Abstract
Few conceptual frameworks attempt to connect disaster‐associated environmental injuries to impacts on ecosystem services (the benefits humans derive from nature) and thence to both psychological and physiological human health effects. To our knowledge, this study is one of the first, if not the first, to develop a detailed conceptual model of how degraded ecosystem services affect cumulative stress impacts on the health of individual humans and communities. Our comprehensive Disaster‐Pressure State‐Ecosystem Services‐Response‐Health model demonstrates that oil spills, hurricanes, and other disasters can change key ecosystem components resulting in reductions in individual and multiple ecosystem services that support people's livelihoods, health, and way of life. Further, the model elucidates how damage to ecosystem services produces acute, chronic, and cumulative stress in humans which increases risk of adverse psychological and physiological health outcomes. While developed and initially applied within the context of the Gulf of Mexico, it should work equally well in other geographies and for many disasters that cause impairment of ecosystem services. Use of this new tool will improve planning for responses to future disasters and help society more fully account for the costs and benefits of potential management responses. The model also can be used to help direct investments in improving response capabilities of the public health community, biomedical researchers, and environmental scientists. Finally, the model illustrates why the broad range of potential human health effects of disasters should receive equal attention to that accorded environmental damages in assessing restoration and recovery costs and time frames.
Keywords: conceptual model, environmental disasters, ecosystem services, human health, stress and health problems, Gulf of Mexico
Key Points
We present a Disaster‐Pressure State‐Ecosystem Services‐Response‐Health framework linking disaster‐degraded ecosystem services to health
Damaged ecosystem services produce acute, chronic, and cumulative stress that are associated with adverse health outcomes in humans
Disaster‐related health effects deserve more attention in planning for future disasters and improving response and restoration efforts
1. Introduction
Humans have been coping with disasters for millennia and in doing so helped shape human development and cultural evolution [Torrence and Grattan, 2002]. Despite this long history of events, impacts, and reactions, the science of disaster management and response is relatively new [Lindell, 2013; Lurie et al., 2013]. While the last several decades have demonstrated rapid advances in our ability to prepare for, respond to, and recover from many kinds of disasters, their occurrences and levels of impacts to humans are increasing at an alarming rate. Since 1990, climate‐weather or geophysical natural disasters have impacted about 217 million people per year globally [Learning and Guha‐Sapir, 2013]. These authors reported a substantial upsurge in such disasters since 1989, with nearly 80% of the overall increase accounted for by a sharp surge in “climate‐related events,” which have been exacerbated by increasing urbanization, deforestation, and environmental degradation. Moreover, many of the worst technological disasters in recorded history, including oil spills in marine environments, have occurred since the 1970s [Aguilera et al., 2010; Krejsa, 1997; Lurie et al., 2013; Silei, 2014].
The recent history of disasters in the United States underscores the magnitude of these impacts in terms of both economic damage and human health effects. In 2005, the U.S. saw approximately $160 billion (B) in disaster damages, of which about $85 B and >1800 deaths resulted from Hurricane Katrina alone [Colgan and Adkins, 2006; National Oceanic and Atmospheric Administration (NOAA), 2016; Sutton‐Grier et al., 2015]. In 2012, there were 11 weather disasters in the U.S. that resulted in 377 deaths and >$110 B in damages, including Hurricane Sandy which accounted for > $70 B in damages in the U.S. [Sutton‐Grier et al., 2015; U.S. Department of Commerce [USDOC], 2013]. The 2010 Deepwater Horizon (DWH) oil catastrophe resulted in 11 deaths and the release of ~5 million barrels of oil into the Gulf of Mexico ecosystem [McNutt et al., 2012]. Payments required of BP and the other responsible parties, including for natural resource damages, previously estimated at ~$54 B, have now approached ~$62 B [Bomey, 2016; Gilbert and Kent, 2015]. However, even this amount does not account for the majority of already documented and likely additional long‐term impacts to human health and well‐being nor the overall impact to the Gulf Coast economy. Adkins [2015] assessed the impacts to GDP (gross domestic product) in coastal areas of Louisiana, Mississippi, and Alabama a decade after hurricanes Katrina and Rita. While GDP in the shore‐adjacent counties and parishes had grown at 3+ % annually from 2000 to 2005, GDP declined in 2006 and 2007 and only reached 2005 levels again in 2010, just before the DWH catastrophe. Since 2010, GDP of the same shore‐adjacent counties and parishes has hovered around 2004 levels.
In addition to economic impact, most disaster response efforts focus on acute injury and exposures (e.g., to infectious disease, toxic substances, or toxins). As a result, a considerable body of literature has documented mostly acute and some chronic human health effects from oil spills, hurricanes, and other natural and technological disasters [e.g., Aguilera et al., 2010; Cheong et al., 2011; Institute of Medicine, 2007; Jung et al., 2013; Keim, 2011; Laffon et al., 2016; Manuel, 2013; Rhodes et al., 2010; Shultz et al., 2015]. Here we do not focus on these direct and often significant impacts to human health that can be as severe as death, largely because they are generally well recognized. Chronic effects of disasters on the health of either humans or the environment, in particular, effects that degraded ecosystem services, the benefits humans derive from nature [Millennium Ecosystem Assessment [MEA], 2005], may have on health, appear to have received less attention than more immediate and direct threats. For example, the 1984 chemical explosion in Bhopal, India, also impacted critical ecosystem services such as clean water, but it is much better known—and rightly so—for the illnesses and massive loss of life it caused [Broughton, 2005; Varma and Varma, 2005]. Even in cases of extreme oil spills in the U.S., such as the DWH catastrophe or the 1989 Exxon Valdez oil spill in Prince William Sound, Alaska, there has been much less emphasis on acute or chronic human health impacts, likely because these are not covered under the Oil Pollution Act of 1990. This act is the primary legislation that controls how the U.S. manages, responds to, determines responsibility for, and assesses damages resulting from oil spills. Perhaps, even more importantly, the policy for dealing with human health impacts of disasters tends to be primarily focused on reactive, after‐the‐event responses [Cutter and Zoback, 2013; Lurie et al., 2013].
There has been as fair amount of effort to develop conceptual models that relate stressor‐caused environmental damage, including climate change, to certain human health and well‐being outcomes [e.g., Abramson et al., 2015; Bradley and Yee, 2015; Briggs, 1999; Hambling et al., 2011; Jackson et al., 2013; Kelble et al., 2013; Oosterbroek et al., 2016; Palinkas, 2012; Patterson et al., 2010; Reis et al., 2015; Sandifer and Sutton‐Grier, 2014; Smith et al., 2013; Summers et al., 2014, 2016; Yee et al., 2012]. Many of these models are derived from the general Driver‐Pressure‐State‐Impact‐Response (DPSIR) ecological model that has been used for decades and was adopted by the United Nations Commission on Sustainable Development [Organisation for Economic Co‐operation and Development, 1993].
One widely adopted model is the Driving force‐Pressure‐State‐Exposure‐Effect (DPSEEA) framework proposed by Corvalan et al. [1996] and Briggs [1999]. This model describes health impacts as being influenced by driving forces (e.g., population growth and economic development) that lead to pressures on the environment (e.g., harvesting, mining, and waste release) that result in changes in the state of the environment (e.g., increases in pollution and increased risk from natural hazards). It requires an assessment of the exposure to these pressures (e.g., external exposure and absorbed dose) that lead to potential health effects (e.g., morbidity and mortality). Hambling et al. [2011] rated this model as best of those reviewed for application to develop environmental health indicators for the effects of climate change on health. However, the DPSEEA model does not assess the impact of natural or technological disasters on the health and functioning of ecosystem services and thus makes no connection between ecosystem services and human health. In addition, the authors noted DPSEEA may have limitations for use with regard to disaster impacts. Reis et al. [2015] improved the DPSEEA model by offering an ecosystems‐enriched or eDPSEEA construct. While the model is general in its presentation, it allows for inclusion of complex considerations and connections, although these are not elaborated in the framework diagram. This model was discussed in a workshop format at a scientific meeting where its utility in helping to identify a wide range of implications, including some related to loss of specific ecosystem services, was demonstrated.
Health impact assessment (HIA) is useful for evaluating the potential health impacts of future activities that will affect the environment. An HIA is “a combination of procedures, methods, and tools by which a policy, program, or project may be judged as to its potential effects on the health of a population, and the distribution of those effects within the population” [Gothenburg Consensus Paper, 1999]. A major advantage of the HIA process is that it brings public health issues to the attention of decision makers around topics and decisions that fall outside of traditional public health arenas, such as transportation or land use [Kemm, 2001]. In the U. S., HIAs may be considered analogous to environmental assessments (EAs), which are required under the National Environmental Policy Act and which assess the impacts of activities on environmental outcomes such as air and water quality. One difference is that HIAs can be voluntary, whereas EAs are required for federally funded projects. Typically, HIAs have not included ecosystem services per se. However, Horwitz and Finlayson [2011] have shown how the HIA approach could be used to demonstrate the human health values of maintaining healthy wetlands, and the U.S. Environmental Protection Agency has developed an approach to bringing ecosystem services into HIA via its geospatially enabled EnviroAtlas [U.S. Environmental Protection Agency [USEPA], 2015].
We are not aware of previous models that have connected natural or technological disasters to stress‐associated physiological and psychological health outcomes that result from loss of ecosystem services. Although it may not be appropriate or useful in all cases, an ecosystem service framework that lays out the connections between ecosystems and human health is relevant to planning for, and responding to, natural and technological disasters, especially for coastal communities that are heavily dependent on natural resources.
The societal costs of not having a conceptual model for how disasters impact the mental and physical health of nearby residents is that the public dramatically underestimates disaster effects on human health and well‐being, local economies, and the resources necessary to effectively prepare for and respond to disasters. This paper begins to fill that gap. We provide one of the first conceptual frameworks that include disaster impacts on environmental conditions and ecosystem services and how impacts to ecosystem services have subsequent negative effects on human physiological, psychological, and community health and well‐being. This conceptual model can be used to enhance both predisaster preparation and postdisaster responses by improving our understanding of the full suite of impacts that disasters cause and the wide range of human health outcomes for which we should prepare and be ready to respond.
2. Materials and Methods
This was a conceptual modeling study and thought experiment. We used the broad definitions of human health and well‐being developed by the World Health Organization [World Health Organization, 1946] and utilized extensively elsewhere [e.g., MEA, 2005; Sandifer et al., 2015] and assessed relevant models of environmental and human health effects of disasters via a broad ranging but targeted literature review. This was followed by an iterative design process among the project team which included information from the literature, original ideas, and in‐depth discussions with a wide range of experts individually and in two focused workshops.
In addition to conceptual model development, we conducted an extensive data mining initiative that focused on available ecosystem pressure, ecosystem state, ecosystem services, human health, and community characteristics data for the Gulf of Mexico and the affected coastal counties of Texas, Louisiana, Mississippi, Alabama, and Florida. Initial data mining efforts by the investigators identified numerous portals providing access to data related to environmental conditions in the Gulf of Mexico prior to and following the DWH incident. Following this assessment of available data sets, we assembled in workshop format a broad mix of carefully selected experts in biomedical (e.g., stress biomarkers, other indicators of mental and physical health, and human microbiome), clinical (involved in assessing and treating disaster victims), and ecological (ecosystem services, ecosystem processes, and biodiversity) sciences, as well as health scientists and ecologists with recent experience in or related to the Gulf of Mexico. The primary purposes of the workshop were to (1) review the available data in the context of our conceptual modeling approach, (2) identify existing data sets that likely could be used to assess health effects of disasters, and (3) conduct a preliminary case study of our model within the context of available data and literature. Results from the data mining activities and the workshop will be reported separately.
Although we found a number of useful frameworks during our literature review, none connected disasters to health effects through impacts to ecosystem services. Therefore, we adopted and modified concepts from several existing frameworks and incorporated them into a more comprehensive and novel model that explicitly identifies and emphasizes the human health consequences that are due to the disaster's effects on the environmental benefits on which people and communities depend.
We chose the model of Kelble et al. [2013], augmented with information from Yee et al. [2012], Bradley and Yee [2015], and other sources as the basis for the environmental‐ecosystem service components of our framework. Foundation blocks for the human health and well‐being elements of our model were the mental health impacts diagram of Palinkas [2012, 2015], the Eco‐Health DPSIR model of Bradley and Yee [2015], and the allostatic load (AL)‐chronic stress model of McEwen and Stellar [1993] and McEwen [1998a, 1998b, 2000]. The literature review was accompanied by two workshops that garnered a wealth of expert opinion from scientists representing diverse disciplines. Similar interdisciplinary expert workshops have produced highly useful results [e.g., see Bradley and Yee, 2015; Foley et al., 2010; Halpern et al., 2012; Kelble et al., 2013; Lovelace et al., 2012; Reis et al., 2015].
The origin of the Kelble et al. [2013] framework is the general DPSIR model that has been used widely in ecology for decades and more recently to explore some aspects of human health and well‐being [Bradley and Yee, 2015; Sekovski et al., 2012; Yee et al., 2012]. The DPSIR model illustrates how certain events or changes (termed “drivers”) exert specific kinds of “pressures” on the condition or “state” of ecosystem components, resulting in impacts to the ecosystem and responses (human actions taken as a result of the impacts). Kelble et al. [2013] modified the DPSIR framework to support ecosystem management approaches to environmental decision‐making. They removed impacts per se and replaced them with ecosystem services and allowed for identification of positive as well as negative effects of stressors. Ecosystem services are shown at the top of their model to emphasize priority. Disasters were not explicitly included among the drivers at the base of this model, and human health is incorporated only as one among many ecosystem services.
Kelble et al. [2013] named their framework the EBM‐DPSER (Ecosystem Based Management‐Driver‐Pressure‐State‐Ecosystem Service‐Response) model because of its focus on supporting ecosystem‐based management decision processes. They presented a more detailed version of the EBM‐DPSER model as a submodel for the South Florida water column.
We made significant changes in these modified DPSIR frameworks to reflect our three‐way focus on disasters as drivers, effects on ecosystem services as avenues through which some environmental consequences of disasters are transmitted to people, and stress‐related human health outcomes as the ultimate focus.
Based primarily on work with the Exxon Valdez oil spill, Palinkas [2012] separated mental health impacts derived from oil spills into three “tiers”: environmental effects (including direct health impacts), community effects (essentially erosion of positive community characteristics that provide support for people), and intrapersonal effects that include a variety of psychological and physiological outcomes. These tiers are interconnected and mediated by the relative risk, vulnerability, and resilience characteristics of individuals and communities. We augmented this framework with additional information gleaned from recent literature particularly relevant to the Gulf of Mexico, hurricanes or oil spills, or to ecosystem service connections to human health and well‐being as well as information garnered from our two expert workshops.
Finally, we included psychological and physiological stress as our primary focus for long‐term health effects because cumulative stress is associated with many chronic illnesses and related mortality among humans, including a variety of both mental (e.g., depression, anxiety, and posttraumatic stress disorder/posttraumatic stress symptoms (PTSD/PTSS)) and physiological (e.g., cardiovascular disease) disorders [Juster et al., 2010; Schneiderman et al., 2005; Segerstrom and Miller, 2004; Thoits, 2010]. Because it is linked with such a broad range of health effects, chronic stress is commonly associated with health problems following traumas of many types, including disasters [Galea et al., 2005; L. S. King et al., 2015; Mills et al., 2007; Neria et al., 2007]. However, chronic stress is generally not well measured via surveys frequently used to assess health status.
Through our literature review and discussions with health researchers, we identified allostatic load (AL) as a powerful concept for understanding impacts of chronic stress on human health [McEwen and Stellar, 1993]. The term “allostasis” refers to physiological processes that “maintain stability through change” [Sterling and Eyer, 1988] and refers to how organisms adapt to acute stress through the production of stress hormones which act to restore homeostasis. AL is defined as the cumulative “wear and tear” on the human body that increases over time with exposure to repeated or chronic stress and recovery cycles [McEwen and Stellar, 1993; McEwen, 1998a, 1998b, 2000]. AL represents both the physiological and psychological consequences of chronic exposure to interconnected biological responses to stress, with diminishing opportunity for reset to a “normal” physiological state [Bizik et al., 2013; Juster et al., 2010, 2016; Logan and Barksdale, 2008; McEwen, 1998a, 1998b, 2000; McEwen and Gianaros, 2010; Picard et al., 2014]. Inclusion of AL considerably strengthened our model by providing a specific mechanistic connection between disasters, increasing and cumulative stress, and myriad negative health outcomes.
AL measures the dysregulation of the nonlinear network of multiple physiological systems, and prolonged dysregulation can increase the susceptibility of an individual to stress‐related disease [Berger et al., 2015; Bizik et al., 2013; Juster et al., 2010, 2011a; McEwen, 1998a, 1998b, 2000]. The severity of AL following a specific event depends on an individual's preexisting AL and a variety of factors that may modify stress effects, such as a person's experiences, environment, genetics, behavior, and relative vulnerability or resilience [Juster et al., 2016]. Overall, the higher the AL, the greater the probability that an individual's health will be negatively impacted. To date, >100 studies have measured AL in order to predict stress‐related diseases. Examples of specific health outcomes correlated with or predicted by AL include cardiovascular disease, physical decline, cognitive declines, and all‐cause mortality among successful agers [Gruenewald et al., 2006; Karlamangla et al., 2002; Seeman et al., 2001, 2004], PTSD in women [Glover et al., 2006], chronic fatigue syndrome [Maloney et al., 2006], mortality among Taiwanese [Goldman et al., 2006] and poor Americans [Crimmins et al., 2007], Type 2 diabetes among American Samoans [Crews, 2007], ischemic heart disease among Americans [Sabbah et al., 2008], and 3 year depressive symptoms among Canadian older adults [Juster et al., 2011b].
AL is typically assessed via biomarkers, which include a variety of endocrine, immunological, metabolic, cardiovascular, respiratory, and anthropometric measures [Juster et al., 2010]. Some of the more readily obtainable include cortisol (from saliva, urine, or hair samples), cholesterol and its lipid components, blood pressure, pulse rate, and body mass index. Cortisol levels can be particularly useful but must be measured multiple times within the same individual because of differences related to diurnal cycles and other natural variation. Biomarker data can be combined via one or several indices [Juster et al., 2010] to provide qualitative and quantitative assessments of AL in individuals or groups. The most commonly employed and potentially useful algorithm for purposes such as the present model is the group AL index which is a “[s]ummary measure representing the number of biomarkers falling within a high risk percentile (i.e., upper or lower 25th percentile based on the sample's distribution of biomarker values” [Juster et al., 2010]. A different and innovative approach that is predictive of AL in youth involves calculating cumulative risk scores from factors such as separation/turmoil, violence, socioeconomic status, single parent, and maternal high school dropout [Evans, 2003; Evans et al., 2007]. One or more AL indices and/or the cumulative risk scores can be included in our model to assess AL of the target population. Overall, AL's holistic approach to combining subclinical thresholds for a number of biomarkers allows for a broader biometric approach to assessing the physiological manifestations related to chronic stress and unhealthy behaviors. Its application in the present context is novel.
3. Results
We developed a Disaster‐Pressure‐State‐Ecosystem Service‐Response‐Health (DPSERH) model that includes both environmental and human health outcomes (Figure 1). The “health” component of this model is the most significant and novel piece that our model adds in connecting disasters to environmental impacts and then to subsequent human health and well‐being effects. In this framework, disasters are the drivers of the changes that cascade through the ecosystem and ultimately end up causing or contributing to human health effects. Pressures are the immediate physical, chemical, and biological effects of disasters that cause changes in the ecosystem. State refers to the condition of the physical, chemical, and biological attributes of the ecosystem that contribute to production, quality, or delivery of ecosystem services. These conditions can be measured objectively and are often changed through pressures exerted by disasters. Ecosystem services are the benefits that people derive from nature and that make human life on Earth possible [Cairns and Pratt, 1995; Daily, 1997; MEA, 2005; Rapport et al., 1998; Yoskowitz et al., 2010, 2016]. These definitions are in accordance with recent standardization recommendations of Oesterwind et al. [2016] for consistent usage. They define driver as “superior complex phenomena governing the direction of the ecosystem change, which could be both of human and nature origin”; pressure as “a result of a driver‐initiated mechanism (human activity/natural process) causing an effect on any part of an ecosystem that may alter the environmental state”; state as “the actual condition of the ecosystem and its components established in a certain area at a specific time frame, that can be quantitatively‐qualitatively described based on physical (e.g., temperature, light), biological (e.g., genetic‐, species‐, community‐, and habitat‐ levels), and chemical (e.g., nitrogen level and atmospheric gas concentration) characteristics”; and impacts as “consequences of environmental state change in terms of substantial environmental and/or socioeconomic effects which can be both, positive or negative.” They also defined response as “all management actions seeking to reduce or prevent an unwanted change or to develop a positive (desirable) change in the ecosystem.” While we include management actions in responses in our model, we followed Kelble et al. [2013] and Bradley and Yee [2015] in using a broader definition, that is, the range of human reactions to disasters. These reactions can have negative and positive consequences and can include anything from first‐responder emergency efforts to long‐term changes in policy and preparedness, how formal and informal institutions and leaders perform and communities respond, media coverage, and how people react to media reports and institutional actions.
Figure 1.
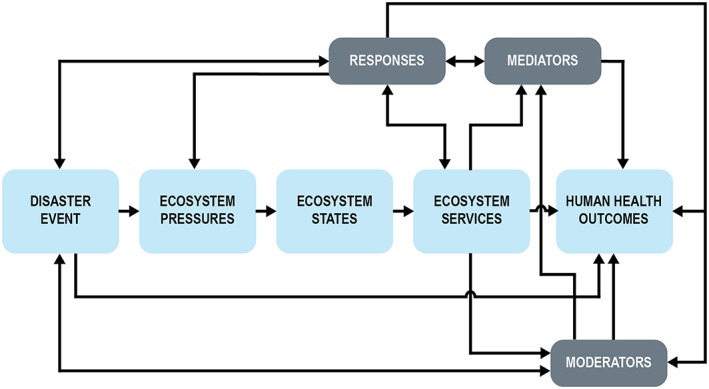
General schema for the overall DPSERH model.
This basic schema (Figure 1) illustrates how disasters create environmental pressures on the state or condition (e.g., contamination) of ecosystem components (e.g., fish stocks), resulting in degradation of ecosystem services (e.g., reduced water quality and loss of fishery harvest and associated income), which in turn produces acute and chronic stress (e.g., through anticipated or realized loss of income and family disruption) that then results in negative health outcomes for individuals, groups, and communities. Moreover, responses taken to mitigate risks after a disaster may affect the flow of ecosystem services, thereby increasing or decreasing stress through lost or improved opportunities to benefit from ecosystem services. Disasters may also have short‐term and chronic effects on health outcomes via traumatic injury and exposure to infectious disease and toxic substances as indicated by a direct arrow from disasters to health. Roles of mediators, moderators, and responses are detailed below.
For the present case, we chose two kinds of disasters, major hurricanes and large oil spills, due to our project's focus on the Gulf of Mexico (Figure 2). However, this model would work equally well for assessing human health effects of loss of ecosystem services caused by other natural and technological disasters, such as extreme weather events, chemical spills, industrial accidents, tsunamis, earthquakes, major harmful algae blooms, and even some terrorism incidents where there is significant environmental damage.
Figure 2.
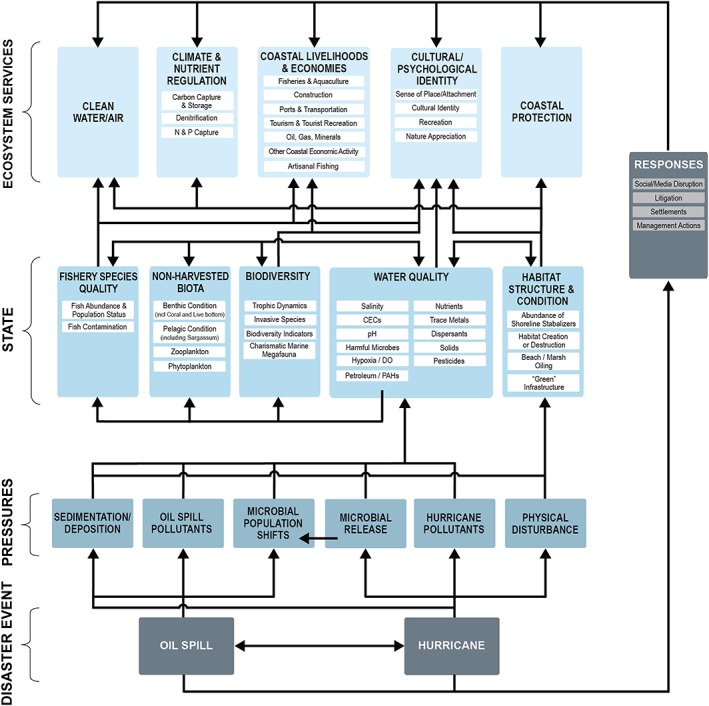
The detailed environmental/ecosystem services module of the DPSERH model.
The pressures we include represent major effects of both hurricanes and oil spills, including physical disturbance and destruction, changes in sedimentation and deposition (increases, decreases, resuspension, redistribution, and accumulation of oil), chemical and other pollution, and changes in microbial community composition and function. Depending on the type of disaster and its proximal effects, other pressures could be added or one or more of these removed, similar to the way Kelble et al. [2013] and Cook et al. [2014] have done in their submodels. However, based on the literature for hurricanes and oil spills, we considered these pressures among the most important [Joye, 2015; Sheikh, 2005; USEPA, 2007].
For simplicity, we grouped ecosystem states into five large categories of ecosystem attributes: water quality, habitat structure and function, biodiversity, nonharvested biota, and fishery (harvested) species. Each of these major component groups is further subdivided into subgroups, which in turn can be subdivided more and more finely as needed for a particular exercise. Fishery states represent all harvested living resources including, but not limited to, finfish, shellfish, and crustaceans. These state groups and subgroups all represent major ecosystem components and attributes that are known to be influenced by hurricanes and oil spills [Barron, 2012; Incardona et al., 2014; Joye, 2015; G. M. King et al., 2015; Kostka et al., 2011; Lee et al., 2015; Mendelssohn et al., 2012; Sheikh, 2005; USEPA, 2007; Venn‐Watson et al., 2015].
While there are many ecosystem services that people derive from the Gulf of Mexico [e.g., Farber et al., 2006; Yoskowitz et al., 2010, 2016], we chose five broad groups of ecosystem services that are known to be particularly important in the gulf: these are clean water and air, climate and nutrient regulation, coastal livelihoods and economies, coastal protection, and cultural/psychological identity. Other ecosystem services could be substituted in the model as needed for a particular scenario. Most of the ecosystem service groups included here are also subdivided into smaller (but still large) component services, and as we point out below, we used a subset of particularly important ecosystem services in the overall model. Arrows, each of which is supported by literature or data, indicate connections between drivers and specific pressures, states, ecosystem services, responses, and eventually human health outcomes. While efforts continue to define individual and cascading connections among the myriad components of the socioecological system in the gulf, it is neither feasible nor practical to include every known interaction. Rather, these connections were selected to represent some of the most well‐documented and pertinent relationships in the study area.
The human health component of our model (Figure 3) includes physiological and psychological health outcomes such as physical illnesses (e.g., cardiovascular disease) and psychological disorders (depression and PTSS), in addition to cognitive and behavioral outcomes and a variety of community environment variables such as community health and security, community attachment, social capital, and community resilience. We also incorporated risk perception, which can be affected by previous disaster experience and social and community factors and can substantially influence actions people take and their levels of anxiety and stress [Eisenham et al., 2007; Levine and Picou, 2012; Slovic and Peters, 2006; Wachinger et al., 2013].
Figure 3.
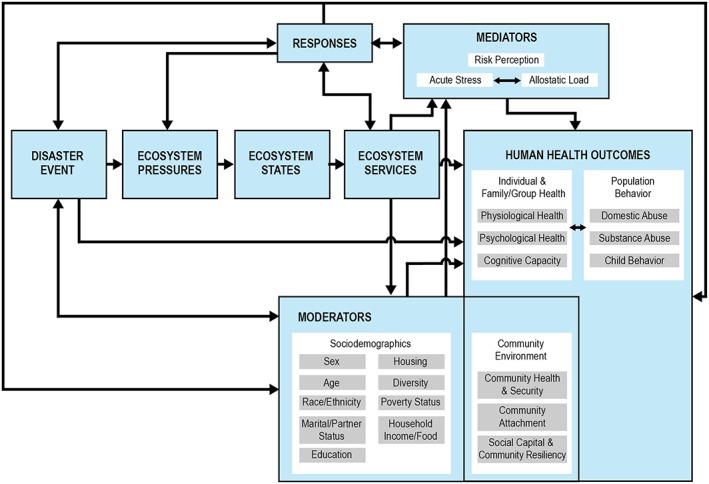
The DPSERH model schema with elaboration of the human health module.
The health module also includes moderators and mediators [Baron and Kenny, 1986]. A moderator is a qualitative or quantitative factor that specifies when or to whom something may happen, while a mediator is a mechanism by which effects occur. Moderators can be considered as predisposing conditions and may include a range of socioeconomic variables such as sex, age, race/ethnicity, diversity, marital status, educational level, housing, poverty status, and income and food availability. The importance of each of these in moderating the health effects caused by disasters is well established [Noji, 1997]. Community variables also can be moderating factors in some situations or they can be health and well‐being outcomes, or both, in a given situation. This duality is illustrated by having the Community Environment measures encompassed in both the Human Health Outcomes and Moderators boxes.
Mediators can include a variety of mechanisms of action. We used acute stress and AL as the primary mediators since we are specifically targeting human health effects associated with stress caused by disasters, although risk perception may also serve a mediating role. As noted previously, we indicate direct effects of disasters, such as traumatic injury, toxicity, or exposure to infectious disease, with an arrow connecting the disaster directly to health outcomes. People's responses in reaction to a disaster and its effects may be positive, negative, or neutral in terms of health effects. Adverse or damaging responses that may increase AL and exacerbate mental and physical distress include negative media reports, litigation, or systematic failure of leaders and social institutions to cope or inspire confidence and trust [Freudenberg, 1997; Juster et al., 2011a; Palinkas, 2012; Vasterman et al., 2005; Weems et al., 2012; Xu et al., 2016]. Positive responses that may ameliorate stress include effective predisaster planning, warnings, and recovery actions, improved building construction requirements, disaster‐focused training and capacity building among public health workers, an emphasis on coastal resilience, and strong community organizations [Adger et al., 2005; Miller et al., 2016; Norris et al., 2008; Qureshi et al., 2004; Shultz et al., 2005].
The entire detailed model is illustrated in Figure 4. We chose to emphasize the following ecosystem services based on literature and expert opinion concerning their linkages to human health and well‐being in the Gulf: commercial fishing and aquaculture, artisanal or subsistence fishing, tourism (including tourist‐associated recreation), nontourist recreation (e.g., the recreational activities local people take part in that help renew and restore their feelings of well‐being), coastal protection, sense of place, and clean water and air. We also included climate and nutrient regulation to represent their importance as ecosystem services, since they may exert additional pressures concurrent with those associated with disasters. However, their effects are likely to take place over much larger temporal and spatial scales that are harder to define than the others. While our choices of ecosystem services were made independently, it is noteworthy that a broad range of Gulf ocean users ranked food (e.g., fisheries), raw materials (including hydrocarbons), and recreation as the top three ecosystem services in a recent relative valuation exercise [Yoskowitz et al., 2016].
Figure 4.
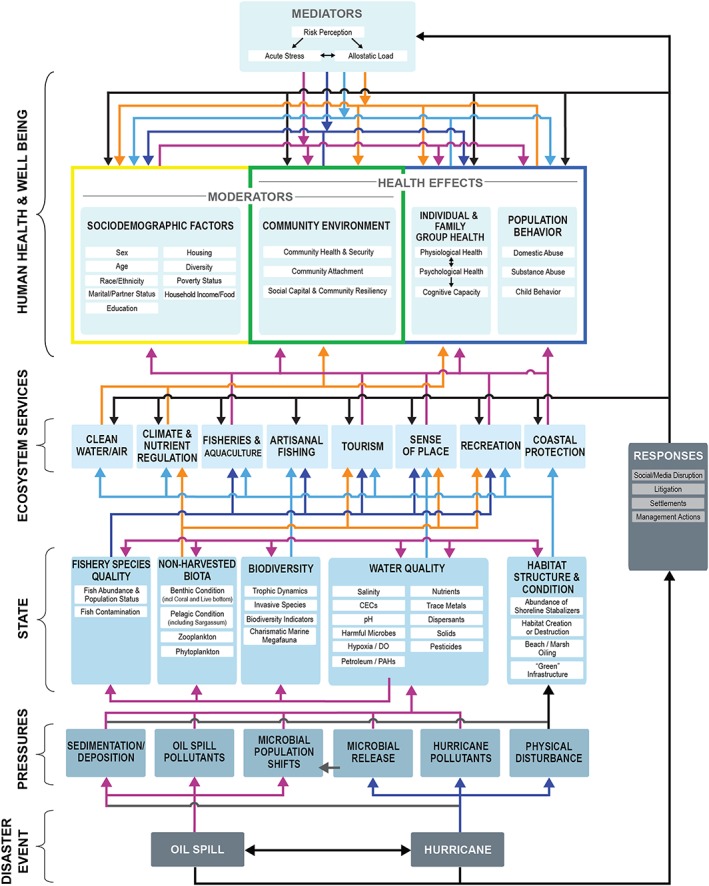
The overall DPSERH model, showing connections among various components. These connections are not meant to be all inclusive but rather illustrative. All arrows shown are based on existing literature or data. Different colors used for arrows have no significance other than to increase ease of following specific connections among model elements.
3.1. Case Study: DWH Disaster, Human Health Impacts of Fishery Closures
Using this new conceptual model, one can trace the potential for stress‐related health effects from a disaster through impacts on one or multiple ecosystem services and then on to specific individual, group, and community health outcomes (Figure 4). Here we apply our new DPSERH model to briefly examine both environmental and human health/well‐being effects of pollution from the DWH oil catastrophe and subsequent management and other responses. The spill resulted in substantial impacts to water and air quality through contamination by crude oil and its components, dispersants, and compounds formed as a result of burning of surface oil and flaring of natural gas, among other things. These pollutants entered the Gulf of Mexico food web, with resulting major concerns about potential for accumulation of contaminants in seafood at sufficiently high levels to cause health problems for other animals consuming them, including humans and marine mammals [Wilson et al., 2015; Ylitalo et al., 2012]. Even months and years after the incident, when the weight of scientific evidence clearly demonstrated that there were no significant levels of oil‐ and dispersant‐related contaminants in commercially or recreationally harvested seafood, there remained widespread distrust and concern among the public, including seafood harvesters and purveyors [McKendree et al., 2013; Morgan et al., 2016; Sandifer et al., 2012]. Both the immediate and longer‐term concerns were widely reported in the media, further raising levels of public anxiety. The near‐term effect was the action by the NOAA to close all federal waters of the Gulf to fishing where oil had been sighted or was expected to be found. Following the first fishery closure on 2 May 2010, the area of closure expanded to a peak of ~229,215 sq km (37%) of gulf federal waters by 2 June. After that point, waters that met all test criteria were systematically reopened, with one third of the total closure reopened on 22 July 2010 and all but 0.4% of Gulf federal waters reopened to fishing by 15 November. The final federal fisheries area was reopened 1 day before the first anniversary of the DWH explosion, 19 April 2011 [Lubchenco et al., 2012; Ylitalo et al., 2012].
The closures resulted in the complete loss of fishery ecosystem services in these areas during the periods that they were closed, including commercial, recreational, and tourist‐related fishing, even though there were relatively little observed impacts, especially from contamination, to the underlying resources. In addition, the specter of oil‐coated marshes, beaches, and wildlife caused major disruptions in tourism. The loss of fishery and tourism ecosystem services—compounded by heavy media coverage, growing uncertainty over the magnitude and duration of the spill and the related moratorium on new oil and gas activities, differences of opinion within the engaged scientific community, and a host of sociodemographic and community factors—caused high levels of anxiety, depression, and other indicators of increased stress among people who were dependent on fisheries and tourism for income, food, and a treasured way of life (Table 1) [Levine and Picou, 2012; Shenesey and Langhinrichsen‐Rohling, 2015; Shultz et al., 2015], and also among oil and gas industry workers and their families, as well as the oil spill cleanup workers [Kwok et al., 2017]. Using existing information from the literature (Table 1) and available data sets, we can trace the path of the disaster's effects beginning with the DWH catastrophe through impacts to water quality and then on to concerns for seafood safety, the loss of fishery and tourism ecosystem services through fishery closures, the consequent loss of livelihoods, food and treasured ways of life, the accumulation of stress in individuals and communities caused by the loss of ecosystem services, and the manifestation of the accumulated stress (AL) in mental and physical disorders and social disruption.
Table 1.
Examples of Health Effects of Hurricane Katrina and the Deepwater Horizon Oil Catastrophe
| Health Effects | Catastrophe (Hurricane/Oil Spill) | Reference |
|---|---|---|
| Elevated anxiety mood disorder and PTSD in New Orleans residents across broad sociodemographic range after hurricane | Katrina |
Galea et al. [2007] |
| Persistent PTSS, especially among the disadvantaged | Katrina |
Paxson et al. [2012] |
| Persistent depression and stress, especially among females, African Americans, less educated, and those affected by separation and severe home and financial damage | Katrina |
Picou and Hudson [2010] |
| Threefold increase in hospital admissions for myocardial infarctions during 6 years after event | Katrina |
Peters et al. [2014] |
| Increased blood pressure, headaches, stomach and respiratory problems, irregular heartbeat; depression and PTSS; especially among females, African Americans, poor, and lacking strong social connections | Katrina | |
| Increased interpersonal violence | Katrina |
Schumacher et al. [2010] |
| High levels of PTSS in children | Katrina |
Jaycox et al. [2010] |
| 2.7 times higher than national incidence for severe emotional distress in children | Katrina |
McLaughlin et al. [2010] |
| >50% of children still reported mental distress 2 years after event | Katrina |
Abramson et al. [2008] |
| Nearly 30% of pediatric patients presented with mental health problems 3 years after event | Katrina |
Olteanu et al. [2011] |
| High levels of tension, anxiety, depression, fatigue, confusion, and less able to cope related to loss of income | DWH |
Grattan et al. [2011] |
| High psychological stress related to economic and health concerns | DWH | |
| Increased and persistent anxiety, depression, and PTSS especially among those previously affected by Katrina | DWH/Katrina |
Osofsky et al. [2011] |
| Stress effects most associated with low income and low social support | DWH |
Laffon et al. [2016] |
| Negative mental and physical health effects were greater in fishing households, among coastal residents, Cajuns, lower socioeconomic status, and less among those with stronger community attachments; effects declined over time | DWH |
Cope et al. [2013] |
| Spill‐related income loss was strong driver of mental health problems, including those related to corrosive community issues and media reporting | DWH |
Morris et al. [2013] |
| High levels of stress, anxiety, depression, and behavioral problems among Vietnamese American fishers especially about economic concerns | DWH |
Ngo et al. [2014] |
| PTSD in children in affected LA parishes; most pronounced for those with previous hurricane exposure and some other personal factors; mental and physical effects connected | DWH |
J. D. Osofsky et al. [2014], and H. J. Osofsky et al. [2014] |
| Nearly 50% of participants affected by DWH; high percentages concerned about wildlife, seafood safety, loss of way of life, and reduced job opportunities; high levels of depression, anxiety, and PTSS | DWH |
H. J. Osofsky et al. [2014] |
| Drug, marijuana, and alcohol use increased among those >12 and young adults experienced depression and increased thoughts of suicide | DWH |
Gould et al. [2015] |
| Negative health indicators of physical and mental distress and depression, with women and children most susceptible; related to loss of income, jobs | DWH |
Fan et al. [2015] |
| Stress, PTSS, anxiety, and serious mental illness in LA coastal residents still high after 2 years; mostly related to disruption of lives, work, family and social engagement | DWH |
Hansel et al. [2015] |
| Children and adolescents highly vulnerable to trauma; cumulative risk of mental health problems increases with multiple traumatic events | DWH |
L. S. King et al. [2015] |
| Economic impact related to increased depression and PTSD symptoms, somewhat alleviated by individual resiliency | DWH |
Shenesey and Langhinrichsen‐Rohling [2015] |
| At large geographic scale, no severe and persistent behavioral effects | DWH |
Shultz et al. [2015] |
| Fishers reported elevated concerns about economic and financial impacts, health, and threat to cultural heritage | DWH |
Cherry et al. [2015] |
| Among oil spill cleanup workers, having prespill mental health concerns associated with postspill counseling and medication | DWH |
Lowe et al. [2015] |
| Study included >2000 women. Physical exposure to spill associated with burning and soreness of nose, throat, and lungs, dizziness, and wheezing; economic exposure associated with wheezing, headaches, stuffy/running nose | DWH |
Peres et al. [2016] |
| Women exposed both economically and physically to the oil spill experienced increased depressive symptoms and domestic violence while physical exposure alone was related to mental distress. | DWH |
Rung et al. [2016] |
4. Discussion
To a significant extent, human health and well‐being depend upon the condition of the environments in which we live and the goods and services they provide. This relationship has been explored in detail in the Millennium Ecosystem Assessments [MEA, 2005] and more recently by the National Academy of Sciences specifically for the Gulf of Mexico [National Academy of Sciences, 2013]. The concept of ecosystem services is explicitly human centric, and human health and well‐being can be considered the cumulative or ultimate ecosystem service [Sandifer and Sutton‐Grier, 2014]. Degraded environments which can no longer produce or deliver high‐quality ecosystem services may have a variety of negative ramifications for human health and well‐being, including poor nutrition and starvation, inadequate shelter, increased incidences of infectious diseases, loss of livelihood and cultural identity, diminished availability of potable water, reduced opportunities for recreation and relaxation, and reduction in climate modulation and nutrient regulation [MEA, 2005; Sandifer and Sutton‐Grier, 2014].
Environmental disasters substantially affect the well‐being of hundreds of millions of people annually [Learning and Guha‐Sapir, 2013]. Yet despite substantial efforts to increase understanding of linkages between ecosystem health and human health via ecosystem services, the pathways and mechanisms through which disasters damage ecosystems and then how those ecological injuries are translated into long‐term and widespread negative effects on human health for the most part are poorly understood. The novel conceptual model presented here is, to our knowledge, the first attempt to elucidate how disaster‐impacted ecosystem services feed into psychological and physiological mechanisms that are associated with specific health problems in humans. Additionally, the model makes possible exploration of health effects of one degraded ecosystem service at a time or simultaneous consideration of several affected ecosystem services. This is important because in the Gulf of Mexico and elsewhere crucially important ecosystem services such as commercial and recreational fisheries, tourism, and cultural identity/sense of place are strongly interlinked, and concerns related to the relative condition of these services may persist long after disaster events.
The model also allows for assessment of interactive effects (synergistic, antagonistic, or additive) of two or more disasters that may affect one another (e.g., hurricane impacts on a recent or ongoing oil spill) and may affect both the environment and human health and well‐being. For example, hurricanes may cause oil spills (there were >130 oil spills associated with Hurricane Katrina [Sever, 2006]) or exacerbate recent or ongoing spills. Additionally, the stress produced by Katrina was a major factor affecting many people who 5 years later were impacted by the DWH catastrophe [H. J. Osofsky et al., 2011, 2014]. Incorporation of AL in the model provides the opportunity to evaluate cumulative stress effects from multiple disaster events and environmental cascades, providing a needed common health and well‐being indicator that transcends disasters and other life changing events.
Development of this model is particularly important for the Gulf of Mexico, a Large Marine Ecosystem with a well‐documented history of major environmental disasters and impacts. The Gulf has been affected by massive modifications to support the offshore oil industry: ongoing subsidence and loss of wetlands associated with flood control, navigation improvements, and sea level rise; annual hypoxic “dead zones” caused principally by anthropogenic eutrophication; invasive species; repeated effects of major storms such as Hurricanes Katrina and Rita; and ongoing oil pollution from both natural seeps and small to massive accidents including the 1979 Ixtoc and more recent DWH catastrophes [Committee on Environment and Natural Resources, 2010; Gulf Coast Restoration Task Force, 2011; Gundlach et al., 1981; McCallum and Heming, 2006; Mississippi River Gulf of Mexico Nutrient Task Force, 2013; Natural Resources Defense Council, 2015; U.S. Fish and Wildlife Service, 2013]. Similarly, most coastal areas in the U.S. and around the world are impacted by multiple stressors, often acting simultaneously and synergistically [Sandifer and Sutton‐Grier, 2014], and this model should be useful for assessing disaster threats and impacts to coastal ecosystems and communities globally.
The DWH catastrophe resulted in the largest marine oil spill in the U.S. and one of the largest ever globally [McNutt et al., 2012]. Environmental impacts of the DWH disaster are being investigated in great detail [Lubchenco et al., 2012], with hundreds of scientific papers reporting effects of the oil, dispersants, and cleanup efforts on the Gulf ecosystem and its component habitats and organisms, from the coast to deep water and including vulnerable species such as sea birds, sea turtles, and marine mammals (e.g., see Beyer et al. [2016] and programs and reports from Deepwater Horizon research workshops held in 2010–2012 and of the Gulf of Mexico Oil Spill and Ecosystem Science Conferences for 2013–2016).
Even though long‐term human health effects of oil spills have received less attention and research funding than the environmental damages, the literature dealing with mental and physical health impacts is growing rapidly [e.g., Aguilera et al., 2010; Kwok et al., 2017; Laffon et al., 2016; Peres et al., 2016; Rung et al., 2016] (Table 1). What is often not recognized is that the two impacts, to ecosystems and human health, are often directly related [H. J. Osofsky et al., 2014]. Even though some previous studies have relied on volunteered, self‐reported health status, behaviors, and risk factors that are subject to bias [McCoy and Salerno, 2010], the overall weight of evidence concerning health impacts is substantial. Even though there remains a comparative paucity of information on effects on physical health, some physical and mental health outcomes are now being assessed in long‐term, cohort‐based studies [Kwok et al., 2017; Peres et al., 2016; Rung et al., 2016].
Available literature demonstrates that disaster‐related impacts to ecosystem services result in significant, long‐lasting, and debilitating stress‐related health effects among human survivors (Table 1). This is particularly true for those ecosystem services that affect (1) jobs, income, and way of life (e.g., natural resource‐based employment such as fishing, many kinds of tourism, and oil and gas extraction); (2) individual, family, and community health (e.g., water and air quality, food safety and supply, housing, and community security); and (3) sense of identity and social connection (e.g., local recreation and sense of place and community). It is also clear that stress is a common and dominant risk factor for long‐term human health effects of disasters in the Gulf of Mexico and in other settings and that cumulative stress may lead to a wide range of negative health effects [Atwoli et al., 2016; Mathur et al., 2016]. Similar to findings about Hurricane Katrina and the DWH catastrophe, stress effects are still observed multiple years after the 2011 Indonesian tsunami and the Fukushima tsunami and nuclear reactor accident, including significant impacts of economic losses, family disruption, concerns about compensation, and social disturbance [Irwantol and Zulfa, 2015; Tsujiuchi, 2015]. Albrecht [2005] coined the word “solastalgia” to encompass the feelings of distress and other mental health effects associated with loss of identity and damage to or loss of home, treasured places, and way of life. Warsini et al. [2014] were apparently the first to use the term to describe the mental anguish, depression, PTSS, and other psychological issues that people may experience following losses of home, livelihood, and other environmental damage due to natural disasters. Some of the impacts of both natural and technological disasters reviewed here also could be classified as solastalgia.
Certain human populations are more vulnerable to effects of disasters and disaster‐associated stress, such as those who have experienced previous trauma (e.g., exposure to Hurricane Katrina in 2005 followed by the DWH in 2010), women, children, the elderly, minorities and those who are economically or socially disadvantaged (Table 1). In addition, recent research on dolphins in areas affected by the DWH oil catastrophe clearly showed negative physiological effects, particularly to adrenal glands (which are involved in stress responses) and lungs [Schwacke et al., 2014; Venn‐Watson et al., 2015; Smith et al., 2017], suggesting that such physiological impacts could occur in exposed people as well. All of this information supports our focus on chronic psychological and physiological stress as a valuable indicator of negative human health outcomes and the use of AL as a mediator of stress pathophysiology.
In contrast to other available frameworks, the DPSERH model presented here deals specifically and in detail with disasters and health impacts related to degradation of ecosystem services. Overall, DPSERH offers a number of important benefits not explicitly incorporated in other frameworks related to disasters.
It elaborates environmental and health connections, includes sociodemographic and community moderators, and identifies potential physiological mechanisms that may result in a variety of stress‐associated negative health outcomes. If supplemented with appropriate environmental, psychological, and physiological data and information from biomarkers and other indicators, DPSERH could be employed to identify specific disaster impacts to one or more critical ecosystem services, possibly measure the associated ALs in affected populations, and assess apparent linkages between increased acute and chronic stress and specific behavioral and physical human health outcomes.
The DPSERH model can help policy makers identify which populations are most vulnerable, who may need more help to recover from specific disasters, and what types of health impacts are likely to result from the disaster. For example, children, women, those who are socially, educationally, and economically disadvantaged, the elderly, and men and women who depend directly on specific ecosystem services (e.g., fisheries and tourism) for their livelihoods are most likely to be impacted (Table 1). Long‐term effects of chronic and cumulative stress and associated negative health outcomes (e.g., PTSS, anxiety, depression, substance abuse, domestic disturbances, and increased cardiovascular and other inflammatory‐based diseases), as well as direct physical and mental traumatic injury, will need both immediate and continuing medical attention following disasters. These populations and health challenges are not the traditional ones considered immediately after a technological disaster such as an oil spill that tends to focus most attention on the direct impacts of oil and toxins on first responders and communities while overlooking or placing less emphasis on other impacts to communities dependent on fisheries and natural resources.
DPSERH can help provide a more realistic cost estimate of disasters. DPSERH shows that there are many effects on humans beyond the initial potential for acute injuries or disease and that, therefore, all of these human health effects should receive at least equal attention to that accorded environmental damages in assessing restoration and recovery costs and time frames. The model helps identify additional impacts of disasters that are not currently accounted for in disaster response or planning. Society is currently grossly underestimating the societal costs of disasters such as the DWH. None of the estimates of economic impact due to Hurricane Katrina or the DWH catastrophe nor those of other similar disasters like Hurricane Sandy [USDOC, 2013] included realistic assessments of costs incurred due to physical and mental illness and diminished well‐being, or for treatment of both short‐ and long‐term health consequences among infants, children, adolescents, adults, and vulnerable subpopulations. To prevent this situation from happening in the future, policy makers should ensure that costs for assessment, treatment, recovery, and monitoring of the health of humans and communities affected by disasters, and the subsequent loss of ecosystem services, are included in calculations of penalties and recovery of damages from responsible parties and in government‐supported recovery efforts.
Disaster preparedness and recovery planning should incorporate the DPSERH framework to account for human health and well‐being requirements. This includes monitoring of selected health and well‐being parameters from individual to community levels in order to determine when damage and recovery have occurred and to what extent.
In conjunction with other tools, the model could be used to direct investments in improving capabilities of the public health community, biomedical researchers, and environmental scientists and to help guide development and implementation of an integrated, rapid disaster research response capacity [Lurie et al., 2013; Miller et al., 2016; Sandifer et al., 2007]. Special emphasis should be placed on predisaster and postdisaster collection of clinically and diagnostically relevant biomarkers, mental health indices, and other data on psychological and physiological conditions of individuals and groups and monitoring of these indicators over time to quantify stress‐related human health impacts and their long‐term recovery. Such data could be used in conjunction with the model described here to help attribute causes of observed effects and to assess and document overall recovery and specifically that related to restoration of the full suite and quality of ecosystem services.
For future disasters including extreme climate events such as drought, forest fires, heat waves, and floods, this model can help fill the gap between our understanding of immediate human health impacts and the longer‐term impacts to human health and well‐being that develop and may persist for extended periods of time due to disaster impacts on ecosystem services on which human communities depend.
5. Conclusions
The DPSERH model described here is among the first to connect damage to ecosystem services from environmental disasters (e.g., hurricanes and major oil spills) to a broad range of human health effects within a comprehensive conceptual framework. To our knowledge, it is the first to connect negative health outcomes associated with acute, chronic, and cumulative stress to disaster‐linked degradation of individual and multiple ecosystem services. In addition to elements of the well known and often modified DPSIR (Driver‐Pressure‐State‐Impacts‐Response) environmental model, our DPSERH model incorporates the allostatic load concept of cumulative stress and the associated physiological mechanisms of action that result in mental and physical disorders. The framework illustrates how disasters have much broader impacts on human health and well‐being at individual to community levels than just direct bodily and property injury. The model allows one to visualize and tease apart the myriad ways by which oil spills, hurricanes, and other disasters cause changes in key ecosystem components and thereby reduce individual and aggregate ecosystem services that support people's livelihoods, health, and way of life. Further, the model elucidates how damage to ecosystem services produces acute, chronic, and cumulative stress in humans and at least some of the physiological mechanisms by which cumulative stress increases risk of adverse psychological and physiological health outcomes. This new and innovative DPSERH tool can be used to improve disaster preparedness and recovery planning for hurricanes, oil spills, and many other kinds of environmental and technological disasters, help target investments in key areas for disaster‐focused public health and research capacity building, including predisaster and postdisaster data collection and analysis, and support development and implementation of policies to identify disaster‐related human health impacts and include human health response and recovery in damage assessments.
Fundamental requirements for community planning include identifying vulnerabilities, risks, priorities, and information gaps and developing courses of action based on available information. Our DPSERH model helps demonstrate the interconnectedness of cascading incidents across the full spectrum of the community that includes ecosystem services. In addition, it provides an ecosystem framework for holistic community planning related to disasters, such as development of community HIAs and the community‐specific emergency support function that addresses public health and medical services. Using this conceptual model, a community can analyze the critical connections among key environmental criteria of “community health,” for example, clean air, water, and natural and open spaces.
Conflict of Interest
The authors declare no conflicts of interest relevant to this study.
Acknowledgments
This work was funded by the National Academy of Sciences Gulf Research Program, exploratory grant 2000005981. Additional financial support was provided by the Gulf of Mexico Research Initiative. Richard Kwok was supported by the Intramural Research Program of the NIH, National Institute of Environmental Health Sciences. A. Sutton‐Grier was supported by NOAA grant NA14NES4320003 (Cooperative Institute for Climate and Satellites‐CICS) at the University of Maryland/ESSIC. The funding sources had no roles in the design or execution of the project, collection, analysis, or interpretation of data/information, writing of the paper, or decision to submit the work for publication. The authors declare no conflicts of interest. We thank the College of Charleston and NOAA's Hollings Marine Laboratory for institutional support, Catherine Polk (NOAA affiliate) for graphics support, and the following experts who, along with the authors, participated in project workshops: Jeffrey Adkins (I.M. Systems Group, NOAA), Kent Carpenter (Old Dominion University), Greg Gibson (Georgia Institute of Technology), Kyle Esteves (Tulane University), Leslie Hart (College of Charleston), Andrew Kane (University of Florida), Susan Lovelace (SC Sea Grant Consortium), Karyn Morrissey (University of Exeter Medical School, UK), Omar Muhammad (SC Department of Natural Resources and Lowcountry Alliance for Model Communities), Steven Murawski (University of South Florida), Liesel Ritchie (University of Colorado), Ariane Rung (Louisiana State University), Lori Schwacke (NOAA), Patricia Sobecky (University of Alabama at Tuscaloosa), Erik Svendsen (Medical University of South Carolina), and Juli Trtanj (NOAA). Data supporting the conclusions of this study may be found in the tables, references cited, and in publicly accessible data portals for the Gulf of Mexico.
Sandifer, P. A. , et al. (2017), A conceptual model to assess stress‐associated health effects of multiple ecosystem services degraded by disaster events in the Gulf of Mexico and elsewhere, GeoHealth, 1, 17–36, doi: 10.1002/2016GH000038.
This article was corrected on 15 JUL 2019. The online version of this article has been modified to include a Conflict of Interest statement.
References
- Abramson, D. , Stehling‐Ariza T., Garfield R., and Redlener I. (2008), Prevalence and predictors of mental health distress post‐Katrina: Findings from the Gulf Coast Child and Family Health Study, Disaster Med. Public Health Prep., 2(2), 77–86, doi: 10.1097/DMP.0b013e318173a8e7. [DOI] [PubMed] [Google Scholar]
- Abramson, D. M. , Grattan L. M., Mayer B., Colten C. E., Arosemena F. A., Bedimo‐Rung A., and Lichtveld M. (2015), The resilience activation framework: A conceptual model of how access to social resources promotes adaptation and rapid recovery in post‐disaster settings, J. Behav. Health Serv. Res., 42(1), 42–57, doi: 10.1007/s114114-014-9420-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adeola, F. O. , and Picou J. S. (2012), Race, social capital, and the health impacts of Katrina: Evidence from the Louisiana and Mississippi Gulf Coast, Res. Hum. Ecol., 19(1), 10–24. [Google Scholar]
- Adeola, F. O. , and Picou J. S. (2014), Social capital and the mental health impacts of Hurricane Katrina: Assessing long‐term patterns of psychosocial distress, IJMED, 32(1), 121–156. [Google Scholar]
- Adger, W. , Hughes T. P., Folke C., Carpenter S. R., and Rockstron J. (2005), Social‐ecological resilience to coastal disasters, Science, 309, 1036–1039, doi: 10.1126/science.1112122. [DOI] [PubMed] [Google Scholar]
- Adkins, J. (2015), The Gulf Coast economy: Ten years after Hurricanes Katrina and Rita, NOAA, Digital Coast GeoZone: Tech Talk for the Digital Coast. [Available at https://geozoneblog.wordpress.com/2015/08/24/katrina-10yr-econ/.]
- Aguilera, F. , Méndez J., Pásaro E., and Laffon B. (2010), Review on the effects of exposure to spilled oils on human health, J. Appl. Toxicol., 30, 291–301. [DOI] [PubMed] [Google Scholar]
- Albrecht, G. (2005), “Solastalgia”: A new concept in health and identity, Philos. Act. Nat., 3, 41–55. [Google Scholar]
- Atwoli, L. , Platt J. M., Basu A., Williams D. R., Stein D. J., and Koenen K. C. (2016), Associations between lifetime potentially traumatic events and chronic physical condition in the South African stress and health survey: A cross‐sectional study, BMC Psychiatry, 16, 214–224, doi: 10.1186/s12888-016-0929-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron, R. M. , and Kenny D. A. (1986), The moderator‐mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations, J. Pers. Soc. Psychol., 51(6), 1173–1182. [DOI] [PubMed] [Google Scholar]
- Barron, M. G. (2012), Ecological impacts of the Deepwater Horizon oil spill: Implications for immunotoxicity, J. Toxicol. Pathol., 40(2), 315–320, doi: 10.1177/0192623311428474. [DOI] [PubMed] [Google Scholar]
- Berger, M. , Juster R.‐P., and Sarnyai Z. (2015), Mental health consequences of stress and trauma: Allostatic load markers for practice and policy with a focus on indigenous health, Australas. Psychiatry, 23(6), 644–9, doi: 10.1177/1039856215608281. [DOI] [PubMed] [Google Scholar]
- Beyer, J. , Trannum H. C., Bakke T., Hodson P. W., and Collier T. K. (2016), Environmental effects of the Deepwater Horizon oil spill: A review, Mar. Pollut. Bull., 110(1), 28–51, doi: 10.1016/j.marpolbul.2016.06.027. [DOI] [PubMed] [Google Scholar]
- Bizik, G. , Picard M., Nijjar R., Tourjman V., McEwen B. S., Lupien S. J., and Juster R.‐P. (2013), Allostatic load as a tool for monitoring physiological dysregulation an comorbidities in patients with severe mental illness, Harv. Rev. Psychiatry, 21(6), 296–313, doi: 10.1097/HRP.0000000000000012. [DOI] [PubMed] [Google Scholar]
- Bomey, N. (2016), BP's Deepwater Horizon costs total $62 B. USA Today, July 14, 2016. [Available at http://www.usatoday.com/story/money/2016/07/14/bp-deepwater-horizon-costs/87087056/.]
- Bradley, P. , and Yee S. (2015), Using the DPSIR framework to develop a conceptual model: Technical support document, USEPA, Office of Research and Development, Atlantic Ecology Division, Narragansett, RI, EPA/600/R‐15/15. [Available at http://www.epa.gov/nscep/index.html.]
- Briggs, D. (1999), Environmental health indicators: Framework and methodologies, World Health Organization, WHO/SDE/OEH/99.10, 122 pp.
- Broughton, E. (2005), The Bhopal disaster and its aftermath: A review, Environ. Health, 4(1), 6, doi: 10.1186/1476-069X-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cairns, J., Jr. , and Pratt J. R. (1995), The relationship between ecosystem health and delivery of ecosystem services, in Evaluating and Monitoring the Health of Large Scale Ecosystems, edited by Rapport D. J., Gaudet C., and Calow P., pp. 63–76, Springer, Verlag. [Google Scholar]
- Cheong, H.‐K. , Lee J. S., Kwon H., Houg Y.‐C., Choi Y., Jeong W.‐C., Lee S.‐M., Kim E.‐J., and Im H. (2011), Hebei Spirit oil exposure and subjective symptoms in residents participating in clean‐up activities, Environ. Health Toxicol., 26, e201107, doi: 10.5260/eht.2011.26.e201107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherry, K. E. , Lyon B. A., Marks L. D., Nezat P. F., Adamek R., Walsh S. D., Fitzgerald K. B., Anbinder D. R., and Bernacchio C. V. (2015), After the BP Deepwater Horizon oil spill: Financial and health concerns among coastal residents and commercial fishers, Curr. Psychol., 34, 576–586, doi: 10.1007/s12144-015-9372-4. [DOI] [Google Scholar]
- Colgan, C. S. , and Adkins J. (2006), Hurricane damage to the ocean economy in the U.S. gulf region in 2005, Monthly Labor Review Aug 2006, 76–78.
- Committee on Environment and Natural Resources (2010), Scientific Assessment of Hypoxia in U.S. Coastal Waters, 154 pp., Interagency Working Group on Harmful Algal Blooms, Hypoxia and Human Health of the Subcommittee on Ocean Science and Technology, Washington, D. C. [Google Scholar]
- Cook, G. S. , Fletcher P. J., and Kelble C. R. (2014), Towards marine ecosystem based management in South Florida: Investigating the connections among ecosystem pressures, states, and services in a complex coastal system, Ecol. Indic., 44, 26–39, doi: 10.1016/j.ecolind.2013.10.026. [DOI] [Google Scholar]
- Cope, M. R. , Slack T., Blanchard T. C., and Lee M. R. (2013), Does time heal all wounds? Community attachment, natural resources employment, and health impacts in the wake of the BP Deepwater Horizon disaster, Soc. Sci. Res., 42, 872–881, doi: 10.1016/j.ssresearch.2012.12.011. [DOI] [PubMed] [Google Scholar]
- Corvalan, C. , Briggs D., and Kjellstrom T. (1996), Development of environmental health indicators, in Linkage Methods for Environment and Health Analyses. General Guidelines, edited by Briggs D., Corvalan C., and Nurminem M., pp. 19–53, UNEP, NSEPA, and WHO, Geneva. [Google Scholar]
- Crews, D. E. (2007), Composite estimates of physiological stress, age, and diabetes in American Samoans, Am. J. Phys. Anthropol., 133, 1028–1034. [DOI] [PubMed] [Google Scholar]
- Crimmins, E. M. , Kim J. K., Alley D. E., Karlamangla A., and Seeman T. (2007), Hispanic paradox in biological risk profiles, Am. J. Public Health, 97, 1305–1310, doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutter, S. L. , and Zoback M. L. (2013), Improving the nation's resilience to disasters, Eos, 94(9), 89–90. [Google Scholar]
- Daily, G. C. (1997), Nature's Services: Societal Dependence on Natural Ecosystems, 392 pp., Island Press, Washington, D. C. [Google Scholar]
- Eisenham, D. P. , Cordasco K. M., Asch S., Golden J. F., and Gilk D. (2007), Disaster planning and risk communication with vulnerable communities: Lessons from Katrina, Am. J. Public Health, 97, S109–S115, doi: 10.2105/AJPH.2005.084335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans, G. W. (2003), A multimethodological analysis of cumulative risk and allostatic load among rural children, Dev. Psychol., 39(5), 924–933, doi: 10.1037/0012-1649.39.5.924. [DOI] [PubMed] [Google Scholar]
- Evans, G. W. , Kim P., Ting A. H., Tesher H. B., and Shannis D. (2007), Cumulative risk, maternal responsiveness, and allostatic load among young adolescents, Dev. Psychol., 43(2), 341–351, doi: 10.1036/0012-1649.43.2.341. [DOI] [PubMed] [Google Scholar]
- Fan, A. Z. , Prescott M. R., Zhao G., Gotway C. A., and Galea S. (2015), Individual and community‐level determinants of mental and physical health after the Deepwater Horizon oil spill: Findings from the Gulf States Population Survey, J. Behav. Health Serv. Res., 42(1), 23–41, doi: 10.1007/s11414-014-9418-7. [DOI] [PubMed] [Google Scholar]
- Farber, S. , et al. (2006), Linking ecology and economics for ecosystem management, Bioscience, 56(2), 117–129, doi: 10.1641/0006-3568(2006)056[0121:LEAEFE]2.0.C. [DOI] [Google Scholar]
- Foley, M. M. , et al. (2010), Guiding ecological principles for marine spatial planning, Mar. Pol., 34(5), 955–966, doi: 10.1016/j.marpol.2010.02.001. [DOI] [Google Scholar]
- Freudenberg, W. (1997), Contamination, corrosion, and the social order: An overview, Curr. Sociol., 45, 19–39, doi: 10.1177/001139297045003002. [DOI] [Google Scholar]
- Galea, S. , Nandi A., and Vlahov D. (2005), The epidemiology of post‐traumatic stress disorder after disasters, Epidemiol. Rev., 27, 78–91, doi: 10.1093/epirev/mxi003. [DOI] [PubMed] [Google Scholar]
- Galea, S. , Brewin C. R., Gruber M., Jones R. T., King D. W., King L. A., McNally R. J., Ursano R. J., Petukhova M., and Kessler R. C. (2007), Exposure to hurricane‐related stressors and mental illness after Hurricane Katrina, Arch. Gen. Psychiatry, 64(12), 1427–1434, doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert, D. , and Kent S. (2015), Deepwater Horizon oil spill claims. Wall Street Journal. 2 July 2015. [Available at http://www.wsj.com/articles/bp-agrees-to-pay-18-7-billion-to-settle-deepwater-horizon-oil-spill-claims-1435842739, accessed 6 Mar 2016.]
- Gill, D. A. , Picou J. S., and Ritchie L. A. (2012), The Exxon Valdez and BP oil spills: A comparison of initial social and psychological impacts, Am. Behav. Sci., 56(1), 3–23, doi: 10.1177/0002264211408585. [DOI] [Google Scholar]
- Gill, D. A. , Ritchie L. A., Picou J. S., Langhinrichsen‐Rohling J., Long M. A., and Shenesey J. W. (2014), The Exxon and BP oil spills: A comparison of psychosocial impacts, Nat. Hazards, 74, 1911–1932, doi: 10.1007/s11069-014-1280-7. [DOI] [Google Scholar]
- Glover, D. A. , Stuber M., and Poland M. E. (2006), Allostatic load in women with and without PTSD symptoms, Psychiatry, 69(3), 101–103, doi: 10.1521/psyc.2006.69.3.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman, N. , Turra C. M., Glei D. A., Seplaki C. L., Lin Y. H., and Weinstein M. (2006), Predicting mortality from clinical and nonclinical biomarkers, J. Gerontol. A Biol. Sci. Med. Sci., 61(10), 1070–1074. [DOI] [PubMed] [Google Scholar]
- Gothenburg Consensus Paper (1999), Health impact assessment. Main concepts and suggested approach, European Centre for Health Policy, Brussels, 11 pp.
- Gould, D. W. , Teich J. L., Pemberton M. R., Pierannunzi C., and Larson S. (2015), Behavioral health in the Gulf Coast region following the Deepwater Horizon oil spill: Findings from two federal surveys, J. Behav. Health Serv. Res., 42(1), 6–22, doi: 10.1007/s11414-014-9441-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grattan, L. M. , Roberts S., Mahan W. T. Jr., McLaughlin P. K., Otwell W. S., and Morris J. G. (2011), The early psychological impacts of the Deepwater Horizon oil spill on Florida and Alabama communities, Environ. Health Perspect., 119(6), 838–843, doi: 10.1289/ehp.1002915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruenewald, T. L. , Seeman T. E., Ryff C. D., Karlamangla A. S., and Singer B. H. (2006), Combinations of biomarkers predictive of later life mortality, Proc. Natl. Acad. Sci. U.S.A., 103, 14158–14163, doi: 10.1073/pnas.0606215103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulf Coast Restoration Task Force (2011), Gulf of Mexico regional ecosystem restoration strategy, 119 pp., USEPA, Washington, D. C. [Available at http://energy.gov/sites/prod/files/GulfCoastReport_Full_12-02_508.pdf.]
- Gundlach, E. R. , Finkelstein K., and Sadd J. (1981), Impact and persistence of Ixtoc I oil on the south Texas coast, in Proceedings of the 1981 International Oil Spill Conference (Prevention, Behavior, Control, Cleanup), pp. 477–485, Atlanta, Georgia.
- Halpern, B. S. , et al. (2012), Near‐term priorities for the science, policy and practice of Coastal and Marine Spatial Planning (CMSP), Mar. Policy, 36, 198–205, epub: 2011, doi: 10.1016/jmarpol.2011.05.004. [DOI] [Google Scholar]
- Hambling, T. , Weinstein P., and Slaney D. (2011), A review of frameworks for developing environmental health indicators for climate change and health, Int. J. Res. Public Health, 8(7), 2854–2875, doi: 10.3390/ijerph8072854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansel, T. C. , Osofsky H. J., Osofsky J. D., and Speier A. (2015), Long‐term mental and behavioral health effects of the Deepwater Horizon Gulf oil spill, J. Mar. Sci. Eng., 3, 1260–1271, doi: 10.3390/jmse3041260.s. [DOI] [Google Scholar]
- Horwitz, P. , and Finlayson M. (2011), Wetlands as settings for human health: Incorporating health impact assessment into water resource management, BioScience, 61(9), 678–688, doi: 10.1525/bio.2011.61.9.6. [DOI] [Google Scholar]
- Incardona, J. P. , et al. (2014), Deepwater Horizon crude oil impacts the developing hearts of large predatory pelagic fish, Proc. Natl. Acad. Sci. U.S.A., 111(15), E1510–E1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (2007), Environmental public health impacts of disasters: Hurricane Katrina, Workshop summary, L Goldman and C. Coussens, rapporteurs, Institute of Medicine Roundtable on Environmental Health Sciences, Research, and Medicine, 101 pp., The National Academies Press, Washington, D. C. [PubMed]
- Irwantol, F. , and Zulfa H. (2015), Posttraumatic stress disorder among Indonesian children 5 years after the tsunami, Southeast Asian J. Trop. Med. Public Health, 46(5), 918–923. [PubMed] [Google Scholar]
- Jackson, L. E. , Daniel J., McCorkle B., Sears A., and Bush K. F. (2013), Linking ecosystem services and human health: The Eco‐Health Relationship Browser, Int. J. Public Health, 58, 747–755, doi: 10.1007/s00038-013-0482-1. [DOI] [PubMed] [Google Scholar]
- Jaycox, L. H. , Cohen J. A., Mannarino A. P., Walker D. W., Langley A. K., Gegenheimer K. L., Scott M., and Schonlau M. (2010), Children's mental health care following Hurricane Katrina: A field trial of trauma‐focused psychotherapies, J. Trauma. Stress, 23, 223–231, doi: 10.1002/jts.20518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joye, S. (2015), Deepwater Horizon, 5 years on, Science, 349(6428), 592–593, doi: 10.1126/science.aab4133. [DOI] [PubMed] [Google Scholar]
- Jung, S.‐C. , et al. (2013), Respiratory effects of the Hebei Spirit oil spill on children in Taean, Korea, Allergy, Asthma Immunol. Res., 5(6), 365–370, doi: 10.4168/aair.2013.5.6.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juster, R. P. , McEwen B. S., and Lupien S. J. (2010), Allostatic load biomarkers of chronic stress and impact on health and cognition, Neurosci. Biobehav. Rev., 35(1), 2–16, doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Juster, R.‐P. , et al. (2011a), A transdisciplinary perspective of chronic stress in relation to psychopathology throughout life span development, Dev. Psychopathol., 23, 725–776, doi: 10.1017/S0954579411000289. [DOI] [PubMed] [Google Scholar]
- Juster, R.‐P. , Marin M.‐F., Sindi S., Nair N. P. V., Ng Y. K., Pruessner J. C., and Lupien S. J. (2011b), Allostatic load associations to acute, 3‐year and 6‐year prospective depressive symptoms in healthy older adults, Physiol. Behav., 104(2), 360–364, doi: 10.1016/j.physbeh.2011.02.027. [DOI] [PubMed] [Google Scholar]
- Juster, R.‐P. , et al. (2016), Chapter 8. Social inequalities and the road to allostatic load: From vulnerability to resilience, in Developmental Psychopathology: Risk, Resilience, and Intervention, vol. 4, 3rd ed., edited by Cichetti D., pp. 381–43, Wiley, New York. [Google Scholar]
- Karlamangla, A. S. , Singer B. H., McEwen B. S., Rowe J. W., and Seeman T. E. (2002), Allostatic load as a predictor of functional decline: MacArthur studies of successful aging, J. Clin. Epidemiol., 55, 696–710. [DOI] [PubMed] [Google Scholar]
- Keim, M. E. (2011), The public health impact of industrial disasters, Am. J. Disaster Med., 6(5), 265–72. [DOI] [PubMed] [Google Scholar]
- Kelble, C. R. , Loomis D. K., Lovelace S., Nuttle W. K., Ortner P. B., Fletcher P., Cook G. S., Lorenz J. J. J., and Boyer J. N. (2013), The EBM‐DPSER conceptual model: Integrating ecosystem services into the DPSIR framework, PLoS ONE, 8(8), e70766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemm, J. (2001), Health impact assessment: A tool for public policy, Health Promot. Int., 16(1), 79–85. [DOI] [PubMed] [Google Scholar]
- King, L. S. , Osofsky J. D., Osofsky H. J., Weems C. F., Hansel T. C., and Fassnacht G. M. (2015), Perceptions of trauma and loss among children and adolescents exposed to disasters, a mixed methods study, Curr. Psychol., 34, 524–536, doi: 10.1007/s12144-015-9348-4. [DOI] [Google Scholar]
- King, G. M. , Kostka J. E., Hazen T. C., and Sobecky P. A. (2015), Microbial responses to the Deepwater Horizon oil spill: From coastal wetlands to the deep sea, Ann. Rev. Mar. Sci., 7, 377–401, doi: 10.1146/annurev-marine-010814-015543. [DOI] [PubMed] [Google Scholar]
- Kostka, J. E. , Prakash O., Overholt W. A., Green S. J., Freyer G., Canion A., Campion J., Norton N., Hazen T. C., and Huettel M. (2011), Hydrocarbon‐degrading bacteria and the bacterial community response in Gulf of Mexico beach sands impacted by the Deepwater Horizon oil spill, Appl. Environ. Micro., 77(22), 7962–7974, doi: 10.1128/AEM.05402.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krejsa, P. (1997), Report on early warning for technological hazards, UN‐IDNDR Secretariat, Geneva, [A Report on technological risks prevention issued for the International Decade for Natural Disaster Reduction – UN, Early Warnings Programme]. [Available at http://www.unisdr.org/2006/ppew/whats-ew/pdf/report-on-ew-for-technological-hazards.pdf.]
- Kwok, R. K. , et al. (2017), The GuLF STUDY: A prospective study of persons involved in the Deepwater Horizon oil spill response and clean‐up, Environ. Health Perspect., 125, 570–578, doi: 10.1289/EHP715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laffon, B. , Pásaro E., and Valdiglesias V. (2016), Effects of exposure to oil spills on human health: Updated review, J. Toxicol. Environ. Health B Crit. Rev., 19(3–4), 105–128, doi: 10.1080/10937404.2016.1168730. [DOI] [PubMed] [Google Scholar]
- Learning, J. , and Guha‐Sapir D. (2013), Natural disasters, armed conflict, and public health, New Engl. J. Med., 369, 1836–1842, doi: 10.1056/NEJMra1109877. [DOI] [PubMed] [Google Scholar]
- Lee, K. , Boufadel M., Chen B., Foght J., Hodson P., Swanson S., and Venosa A. (2015), Expert panel report on the behaviour and environmental impacts of crude oil released into aqueous environments, Roy. Soc. Canada, Ottawa, ON. [Available at http://www.cepa.com/wp-content/uploads/2014/01/OIW-Report.compressed.pdf.]
- Levine, E. , and Picou J. S. (2012), Dispersants and risk communication whitepaper, in The Future of Dispersant Use in Oil Spill Response Initiative, edited by Kinner N. and Helton D., Appendix 1 g, pp. 16, Coastal Response Research Center, Research Planning Incorporated, National Oceanic and Atmospheric Administration, Mobile, Ala. [Google Scholar]
- Lindell, M. K. (2013), Disaster studies, Curr. Sociol., 61(5–6), 797–825. [Google Scholar]
- Logan, J. G. , and Barksdale D. J. (2008), Allostasis and allostatic load: Expanding the discourse on stress and cardiovascular disease, J. Clin. Nurs., 17(7b), 201–208, doi: 10.1111/j.1365-2702.2008.02347.x. [DOI] [PubMed] [Google Scholar]
- Lovelace, S. , Goedeke T.L., and Dillard M. (2012), Prioritizing county‐level well‐being: Moving toward assessment of Gulf coast counties impacted by the Deepwater Horizon industrial disaster, NOAA Tech Mem NOS/NCCOS 146, 48 pp.
- Lowe, S. R. , Kwok R. K., Payne J., Engel L. S., Galea S., and Sandler D. P. (2015), Mental health service use by cleanup workers in the aftermath of the Deepwater Horizon oil spill, Soc. Sci. Med., 130, 125–134, doi: 10.1016/j.socscimed.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubchenco, J. , McNutt M. K., Dreyfus G., Murawski S. A., Kennedy D. M., Anastas P. A., Chu S., and Hunter T. (2012), Science in support of the Deepwater Horizon response, Proc. Natl. Acad. Sci. U.S.A., 109(50), 20212–20221, doi: 10.1073/pnas.1204729109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie, N. , Manolio T., Patterson A. P., Collins F., and Frieden T. (2013), Research as a part of public health emergency response, N. Engl. J. Med., 368(13), 1251–1255, doi: 10.1056/NEJMsb1209510. [DOI] [PubMed] [Google Scholar]
- Maloney, E. M. , Gurbaxani B. M., Jones J. F., de Souza Coelho L., Pennachin C., and Goertzel B. N. (2006), Chronic fatigue syndrome and high allostatic load, Pharmacogenomics, 7(3), 467–473, doi: 10.2217/14622416.7.3.467. [DOI] [PubMed] [Google Scholar]
- Manuel, J. (2013), The long road to recovery: Environmental health impacts of Hurricane Sandy, Environ. Health Perspect., 121, A152–A159, doi: 10.1289/ehp.121-a152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathur, M. B. , Epel E., Kind S., Desai M., Parks C. G., Sandler D. P., and Khazeni N. (2016), Perceived stress and telomere length: A systematic review, meta‐analysis, and methodologic considerations for advancing the field, Brain Behav. Immun., 4, 158–69, doi: 10.1016/j.bbi.2016.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCallum, E. , and Heming J. (2006), Hurricane Katrina: An environmental perspective, Phil. Trans. R. Soc. A, 364, 2099–2115, doi: 10.1098/rsta.2006.1815. [DOI] [PubMed] [Google Scholar]
- McCoy, M. A. , and Salerno J. A.(rapporteurs) (2010), Assessing the Effects of the Gulf of Mexico Oil Spill on Human Health, A Summary of the June 2010 Workshop, 201 pp., Institute of Medicine, National Academies of Science, National Academy Press, Washington, D. C. [PubMed] [Google Scholar]
- McEwen, B. S. (1998a), Stress, adaptation, and disease: Allostasis and allostatic loading, Ann. N. Y. Acad. Sci., 840, 33–44. [DOI] [PubMed] [Google Scholar]
- McEwen, B. S. (1998b), Protective and damaging effects of stress mediators, N. Engl. J. Med., 338, 171–179. [DOI] [PubMed] [Google Scholar]
- McEwen, B. S. (2000), Allostasis and allostatic load: Implications for neuropsychopharmacology, Neuropsychopharmacology, 22, 108–124. [DOI] [PubMed] [Google Scholar]
- McEwen, B. S. , and Gianaros P. J. (2010), Stress‐ and allostasis‐induced brain plasticity, Annu. Rev. Med., 62, 5.1–5.15, doi: 10.1146/annurev-med-052209-100430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen, B. S. , and Stellar E. (1993), Stress and the individual: Mechanisms leading to disease, Arch. Intern. Med., 53, 2093–2101. [PubMed] [Google Scholar]
- McKendree, M. G. , Ortega D.L., Widmar N. O., and Wang H. H. (2013), Consumer perceptions of seafood industries in the wake of the Deepwater Horizon oil spill and Fukushima Daiichi nuclear disaster, Michigan State University, Department of Agricultural, Food, and Resource Economics, No. 155582. [Google Scholar]
- McLaughlin, K. A. , Fairbank J. A., Gruber M. J., Jones R. T., Osofsky J. D., Pfefferbaum B., Sampson N. A., and Kessler R. C. (2010), Trends in serious emotional disturbance among youths exposed to Hurricane Katrina, J. Amer. Acad. Child Adolesc. Psychiatry, 49, 990–1000, 1000.e1‐2, doi: 10.1016/j.jaac.2010.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNutt, M. K. , Camilli R., Crone T. J., Guthrie G. D., Hseih P. A., Ryerson J. B., Savas O., and Shaffer F. (2012), Review of oil flow rate estimates of the Deepwater Horizon oil spill, Proc. Natl. Acad. Sci. U.S.A., 109, 20260–20267, doi: 10.1073/pnas.1112139108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendelssohn, I. A. , et al. (2012), Oil impacts on coastal wetlands: Implications for the Mississippi River Delta ecosystem after the Deepwater Horizon oil spill, BioScience, 62(6), 562–574, doi: 10.1525/bio.2012.62.6.7. [DOI] [Google Scholar]
- Millennium Ecosystem Assessment (MEA) (2005), Millennium Ecosystem Sssessment (Synthesis Report), Island Press, Washington, D. C. [Google Scholar]
- Miller, A. , et al. (2016), Integrating health research into disaster response: The new NIH disaster research response program, Int. J. Environ. Res. Public Health, 13, 676, doi: 10.3390/ijerph13070676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills, M. A. , Edmondson D., and Park C. L. (2007), Trauma and stress response among Hurricane Katrina evacuees, Amer. J. Pub. Health, 97(S1), S116–S123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mississippi River Gulf of Mexico Nutrient Task Force (2013), Reassessment 2013. Progress made since 2008, USEPA, 86 pp., Washington, D. C. [Available at https://www.epa.gov/ms-htf/hypoxia-task-force-reassessment-2013-assessing-progress-made-2008.]
- Morgan, O. A. , Whitehead J. C., Huth W. L., Martin G. S., and Sjolander R. (2016), Measuring the impact of the BP Deepwater Horizon oil spill on consumer behavior, Land Econ., 92(1), 82–95, doi: 10.3368/le.92.1.82. [DOI] [Google Scholar]
- Morris, J. G., Jr. , Grattan L. M., Mayer B. M., and Blackburn J. K. (2013), Psychological responses and resilience of people and communities impacted by the Deepwater Horizon oil spill, Trans. Amer. Clin. Climatol. Assoc., 124, 191–201. [PMC free article] [PubMed] [Google Scholar]
- National Academy of Sciences (2013), An Ecosystem Services Approach to Assessing the Impacts of the Deepwater Horizon Oil Spill in the Gulf of Mexico, Committee on the Effects of the Deepwater Horizon Mississippi Canyon‐252 Oil Spill on Ecosystem Services in the Gulf of Mexico, 265 pp., The National Academies Press, Washington, D. C. [PubMed] [Google Scholar]
- National Oceanic and Atmospheric Administration (NOAA) (2016), National Weather Service, Aug 2016 update. [Available at http://www.srh.noaa.gov/mob/?n=katrina.]
- Neria, Y. , Nandi A., and Galea S. (2007), Post‐traumatic stress disorder following disasters: A systematic review, Psychol. Med., 38, 467–480, doi: 10.1017/S0033291707001353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngo, D. , Gibbons J. L., Scire G., and Le D. (2014), Mental health needs in Vietnamese American communities affected by the oil spill, Psychol., 5(2), 109–115, doi: 10.4236/psych.2014.52017. [DOI] [Google Scholar]
- Noji, E. K. (1997), The Public Health Consequences of Disasters, 468 pp., Oxford Univ. Press, New York. [Google Scholar]
- Norris, F. H. , Stevens S. P., Pfefferbaum B., Wyche K., and Pfefferbaum R. L. (2008), Community resilience as a metaphor, theory, set of capacities, and strategy for disaster readiness, Am. J. Commun. Psychol., 41, 127–150, doi: 10.1007/s10464-007-9156-6. [DOI] [PubMed] [Google Scholar]
- Natural Resources Defense Council (2015), Summary of information concerning the ecological and economic impacts of the BP Deepwater Horizon oil spill disaster, NRDC Issue Paper IP‐15‐04‐A. 9 pp.
- Oesterwind, D. , Rau A., and Zaiko A. (2016), Drivers and pressures—Untangling the terms commonly used in marine science and policy, J. Environ. Manage., 181, 8–15, doi: 10.1016/j.jenvman.2016.05.058. [DOI] [PubMed] [Google Scholar]
- Olteanu, A. , Arnberger R., Grant R., Davis C., Abramson D., and Asola J. (2011), Persistence of mental health needs among children affected by Hurricane Katrina in New Orleans, Prehosp. Disaster Med., 26(1), 3–6. [DOI] [PubMed] [Google Scholar]
- Oosterbroek, B. , de Kraker J., Huynen M. M., and Martens P. (2016), Assessing ecosystem impacts on health: A tool review, Ecosyst. Serv., 17, 37–254, doi: 10.1016/j.ecoser.2015.12.008. [DOI] [Google Scholar]
- Organisation for Economic Co‐operation and Development (1993), OECD core set of indicators for environmental performance reviews: A synthesis report by the Group on the State of the Environment, Environ. Monogr., 83, 1–39. [Google Scholar]
- Osofsky, H. J. , Osofsky J. D., and Hansel T. C. (2011), Deepwater horizon oil spill: Mental health effects on residents in heavily affected areas, Disaster Med. Public Health Prep., 5(4), 280–286, doi: 10.1001/dmp.2011.85. [DOI] [PubMed] [Google Scholar]
- Osofsky, H. J. , Osofsky J. D., Wells J., Weems C. F., Hansel T. C., King L., and Ciccone A. (2014), Integrating mental and behavioral health into primary care clinics to develop a system of care following the Deepwater Horizon oil spill, IADC/SPE SPE‐168522‐MS/.
- Osofsky, J. D. , Osofsky H. J., Weems C. F., Hansel T. C., and King L. S. (2014), Effects of stress related to the gulf oil spill on child and adolescent mental health, J. Pediatric Psychol., 41(1), 65–72. [DOI] [PubMed] [Google Scholar]
- Palinkas, L. A. (2012), A conceptual framework for understanding the mental health impacts of oil spills: Lessons from the Exxon Valdez oil spill, Psychiatry, 75(3), 203–222, doi: 10.1521/psyc.2012.75.3.203. [DOI] [PubMed] [Google Scholar]
- Palinkas, L. A. (2015), Behavioral health and disasters: Looking to the future, J. Behav. Health Serv. R., 42(1), 86–95, doi: 10.1007/s11414-013-9390-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson, O. , Wall F., and Patel K. (2010), The role of community in disaster response: Conceptual models, Popul. Res. Policy Rev., 29, 127–141, doi: 10.1007/s11113-009-9133-x. [DOI] [Google Scholar]
- Paxson, C. , Fussell E., Rhodes J., and Waters M. (2012), Five years later: Recovery from post‐traumatic stress and psychological distress among low‐income mothers affected by Hurricane Katrina, Soc. Sci. Med., 74(2), 150–157, doi: 10.1016/j.socscimed.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peres, L. C. , Trapido E., Rung A. L., Harrington D. J., Oral E., Fang Z., Fontham E., and Peters E. S. (2016), The Deepwater Horizon oil spill and physical health among adult women in southern Louisiana: The Women and Their Childrens' Health (WaTCH) study, Environ. Health Perspec., 124, 1208–1213, doi: 10.1289/ehp.1510348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters, M. N. , et al. (2014), Natural disasters and myocardial infarction: The six years after Hurricane Katrina, Mayo Clinic Proc., 89, 472–477, doi: 10.1016/j.mayocp.2013.12.013. [DOI] [PubMed] [Google Scholar]
- Picard, M. , Juster R.‐P., and McEwen B. S. (2014), Mitochondrial allostatic load puts the “gluc” back in glucocorticoids, Nat. Rev. Endocrinol., 10, 303–310, doi: 10.1038/nrendo.2014.22. [DOI] [PubMed] [Google Scholar]
- Picou, J. S. , and Hudson K. (2010), Hurricane Katrina and mental health: A research note on Mississippi coastal residents, Sociol. Inq., 80(3), 513–524, doi: 10.1111/j.1475-682X.2020.00345.x. [DOI] [PubMed] [Google Scholar]
- Qureshi, K. A. , Gershon R., Merrill J. A., Calero‐Breckheimer A., Murrman M., Gebbie K. M., Moskin L. C., May L., Morse S., and Sherman M. (2004), Effectiveness of emergency preparedness training program for public health nurses in New York City, Fam. Community Health, 27(3), 242–249. [DOI] [PubMed] [Google Scholar]
- Rapport, D. J. , Costanza R., and McMichael A. J. (1998), Assessing ecosystem health, Trends Ecol. Evol., 13(10), 397–402, doi: 10.1016/S0169-5347(98)01449-9. [DOI] [PubMed] [Google Scholar]
- Reis, S. , et al. (2015), Integrating health and environmental impact, Pub. Health, 129, 1383–1389. [DOI] [PubMed] [Google Scholar]
- Rhodes, J. , Chan C., Paxson C., Rouse C. E., Waters M., and Fussell E. (2010), The impact of Hurricane Katrina on the mental and physical health of low‐income parents in New Orleans, Am. J. Orthopsychiatry, 80(2), 237–247, doi: 10.1111/j.1939-0025.2010.01027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rung, A. L. , Gaston S., Oral E., Robinson W. T., Fontham E., Harrington D. J., Trapido E., and Peters E. S. (2016), Depression, mental distress, and domestic conflict among Louisiana women exposed to the Deepwater Horizon oil spill in the WaTCH study, Environ. Health Perspect., 124(9), 1429–1435, doi: 10.1289/EHP167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabbah, W. , Watt R. G., Sheiham A., and Tsakos G. (2008), Effects of allostatic load on the social gradient in ischaemic heart disease and periodontal disease: Evidence from the Third National Health and Nutrition Examination Survey, J. Epidemiol. Community Health, 62, 415–420, doi: 10.1136/jech.2007.064188. [DOI] [PubMed] [Google Scholar]
- Sandifer, P. , Sotka C., Garrison D., and Fay V. (2007), Interagency oceans and human health research implementation plan: A prescription for the future, Interagency Working Group on Harmful Algal Blooms, Hypoxia and Human Health of the Joint Subcommittee on Ocean Science and Technology, 92 pp., Washington, D. C. [Google Scholar]
- Sandifer, P. A. , and Sutton‐Grier A. E. (2014), Connecting stressors, ocean ecosystem services, and human health, Nat. Res. Forum, 38, 157–167, doi: 10.1111/1477-8947.12047. [DOI] [Google Scholar]
- Sandifer, P. A. , Collier T. K., and Trtanj J. M. (2012), Coastal ecosystems, sustainable management, Encycl. Sustain. Sci. Technol., 4, 2258–2270. [Google Scholar]
- Sandifer, P. A. , Sutton‐Grier A. E., and Ward B. P. (2015), Exploring connections among nature, biodiversity, ecosystem services, and human health and well‐being: Opportunities to enhance health and biodiversity conservation, Ecosyst. Serv., 12, 1–15, doi: 10.1016/j.ecoser.2014.12.007. [DOI] [Google Scholar]
- Schneiderman, N. , Ironson G., and Siegel S. D. (2005), Stress and health: Psychological, behavioral, and biological determinants, Annu. Rev. Clin. Psychol., 1, 607–628, doi: 10.1146/annurev.clinpsy.1.102803.144141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumacher, J. A. , Coffey S. F., Norris F. H., Tracy M., Clements K., and Galea S. (2010), Intimate partner violence and Hurricane Katrina: Predictors and associated mental health outcomes, Violence Vict., 25, 588–603, doi: 10.1891/0886-6708.25.5.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwacke, L. I. , et al. (2014), Health of common bottlenose dolphins (Tursiops truncatus) in Barataria Bay, Louisiana, following the Deepwater Horizon oil spill, Environ. Sci. Technol., 48(1), 93–103, doi: 10.1021/es403610f. [DOI] [PubMed] [Google Scholar]
- Seeman, T. E. , McEwen B. S., Rowe J. W., and Singer B. H. (2001), Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging, Proc. Natl. Acad. Sci. U.S.A., 98, 4770–4775, doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman, T. E. , Crimmins E., Huang M. H., Singer B., Bucur A., Gruenewald T., Berkman L. F., and Reuben D. B. (2004), Cumulative biological risk and socio‐economic differences in mortality: MacArthur studies of successful aging, Soc. Sci. Med., 58, 1985–1997, doi: 10.1016/S0277-9536(03)00402-7. [DOI] [PubMed] [Google Scholar]
- Segerstrom, S. C. , and Miller G. E. (2004), Psychological stress and the human immune system: A meta‐analytic study of 30 years of inquiry, Psychol. Bull., 130(4), 601–630, doi: 10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekovski, I. , Newton A., and Dennison W. C. (2012), Megacities in the coastal zone: Using a driver‐pressure‐state‐impact‐response framework to address complex environmental problems, Estuar. Coast. Shelf Sci., 96, 48–59, doi: 10.1016/j.ecss.2011.07.011. [DOI] [Google Scholar]
- Sever, M. (2006), After Katrina: Oil spill first responders, Geotimes Feb. 2006.
- Sheikh, P. A. (2005), The impact of Hurricane Katrina on biological resources, Congressional Research Service, Library of Congress, Washington, D. C., Order Code RL33117.
- Shenesey, J. W. , and Langhinrichsen‐Rohling J. (2015), Perceived resilience: Examining impacts of the Deepwater Horizon oil spill one‐year post‐spill, Psychol. Trauma., 7(3), 252–258, doi: 10.1037/a0035182. [DOI] [PubMed] [Google Scholar]
- Shultz, J. M. , Russell J., and Espinel Z. (2005), Epidemiology of tropical cyclones: The dynamics of disaster, disease, and development, Epidemiol. Rev., 27, 21–35, doi: 10.1093/epirev/mxi011. [DOI] [PubMed] [Google Scholar]
- Shultz, J. M. , Walsh L., Garfin D. R., Wilson F. E., and Neria Y. (2015), The 2010 Deepwater Horizon oil spill: The trauma signature of an ecological disaster, J. Behav. Health Serv. Res., 42(1), 58–76, doi: 10.1007/s11414-014-9398-7. [DOI] [PubMed] [Google Scholar]
- Silei, G. (2014), Technological hazards, disasters and accidents, in The Basic Environmental History, pp. 227–253, Springer International Publishing. [Google Scholar]
- Slovic, P. , and Peters E. (2006), Risk perception and affect, Curr. Dir. Psychol. Sci., 15(6), 322–325, doi: 10.1111/j.1467-8721-2006-0461.x. [DOI] [Google Scholar]
- Smith, C. , et al. (2017), Slow recovery of Barrataria Bay dolphin health following the Deepwater Horizon oil spill (2013–2014), with evidence of persistent lung disease and impaired stress response, Endanger. Species Res., 33, 127–142, doi: 10.3354/esr00778. [DOI] [Google Scholar]
- Smith, L. M. , Case J. L., Smith H. M., Harwell L. C., and Summers J. K. (2013), Relating ecosystem services to domains of human well‐being: Foundation for a U.S. index, Ecol. Indic., 28, 79–90, doi: 10.1016/j.ecolind.2012.02.032. [DOI] [Google Scholar]
- Sterling, P. , and Eyer J. (1988), Allostasis: A new paradigm to explain arousal pathology, in Handbook of Life Stress, Cognition and Health, edited by Fisher S. and Reason J., pp. 629–649, John Wiley, New York. [Google Scholar]
- Summers, J. K. , Smith L. M., Harwell L. C., Case J. L., Wade C. M., Straub K. R., and Smith H. M. (2014), An index of human well‐being for the U.S.: A TRIO approach, Sustainability, 6, 3915–3935, doi: 10.3390/su6063915. [DOI] [Google Scholar]
- Summers, J. K. , Harwell L. C., and Smith L. M. (2016), A model for change: An approach for forecasting well‐being from service‐based decisions, Ecol. Indic., 69, 295–309, doi: 10.1016/j.ecolind.2016.04.033. [DOI] [Google Scholar]
- Sutton‐Grier, A. E. , Wowk K., and Bamford H. (2015), Future of our coasts: The potential for natural and hybrid infrastructure to enhance the resilience of our coastal communities, economies and ecosystems, Environ. Sci. Pol., 51, 137–148, doi: 10.1016/j.envsci.2015.04.0061462-9011. [DOI] [Google Scholar]
- Thoits, P. A. (2010), Stress and health major findings and policy implications, J. Health Soc. Behav., 51(1 suppl), S41–S53, doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- Torrence, R. , and Grattan J. (2002), Archaeology of disasters: Past and future trends, in Natural Disasters and Cultural Change, edited by Torrence R. and Grattan J., pp. 1–18, Routledge, Abingdon CA and New York. [Google Scholar]
- Tsujiuchi, T. (2015), Mental health impact of the Fukushima nuclear disaster: Posttraumatic stress and psycho‐socio‐economic factors, United Nations University (UNU‐IAS), Fukushima Global Communication Programme, Working Paper Series No. 8, Dec. 2015. 7 pp.
- U.S. Department of Commerce (USDOC) (2013), Economics and statistics administration, economic impact of Hurricane Sandy: Potential economic activity lost and gained in New Jersey and New York, Washington, DC, pp. 35 [Available at http://www.esa.doc.gov/reports/economic-impact-hurricane-sandy.] [Google Scholar]
- U.S. Fish and Wildlife Service (2013), Vision for a health Gulf of Mexico watershed, 24 pp.
- U.S. Environmental Protection Agency (USEPA) (2007), Environmental conditions in northern Gulf of Mexico coastal waters following Hurricane Katrina, /R‐07/063, Office of Research and Development, National Health and Environmental Effects Research Laboratory, Gulf Ecology Division, Gulf Breeze, Florida, 68 pp. [Google Scholar]
- U.S. Environmental Protection Agency (USEPA) (2015), Health impact assessment (HIA) & EnviroAtlas: Integrating ecosystem services into the decision making process, Office of Research and Development, National Health and Environmental Effects Laboratory, Research Triangle Park, NC, EPA/600/RR-15/128. [Google Scholar]
- Varma, R. , and Varma D. R. (2005), The Bhopal disaster of 1984, Bull. Sci. Technol. Soc., 25, 37–45, doi: 10.1177/027046704273822. [DOI] [Google Scholar]
- Vasterman, P. , Yzermans C. J., and Dirkzwager A. J. E. (2005), The role of the media and media hype in the aftermath of disasters, Epidemiol. Rev., 27, 107–114, doi: 10.1093/eoirev/mxi002. [DOI] [PubMed] [Google Scholar]
- Venn‐Watson, S. , et al. (2015), Adrenal gland and lung lesions in Gulf of Mexico common bottle nose dolphins (Tursiops truncatus) found dead following the Deepwater Horizon oil spill, PLoS ONE, 10(5), e0126538, doi: 10.1271/journal.pone.0126538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wachinger, G. , Renn O., Begg C., and Kuhlicke C. (2013), The risk perception paradox—Implications for governance and communication of hazards, Risk Anal., 33(6), 1049–1065, doi: 10.1111/j.1539-6924.2012.01942.x. [DOI] [PubMed] [Google Scholar]
- Warsini, S. , Mills J., and Usher K. (2014), Solastalgia: Living with the environmental damage caused by natural disasters, Prehosp. Disaster Med., 29(1), 87–90, doi: 10.1017/S1049023X13009266. [DOI] [PubMed] [Google Scholar]
- Weems, C. F. , Scott B. G., Banks D. M., and Graham R. A. (2012), Is TV traumatic for all youths? The role of pre‐existing posttraumatic stress symptoms on the link between disaster and stress, Psychol. Sci., 23, 1293–1297, doi: 10.1177/10956797612446952. [DOI] [PubMed] [Google Scholar]
- World Health Organization (1946), Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference, New York, 19–22 June, 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April 1948.
- Wilson, M. J. , Frickel S., Nguyen D., Bui T., Echsner S., Simon B. R., Howard J. L., Miller K., and Wickliffe J. K. (2015), A targeted health risk assessment following the Deepwater Horizon oil spill: Polycyclic aromatic hydrocarbon exposure in Vietnamese‐American shrimp consumers, Environ. Health Perspect., 123(2), 152–159, doi: 10.1289/ehp.1408684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu, J. , Wang Z., Shen F., Ouyang C., and Tu Y. (2016), Natural disasters and social conflict: A systematic literature review, Int. J. Disaster Risk Reduct., 17, 38–48, doi: 10.1016/j.ijdrr.2016.04.001. [DOI] [Google Scholar]
- Yee, S. H. , Bradley P., Fisher W. H., Perreault S. D., Quackenboss J., Johnson E. D., Bousquin J., and Murphy P. A. (2012), Integrating human health and environmental health into the DPSIR framework: A tool to identify research opportunities for sustainable and healthy communities, Ecohealth, 9, 411–426, doi: 10.1007/s10393-012-0805-3. [DOI] [PubMed] [Google Scholar]
- Ylitalo, G. M. , et al. (2012), Federal seafood safety response to the Deepwater Horizon oil spill, Proc. Natl. Acad. Sci. U.S.A., 109(50), 20274–20279, doi: 10.1073/pnas.1108886109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoskowitz, D. , Santos C., Allee B., Carollo C., Henderson J., Jordan S., and Ritchie J. (2010), Proceedings of the Gulf of Mexico ecosystem services workshop: Bay St. Louis, Mississippi, Harte Research Institute for Gulf of Mexico Studies, Texas A&M University, pp. 16. [Google Scholar]
- Yoskowitz, D. W. , Werner S. R., Carollo C., Santos C., Washburn T., and Isaksen G. H. (2016), Gulf of Mexico offshore ecosystem services: Relative valuation by stakeholders, Mar. Policy, 66, 132–136, doi: 10.1016/j.marpol.2015.03.031. [DOI] [Google Scholar]


