Abstract
Background:
Asthma is common in children with indoor pollutants influencing the development of the disease. Since children spend most of their time outside their homes within the school environment, school indoor air quality can directly influence their respiratory health.
Aims:
This study aims to analyze the indoor and outdoor air quality of Maltese schools and if an association exists between indoor pollutants and respiratory health in children.
Settings and Design:
Five primary schools were selected with 9- to 11-year-old students participating.
Materials and Methods:
Standardized health questionnaires and lung function tests were utilized. Indoor and outdoor air sampling together with traffic counts were carried out.
Statistical Analysis Used:
SPSS version 21 was used and the Chi-squared, logistic regression, and Pearson's correlation were used.
Results:
The mean indoor PM 2.5 level of 17.78 μg/m3 and CO (9.11 ppm) exceeded World Health Organization thresholds. Indoor ozone levels exceeded the mean European school's indoor ozone concentration of 8 μg/m3. High exposure to formaldehyde, NO2, and ozone was associated with atopy in children. Heavy vehicles passing near the schools were associated with current wheezing (P < 0.001) but not nocturnal cough (P = 0.34).
Conclusions:
School indoor and outdoor environment has a direct impact on children's respiratory health. This study has identified significant associations between high exposures to indoor air pollutants, school characteristics, and upper and lower airway inflammation.
Keywords: Asthma, atopy, ozone, school
INTRODUCTION
The International Study of Asthma and Allergies in Childhood (ISAAC) study has shown a significant increase in prevalence of wheezing in the previous 12 months in most regions of the Maltese Islands in 5- to 8-year-old children[1] between ISAAC Phases 1 (1990) and 3 (2001). Genetic components together with several environmental factors must influence the geographical distribution of wheezing in the Maltese Islands. More research is needed to identify the causes of atopy focusing specifically on school indoor air quality since children spend most of their time outside their house within the school environment. This knowledge will help in the development of a national preventive strategy so as to decrease the risk of asthma for children and to identify which pollutants are affecting the air quality of schools.
MATERIALS AND METHODS
Data collection
Five primary state schools were selected randomly from five geographical clusters of schools designated north, south, central, east, and west. Three classrooms within each school were selected among the 9- to 11-year age group with all students asked to participate. The classrooms were randomly selected by ballot system so as to eliminate potential bias. Primary state schools in Malta are coeducational.
Ethical approval and consent
This study was approved by the University of Malta Research Ethics Committee and the Education Department Research Directorate.
Health assessment and school characterization
Standardized ISAAC health questionnaires focusing on wheezing, rhinitis, and eczema were answered by the children's parents. Lung function tests, acoustic rhinometry, exhaled NO, exhaled CO, and nasal lavage were performed on the participating children. Characterization of each participating school was performed focusing on the school building, classrooms, cleaning/maintenance protocols, and the outdoor environment.
Chemical and physical parameters
A total of 16 parameters were measured per school in parallel in each of the three individual classrooms. Outdoor sampling was carried out simultaneously during the same period. Methods of air sampling were based on the International Organization for Standardization (ISO) 16000 series.[2]
Radiello passive diffusive tubes (Fondazione Salvatore Maugeri) were utilized for benzene, trichloroethylene, tetrachloroethylene, formaldehyde, pinene, limonene, NO2, and ozone. Carbon monoxide, CO2, temperature, and humidity were measured continuously using TSI 7525 IAQ-Calc low-cost loggers, whereas PM 10 levels were measured using a portable HAZ-DUST EPAM-5000 light scattering monitor. The gravimetric method was utilized for PM 2.5 measurements using SKC Leland Air Sampling Sample Pumps with the particulate matter being analyzed for chlorates and perchlorates. Passive radon detectors were exposed for 30 days within each of the participating classrooms and CO2 levels were used to calculate ventilation rates.
Sampling within the schools took place over a 5-day period (Monday morning until Friday afternoon). In the case of passive air sampling techniques, the reported pollutants were time averaged. Due to the fact that PM 2.5 levels are closely related to occupancy density (m2 per child), the PM 2.5 samples for gravimetric analysis were collected during teaching hours starting at 8 am and ending at 14.30 pm in all the participating schools.
Statistical analysis
Data were transferred to IBM SPSS Statistics version 21 Inc. (Chicago, IL, USA) for analysis. For statistical significance, a P value cutoff point of 0.05 was adopted. In the case of multiple comparisons, the Bonferroni correction was applied to avoid inflation of the Type 1 error. Regression analysis was used to eliminate any possible confounding factors.
RESULTS
Indoor
The indoor levels of pollutants and physical parameters from all five schools are shown in Table 1 together with the respective recommended short- and long-term exposure cutoff values as recommended in published guidelines. Mean levels of long-term exposure that exceed any published recommendations and guidelines are presented in bold. The data have also been compared with the SINPHONIE study due to the similar methodologies used.[3]
Table 1.
Indoor chemical and physical parameters compared with published guidelines and Schools Indoor Pollution and Health Observatory Network in Europe results
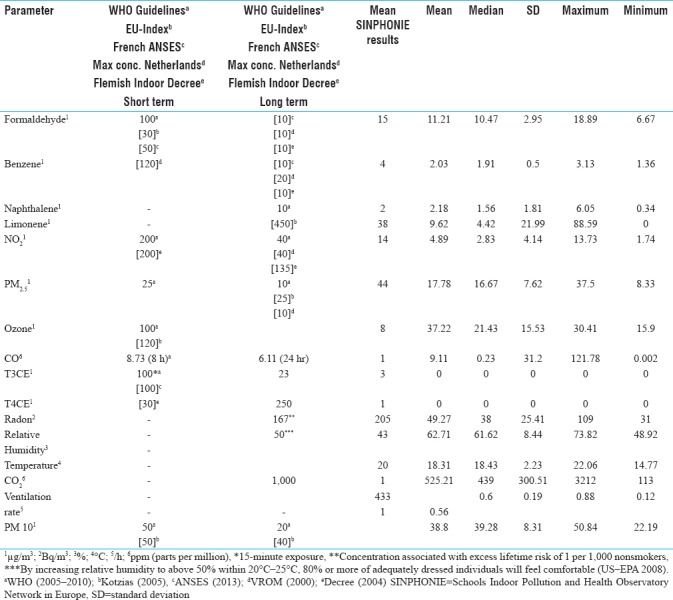
The mean indoor PM 2.5 level of 17.78 μg/m3 exceeded the long-term World Health Organization (WHO) recommended levels[4] with 86.67% of classrooms having levels above the WHO limit, whereas the short-term (24 hour) threshold was exceeded in 13.33% of classrooms. The indoor PM 10 level was higher than long-term WHO threshold of 20 μg/m3 with all classrooms having levels above the WHO limit.[5]
Ozone levels in all five schools were below the WHO[5] recommended indoor ozone threshold of 100 μg/m3; however, all classrooms exceeded the mean European school indoor ozone concentration[3] of 8 μg/m3. The mean indoor carbon monoxide level (9.11 ppm) exceeded both WHO exposure levels[4] and indoor SINPHONIE mean of 1 ppm.[3] The mean indoor CO2 during school hours was 634.32 ppm (SD 201.34 ppm) with peak levels of 32,12 ppm detected. Relative humidity within Maltese classrooms was 62.71% with all classrooms being more humid than their European counterparts (43%).[3]
Outdoor
Outdoor samples for all pollutants and physical parameters were taken in each of the five schools as shown in Table 2. The mean outdoor ozone level in all five schools was 251.36 μg/m3 (SD70.44), which exceeded both the recommended maximum WHO 8-hour mean ozone[5] threshold of 100 μg/m3 and the southern European[3] outdoor mean ozone levels (Cluster 4: 100.41 μg/m3). Both PM 2.5 and PM 10 levels exceeded the WHO long-term exposure limits of 10 and 20 μg/m3, respectively.[5] Local outdoor PM 2.5 levels were lower than southern European[3] mean levels of 31.67 μg/m3.
Table 2.
Outdoor chemical and physical parameters compared with Schools Indoor Pollution and Health Observatory Network in Europe results
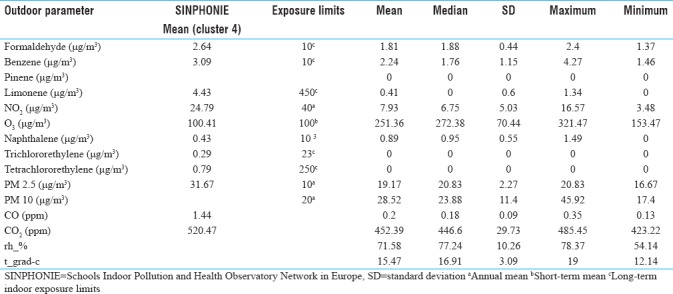
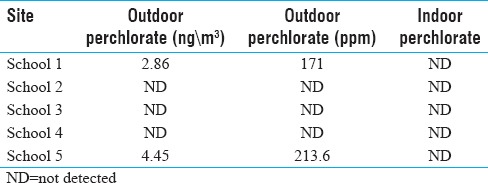
Both indoor and outdoor samples of PM 2.5 were analyzed for the presence of perchlorate residues with two sites (schools 1 and 2) outdoor PM 2.5 having traces of this chemical [Table 3].
Table 3.
Perchlorate levels detected in PM 2.5 samples
Traffic counts carried out in streets bordering the individual schools detected a total of 942 light cars and 87 heavy good vehicles (94 light cars and 9 heavy goods vehicles per school per hour) passing by the schools during the sampling period. A significant positive correlation was found between the numbers of light and heavy vehicles passing by the schools (r = 0.42; P = 0.007) [Figure 1].
Figure 1.
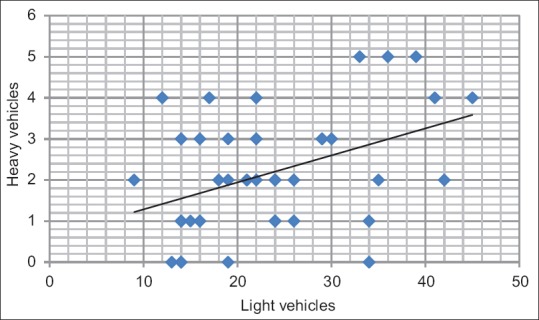
Correlation between light and heavy vehicles passing near the selected schools (r = 0.42, P = 0.007)
Association between exposure to pollutant and environmental parameters and health outcomes
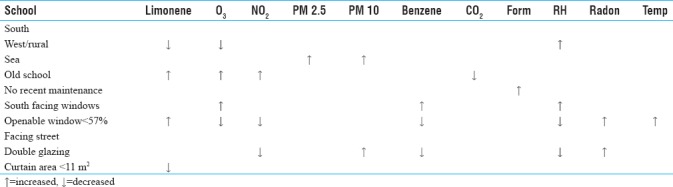
The odds ratios between symptomatology, school characteristics, and environmental exposures were determined by comparing symptoms with high- versus low-exposure levels to the particular irritant. The high-exposure category consisted of pollutant levels equal to or more than the second tertile of concentrations, whereas lower levels of pollutant were defined as low exposure. A logistic regression model was designed so as to eliminate potential confounding factors. Significant associations were found between high exposure to indoor chemical pollutants, such as formaldehyde, NO2, and ozone, and upper and lower airway atopy [Table 4]. Classroom and window characteristics, school cleaning/maintenance protocols, and location were also significantly associated with a high exposure to indoor pollutants [Table 5].
Table 4.
Impact of high exposure to pollutants on children's health
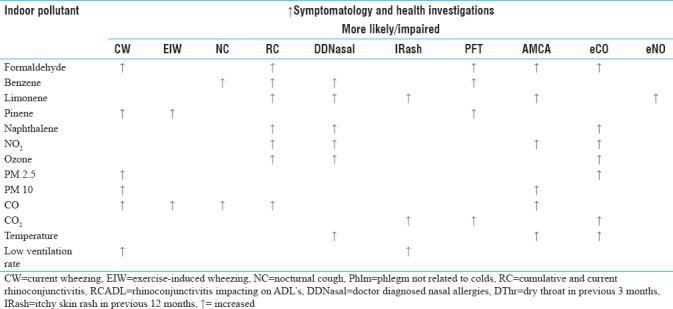
Table 5.
Impact of school characteristics on indoor pollutant exposure risk
A significant association was seen between light car traffic, current wheezing (P < 0.001), rhinoconjunctivitis in the previous 12 months (P < 0.001), and doctor diagnosed allergic rhinitis (P = 0.002). Heavy vehicles passing near the schools were associated with current wheezing (P < 0.001) but not nocturnal cough (P = 0.34).
DISCUSSION
Summary of key findings
Indoor formaldehyde, particulate matter (PM 2.5 and PM 10), CO, outdoor particulate matter (PM 2.5, PM 10), and ozone exceeding recommended international thresholds
Perchlorate residues were detected in outdoor PM 2.5 samples collected from schools 1 and 5 several months after the feast season had ended
Old buildings, south facing windows, and cleaning/maintenance schedules were found to have an increased risk of exposure to limonene, CO, and outdoor pollutants (NO2 and ozone).
Indoor formaldehyde, particulate matter (PM 2.5 and PM 10), CO, outdoor particulate matter (PM 2.5, PM 10), and ozone exceeded recommended international thresholds. The primary source of formaldehyde is the natural environment; however, man-made sources also contribute to indoor formaldehyde mainly due to the widespread use of fixatives and preservatives in furniture together with fuel combustion activities and tobacco smoke.[4] Oxidation of volatile organic compounds and reactions between outdoor ozone and alkenes also influence the distribution of indoor formaldehyde.[4] Computers have also been implicated as significant sources of indoor formaldehyde.[6]
This is particularly relevant due to the fact that each class had four computers, which were switched on during school hours. These findings suggest that indoor formaldehyde in schools is a potential cause of poor indoor air quality that needs to be tackled using specific abatement techniques, such as improved ventilation, ultra-low-emitting formaldehyde furniture, strict enforcement of no-smoking policies, and the use of low-VOC paint products.[7] School policy should also recommend the switching off of all class electronic equipment including computers and printers when not in use.[6]
Both mean indoor and outdoor PM 2.5 and PM 10 levels exceeded long-term WHO levels.[4] This study has shown that PM 10 originated mainly from within the indoor school environment (I/O ratio 1.34), which can be explained by the fact that all the local schools are built using lime stone and concrete/cement bricks that tend to shed off surface dust especially if not properly maintained or exposed to corrosive sea air. Car ownership in Malta is exceedingly high with the fifth highest number of vehicles per capita in the world, and as of 2009, there were 607 motor vehicles per 1000 people.[8] Combustion engines are a major source of PM 2.5,[5] thus accounting for the high levels of PM 2.5 detected within and around the school indoor environment especially when considering that a traffic count near the selected schools showed a mean of 94 light cars and 9 heavy goods vehicles passing beside each school per hour. Better traffic management around schools is, therefore, needed so as to minimize the exposure of both children and staff to emissions especially particulate matter.
Perchlorate is an inorganic anion used as a propellant in fireworks, with a potential negative impact in humans and the environment due to contamination of the food chain[9,10] resulting in thyroid pathology. Perchlorate is also found naturally in the environment in areas rich in nitrate deposits and potash.[11] Interestingly perchlorate residues were detected in outdoor PM 2.5 samples collected from schools 1 and 5 several months after the feast season had ended. These results suggest that perchlorate might influence both short- and long-term local air quality with potential damage to the health of humans especially children.[11]
NO2 is mainly produced by the combustion of fossil fuels and a reaction between ozone and NO in the atmosphere.[5] We hypothesize that high temperatures and increased solar radiation that characterize the Maltese climate[12] might explain the relatively low levels of NO2 detected in this study.
Ozone is another potential confounding variable that could influence the distribution of NO2 since an increase in ozone is accompanied by low NO2 levels.[13] Although indoor ozone levels in all five schools were below the WHO[5] recommended indoor ozone threshold of 100 μg/m3, these were higher than the mean levels found in European schools.[3] Potential indoor sources include laser printers and photocopiers.
This indoor pollutant, therefore, should still be considered as a potential cause for poor indoor air quality in schools. Furthermore, the outdoor mean ozone concentration exceeded WHO limits, thus confirming that abatement measures for this pollutant are urgently needed. Solar radiation catalyzes a reaction between nitrogen oxides (NOx) and VOCs and is, in turn, degraded by reacting with NO2.[5] This means that the local climate, characterized by elevated temperatures and a high amount of solar radiation, favors the production of ozone. Suqin et al.[13] have shown that wind direction influences the ozone concentration with NE-N winds being associated with low ozone levels, whereas SW-S-SE winds (and associated higher temperatures) favored higher concentrations of ozone. Since these wind directions correspond with the predominant wind directions found in the Maltese Islands,[12] local ozone trends might be influenced by the prevailing winds.
School building
High indoor exposures to benzene and NO2 in central/urban schools highlight the impact of the outdoor environment on indoor air quality. This is particularly relevant in these densely populated areas characterized by narrow streets, high-volume idling traffic, and industrial activities. The prevailing warm, humid southerly winds[12] might increase indoor school contamination with microbiological pollutants in settled dust. Particulate matter in Malta is characterized by high levels of salt and Sahara dust.[14] This explains the increased risk of high exposure to particulate matter in schools located near the sea. Salt air is corrosive and will cause degradation of limestone and cement products, thus increasing the particulate matter burden within the building. Schools near the sea had high levels of indoor PM 10, which could account for the increased risk of atopy and abnormal pulmonary function tests seen among the students. The importance of school building age has been recently recognized as being one of the contributing factors for school indoor air quality.[15] Students in schools housed in old buildings were found to have an increased risk of exposure to limonene, CO, and outdoor pollutants (NO2 and ozone).
Classrooms
Classes with south facing windows were associated with high exposure to pollutants such as benzene, ozone, and NO2, which were predominantly sourced from the outdoor environment. The most common wind direction in the Maltese Islands is the north-westerly wind followed by west southwest winds (8.9%) and the south southwest wind (7.8%).[12]
These predominant winds must push outdoor environmental irritants into the inside of the classroom, thus accounting for the increased prevalence of allergies in children residing in classrooms having south or west window orientations.
Current wheezing, pollen allergies, and increased exhaled CO were more likely in classrooms situated near a street, highlighting the possible impact of traffic on the children's health status. Exhaled CO can arise either secondary to exogenous inhalation such as that derived from traffic or could be considered as an independent marker of airway inflammation.[16]
Cleaning and maintenance schedules
Several different floor cleaning practices were observed with intensive cleaning regimens being associated with atopic disease and increased risk of high exposure to particulate matter (PM 2.5 and PM 10). This cleaning practice must resuspend previously settled dust from the floor with deleterious effects on the indoor air quality.
Outdoor school environment
Pupils sitting in classrooms facing the street had the highest risk of atopy and were more likely to have a high indoor exposure to limonene, NO2, ozone, and carbon monoxide. Traffic was the most likely source of NO2, ozone, and carbon monoxide in these schools with wheezing and upper airway symptoms significantly related to the amount of light and heavy vehicles passing near the school. High exposures to indoor limonene in these classes could be explained by the fact that teachers within these classes tend to keep most of the windows closed at specific times of the day due to traffic-related noise and fumes.
Association between exposure to pollutant, environmental parameters, and health outcomes
This study has identified a direct association between wheezing and high exposure to indoor formaldehyde, pinene, particulate matter (PM 10, PM 2.5), and carbon monoxide, whereas students exposed to high benzene levels were more likely to complain of a nocturnal cough. Similar associations were observed between exposure to these pollutants and impaired spirometry, exhaled CO, and exhaled NO. Formaldehyde,[17,18] VOC,[19] PM 2.5,[20] and CO[21] exposure have been associated with asthma, whereas Csobod et al.[22] have described an increased prevalence of nocturnal cough with high exposure to indoor PM 10 and benzene.[23] The increased nasal lavage lysozyme seen in this study provides objective evidence about the strong inflammatory effect of PM 10 and VOC exposure in children.
Elevated exposures to VOC, NO2, ozone, and CO were significantly related to upper airway symptomatology, reduced mean cross-sectional nasal areas, and nasal volumes among the participating students. Upper airway atopy has been described following exposure to VOC,[20,24] but very little data exist about the role of other pollutants listed above. NO2 has been associated with respiratory disease and skin atopy,[20] whereas conflicting results have been published regarding the association between ozone exposure and the health of school children. This study has shown a significant association between NO2 and CO exposure and reduced nasal cross-sectional volumes, whereas high exposure to ozone was associated with increased CO levels. One can speculate that exposure to these irritants is responsible for upper airway atopy.
The prevalence of wheezing in school children was lower in classrooms having higher temperatures;[19] however, children were more likely to complain of breathlessness.[25] Maltese school children were more likely to complain of nasal allergies and have narrow nasal cross sectional areas in warm classrooms. High levels of indoor relative humidity were also significantly associated with decreased nasal cross-sectional areas and volumes. No studies have linked rhinitis with increasing temperature, although a weak association exists with the prevalence of sinusitis.[26] The local findings might be explained by the fact that warm and/or humid classrooms increased the growth of bacteria and fungi, thus potentially increasing the exposure levels to these pollutants.
Strengths and limitations of study
An even distribution of males and females eliminated gender bias. Due to the small size of the country, there were no confounding microclimates and the children resided in the town where the school was located. The high participation rate among the students was advantageous. The absolute majority of participating children were Caucasian, thus eliminating ethnicity as a potential confounding factor.
Chemical pollutants were measured using standardized methodology and quality control. The main limitation of this study is the relatively small number of children participating when compared with studies such as ISAAC. The selected age group differs from ISAAC protocol, thus resulting in potential problems when comparing the two studies. Although not a limitation to this study, it is worth mentioning that lung function tests were not performed within the domestic environment due to logistical reasons. CO2 data interpretations might result in the overestimation of ventilation rates.
CONCLUSIONS
This study proves that school indoor and outdoor environment has a direct impact on children's respiratory health. School indoor air quality is dependent on the school/classroom characteristics and exposure levels to several indoor chemical and biological pollutants, which themselves induce atopy. This study has identified significant associations between high exposures to indoor air pollutants; school characteristics including building, classroom, and cleaning/maintenance schedules; and upper and lower airway inflammation. Recommendations to improve school indoor air quality can, therefore, be presented to the relevant authorities so as to obtain the best health status for our present and future children. Schools are controlled areas where policies can be rigorously implemented, thus achieving the best possible outcomes.
Financial support and sponsorship
The study was supported by a research grant awarded by the University of Malta Faculty of Medicine and Surgery. Further support was provided by the SINPHONIE Study (DG SANCO).
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fsadni P, Ellul P, Montefort M, Caruana S, Agius Muscat H, Montefort S. ISAAC Malta: Changes in geographical distribution of wheezing children in Malta between 1994 and 2002. J Asthma Allergy Educ. 2012;5:208–14. [Google Scholar]
- 2.Indoor air – Part 1: General Aspects of Sampling Strategy. 2004. [Last accessed on 2018 Mar 08]. Available from: https://www.iso.org/standard/39844.html .
- 3.Csobod E, Annesi-Maesano I, Carrer P, Kephalopoulos S, Madureira J, Rudnai P, et al. SINPHONIE (Schools Indoor Pollution and Health Observatory Network in Europe) – Final Report. Co-published by the European Commission's Directorates General for Health and Consumers and Joint Research Centre, Luxembourg. 2014 [Google Scholar]
- 4.World Health Organization. WHO Guidelines for Indoor Air Quality: Selected Pollutants. Copenhagen: WHO Regional Office for Europe; 2010. [PubMed] [Google Scholar]
- 5.World Health Organization. Air Quality Guidelines Global Update 2005 Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide. World Health Organization. 2005 [Google Scholar]
- 6.McKone T, Maddalena R, Destaillats H, Hammond K, Hodgson A, Russel M, et al. Indoor pollutant emissions from electronic office equipment. Atmos Environ. 2008;42:1371–88. [Google Scholar]
- 7.U.S. Environmental Protection Agency. Protect Against Exposure on Formaldehyde. 2014 [Google Scholar]
- 8.NationMaster – Transportation Statistics. [Last retrieved on 2009 Oct 21]. Available from: http://www.nationmaster.com/country/mt-malta/tra-transportation .
- 9.Sijimol MR, Mohan M. Environmental impacts of perchlorate with special reference to fireworks – A review. Environ Monit Assess. 2014;186:7203–10. doi: 10.1007/s10661-014-3921-4. [DOI] [PubMed] [Google Scholar]
- 10.Food and Agriculture Organization of the United Nations. Working Document for Information and use in Discussions Related to Contaminants and Toxins in the GSCTFF. 2011 Mar [Google Scholar]
- 11.Gouder C, Montefort S. Potential impact of fireworks on respiratory health. Lung India. 2014;31:375–9. doi: 10.4103/0970-2113.142124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galdies C. The Climate of Malta: Statistics, Trends and Analysis, 1951-2010. Valletta: National Statistics Office; 2011. p. 45.p. viii. [Google Scholar]
- 13.Han S, Bian H, Feng Y, Liu A, Li X, Zeng F, Zhang X. Analysis of the Relationship between O3, NO and NO2in Tianjin, China. Aerosol Air Qual Res. 2011;11:128–39. [Google Scholar]
- 14.Malta Environment and Planning Authority. Malta Environment and Planning Authority. Justification Report on the Contribution of Natural Events to the PM 10 Daily Limit Value. MEPA. 2010 [Google Scholar]
- 15.Mori M, Hara K, Miyakita T, Ishitake T. Association of indoor air quality with physical health of users in a newly built school building in a university. Nihon Eiseigaku Zasshi. 2011;66:122–8. doi: 10.1265/jjh.66.122. [DOI] [PubMed] [Google Scholar]
- 16.Paredi P, Leckie MJ, Horvath I, Allegra L, Kharitonov SA, Barnes PJ, et al. Changes in exhaled carbon monoxide and nitric oxide levels following allergen challenge in patients with asthma. Eur Respir J. 1999;13:48–52. doi: 10.1183/09031936.99.13104899. [DOI] [PubMed] [Google Scholar]
- 17.Zhao Z, Sebastian A, Larsson L, Wang Z, Zhang Z, Norbäck D, et al. Asthmatic symptoms among pupils in relation to microbial dust exposure in schools in Taiyuan, china. Pediatr Allergy Immunol. 2008;19:455–65. doi: 10.1111/j.1399-3038.2007.00664.x. [DOI] [PubMed] [Google Scholar]
- 18.Smedje G, Norbäck D. Irritants and allergens at school in relation to furnishings and cleaning. Indoor Air. 2001;11:127–33. doi: 10.1034/j.1600-0668.2001.110207.x. [DOI] [PubMed] [Google Scholar]
- 19.Smedje G, Norbäck D, Edling C. Asthma among secondary schoolchildren in relation to the school environment. Clin Exp Allergy. 1997;27:1270–8. [PubMed] [Google Scholar]
- 20.Annesi-Maesano I, Hulin M, Lavaud F, Raherison C, Kopferschmitt C, de Blay F, et al. Poor air quality in classrooms related to asthma and rhinitis in primary schoolchildren of the french 6 cities study. Thorax. 2012;67:682–8. doi: 10.1136/thoraxjnl-2011-200391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pénard-Morand C, Raherison C, Charpin D, Kopferschmitt C, Lavaud F, Caillaud D, et al. Long-term exposure to close-proximity air pollution and asthma and allergies in urban children. Eur Respir J. 2010;36:33–40. doi: 10.1183/09031936.00116109. [DOI] [PubMed] [Google Scholar]
- 22.Csobod E, Rudnai P, Vaskovi E. School Environment and Respiratory Health of Children (Search) The Regional Environmental Center for Central and Eastern Europe Country Office Hungary. 2010 [Google Scholar]
- 23.MICROMEDEX Thomson. Benzene CAS RN: 71-43-2. 2004. [Last accessed on 2018 Jan 20]. Available from: http://www.webwiser.nlm.nih.gov .
- 24.Norbäck D, Wålinder R, Wieslander G, Smedje G, Erwall C, Venge P, et al. Indoor air pollutants in schools: Nasal patency and biomarkers in nasal lavage. Allergy. 2000;55:163–70. doi: 10.1034/j.1398-9995.2000.00353.x. [DOI] [PubMed] [Google Scholar]
- 25.Mi YH, Norbäck D, Tao J, Mi YL, Ferm M. Current asthma and respiratory symptoms among pupils in Shanghai, China: Influence of building ventilation, nitrogen dioxide, ozone, and formaldehyde in classrooms. Indoor Air. 2006;16:454–64. doi: 10.1111/j.1600-0668.2006.00439.x. [DOI] [PubMed] [Google Scholar]
- 26.Bhattacharyya N. Does annual temperature influence the prevalence of otolaryngologic respiratory diseases? Laryngoscope. 2009;119:1882–6. doi: 10.1002/lary.20613. [DOI] [PubMed] [Google Scholar]


