences in the percentage of participants in both conditions who no longer met criteria for any of the threshold or subthreshold eating disorders required for enrollment, as this remission outcome has been used in past trials (e.g., Kristeller et al., 2013; Munsch et al., 2007) and seemed ideally suited for a sample containing individuals with the full range of eating disorders, some of which might not involve binge eating or compensatory behaviors (e.g., AN or subthreshold AN). Nonetheless, we also compared the percentage of participants in both conditions who reported abstinence from binge eating or compensatory behaviors in the past 28 days, as this outcome has been used in past trials (e.g., Agras et al., 2000; Fairburn et al., 2015; Wonderlich et al., 2014).
Methods
Participants and Procedure
Women (N = 84) recruited from universities and surrounding communities in Eugene, Oregon and Austin, Texas (61% were from Eugene) enrolled based on data provided on a web-screener for eating disorders. For inclusion, participants had to meet criteria for a DSM-5 eating disorder at the baseline interview, which included Other Specified Feeding or Eating Disorder (OSFED). Baseline eating disorder diagnoses were AN = 1, BN = 38, BED = 8, subthreshold AN = 2, subthreshold BN = 22, subthreshold BED = 5, PD = 8. See Table 1 for the operationalization for these diagnoses. Women with AN with a BMI below 17 were excluded because they were not deemed appropriate for outpatient treatment without medical monitoring, similar to the exclusion criteria used previously for transdiagnostic outpatient treatment trials (e.g., Fairburn et al., 2015). Suicidal ideation and substance misuse were also exclusion criteria. We did not have any other exclusion criteria to maximize generalizability. We planned to recruit at least 80 participants for this trial because it should have provided a power of .80 to detect medium effect sizes (d = .50) or larger for the continuous outcomes.
Table 1.
Diagnostic criteria for DSM-5 eating disorders
| Eating Disorder | |
| Anorexia nervosa |
|
| Bulimia nervosa |
|
| Binge eating disorder |
|
| Other Specified Feeding or Eating Disorder | |
| Atypical anorexia nervosa |
|
| Subthreshold bulimia nervosa |
|
| Subthreshold binge eating nervosa |
|
| Purging disorder |
|
Note: Anorexia nervosa took diagnostic precedence over bulimia nervosa and binge eating disorder.
Table 2 provides information on demographic factors and other descriptive data for the two groups. Participants were randomized to BPT (n = 39) or supportive mindfulness group treatment (n = 45) without stratification using a random number table generated by our statistician. The Project Coordinator was solely responsible for allocation and did not know which condition participants would be assigned to until each had completed their pretest assessment. Research assistants who did all assessments were not informed of the allocation of each potential participant to condition. Both interventions consisted of 8 weekly 1-hour group sessions with 4–9 participants led by a pair of therapists. Participants completed assessments at pretest, posttest [2-month later], and at 6-months after posttest. Figure 1 depicts enrollment and participation flow in this study.
Table 2.
Study demographic and pretest characteristics by study condition
| Supportive Mindfulness | Body Project Treatment | |||
|---|---|---|---|---|
| Age [Mean, (SD)] | 26.6 | (10.3) | 22.6 | (5.1) |
| BMI [Mean, (SD)] | 29.5 | (10.5) | 25.9 | (5.4) |
| Hispanic (%) | 13.3 | 7.7 | ||
| Race (%) | ||||
| American Indian or Alaskan Native | 4.7 | 2.6 | ||
| Asian | 9.3 | 13.2 | ||
| Black or African American | 2.3 | 0.0 | ||
| White or Caucasian | 83.7 | 84.2 | ||
| Maximum parental education (%) | ||||
| Some high school | 0.0 | 5.1 | ||
| High school graduate | 11.1 | 10.3 | ||
| Some college | 24.4 | 23.1 | ||
| College graduate | 42.2 | 28.2 | ||
| Advanced degree | 22.2 | 33.3 | ||
| Binge eating frequency, monthly [Mean, (SD)] | 6.7 | (5.6) | 5.4 | (5.3) |
| Compensatory behaviors, monthly [Mean, (SD)] | 12.7 | (12.7) | 17.6 | (30.5) |
Figure 1.
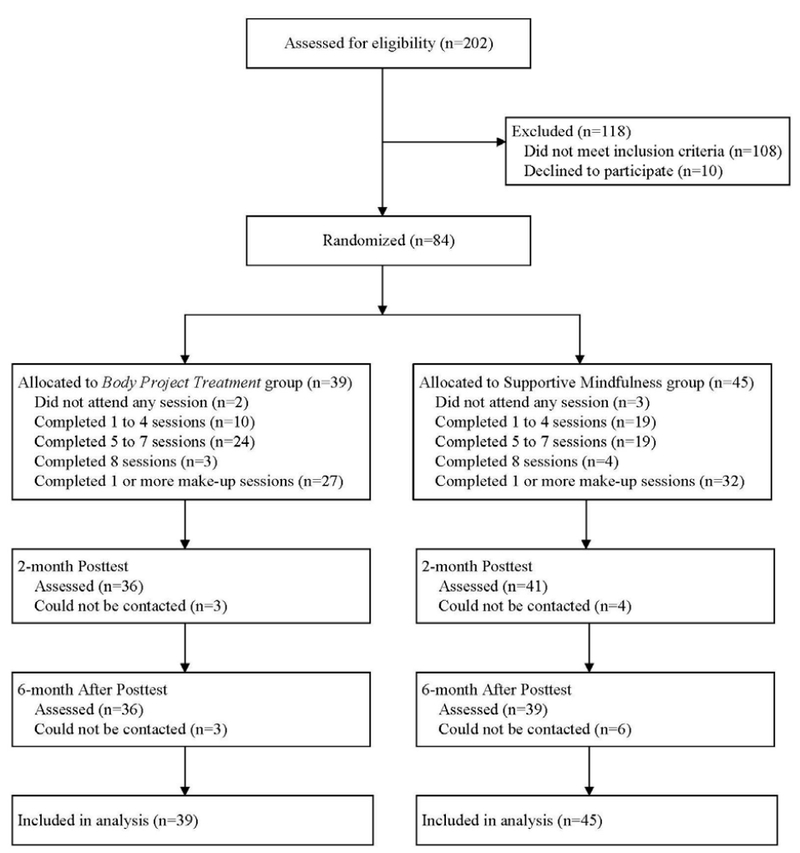
Participant flow througout the study
Facilitators in both conditions had either a doctoral or master’s degree in clinical psychology. Two clinicians at each site had experience implementing the Body Project eating disorder prevention program, so they implemented the BPT in this trial. The other two clinicians at each site implemented the supportive mindfulness treatment. Facilitator training involved reading the relevant intervention manual and attending a 4-hour workshop to learn the intervention rationale, role-play delivery of intervention components, and discuss process issues (e.g., homework compliance and retention). Treatment sessions were video-recorded and reviewed by Drs. Rohde and Shaw, who provided emailed supervision before the next session. During delivery of both treatments, facilitators tracked attendance (4-point scale; absent, partial attendance, full attendance, make-up session), participation (3-point scale; none or negative, minimal, good/active), and homework completion (4-point scale; none, some, all, didn’t bring materials).
Body Project Treatment (BPT)
Participants begin each session by stating their willingness to actively participate in the session. In-session exercises include defining the thin ideal, discussing costs of pursuing this ideal, completing motivational writing exercises (e.g., stating the importance of addressing their disordered eating), role-plays in which participants dissuade facilitators from endorsing the thin ideal or engaging in disordered eating behaviors, and reading aloud their home exercises. Between-session home exercises include writing letters (to a young girl about costs of pursuing the thin ideal, to someone who pressured the participant to be thinner, to their eating disorder), a mirror body acceptance exercise, generating lists of “body activism” behaviors women can do to challenge the thin ideal, writing a presentation on the adverse effects of eating disorders, engaging in behaviors they avoid because of body image concerns, and reducing “linchpin” eating disorder symptoms that maintain other symptoms (starting with consuming 3 healthy meals daily). A detailed description of the BPT intervention appears in Stice et al. (2015).
Supportive mindfulness group.
A supportive mindfulness treatment was selected as representative of typical treatment groups offered at settings such as universities. It was designed to match BPT on treatment modality (group-based), duration (8 1-hr sessions), and use of a manualized intervention script created for this study. Sessions provide basic education about eating disorders, articulate recovery goals, provide and work to enhance social support, and included mindfulness activities for coping with negative affect. It is important to note that only 6 sessions included mindfulness techniques, which focused on managing emotions (e.g., practicing emotional self-soothing and identifying moments of gratitude). Thus, this treatment only included mindfulness elements, rather than representing a treatment based solely on mindfulness. Drs. Rohde and Shaw watched 100% of sessions from the first group in each condition and a random 50% of subsequent sessions to ensure fidelity and no cross-condition contamination.
Measures
Thin-ideal internalization.
To provide a more sensitive measure for the present trial, we generated an additional 14 items assessing pursuit of the unrealistic beauty ideal, which we added to the original 6-item Ideal-Body Stereotype Scale-Revised scale (Stice et al., 2006). The new 20-item Thin-Ideal Internalization Scale used response options ranging from 1 = strongly disagree to 5 = strongly agree. Items were averaged for this and the other scales. The original scale has shown internal consistency (α = .91), 2-week test-retest reliability (r = .80), predictive validity for eating disorder symptom onset, and sensitivity to detecting effects of eating disorder prevention programs (Stice et al., 2006). The new 20-item version of this scale showed internal consistency in the present trial; α = .93 at pretest.
Dissonance regarding affirming the thin ideal.
We used the 10-item Thin-Ideal Affirmation Dissonance Scale to assess feelings of cognitive dissonance regarding engaging in behaviors that affirm the thin ideal (Stice et al., 2015). Sample items: I feel uneasy if I find myself obsessing about aspects of my appearance that don’t conform to the thin ideal and I feel better about myself if I challenge my friends not to pursue the thin ideal for women glorified in the media (reverse coded). Response options ranged from 1 = strongly agree to 5 =strongly disagree. This scale has shown internal consistency (α = .75), 8-week test-retest reliability in usual care controls (r = .61), and sensitivity to detecting intervention effects (Stice et al., 2015); α = .75 at pretest.
Body dissatisfaction.
The 17-item Satisfaction and Dissatisfaction with Body Parts Scale (Berscheid, Walster, & Bohrnstedt, 1973) assessed body dissatisfaction using response options ranging from 1 = strong positive feelings to 5 = strong negative feelings. It has exhibited internal consistency (α = .94), 3-week test-retest reliability (r = .90), predictive validity for bulimic symptom onset, and sensitivity to intervention effects (Stice et al., 2006); α = .83 at pretest.
Negative affect.
Negative affect was assessed with 20 items from the sadness, guilt, and fear/anxiety subscales from the Positive Affect and Negative Affect Scale-Revised (PANAS-X; Watson & Clark, 1992). Participants reported the extent to which they had felt various negative emotional states on scales ranging from 1 = very slightly or not at all to 5 = extremely. This scale has shown internal consistency (α = .95), 3-week test-retest reliability (r = .78), convergent validity, and predictive validity for bulimic symptom onset (Stice et al., 2006; Watson & Clark, 1992); α = .93 at pretest.
Eating disorder symptoms.
The semi-structured Eating Disorder Diagnostic Interview (EDDI; Stice et al., 2006) assessed eating disorder symptoms and diagnoses. It assesses the frequency of eating disorder symptoms on a month-to-month basis in the past 3 months before the pretest assessment and since the last assessment at posttest and 6-month follow-up. These data were used to confirm inclusion criteria and served as the primary outcome. The first primary outcome was a continuous symptom composite, which reflected symptoms in the past month (frequency of binge eating, vomiting, laxative/diuretic use, fasting, and excessive exercise, as well as distress about binge eating, endorsement of key features of binge eating [e.g., rapid eating, feeling disgusted, depressed or guilty about binge eating], overvaluation of weight/shape, fear of weight gain/becoming fat, and less than 85% of expected weight). This composite has shown internal consistency (α = .92), inter-rater agreement (ICC r = .93), 1-week test-retest reliability (ICC r = .95), sensitivity to detecting prevention and treatment intervention effects, and predictive validity for future onset of depression (Stice, Butryn et al., 2013; Stice, Rohde et al., 2015); α = .73 at pretest. The second primary outcome was the percentage of participants who no longer met criteria for the threshold or subthreshold DSM-5 eating disorders required for enrollment (Table 1) at 6-month follow-up. We selected this definition of remission because it best accommodated the different symptom presentation for participants with each of the four types of eating disorders (e.g., participants with AN or subthreshold AN might not have endorsed binge eating or compensatory behaviors at pretest). Nonetheless, we also report the percentage of participants who reported no binge eating or compensatory behaviors in the past month at 6-month follow-up because other eating disorder treatment trials have reported this outcome (e.g., Fairburn et al., 2015). EDDI eating disorder diagnoses have shown 1-week test-retest reliability (κ = .79), inter-rater agreement (κ = .75), sensitivity to detecting intervention effects, and participants with versus without EDDI-diagnosed eating disorders show greater functional impairment, emotional distress, and mental health treatment (Stice et al., 2008; Stice, Butryn et al., 2013).
Functional impairment.
Functional impairment with family members, peers, and at school and work was assessed with items from the Social Adjustment Scale (Weissman & Bothwell, 1976) using response options ranging from 1= never to 5 = very often. The original scale showed convergent validity with clinician and collateral ratings (M r = .72), discriminant validity, and treatment sensitivity (Weissman & Bothwell, 1976). The adapted items, which were those most relevant to young women, have shown internal consistency (α = .77), 1-week test-retest reliability (r = .83), and sensitivity to detecting effects of prevention programs (Stice et al., 2006, 2008); α = .78 at pretest.
Ancillary Treatment.
Participants were coded as having received ancillary treatment if they had spoken to a psychiatrist, psychologist, or other counselor, or a support group about an eating disorder or body image concern. Ancillary treatment was assessed over the past year at pretest, and since the last assessment at posttest and 6-month follow-up.
Statistical Methods
Preliminary analyses.
We examined the distribution of outcomes and applied normalizing transformations as necessary to reduce the potential for disproportionate influence of outliers and decrease residual heterogeneity. Comparisons between conditions were made for pretest values of outcomes and demographics (race, ethnicity, age, and parental education) to assess whether randomization created equivalent groups; any significant pretest differences were included as covariates in subsequent analyses. Comparisons between participants who completed all assessments and those who did not were made for study condition, pretest values of outcomes, and demographics to assess differential attrition.
Model building.
Intent-to-treat analyses of condition effects were evaluated with mixed effects analysis of covariance model fits with SAS 9.2 PROC MIXED (SAS/STAT, 2011). Individual variability in outcomes was modeled separately at posttest and 6-month follow-up, as a function of condition (coded 0 for BPT and 1 for supportive mindfulness), adjusting for pretest outcome values, to ensure that any differences in pretest levels of the outcome did not bias estimates of intervention effects. Nested models accounted for group variability, where participants in the conditions were clustered in treatment groups; clustering effects were removed if group level variance was estimated to be zero. Effect sizes were computed as Cohen’s d by dividing the difference between the estimated means of conditions at posttest and 6-month follow-up by the baseline pooled standard deviation (SD); a d = .30 corresponds to a small effect, a d = .50 to a medium effect, and a d = .80 to a large effect. We also computed within-condition Cohen’s d effect sizes to facilitate interpretation of the effects and comparison with effects from our earlier trial, which reflected the mean at posttest minus the mean at baseline, divided by the within-condition SD. Missing data were imputed using PROC MI and the imputation model included demographics and ancillary treatment, with imputed data in 20 data sets analyzed separately; model parameters and standard errors were combined following Rubin (1987) as implemented in SAS PROC MIANALYZE.
Given that this trial was designed to test the hypothesis that participants randomized to BPT would show greater reductions in outcomes than participants randomized to supportive mindfulness treatment, which is a directional hypothesis, we used directional inferential tests to optimize sensitivity. The fact that all of the observed effects favored BPT over supportive mindfulness treatment, and never vice versa, suggests it was reasonable to use directional tests. Power analysis indicated the study had adequate power (>.80) to detect effects of d = .54 or larger for all outcomes.
Results
Preliminary analyses.
Distributions of the outcomes approximated normality, except eating disorder symptoms, which were normalized with natural log transformations. Participants in the two conditions did not differ significantly on demographics, pretest values of outcomes, use of psychiatric medications, or ancillary treatment at any assessment, with the exception of age (t-value = 2.30, p-value = .031, d = .48; average age of 22.6 [SD = 5.1] and 26.6 [SD = 10.2] for BPT and supportive mindfulness participants, respectively). BPT and supportive mindfulness participants reported non-significant differences (p’s > .469) in use of psychiatric medications at pretest (25% vs. 24%), during the intervention period (17% vs. 29%), and over the 6-month follow-up (20% vs. 28%); and in ancillary treatment for eating disorders and body image concerns at pretest (13% vs. 16%), during the intervention period (3% vs. 12%) and over the 6-month follow-up (6% vs. 13%). Statistically covarying for receving ancillary treatment did not affect the significance of any findings reported herein.
Means and SDs for outcomes for each condition at each time point are presented in Table 3. The mean eating disorder symptom composite score of 47 for participants in the BPT condition reflects clinically significant eating pathology; for instance, a participant with BN who reported binge eating and use of compensatory weight control behaviors four times each per week, who also reported supreme importance of weight and shape and endorsed the items assessing distress about binge eating, would have an eating disorder symptom composite of 44. Table 4 provides the correlations of outcomes at pretest (correlations range from r = −.33 to .44, mean r = .07). Rates of missing data were 8.3% at posttest and 11.9% at 6-month follow-up; the missing completely at random assumption (MCAR) remained tenable (Little’s MCAR test χ2[107] = 128.64, p = .076). Attrition was not related to condition, demographics, or pretest outcomes. Age was included in subsequent models to adjust for baseline differences.
Table 3.
Means and standard deviations for outcomes by condition at pretest, 2-month posttest, and 6-month posttest
| Variable | Pretest | Posttest | 6-month Posttest |
|||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Thin-ideal internalization | ||||||
| Supportive mindfulness control | 3.81 | 0.57 | 3.46 | 0.60 | 3.49 | 0.62 |
| Body Project Treatment | 3.91 | 0.51 | 3.23 | 0.72 | 3.24 | 0.74 |
| Dissonance about affirming thin ideal | ||||||
| Supportive mindfulness control | 2.02 | 0.51 | 2.09 | 0.56 | 2.08 | 0.49 |
| Body Project Treatment | 1.96 | 0.55 | 1.88 | 0.51 | 1.90 | 0.52 |
| Body dissatisfaction | ||||||
| Supportive mindfulness control | 3.63 | 0.45 | 3.19 | 0.65 | 3.24 | 0.62 |
| Body Project Treatment | 3.78 | 0.52 | 3.02 | 0.73 | 3.03 | 0.79 |
| Negative affect | ||||||
| Supportive mindfulness control | 3.03 | 0.89 | 2.65 | 1.04 | 2.55 | 1.07 |
| Body Project Treatment | 3.25 | 0.65 | 2.22 | 0.94 | 2.24 | 0.96 |
| Eating disorder symptoms | ||||||
| Supportive mindfulness control | 44.78 | 19.30 | 23.55 | 18.14 | 18.21 | 25.64 |
| Body Project Treatment | 47.19 | 32.53 | 20.65 | 18.81 | 14.72 | 13.05 |
| Functional Impairment | ||||||
| Supportive mindfulness control | 2.49 | 0.53 | 2.32 | 0.62 | 2.37 | 0.59 |
| Body Project Treatment | 2.68 | 0.64 | 2.21 | 0.63 | 2.27 | 0.58 |
SD = standard deviation. Non-log transformed values of eating disorder symptoms reported.
Table 4.
Correlations among pretest outcome measures.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Thin-ideal internalization | 1.0 -- |
|||||
| 2. Dissonance about affirming thin ideal | .12 (291) |
1.0 -- |
||||
| 3. Body dissatisfaction | .33 (.002) |
.05 (.666) |
1.0 -- |
|||
| 4. Negative affect | −.08 (.494) |
−.16 (151) |
.27 (.013) |
1.0 -- |
||
| 5. Eating disorder symptoms | .06 (584) |
.02 (871) |
.23 (.039) |
.22 (.052) |
1.0 -- |
|
| 6. Functional Impairment | .15 (.188) |
−.16 (.141) |
.40 (<.001) |
.44 (<.001) |
.11 (.299) |
1.0 -- |
P-values are reported in parenthesis.
BPT participants attended a mean of 5.1 (SD = 2.4) sessions. Three (8%) attended all 8 sessions, 24 (62%) attended 5 to 7 sessions, 10 (25%) attended 1 to 4 sessions, and 2 (5%) did not attend any sessions; on average, 1.2 (SD = 0.1) make-up sessions were attended. BPT participants completed an average of 70% of the home exercises. Supportive mindfulness participants attended a mean of 4.4 (SD = 2.5) sessions. Four (9%) attended all 8 sessions, 19 (42%) attended 5 to 7 sessions, 19 (42%) attended 1 to 4 sessions, and 3 (7%) did not attend any sessions; on average, 1.1 (SD = 0.1) make-up sessions were attended. Supportive mindfulness participants completed an average of 53% of the home exercises.
Primary outcomes.
Intent-to-treat analyses of group effects at posttest and 6-month follow-up for continuous outcomes are shown in Table 5. BTP versus supportive mindfulness participants did not show differences in change in the eating disorder symptom composite over follow-up. However, at 6-month follow-up 77% of BPT participants and 60% of supportive mindfulness control participants no longer met criteria for any threshold or subthreshold eating disorder that was required for enrollment; remission from eating disorder diagnoses was significantly more likely for BPT versus supportive mindfulness participants (χ2[1,84] = 2.74 p = .049; relative risk ratio = 2.22; 95% CI = 1.01–4.93).
Table 5.
Test of posttest and follow-up group differences from mixed effects analysis of covariance models.
| Estimate | SE | t-value | p-value | d | |
|---|---|---|---|---|---|
| Thin-ideal internalization | |||||
| Posttest | 0.288 | 0.213 | 1.36 | 0.088 | 0.53 |
| 6-month follow-up | 0.302 | 0.220 | 1.37 | 0.085 | 0.55 |
| Dissonance about affirming thin ideal | |||||
| Posttest | 0.201 | 0.117 | 1.72 | 0.043 | 0.38 |
| 6-month follow-up | 0.171 | 0.099 | 1.73 | 0.043 | 0.32 |
| Body dissatisfaction | |||||
| Posttest | 0.298 | 0.146 | 2.04 | 0.021 | 0.62 |
| 6-month follow-up | 0.301 | 0.154 | 1.96 | 0.026 | 0.62 |
| Negative affect | |||||
| Posttest | 0.385 | 0.223 | 1.73 | 0.043 | 0.49 |
| 6-month follow-up | 0.380 | 0.231 | 1.65 | 0.050 | 0.48 |
| Eating disorder symptoms | |||||
| Posttest | 0.067 | 0.180 | 0.37 | 0.355 | 0.18 |
| 6-month follow-up | 0.136 | 0.186 | 0.73 | 0.232 | 0.36 |
| Functional Impairment | |||||
| Posttest | 0.199 | 0.125 | 1.59 | 0.056 | 0.34 |
| 6-month follow-up | 0.208 | 0.118 | 1.76 | 0.039 | 0.36 |
SE = standard error, d = Cohen’s d-statistic
Secondary outcomes.
BPT participants did not show significantly greater reduction in thin-ideal internalization and eating disorder symptoms at posttest or 6-month follow-up compared to supportive mindfulness participants. BPT versus supportive mindfulness participants showed significantly greater reductions in dissonance about affirming the thin ideal at posttest (d = .38) and 6-month follow-up (d = .32), body dissatisfaction at posttest (d = .62) and 6-month follow-up (d = .62), and negative affect at posttest (d = .49) and at 6-month follow-up (d = .48). BPT showed significantly greater reduction in functional impairment at 6-month follow-up (d = .36), but not at posttest. At 6-month follow-up, 55% of BPT participants and 39% of supportive mindfulness control participants reported no binge eating or compensatory behaviors in the past 28 days (p = .191).
Dose-response relations.
Eating disorder symptom composite reduction for BPT participants at posttest was larger (d = 1.32) for those who attended > 50% of the sessions vs. those who attended fewer sessions (d = .42). The trend of larger effects for those attending more > 50% of sessions versus those who attended fewer was seen for all outcomes: thin-ideal internalization (d = 1.69 vs. .65), dissonance about affirming thin ideal (d = .32 vs. −.31), body dissatisfaction (d = 1.71 vs. .83), negative affect (d = 1.73 vs 1.29), and functional Impairment (d = .95 vs. .21).
Discussion
With regard to the primary outcomes, remission from eating disorder diagnoses by 6-month follow-up was significantly higher in BPT (77%) versus supportive mindfulness treatment (60%), though the groups did not show significant differences in reduction in the eating disorder symptom composite. In terms of secondary outcomes, participants assigned to BPT showed significantly greater reductions in dissonance regarding thin-ideal affirmation, body dissatisfaction, negative affect, and functional impairment compared to participants assigned to the supportive mindfulness treatment. These effects were medium in magnitude. However, contrary to expectations, there were no significant differences in reductions in thin-ideal internalization and abstinence from binge eating and compensatory behaviors at 6-month follow-up. Data also indicated that participants who attended at least 50% of BPT sessions showed larger reductions in outcomes than those who attended fewer sessions, providing evidence of a dose-response relation.
It is encouraging that BPT produced significantly greater remission from eating disorder diagnoses and greater reductions in four of the six continuous outcomes, as the effects are theoretically not due to differential demand characteristics for the BPT participants versus supportive mindfulness treatment participants given that both were credible treatments matched on number and duration of sessions and on delivery modality. The significant difference for one of the two primary outcomes is noteworthy given that only 2 of the 15 trials that compared an eating disorder treatment to a credible alternative treatment matched for intervention modality (e.g., individual therapy) and duration produced such an effect (Agras, Walsh, Fairburn, Wilson, & Kraemar, 2000; Cooper & Steere, 1995; Eisler et al., 2000; Fairburn et al., 2015; Jones, Peveler, Hope, & Fairburn, 1993; Kirkley et al., 1985; le Grange et al., 2007; McIntosh et al., 2005; Munsch et al., 2007; Safer, Robinson, & Jo, 2010; Schmidt et al., 2015; Treasure et al., 1995; Wilfley et al., 2002; Wilson, Wilfley, Agras, & Bryson, 2010; Wonderlich et al., 2014). Thirteen of these trials did not detect a significant difference between conditions in eating disorder symptom reductions or remission. One trial found that adolescents with BN who received Family Based Treatment showed significantly higher remission from binge eating and compensatory behaviors for a 1-month period than those who received supportive psychotherapy (relative risk ratio = 2.9 at 6-month follow-up, which translates into a d = .47; le Grange et al., 2007). In contrast, another trial found that women with AN who received nonspecific support clinical management showed significantly greater reduction in global symptom severity than those who received Interpersonal Therapy (d = −1.53; McIntosh et al., 2005). The fact that BPT produced significantly greater diagnostic remission than the supportive mindfulness intervention is noteworthy given that CBT has not been found to produce superior remission than several alternative treatments, including IPT, ICAT, mindfulness treatment, and acceptance and commitment theory (Fairburn et al., 2015; Linardon, Fairburn, Fitzsimmons-Craft, Wilfley, & Brennan, 2017; Wonderlich et al., 2014).
The evidence that remission from eating disorder diagnoses was 77% for BPT participants versus 60% for supportive mindfulness participants was encouraging. Moreover, the fact that 55% of BPT participants achieved abstinence from binge eating and compensatory behaviors by 6-month follow-up is also encouraging given that the parallel abstinence rates were 23%−34% for CBT-E at the end of follow-up in the two randomized trials that compared CBT-E to alternative treatments (Fairburn et al., 2015; Wonderlich et al., 2014). However, the 55% abstinence rate for BPT was not significantly higher than the 39% abstinence rate observed for supportive mindfulness treatment in our trial. It was also encouraging that the 55% abstinence rate for BPT compares favorably to the average abstinence rate of 47% for more intensive 20-session individually delivered empirically supported treatments (Hay, 2013). When interpreting these remission rates, it is important to consider whether participants in this sample are representative of individuals with eating disorders in the community, those that have participated in previous trials, and those who actively seek care at specialty eating disorder treatment centers. Given that we used outreach efforts to recruit individuals with eating disorders who were not actively seeking treatment, the present sample is probably representative of individuals with eating disorders in the community and of samples examined in studies that recruited individuals with threshold or subthreshold eating disorders from the community for treatment trials (Kirkley et al., 1985; Munsch et al., 2007). However, the present sample is probably not representative of samples that contain only individuals with full threshold eating disorders (e.g., Eisler et al., 2000; Safer et al., 2010; Wilfley et al., 2002; Wilson et al., 2010) or only patients that actively sought treatment through existing clinics (e.g., Cooper & Steele, 1995; Eisler et al., 2000; Jones et al., 1993; le Grange et al., 2007; Schmidt et al., 2015; Treasure et al., 1995), the latter of whom probably have more severe eating pathology that the broader population of individuals with eating disorders.
It is important to consider the mechanism by which BPT produced significantly larger remission from eating disorder diagnoses than supportive mindfulness treatment. Theoretically, the larger reductions in dissonance regarding affirming the thin ideal, body dissatisfaction, and negative affect produced greater reductions in eating disorder diagnosis. This interpretation is consistent with the evidence that BPT produced larger reductions in these variables than did supportive mindfulness therapy (mean d = .49, corresponding to a medium effect). An important direction for future studies will be to examine the mechanism of treatment effects and target engagement in greater detail.
Although BPT did not produce significantly greater reductions in eating disorder symptoms than supportive mindfulness treatment, it is noteworthy that the effect sizes for this outcome at posttest (d = .18) and at 6-month follow-up (d = .36) were similar to the pre-post effects for from published trials that compared evidence-based eating disorder treatments (e.g., CBT) to alternative treatments (e.g., Interpersonal Therapy; M d = .05; Agras et al., 2000 [d = .06]; Cooper & Steele, 1995 [d = −.39]; Eisler et al., 2000 [d = −.27]; Fairburn et al., 2015 [d = .02] Jones et al., 1993 [d = .26]; Munsch et al., 2007 [d = .18]; Safer et al., 2010 [d = .18]; Wilfley et al., 2002 [d = .18]; Wilson et al., 2010 [d = .17]; Wonderlich et al., 2014 [d = .05]) or active comparison interventions that involve the same contact time with clinicians but lack the theorized active ingredient (M d = −.01; Kirkley, Schneider, Agras, & Bachman, 1985 [d = .35]; le Grange, Crosby, Rathouz, & Leventhal, 2007 [d = .47]; McIntosh et al., 2005 [d = −1.53]; Schmidt et al., 2015 [d = .31]; Treasure, Todd, Brolly, Tiller, Nehmed, & Denman, 1995 [d = .37]). It is unclear why the eating disorder symptom reduction effects for BPT were larger at 6-month follow-up than at posttest, but this might have emerged because the dissonance-based intervention was more effective than supportive mindfulness therapy in reducing variables that serve to maintain eating disordered behaviors (e.g., body dissatisfaction).
However, we had hypothesized that BPT would produce significantly greater reductions in the outcomes in this trial compared to supportive mindfulness treatment. To properly interpret the non-significant effects, it is vital to determine whether the supportive mindfulness treatment is effective. We compared the average within-condition pre-post d for BPT and supportive mindfulness treatment in this study, as well as the parallel effect sizes from BPT and usual care in the initial trial (Stice et al., 2015) of this new treatment (Table 6). The average effects reveal four important trends. First, the average pre-post d was .98 for BPT and .36 for usual care controls in the first trial; the fact that the average effect size for the continuous outcomes was over twice as large for BPT versus usual care suggests BPT is effective and produced larger reductions in outcomes than the usual care young women with eating disordered received. Second, the average pre-to-post effect was 1.20 for BPT and .79 for supportive mindfulness treatment in the present trial; the fact that the average effect size was nearly twice as large for BPT versus supportive mindfulness treatment provides evidence that BPT is more effective, though these effects do suggest that supportive mindfulness treatment is also effective. It is important to acknowledge that expectancies, demand characteristics, and non-specific effects probably partially explain the reductions in the outcomes within condition, though those effects should have been similar for BPT and supportive mindfulness treatment. Third, the fact that the average pre-post effect for supportive mindfulness treatment (d = .79) was over twice as large as the effects for the usual care condition in the first trial (d = .36) provides additional evidence that supportive mindfulness treatment is effective. Fourth, it was encouraging that the average pre-post effect for BPT increased from .98 in the first trial to 1.20 in the present trial, as it provides evidence that the refinements we made to this new treatment may have contributed to the larger effects.
Table 6.
Comparison of Pretest to Posttest Effect Size (d-statistic) Estimates for the Initial and Present Body Project Treatment Trials.
| Initial Trial | Present Trial | |||
|---|---|---|---|---|
| BPT | Usual Care Control | BPT | Supportive Mindful Control | |
| Thin-ideal internalization | 1.23 | 0.48 | 1.33 | 0.63 |
| Dissonance about affirming thin ideal | 0.69 | 0.05 | 0.15 | 0.13 |
| Body dissatisfaction | 1.44 | 0.41 | 1.47 | 1.00 |
| Negative affect | 0.90 | 0.35 | 1.59 | 0.43 |
| Eating disorder symptoms | 0.90 | 0.53 | 1.94 | 2.22 |
| Functional Impairment | 0.72 | 0.32 | 0.72 | 0.31 |
| Average Effect | 0.98 | 0.36 | 1.20 | 0.79 |
BPT = Body Project Treatment
The fact that participants who attended more sessions and completed more home exercises showed larger reductions in outcomes implies that improving retention and home exercise completion might improve the efficacy of this treatment, as on average participants only attended 5.1 out of 8 sessions. The dose-response relation also suggests that making BPT longer than 8 sessions might also increase efficacy.
Results also suggest that BPT was somewhat more acceptable than the supportive mindfulness treatment. Participants in BPT groups attended a mean of 5.1 sessions versus 4.4 sessions for the supportive mindfulness treatment. Further, BPT participants completed an average of 70% of the home exercises, compared to 53% for the supportive mindfulness treatment. Further, 8% of participants dropped out of BPT before the posttest assessment, compared to 10% of supportive mindfulness participants. Nonetheless, a vital priority for future research will be to develop procedures for improving engagement in this new treatment, particularly given that effects were larger for participants who attended more rather than fewer sessions of BPT.
It is important to consider the limitations of this study. First, the present trial was only powered to detect medium effects in terms of differential change in outcomes across condition, but many of the between condition effects were small. This suggests that future trials comparing two credible treatments should use larger samples. Second, because we had limited sensitivity we did not use a more stringent alpha level to correct for multiple testing because this would have reduced sensitivity further and it is important to balance risk for false positive and false negative findings. However, because we only conducted 14 tests of intervention effects, not even one would have been expected to be significant based on chance alone. Further, we focused more on effect sizes than on significance when interpreting the findings. Third, all outcomes were based on self-reported data, opening up the possibility that expectancies and demand characteristics contributed to reductions in outcomes, though the use of a credible alternative treatment comparison condition should have equated these factors across conditions. Fourth, we did not have enough participants with each of type of eating disorder to allow analyses that test whether BPT produces larger effects than supportive mindfulness treatment for each eating disorder type. Fifth, we allowed participants in both conditions to receive ancillary treatment for eating disorders because we did not think it was ethical to ask that they not seek ancillary treatment if necessary, but it might have altered the estimates of intervention effects.
In conclusion, this report provides evidence that the new dissonance-based eating disorder treatment produced significantly larger reductions in dissonance regarding affirming the thin ideal, body dissatisfaction, negative affect, functional impairment, and remission from eating disorder diagnoses than was observed for a supportive mindfulness treatment typical of that offered at many universities to students with eating disorders. However, BPT versus supportive mindfulness participants did not show greater reductions in eating disorder symptoms, thin-ideal internalization, or abstinence from binge eating and compensatory behaviors. Indeed, the pattern of findings suggests that supportive mindfulness treatment also represents an effective intervention. Results from this trial, and the previous trial of BPT (Stice et al., 2015) imply that the new dissonance-based eating disorder treatment produces clinically meaningful reductions in outcomes and is more cost effective than 20-session individually administered treatments for eating disorders. We hope that with continued refinement of engagement and retention procedures and to the intervention content, it will represent an even more efficacious front-line group treatment for the range of eating disorders that could be broadly disseminated, addressing a key barrier to treating eating disorders.
Acknowledgments
This trial was supported in part by a NIH grant MH111782. This trial was registered at ClinicalTrials.gov: Identifier NCT03259347.
References
- Agras WS, Walsh BT, Fairburn CG, Wilson GT, & Kraemar HC (2000) A multicenter comparison of cognitive-behavioral therapy and interpersonal therapy psychotherapy for bulimia nervosa. Archives of General Psychiatry, 57, 459–466. [DOI] [PubMed] [Google Scholar]
- Allen K, Byrne S, Oddy W, & Crosby R (2013). DSM-IV-TR and DSM-5 eating disorders in adolescents; Prevalence, stability, and psychosocial correlates in a population-based sample of male and female adolescents. Journal of Abnormal Psychology, 122, 720–732. [DOI] [PubMed] [Google Scholar]
- Bardone-Cone A, Harney M, Maldonado C, Lawson M, Robinson D, Smith R, & Tosh A (2010). Defining recovery from an eating disorder: Conceptualization, validation, and examination of psychosocial functioning and psychiatric comorbidity. Behaviour Research & Therapy, 48, 194–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker C, Smith L, & Ciao A (2005). Reducing eating disorder risk factors in sorority members: A randomized trial. Behavior Therapy, 36, 245–253. [Google Scholar]
- Berscheid E, Walster E, & Bohrnstedt G (1973). The happy American body: A survey report. Psychology Today, 7, 119–131. [Google Scholar]
- Cooper P, & Steere J (1995). A comparison of psychological treatments for bulimia nervosa: Implications for models of maintenance. Behaviour Research and Therapy, 33, 875–885. [DOI] [PubMed] [Google Scholar]
- Crow S, Peterson C, Swanson S, Raymond N, Specker S, Eckert E, & Mitchell J (2009). Increased mortality in bulimia nervosa and other eating disorders. American Journal of Psychiatry, 166, 1342–1346. [DOI] [PubMed] [Google Scholar]
- Dare C, Eisler I, Russell G, Treasure J, & Dodge L (2001). Psychological therapies for adults with anorexia nervosa: Randomised controlled trial of outpatient treatments. British Journal of Psychiatry, 178, 216–221. [DOI] [PubMed] [Google Scholar]
- Eisler I, Dare C, Hodes M, Russell G, Dodge E, & Le Grange D (2000). Family therapy for adolescent anorexia nervosa: the results of a controlled comparison of two family interventions. Journal of Child Psychology and Psychiatry, 41, 727–736. [PubMed] [Google Scholar]
- Fairburn C, Bailey-Straebler S, Basden S, Doll H, Jones R, Murphy R et al. , (2015). A transdiagnostic comparison of enhanced cognitive behaviour therapy (CBT-E) and interpersonal psychotherapy in the treatment of eating disorders. Behaviour Research and Therapy, 70, 64–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green M, Scott N, Diyankova I, Gasser C, & Pederson E (2005). Eating disorder prevention: An experimental comparison of high level dissonance, low level dissonance, and no-treatment control. Eating Disorders, 13, 157–169. [DOI] [PubMed] [Google Scholar]
- Grilo C, Masheb R, & Wilson G (2005). Efficacy of cognitive behavioral therapy and fluoxetine for the treatment of binge eating disorder: A randomized double-blind placebo-controlled comparison. Biological Psychiatry, 57, 301–309. [DOI] [PubMed] [Google Scholar]
- Halliwell E, & Diedrichs P (2014). Brief report: Testing a dissonance body image intervention among young girls. Healthy Psychology, 33, 201–204. [DOI] [PubMed] [Google Scholar]
- Hay P (2013). A systematic review of evidence for psychological treatments in eating disorders: 2005–2012. International Journal of Eating Disorders, 46, 462–469. [DOI] [PubMed] [Google Scholar]
- Jones R, Peveler R, Hope A, & Fairburn C (1993). Changes during treatment for bulimia nervosa: a comparison of three psychological treatments. Behavior Research and Therapy, 31, 479–485. [DOI] [PubMed] [Google Scholar]
- Kirkley B, Schneider J, Agras W, & Bachman J (1985). Comparison of two group treatments for bulimia. Journal of Consulting And Clinical Psychology, 53, 43–48. [DOI] [PubMed] [Google Scholar]
- Kristeller J Wolever R, & Sheets V (2013) Mindfulness-based eating awareness training (MB-EAT) for binge eating: A randomized clinical trial. Mindfulness, 5, 282–297. [Google Scholar]
- le Grange D, Binford R, Peterson C, Crow S, Crosby R, Klein M, et al. (2006). DSM-IV threshold versus subthreshold bulimia nervosa. International Journal of Eating Disorder, 39, 462–467. [DOI] [PubMed] [Google Scholar]
- le Grange D, Crosby RD, Rathouz PJ, & Leventhal BL (2007). A randomized controlled comparison of family-based treatment and supportive psychotherapy for adolescent bulimia nervosa. Archives of General Psychiatry, 64, 1049–1056. [DOI] [PubMed] [Google Scholar]
- Lilienfeld S, Ritschel L, Lynn S, Brown A, Cautin R, & Latzman R (2013). The research-practice Gap: Bridging the schism between eating disorder researchers and practitioners. International Journal of Eating Disorders, 46, 386–394. [DOI] [PubMed] [Google Scholar]
- Linardon J, Fairburn C, Fitzsimmons-Craft E, Wilfley D, & Brennan L (2017). The empirical status of the third-wave behavior therapies for the treatment of eating disorders: A systematic review. Clinical Psychology Review, 58, 125–140. [DOI] [PubMed] [Google Scholar]
- McIntosh V, Jordan J, Carter F, Luty S, McKenzie J, Bulik C, et al. , (2005). Three psychotherapies for anorexia nervosa: a randomized, controlled trial. American Journal of Psychiatry, 162, 741–747. [DOI] [PubMed] [Google Scholar]
- Mitchell K, Mazzeo S, Rausch S, & Cooke K (2007). Innovative interventions for disordered eating: Evaluating dissonance-based and yoga interventions. International Journal of Eating Disorders, 40, 120–128. [DOI] [PubMed] [Google Scholar]
- Müller S & Stice E (2013). Moderators of the intervention effects for a dissonance-based eating disorder prevention program; results from an amalgam of three randomized trials. Behaviour Research and Therapy, 51, 128–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munsch S, Biedert E, Meyer A, Michael T, Schlup B, Tuch A, & Margraf J (2007). A randomized comparison of cognitive behavioral therapy and behavioral weight loss treatment for overweight individuals with binge eating disorder. International Journal of Eating Disorders, 40, 102–113. [DOI] [PubMed] [Google Scholar]
- Peterson C, Mitchell J, Crow S, Crosby R, & Wonderlich S (2009). The efficacy of self-help group treatment and therapist-led group treatment for binge eating disorder. The American Journal of Psychiatry, 166, 1347–1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safer D, Robinson A, & Jo B (2010). Outcome from a randomized controlled trial of group therapy for binge eating disorder: comparing dialectical behavior therapy adapted for binge eating to an active comparison group therapy. Behavior Therapy, 41, 106–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt U, Magill N, Renwick B, Keyes A, Kenyon M, Dejong H, et al. , (2015). The Maudsley Outpatient Study of Treatments for Anorexia Nervosa and Related Conditions (MOSAIC): Comparison of the Maudsley Model of Anorexia Nervosa Treatment for Adults (MANTRA) with specialist supportive clinical management (SSCM) in outpatients with broadly defined anorexia nervosa: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 83, 796–807. [DOI] [PubMed] [Google Scholar]
- Spielmans G, Benish S, Marin C, Bowman W, Menster M, & Wheeler A (2013). Specificity of psychological treatments for bulimia nervosa and binge eating disorder? A meta-analysis of direct comparisons. Clinical Psychology Review, 33, 460–469. [DOI] [PubMed] [Google Scholar]
- Stice E, Butryn M, Rohde P, Shaw H, & Marti N (2013). An effectiveness trial of a new enhanced dissonance eating disorder prevention program among female college students. Behaviour Research and Therapy, 51, 862–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti N, & Rohde P (2013). Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. Journal of Abnormal Psychology, 122, 445–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti N, Spoor S, Presnell K, & Shaw H (2008). Dissonance and healthy weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology, 76, 329–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Butryn M, Menke KS, & Marti CN (2015). Randomized controlled pilot trial of a novel dissonance-based group treatment for eating disorders. Behaviour Research and Therapy, 65, 67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Shaw H, & Gau J (2017). Clinician-led, peer-led, and Internet-delivered dissonance-based eating disorder prevention programs: Acute effectiveness of these delivery modalities. Journal of Consulting and Clinical Psychology, 85, 883–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Burton E & Wade E (2006). Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. Journal of Consulting and Clinical Psychology, 74, 263–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Striegel-Moore R, Leslie D, Petrill S, Garvin V, & Rosenheck R (2000). One-year use and cost of inpatient and outpatient services among female and male patients with an eating disorder: Evidence from a national database of health insurance claims. International Journal of Eating Disorders, 27, 381–389. [DOI] [PubMed] [Google Scholar]
- Swanson S, Crow S, Le Grange D, Swendsen J, & Merikangas K (2011). Prevalence and correlates of eating disorders in adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry, 68, 714–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treasure J, Todd G, Brolly M, Tiller J, Nehmed A, & Denman F (1995). A pilot study of a randomised trial of cognitive analytical therapy vs educational behavioural therapy for adult anorexia nervosa. Behavioural Research and Therapy, 33, 363–367. [DOI] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1992). Affects separable and inseparable: On the hierarchical arrangement of the negative affects. Journal of Personality Social Psychology, 62, 489–505. [Google Scholar]
- Weissman M & Bothwell S (1976). Assessment of social adjustment by patient self-report. Archives of General Psychiatry, 33, 1111–1115. [DOI] [PubMed] [Google Scholar]
- Wilfley D, Welch R, Stein R, Spurrell E, Cohen L, Saelens B, et al. , (2002). A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Archives of General Psychiatry, 59, 713–721. [DOI] [PubMed] [Google Scholar]
- Wilson G, & Zandberg L (2012). Cognitive–behavioral guided self-help for eating disorders: Effectiveness and scalability. Clinical Psychology Review, 32, 343–357. [DOI] [PubMed] [Google Scholar]
- Wilson G, Wilfley D, Agras W, & Bryson S (2010). Psychological treatments for binge eating disorder. Archives of General Psychiatry, 67, 94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wonderlich S, Peterson C, Crosby R, Smith T, Klein M, Mitchell J, & Crow J (2014). A randomized controlled comparison of integrative cognitive-affective therapy (ICAT) and enhanced cognitive-behavioral therapy (CBT-E) for bulimia nervosa. Psychological Medicine, 44, 543–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandberg L, & Wilson G (2013). Train-the-trainer: Implementation of cognitive behavioural guided self-help for recurrent binge eating in a naturalistic setting. European Eating Disorders Review, 21, 230–237. [DOI] [PubMed] [Google Scholar]


