Abstract
Close relationships are a resource for mental and physical health that, like other social resources, is unequally distributed in the population. This article focuses on racial disparities in the loss of relationships across the life course. Racial disparities in life expectancy in the United States mean that black Americans experience the deaths of more friends and family members than do white Americans from childhood through later life. I argue that these losses are a unique type of stress and adversity that, through interconnected biopsychosocial pathways, contributes to disadvantage in health over the life course. I focus particularly on how the interconnected pathways associated with loss undermine opportunities for and increase risks to social ties throughout life, adding to disadvantage in health. I call on social scientists and policymakers to draw greater attention to this unique source of disadvantage for black children, adults, and families.
Keywords: bereavement, mental health, racial disparities, social relationships
Close relationships benefit mental health, physical health, and longevity. The evidence for this assertion is strong and indisputable (Holt-Lunstad, Smith, and Layton 2010; House, Landis, and Umberson 1988; Uchino, Cacioppo, and Kiecolt-Glaser 1996). Prospective evidence from developed nations around the world shows that, over a period of years, individuals with higher levels of social involvement are significantly less likely to die than their more socially isolated counterparts, even taking baseline health status into account (House, Landis, and Umberson 1988; Holt-Lunstad, Smith, and Layton 2010). Social ties are certainly a potential resource for health and well-being, but social ties can be a double-edged sword. Strained and conflicted social ties undermine health and well-being (Umberson and Montez 2010) and the loss of close relationships, particularly through death, can be devastating (Stroebe, Schut, and Stroebe 2007). In this article, I emphasize that social ties are a resource for health and well-being that is unequally distributed in the population. Social conditions associated with systems of stratification foster opportunities for forming and sustaining social relationships, as well as imposing constraints, obligations, and risks in relationships (Umberson and Montez 2010). This inequality has been studied most often in relation to gender differences in social ties, but evidence also points to structural conditions that foster greater disadvantage for the social ties of black Americans than for other racial-ethnic groups in the United States (Umberson et al. 2014; Williams and Sternthal 2010).
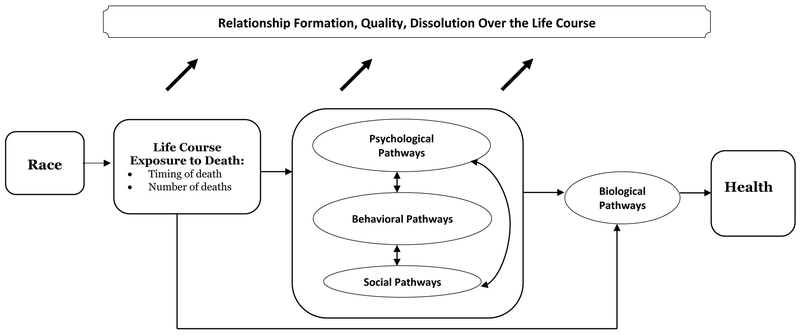
This article focuses specifically on racial disparities in the deaths of friends and family members as a unique cause of lifelong disadvantage in social ties with adverse effects on health and well-being. The historic legacy of racism in the United States is reflected in significant and persistent racial disparities in life expectancy (Williams and Mohammed 2013). These race differences in life expectancy mean that, compared with white Americans, black Americans are exposed to the deaths of more friends and family members throughout life (Umberson et al. 2017). I build on Pearlin’s stress and life course perspective (Pearlin et al. 2005) to argue that these losses have reverberating effects throughout the life course by affecting relationship formation, quality, and dissolution, as well as health, and that this disadvantage begins in childhood. In laying out this argument (summarized in Figure 1 and discussed in detail later in the article), I explain why bereavement and loss constitute a unique stressor that shapes social ties, health, and well-being through interconnected social, psychological, behavioral, and biological pathways. This approach points to repeated relationship losses over the life course as a source of tremendous racial disadvantage in relationships and in the potential benefits of social ties for health and well-being.
Figure 1.
Conceptual Model of Life Course Exposure to Death and Cumulative Disadvantage in Relationships and Health.
THE STRESS AND LIFE COURSE PERSPECTIVE
Pearlin’s classic stress model (Pearlin et al. 1981) provides the scaffolding for understanding the processes through which race differences in death exposures create massive racial disparities in lifelong possibilities for relationships and in overall health and well-being. The stress model emphasizes that socially patterned variation in stressors and resources accumulates over the life course to produce advantage or disadvantage in health (Pearlin et al. 2005). In the United States, this socially patterned variation is most dramatic for race. Race is a structural system of inequality that systematically imposes demands, risks, and stressors—and undermines opportunities and resources—for black Americans (Williams and Mohammed 2013). Higher levels of stress associated with racism and discrimination begin in childhood and continue throughout the life course, adding to cumulative disadvantage in health over time (Geronimus et al. 2006; Williams and Sternthal, 2010). This disadvantage is dramatically illustrated in race differences in life expectancy and mortality risk. The racial disparity in mortality risk across the life course is smaller than it has been at previous points in history but remains significant, especially at younger ages (Geronimus, Bound, and Colen 2011; Hummer and Chinn 2011). Infant mortality remains more than twice as high for black infants as for white infants (Heron 2015), and maternal mortality is more than three times higher for black mothers than for white mothers (Centers for Disease Control and Prevention 2017). Homicide is the leading cause of death for black males aged 15 to 24 and accounts for half of all deaths for this group, compared with 8% of deaths among white males aged 15 to 24 (National Center for Health Statistics 2015). Racial disparities in adult mortality go well beyond homicide statistics and can be seen for almost every leading cause of death (Heron 2015). Racial disparities in mortality are apparent through mid- to later life; up to about age 80, blacks have higher death rates than whites for most leading causes of death, including heart disease, cancer, and diabetes (Heron 2015).
Racial disparities in life expectancy are a national tragedy that goes well beyond the deceased person to reverberate throughout his or her social networks. Central to the life course perspective is a focus on the importance of “linked lives”––that is, close social ties between significant others––for health and well-being over the life course (Elder, Johnson, and Crosnoe 2003). The death of a significant other (e.g., parent, spouse, child) has been identified as the most stressful type of life event that the majority of Americans ever experience and one with lasting effects on health (Stroebe et al. 2007). I argue that racial disparities in exposure to the deaths of friends and loved ones is a unique type of stress for black Americans that not only obliterates important social connections, but also launches a lifelong cascade of psychological, social, behavioral, and biological consequences that undermine other relationships, as well as health, over the life course. This perspective broadens the focus on racial disparities in life expectancy in the United States to include the impact of such disparities on surviving children, adults, and families.
DEATH OF SIGNIFICANT OTHERS AS A UNIQUE LIFE COURSE STRESSOR
The death of a loved one is widely documented as a significant stressor that undermines health (Stroebe et al. 2007). Taking racial disparities in life expectancy into account, I suggest that repeated and early life course exposure to death is a novel type of socially patterned adversity that has lifelong consequences for relationships and health. This is a unique stressor for black Americans in at least five general ways: (1) earlier and more frequent death exposures for black Americans reflect a collective threat and personal vulnerability associated with being black; (2) racial discrimination undermines health, and the lower life expectancy for blacks is an extreme consequence of racism; (3) social relationships are fundamental to human development and health, and black Americans face heightened structural challenges and risks in their relationships, (4) bereavement and loss of relationships have long-term adverse effects on individuals, and black Americans are disproportionately exposed to loss, and (5) such losses occur earlier in the life course for black than white Americans.
Collective Threat and Personal Vulnerability
Most Americans rarely experience the death of someone close to them until mid- to later life. Pulitzer Prize-winning author Ernest Becker (1973) argued that death is so foreign and abstract to most Americans that they easily engage in “denial of death,” allowing them to mindlessly engage in daily activities with little thought or concern about death. The death of someone close to us pierces this denial, forcing us to recognize our own inevitable mortality, as well as that of our loved ones. Becker suggests that without denial of death as a basic psychological defense, panic and chaos would ensue. As long as we are able to view death as exceptional and something that happens to “others,” we can continue to engage in denial. Denial of death for oneself and those we care about is much more difficult when we are repeatedly confronted with the premature deaths of family members, friends, and neighbors—as is the case for many black Americans. The highly visible premature deaths of young black Americans, as underscored in the Black Lives Matter movement, surely further contributes to a sense of collective threat and personal vulnerability (Ross 2011). Indeed, this perceived vulnerability is a real and unique source of stress for black Americans. Moreover, much like mass incarceration, the frequent and highly publicized deaths of young black Americans across the United States, particularly those at the hands of the police, may contribute to a sense of collective trauma that stems from the legacy of slavery and racism in the United States (Eyerman 2004) and likely adds to a sense of personal vulnerability and loss.
Racism and Health
It is well established that the stress of racial discrimination undermines health, and extensive reviews of this evidence are widely available (Geronimus et al. 2006; Williams and Mohammed 2013; Phelan and Link 2015). But the premature deaths of friends and family members may be the most vivid and fearsome illustrations of racial discrimination in the United States (Vargas 2008). Beginning with the colonial-era murders of slaves and public lynchings, racial discrimination has continued into the twenty-first century, as reflected in lower life expectancies for blacks and the strikingly heightened risk of premature and violent death for blacks. Premature death is an ever-present threat in the lives of black Americans, a threat that every black parent is well aware of.
Importance of Relationships for Human Development and Well-being
What does it mean to live with this ever-present threat and to experience the deaths of friends and family members beginning early in the life course? A vast scientific literature points to the importance of relationships for health and well-being (Uchino, Cacioppo, and Kiecolt-Glaser 1996) and to the loss of those relationships as traumatic stressors (Stroebe et al. 2007). Social scientists from diverse disciplines have clearly established that greater involvement in social relationships throughout the life course enhances mental and physical health and promotes longevity through biopsychosocial pathways (House et al. 1988; Uchino et al. 1996). Developmental psychologists emphasize that healthy human development depends on early social connections that foster secure attachment to others and a sense of predictability and mastery (Bowlby 1980; Repetti, Taylor, and Seeman 2002). Disruptions to early social connections through separation or loss interfere with healthy child development and increase the risk of hypervigilance as well as emotional and physical reactivity in response to stress (Repetti et al. 2002). Recent work on child development also suggests that different types of stress (e.g., stress characterized more by threat as compared to deprivation, or perhaps loss) have distinctly different effects on neural development (McLaughin, Sheridan, and Lambert 2014). If black Americans lose significant others early in the life course, then relationship loss is likely to affect numerous facets of child and adolescent development that are carried with them as they grow older.
Bereavement and Health
The effects of bereavement on health and well-being are well-documented and indicate that death of a significant other is often a turning point in the life course that triggers changes in worldviews, views of self, social roles, well-being, and health (Stroebe et al. 2007). Most bereavement research focuses on the deaths of close family members; this research clearly shows that the loss of even one family member undermines mental and physical health and increases mortality risk. These effects are well-documented for the death of a spouse (e.g., Dupre, Beck, and Meadows 2009), a child (e.g., Floyd et al. 2013; Li et al. 2003), a sibling (e.g., Rostila, Saarela, and Kawachi 2012), and a parent (e.g., Guldin et al. 2015; Umberson 2003), and the available evidence indicates that such effects are apparent many years after the loss. The bereavement literature also suggests that loss often strains survivors’ relationships with others (Rogers et al. 2008; Umberson 2003). Since one family member death adversely affects both children and adults, additional losses are likely to add to this disadvantage. Stroebe and colleagues (2007) report that having experienced a prior loss may increase health risks following bereavement. However, very few studies have considered the effects of multiple losses, and those that have done so have been restricted to non-representative samples of veterans who lost unit members in combat (Toblin et al. 2012) and gay men who lost close friends to AIDS (Springer and Lease 2000); these studies suggest that multiple losses in adulthood are likely to increase mental and physical health costs. The bereavement literature also indicates that certain types of loss and certain causes of death are more traumatic than others, with unexpected, violent, and premature (earlier than expected) losses as most traumatic (Stroebe et al. 2007); each of these circumstances of loss is more common for black than for white Americans.
Life Course Timing of Loss
Life course timing of loss may be critical to understanding the long-term health consequences of loss. If loss occurs during sensitive periods of development, the consequences are likely to be stronger and longer-lasting (Braveman and Barclay 2009; Shonkoff et al. 2012). Substantial evidence shows that childhood and adolescence are particularly vulnerable periods, during which stress is likely to have lasting effects on biopsychosocial pathways that affect health (Braveman and Barclay 2009; Miller, Chen, and Parker 2011; Repetti et al. 2002; Shonkoff et al. 2012). Major stress exposure during these sensitive periods contributes to lifelong patterns of emotional and physiological arousal that undermine health (Braveman and Barclay 2009; Shonkoff et al. 2012). A significant stressor, such as the death of a loved one early in the life course, may also lead to a psychological state of hypervigilance in anticipation of new threats (losses), as well as maladaptive behavioral strategies (e.g., self-medication with drugs or alcohol) for reducing emotional and physical arousal. These patterns of arousal and response to arousal undermine physical health over time. Danese and McEwan (2012) describe a process of “biological embedding” of vulnerability such that adverse childhood experiences have lasting effects on biological systems that affect health over the life course (Braveman and Barclay 2009; Shonoff et al. 2012). In addition to lifelong patterns of emotional and physiological arousal, subsequent losses may reactivate and exacerbate patterns of emotional and physical dysregulation and arousal that add to disadvantage over time. Although early losses may have the strongest effects on increased vulnerability, loss at any point in life can trigger system dysregulation, adding to disadvantage in health.
EVIDENCE FOR RACIAL DISPARITIES IN RELATIONSHIP LOSS
The first important question to ask is whether there are racial disparities in exposure to death and in the timing of death exposures over the life course. This section presents the evidence for such disparities.
Death of Family Members
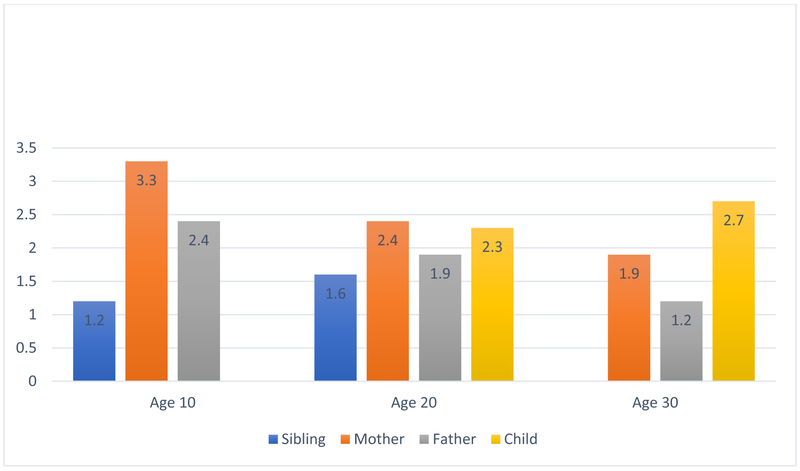
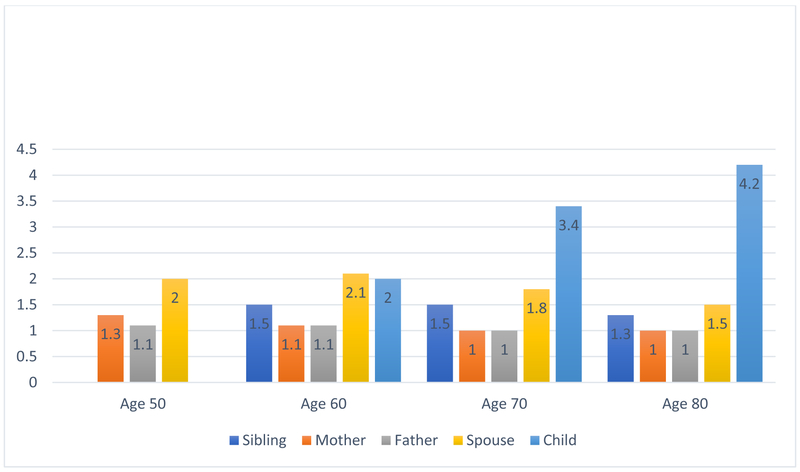
Several colleagues and I recently estimated non-Hispanic black–white differences in exposure to the deaths of mothers, fathers, siblings, children, and spouses using four data sets that are representative of the U.S. population (see detailed results in Umberson et al. 2017). We analyzed two data sets that include younger age cohorts and two that include older age cohorts. The pattern of results was similar across data sets. Figure 2 summarizes general patterns of loss for deaths occurring by age 30 in the National Longitudinal Study of Youth 1997 (NLSY97), and Figure 3 summarizes such patterns for deaths occurring by age 80 in the Health and Retirement Study (HRS). These figures show the relative risk of specific types of loss for blacks compared with whites at different ages (results are based on nonparametric life table results; see Umberson et al. 2017 for details). The overall pattern of results is dramatic: black Americans are at greater risk of experiencing the death of a mother, father, sibling, spouse, and child than are white Americans. For example, Figure 2 shows that black children were more than three times as likely as white children to lose a mother by age 10 (2% of black respondents, .06% of white respondents), and black adults were more than 2.5 times as likely as white adults to lose a child by age 30 (4.9% of black respondents, 1.8% of white respondents). Figure 3 shows that black respondents were more than twice as likely to lose a spouse by age 60 (10.5% of black respondents, 4.9% of white respondents) and four times more likely to lose a child when respondents were between the ages of 50 and 80 (10.4% of black respondents and 2.5% of white respondents; these statistics do not include information on deaths of children before respondents were 50 and thus underestimate the total number of respondents who have experienced the death of a child). For additional information on prevalence of loss of specific family members across the life course, see Umberson et al. 2017.
Figure 2.
Relative Risk of Loss for Black Americans Compared to White Americans by Age 30 (National Longitudinal Study of Youth 1997).
Figure 3.
Relative Risk of Loss for Black Americans Compared to White Americans, Age 50–80 (Health and Retirement Study 1992–2012)a.
Note: aDeath of sibling and death of child were assessed only at age 50 and older in the Health and Retirement Study.
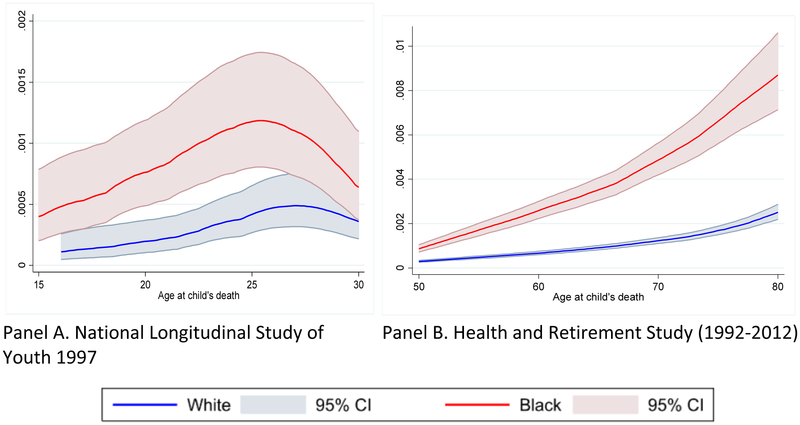
Our more detailed analysis of the timing of life course losses (Umberson et al. 2017) confirms that black Americans also experienced losses earlier in the life course than white Americans did. For example, we found in the NLSY97 that, “compared with whites, blacks were at greater risk of losing a mother from early childhood through young adulthood, losing a father through their midteens, losing a sibling in their teens, and losing a child through their late twenties” (Umberson et al. 2017:917). In the HRS data, “the race gap in the age-specific hazard of exposure to death of a mother, father, spouse, and sibling is apparent at most ages until later in life,” at which point whites begin to lose more family members (Umberson et al. 2017:917). Perhaps most striking, the race gap in the hazard of exposure to death of a child continued to grow with advancing age, as illustrated in Figure 4. Whereas the race gap in exposure to other family member losses diminished with advancing age, Figure 4 shows that the race gap in loss of a child grew through the early life course (to age 25, as shown in Panel A, NLSY97) and continued to diverge from mid- to later life (for deaths occurring after age 50 and up to age 80, as shown in Panel B, HRS). Given the scientific evidence as well as the general lay belief that the death of a child is the most devastating kind of loss that adults can experience, this racial disparity is extraordinary. Moreover, the loss of a parent is generally considered the most devastating kind of loss that a child can experience (Guldin et al. 2015; Stroebe et al. 2007), and we find that the greatest racial disparity in the early life course is for death of a mother (see Figure 2 and Umberson et al. 2017).
Figure 4.
Age-specific Hazard of Child Death for Blacks and Whites (Shown with 95% Confidence Intervals).
Note: Figure adapted from Umberson et al. 2017.
In sum, population-level data make it clear that blacks lose mothers, fathers, siblings, and children earlier in the life course than whites do. Moreover, we found clear evidence that blacks experienced greater cumulative exposure to family member deaths. For example, in the NLSY97, blacks were three times more likely than whites to have experienced the death of two or more family members by age 30, and in the HRS, blacks were almost twice as likely to have lost four or more family members by age 60, even after controlling for variables known to increase risk (Umberson et al. 2017).
Other Losses
The available data have allowed us to assess deaths of parents, children, spouses, and siblings, but racial disparities in death exposure likely go well beyond these family members to include extended kin, friends, and community members. For example, black children are more likely than white children to be raised by grandparents (Baker, Silverstein, and Putney 2008), who are also at elevated mortality risk due to racial disparities in life expectancy. Smith (2015) has focused on the high rates of homicide in certain urban areas and described the grief that young black men experience following the violent deaths of close friends and relatives. Future research should estimate race differences in the full extent of death exposures over the life course.
RACE, DEATH EXPOSURES, AND PATHWAYS TO HEALTH AND WELL-BEING
The model presented in Figure 1 conceptualizes how death exposures shape the interconnected pathways that create cumulative disadvantage in social connections and health over the life course. This model asserts that (1) death of significant others is more common and occurs earlier in the life course for blacks than whites; (2) death exposures shape the integrated biopsychosocial pathways that lead to poor health; and (3) at each stage of the model, death exposures further diminish resources associated with social relationships. This section describes each of this model’s major components in turn.
Race and Life Course Exposure to Loss
One of Pearlin’s greatest contributions to the study of stress was to articulate how social conditions associated with one’s position in the social structure shape access to resources and exposure to stress (Pearlin et al. 2005). Substantial evidence shows that structural conditions associated with segregation and discrimination expose black Americans to more stress and fewer resources throughout life, a combination that, in turn, erodes health and increases mortality risk (Phelan and Link 2005; Williams and Sternthal 2010). Here, I focus specifically on how race differences in life expectancy constitute a unique stressor for survivors that may launch a lifelong cascade of adversity that further depletes resources and increases stress. This first component of Figure 1 is grounded in research showing that black Americans experience more and earlier exposure to the death of significant others than white Americans do (Umberson et al. 2017).
Interconnected Pathways
Figure 1 suggests that life course exposures to death activate pathways that operate in tandem and unfold over years and decades to influence racial disparities in health and well-being. Figure 1 shows four broad pathways—psychological, social, behavioral, and biological—that link death exposures to disadvantage in health. Each of these pathways (e.g., psychological distress, health behavior) is an important outcome in and of itself, perhaps particularly among younger cohorts for whom long-term health disadvantage in chronic and disabling health conditions is not yet apparent. These pathways are particularly significant mechanisms of developmental vulnerability and risk in childhood, adolescence, and emerging adulthood, and this early developmental vulnerability shapes social relationships throughout the life course (indicated by arrows broadly linking loss to social relationships over the life course, shown across the top of Figure 1), as well as long-term health. Stress affects health through each of these pathways—psychological, behavioral, social, and biological (see overviews in Miller, Chen, and Parker 2011; Shonkoff, Boyce, and McEwen 2009). Below, I suggest specific ways that early and multiple death exposures may shape the biopsychosocial and behavioral pathways that contribute to health and well-being; a later section describes the implications of such death exposures for social connections over the life course. Death exposures activate these pathways much as other stressful life events do but in a heightened fashion, due to the unique and extreme stress that the death of significant others creates, especially when those deaths occur earlier than expected and when multiple losses occur over the life course.
Psychological and Cognitive Pathways
The death of a significant other is a turning point that causes emotional arousal and psychological disruption. The death of a significant other at any point in the life course is associated with increased psychological distress and anxiety (Stroebe et al. 2007). Loss may also undermine the sense that one has the power to control life circumstances, disrupt the sense that the world is a just place where one gets what one deserves and deserves what one gets, increase a sense of vulnerability and collective threat to one’s own and loved ones’ safety (Ross 2011), and increase hypervigilance—the state of being always on the alert for new threats (Repetti et al. 2002; Smith 2015). These psychological effects are also interrelated—for example, diminished personal control may add to feelings of distress and anxiety. Losses that occur during sensitive periods early in the life course may have more dramatic and lasting consequences for these psychological pathways, consequences that are further exacerbated by subsequent losses. The stress of multiple, premature losses may also have lifelong effects on cognitive capacity. Distress may make it more difficult for bereaved children to focus in class or to attend school (Sharkey 2010), with effects on long-term educational outcomes (interconnected social pathways), which are, in turn, strongly associated with health and longevity (Montez et al. 2011). As people age, a life course history of multiple death exposures may be associated with an earlier and more rapid decline in cognitive functioning and accelerated cognitive impairment (through interconnected biopsychosocial pathways; Norton et al. 2009).
The psychological and cognitive pathways most activated by loss may vary for black and white Americans. For example, the available evidence suggests that while stress and discrimination are more pervasive for black than white Americans, psychological distress and depression is at about the same level (or even lower) for black Americans (McGuire and Miranda 2008). Thus, racial disparities in exposure to loss may be expressed less often in psychiatric disorders and more often in symptoms that do not meet criteria for diagnosis (McGuire and Miranda 2008). Another possibility is that loss activates psychological pathways less and behavioral or biological pathways more for black Americans compared with white Americans (Jackson, Knight, and Rafferty 2010). These possibilities are all important nuances to be investigated in future studies and may contribute to our understanding of race differences in the effects of stress and loss.
Behavioral Pathways
Health behaviors contribute significantly to overall health and longevity throughout the life course (Health Policy Brief 2014). Loss may affect health behaviors in four general ways. First, in response to emotional upset and distress, people may engage in health behaviors that are distracting or soothing (not necessarily through a conscious strategy) by self-medicating with drugs and alcohol or self-comforting with overeating (Umberson, Liu, and Reczek 2008). Second, the bereaved may take behavioral risks (e.g., risky sexual behavior, fighting, reckless driving) because they care less about their own safety and survival after losing someone they care about; this is suggested by research linking bereavement to passive suicidal ideation (Stroebe, Stroebe, and Abakoumkin 2005). Moreover, premature losses may lead to a sense of futility about efforts to postpone one’s own death, partly by undermining a sense of personal control—an interconnected psychological pathway. Indeed, emerging evidence suggests that early and multiple life course losses reduce subjective life expectancy throughout the life course (Donnelly, Umberson, and Pudrovska 2017).
Third, the trauma of loss disrupts some behaviors that individuals have little control over, such as sleep patterns and healthy eating. Recent research shows that the daily strains of racial discrimination disrupt sleep patterns, contributing to black Americans’ disproportionate cardiovascular and metabolic illnesses; this work identifies interconnected behavioral and physiological pathways linking racial discrimination to health (Goosby, Straley, and Cheadle 2017). Racial disparities in exposure to loss may trigger significant and lasting changes in sleep patterns and in other health behaviors that undermine health over time. Finally, significant others often influence health behaviors through social control, and the loss of key social ties may mean the loss of this potentially positive influence (Umberson 2003). For adolescents, for example, the loss of a parent may mean less deterrence of alcohol and drug use.
Health behavior trajectories are set in motion early in life, and family members play a key role in shaping those trajectories in childhood (Umberson et al. 2010). Parents and siblings are highly influential in establishing health habits in childhood, and close peers begin to play a more influential role in adolescence. In adulthood, intimate partners and children influence health behaviors. Because behavioral proclivities form in childhood, adolescence, and emerging adulthood, loss may have greater and more lasting effects on health behaviors during these periods of the life course. Moreover, because the impact of health behaviors on health accumulates over the life course, early disadvantage in health behaviors means more cumulative disadvantage in health over the entire life course. Death exposures at any point in the adult life course may also trigger turning points in health behaviors, and losses in adulthood may exacerbate or compound the effects of earlier losses.
Social Pathways
Death exposures also undermine health by altering social pathways, including not only social relationships, but also socioeconomic status and other social stressors. Pearlin described how stressful life events alter an individual’s social environment in ways that lead to additional chronic stressors and stressful life events, a process referred to as “stress proliferation” (Pearlin et al. 2005). Stress proliferation is common following the death of a significant other; for example, a death in the family may lead to new financial strains, caregiving responsibilities, and social roles and responsibilities (Stroebe, Schut, and Stroebe 2007). The death of a parent may mean the loss of family wages, new responsibilities for older siblings to care for younger siblings, moving to a less expensive and less desirable neighborhood, or changing schools. The death of a parent early in the life course may interfere with success in school, which then reduces future socioeconomic success (SES; Sharkey 2010). In turn, decreased SES, increased neighborhood stress, and a cascade of stressful life events and chronic strains erode health and well-being. One of the most significant social pathways concerns the effects of loss on social ties. I devote specific attention to this pathway after a brief description of biological pathways.
Biological Pathways
Stressful events and chronic stress affect health through well-documented biological processes (Danese and McEwan 2012; Miller, Chen, and Parker 2011; Shonkoff et al. 2012). Perceived stress activates a physiologic response that, if prolonged, leads to dysregulated cardiovascular, immune, and endocrine functioning and increased allostatic load (cumulative wear and tear on physiological systems resulting from stress exposure) that then accelerates biological aging and undermines health (Danese and McEwan 2012). Through this process, traumatic life events and subsequent stress proliferation add to cumulative disadvantage in health over time. As Figure 1 suggests, the psychological, behavioral, and social consequences of bereavement contribute to biological responses to stress. For example, the psychological responses of hypervigilance and emotional reactivity may contribute to cardiovascular dysregulation, the behavioral responses of heavy drinking and overeating may contribute to endocrine dysregulation, and the social response of isolation may contribute to immune dysregulation through increased inflammation.
Social Ties
Central to the conceptual model in Figure 1 is the premise that death exposures weaken the potential for social connection over the life course (indicated by the arrows across the top of the figure). Pathways of risk ultimately intersect to erode social connections as a resource that promotes health and well-being throughout life. Research is needed to identify the specific linkages of loss to social connection, but current theory and research point to several key processes that are likely to increase strain in relationships, create barriers to the formation and stability of relationships, diminish access to supportive social ties, and increase the risk of social isolation. I am not suggesting that loss makes people care less about social connection; on the contrary, loss may trigger a stronger desire and need for social connection.
The first and most obvious hit to social ties is the death itself—the literal and irrevocable loss of a significant other. But this loss activates intersecting pathways that further erode social ties. Through psychological pathways, the bereaved may approach relationships in ways that diminish opportunities for support and connection. The development of secure attachment to others from childhood through young adulthood is especially important for the formation and stability of relationships in adulthood as well as for lifelong psychological well-being (Repetti et al. 2002). Early losses may lead to insecure attachment patterns that interfere with relationships in adulthood (Repetti et al. 2002), reducing opportunities for supportive social ties throughout life. Of course, at any point in adulthood, the distress and anxiety (additional psychological pathways) that follow a loss are likely to contribute to relationship strain and dissolution; this is suggested in studies showing increased risk for marital strain following the death of a child (Rogers et al. 2008) or parent (Umberson 2003). Even apart from distress, the effects of loss on views of self and worldviews are likely to undermine social ties, further depleting important resources from social connections. For example, hypervigilance and emotional reactivity resulting from early and multiple losses may lead to strain in adult relationships (Repetti et al. 2002). A sense of vulnerability and inability to control life’s circumstances, including the safety of loved ones, may lead the bereaved person to avoid forming new relationships and increase social isolation throughout adulthood (Umberson et al. 2015).
Loss may also interfere with social ties through social pathways in the form of stress proliferation. For example, when the loss of a significant other results in financial strain, problems at school or work, and neighborhood or residential transitions, these new sources of stress add to the already substantial strains of loss. All these new sources of stress further interfere with the formation, stability, and quality of social ties. Each family member may be affected by the loss in ways that create new, unique strains for each of the other family members. In an example of the intersection of social and psychological pathways to poor health, the stress associated with widowhood, single parenting, or financial strain may affect a surviving parent’s mental health and ability to parent, with adverse consequences for children (Melhem et al. 2011). Behavioral and social pathways to poor health may intersect if older siblings and other family members turn to drugs or alcohol to alleviate their own distress. In these ways, adult caregivers and siblings may become less supportive and less available, their relationships with bereaved youths may become more strained, and youth may become more socially isolated. Again, it is not that individuals who have experienced loss do not desire social connection. In fact, recent qualitative research suggests that this desire may lead to repeated attempts to form meaningful intimate relationships beginning early in the life course, but these relationships are at high risk for additional stress and dissolution (Umberson et al. 2015).
Loss may also interfere with the quality and stability of social ties through behavioral pathways, including health behaviors and risk-taking behaviors, perhaps especially drug and alcohol use. As an example of interconnected social and behavioral pathways, self-medication and risk-taking behaviors impose strain on relationships with others––especially parents, intimate partners, and children––potentially leading to additional relationship losses through divorce, breakups, and loss of contact (Umberson et al. 2015). Behavioral and social pathways intersect again when the loss of significant others means the loss of positive social influences that might prevent health-compromising behaviors and promote health-enhancing behaviors.
In sum, the impact of early and repeated losses on social, psychological, and behavioral pathways can lead to lifelong risks and the loss of the resources offered by social relationships, further adding to disadvantage over the life course. Although some types of evidence are inconsistent (see Sarkisian and Gerstel 2004), a significant body of evidence points to several types of disadvantage that black Americans face in social ties, including more strain in adult relationships (Umberson et al. 2014), less support from relationships (Ferraro and Koch 1994), lower levels of marital quality (Broman 2005; Bulanda and Brown 2007), higher risk of divorce (Bulanda and Brown 2007), and higher levels of social isolation (McPherson, Smith-Lovin, and Brashears 2006) compared with white Americans. The significantly greater exposure of black Americans to the deaths of significant others throughout the life course may lead to disadvantage in social ties that adds to cumulative disadvantage in health over the life course. Future studies should determine whether the deaths of loved ones, beginning in childhood, contribute to life course disadvantage in social relationships.
Intersecting Pathways
Intersecting pathways in Figure 1 may contribute to racial disparities in social ties and health in two basic ways. First, blacks are more likely than whites to experience accumulated and earlier exposures to death, and, acting through integrated social, behavioral, psychological, and biological pathways, these exposures may increase black Americans’ relative disadvantage in health. Second, and in addition to relative disadvantage, there may be race differences in the impact of death exposures on specific pathways. Moreover, the linkage between loss and health may be better explained by complex interconnections among multiple pathways than by a single mechanism, and these interconnections may affect lifelong relationship patterns that may also differ by race. Bereavement may be more likely to activate behavioral risks for blacks than whites, particularly among men—an example of differences in behavioral pathways (Jackson, Knight, and Rafferty 2010). In an example of the interaction of psychological and biological pathways, a tendency to socially isolate in response to previous death exposures may also elevate psychological distress, which, in turn, precipitates heart disease by increasing chronic inflammation (Howren, Lamkin, and Suls 2009). Blacks, particularly men, may be more likely than whites to socially isolate in response to stress—a difference in social pathways (Umberson et al. 2015). Behavioral pathways may exacerbate this effect if health behaviors create strain in ongoing social relationships and lead to additional relationship losses and social isolation. Taken together, these patterns may make black Americans more vulnerable than white Americans to the effects of prior death exposures on heart disease via the biological pathway of chronic inflammation.
The main point is that early and repeated exposures to loss activate multiple and intersecting life course pathways that add to disadvantage in social connections and health throughout the life course—and this disadvantage is disproportionately experienced by black Americans, beginning in childhood.
OTHER IMPORTANT CONSIDERATIONS
Gender
The impact of loss is likely to differ for men and women because of gender differences in relationships, health outcomes, and the possible mediating pathways. For example, the close relationships of men and women differ in both structure (e.g., marital status, social networks) and content (e.g., stress levels and support given/received; Umberson et al. 2014), suggesting different experiences of relationship loss. Various types of evidence suggest that the pathways linking loss to health also differ for men and women. For example, psychological pathways may diverge because women are more likely than men to experience psychological distress in response to stress (Rosenfield and Mouzon 2013). Behavioral pathways may differ because men are more likely than women to increase alcohol consumption whereas women are more likely to gain weight in response to stress (Umberson et al. 2008). Social pathways may differ because men are more likely to withdraw from social relationships in response to stress while women are more likely to seek social connection and support and to have supportive non-kin relationships, which may help ameliorate the impact of loss on women (Taylor et al. 2000). Yet women are also more likely than men to provide care to others (Pinquart and Sorenson 2006), and the need for potentially stressful family caregiving is likely to increase following loss. The gendered nature of relationships and loss may further differ by race. For example, the gender gap in relationship support and stress is greater among blacks than among whites, and the impact of relationship strain on health explains the race gap in self-rated health of men but not women (Umberson et al. 2014). Such findings point to the importance of future studies that consider the intersection of gender and race in the experiences and consequences of loss.
Other Vulnerable Populations
I have focused on non-Hispanic black–white differences in relationship loss across the life course, but disparities in relationship loss must also be considered for other populations at risk, including native populations. Life expectancy is lower for American Indian and Alaskan Native populations than for black Americans (Shiels et al. 2017). Moreover, while the life expectancy of blacks has improved over the past two decades, the life expectancy of native populations has declined during this period (Shiels et al. 2017). The national media and scholars have drawn a great deal of attention to rising death rates among middle-aged whites in the United States (e.g. Case and Deaton 2015), particularly less educated whites and partly due to the opioid epidemic. However, little attention has been directed to the rising mortality rates of native populations, which are already characterized by the lowest life expectancy of all racial and ethnic groups in the United States (Shiels et al. 2017). Like black Americans, native communities in the United States have a historic legacy of trauma and loss, and this history of loss combined with contemporary life expectancy patterns is likely to have a significant impact on individuals, families, and communities (Evans-Campbell 2008). Communities characterized by the lowest levels of life expectancy are those whose members experience the greatest loss of friends and family members over the life course. The U.S. communities most affected by the opioid crisis—for example, Appalachia—also warrant attention for greater exposure to multiple losses. The conceptual model proposed in this paper should apply to any population at risk of loss. Future research should identify specific and varied populations at high risk of loss and document the patterns and consequences of loss for those populations.
Geography
Geographic concentration of loss draws attention to communities at high risk but also raises questions about whether racial and ethnic variation in loss is apparent within communities or is greater in certain geographic contexts (Massey 2017). U.S. life expectancy varies across regions, states, and neighborhoods. For example, life expectancy is lower in the South than non-South, in neighborhoods characterized by higher levels of poverty and population density, and in states whose economics and infrastructure are relatively weak (Geronimus et al. 2011; Massey 2017; Montez, Zajacova, and Hayward 2016). One new study has begun to address this issue, finding that black–white racial disparities in family member deaths are greater for young people in the non-South than the South, perhaps because whites are more economically disadvantaged in the South than in the non-South, which increases their risk relative to blacks (Olson and Umberson 2017). This study also finds that racial disparities in loss are greater for young blacks in urban than in non-urban areas. Berman and colleagues (2015) point to the possibility that death of a parent or caregiver may contribute to residential instability and homelessness for youth and might mean transitioning to more unstable and dangerous geographic areas following loss. Future research should further clarify how racial and ethnic disparities in exposure to loss vary across geographic contexts and how loss affects geographic relocation.
Hispanic Paradox
Despite their relatively lower levels of education and income, the life expectancy of Latinos is modestly higher than that of non-Hispanic whites and significantly higher than that of non-Hispanic blacks in the United States (Heron 2015). This raises the possibility that Latinos have about the same exposure to the death of family members as whites and much less exposure than blacks, which may contribute to the relatively favorable health profile of U.S. Latinos, despite their poorer socioeconomic status relative to whites. In addition, evidence suggests that Latinos are more family oriented than whites or blacks (Landale, Oropesa, and Bradatan 2006). Stronger kin networks characterized by less loss may protect Latinos’ health. Future research should consider whether and how family ties and racial and ethnic differences in family member loss help explain the Hispanic paradox.
Next Steps
Throughout this article, I have suggested directions for future research. Next steps also include attention to theory, data, policy, and practice. I have drawn on social psychological perspectives to suggest how structural conditions associated with race affect individuals’ social connections, relationship losses, health, and well-being. Diverse theoretical perspectives on the causes and consequences of racial disparities in loss can help frame new research in this area and address policy concerns. Perspectives that bridge micro- and macro-levels of analysis will be particularly useful in this endeavor. The kinds of data and methods that are brought to bear should also be diverse. Documentation of disparities in loss and the consequences of loss require large, representative data sets with substantial numbers of individuals from groups that are often underrepresented in large-scale surveys (e.g., diverse racial-ethnic groups and both men and women). Understanding the pathways through which loss affects health and well-being also requires data sets with sophisticated measures of psychological processes (e.g., distress, anxiety, trauma, anger, personal control), behavioral processes (e.g., alcohol consumption, drug use, risk-taking), social processes (e.g., socioeconomic status, children’s school experiences, relationships, and social connections), and biological processes (e.g., immune, cardiovascular, and metabolic functioning; allostatic load). Such measures are needed to assess the interconnected pathways illustrated in Figure 1 and described throughout this article. At the same time, ethnographic and qualitative data are needed to dig deeply into the meanings and experiences of loss for individuals, families, and communities, with attention to diverse populations at high risk of loss. Beyond basic research and theory, scholarship on this topic must attend to the need for translation of research into concrete strategies for policymakers, politicians, and practitioners who will work to bring attention to the disparities of loss and to reduce those disparities.
CONCLUSION
It is difficult to imagine a more traumatic experience than the death of a loved one, particularly an unexpected and premature death—a view well supported by empirical evidence (Stroebe et al. 2007). Racial disparities in life expectancy are one of the most egregious consequences of racism that one can imagine. But the consequences are even more vast when we consider their reverberating effects throughout the social networks of the deceased. Black Americans are more likely than white Americans to experience the premature death of mothers, fathers, siblings, children, and other relatives and friends. These disparities begin in childhood and are repeated throughout the life course in ways that likely contribute to accumulating disadvantage in health and well-being throughout life. A central premise of this article is that this disadvantage results from a complex interplay of psychological, social, behavioral, and biological sequelae that further undermine social relationships as a potential resource for health and well-being throughout the life course. These interconnected sequelae contribute to strain in surviving social relationships, interfere with the formation of close social ties, increase social isolation, increase the risk of relationship dissolution, and diminish opportunities for supportive social ties.
Racial disparities in exposure to premature deaths are life course flashpoints in a racist society—flashpoints that are highly likely to trigger change in biopsychosocial and behavioral pathways to health, as well as lifelong opportunities for close and salutary social ties that benefit health. Scholarly work on collective trauma also points to the potential impact of racial and ethnic disparities in death exposures on community members who have not directly experienced personal losses (Alexander et al. 2004; Eyerman 2004). While trauma disrupts communities and the lives of individuals, collective trauma may also bind communities together in ways that promote social action (Alexander et al. 2004), as in the Black Lives Matter movement. Basic research and policies that address racial and ethnic disparities in loss, along with social and political action, have the power to disrupt a vicious loop of life course stress and loss that likely undermines social connections, health, and well-being across generations—a pattern that is currently a fact of life for black children and families.
REFERENCES
- Alexander Jeffrey C., Eyerman Ron, Giesen Bernard, Smelser Neil J., and Sztompka Piotr. 2004. Cultural Trauma and Collective Identity. Berkeley: University of California Press. [Google Scholar]
- Baker Lindsey A., Silverstein Merril, and Putney Norella M.. 2008. “Grandparents Raising Grandchildren in the United States: Changing Family Forms, Stagnant Social Policies.” Journal of Societal and Social Policy 7:53–69. [PMC free article] [PubMed] [Google Scholar]
- Becker Ernest. 1973. The Denial of Death. New York: Free Press. [Google Scholar]
- Berman Leslie R., Snow Rachel C., Moorman Jessica D., Policicchio Deena, Geronimus Arline T., and Padilla Mark B.. 2015. “Parental Loss and Residential Instability: The Impact on Young Women from Low-income Households in Detroit.” Journal of Child and Family Studies 24(2):416–26. [Google Scholar]
- Bowlby John. 1980. Attachment and Loss. Vol. 3 New York: Basic Books. [Google Scholar]
- Braveman Paula, and Barclay Colleen, 2009. “Health Disparities Beginning in Childhood: A Life-course Perspective.” Pediatrics 124(Supplement):S163–75. [DOI] [PubMed] [Google Scholar]
- Case Anne, and Deaton Angus. 2015. “Rising Morbidity and Mortality in Midlife among White Non-Hispanic Americans in the 21st Century.” Proceedings of the National Academy of Sciences 112(49):15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2017. “Reproductive Health, Pregnancy Mortality Surveillance System.” Retrieved October 6, 2017, (https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html).
- Danese Andrea, and McEwen Bruce S.. 2012. “Adverse Childhood Experiences, Allostasis, Allostatic Load, and Age-related Disease.” Physiology & Behavior 106(1):29–39. [DOI] [PubMed] [Google Scholar]
- Donnelly Rachel, Umberson Debra, and Pudrovska Tetyana. 2017. “Race Differences in Family Death Exposures and Subjective Life Expectancy” Presented at the annual conference of the Population Association of America, Chicago, IL. [Google Scholar]
- Dupre Matthew E., Beck Audrey N., and Meadows Sarah O.. 2009. “Marital Trajectories and Mortality among U.S. Adults.” American Journal of Epidemiology 170(5):546–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder Glen H. Jr., Johnson Monica K., and Crosnoe Robert. 2003. “The Emergence and Development of Life Course Theory” Pp. 3–19 in Handbook of the Life Course, edited by Mortimer JT and Shanahan MJ. New York: Kluwer Academic/Plenum Publishers. [Google Scholar]
- Evans-Campbell Teresa. 2008. “Historical Trauma in American Indian/Native Alaska Communities: A Multilevel Framework for Exploring Impacts on Individuals, Families, and Communities.” Journal of Interpersonal Violence 23(3):316–38. [DOI] [PubMed] [Google Scholar]
- Eyerman Ron. 2002. Cultural Trauma: Slavery and the Formation of African American Identity. Cambridge: Cambridge University Press. [Google Scholar]
- Geronimus Arline T., Hicken Margaret, Keene Danya, and Bound John. 2006. “‘Weathering’ and Age Patterns of Allostatic Load Scores among Blacks and Whites in the United States.” American Journal of Public Health 96(5):826–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus Arline T., Bound John, and Colen Cynthia G.. 2011. “Excess Black Mortality in the United States and in Selected Black and White High-poverty Areas, 1980–2000.” American Journal of Public Health 101(4):720–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goosby Bridget J., Straley Elizabeth and Cheadle Jacob E.. 2017. “Discrimination, Sleep, and Stress Reactivity: Pathways to African American–White Cardiometabolic Risk Inequities.” Population Research and Policy Review. Retrieved October 5, 2017 (doi: 10.1007/s11113-017-9439-z). [DOI] [Google Scholar]
- Guldin Mai-Britt, Li Jiong, Pedersen Henrik S., Obel Carsten, Agerbo Esben, Gissler Mika, Cnattingius Sven, Olsen Jorn and Vertergaard Mogens. 2015. “Incidence of Suicide among Persons Who had a Parent Who Died during Their Childhood: A Population-based Cohort Study.” Journal of the American Medical Association Psychiatry 72(12):1227–34. [DOI] [PubMed] [Google Scholar]
- Floyd Frank J., Seltzer Marsha M., Greenberg Jan S., and Song Jieun. 2013. “Parental Bereavement during Mid-to-later Life: Pre-to-post Bereavement Functioning and Intrapersonal Resources for Coping.” Psychology and Aging 28(2):402–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Policy Brief. 2014. “The Relative Contribution of Multiple Determinants to Health Outcomes.” Health Affairs, August 21. [Google Scholar]
- Heron Melonie. 2015. “Deaths: Leading Causes for 2012” Pp. 1–93 in National Vital Statistics Report. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Julianne Holt-Lunstad, Smith Timothy B., and Layton J. Bradley. 2010. “Social Relationships and Mortality Risk: A Meta-analytic Review.” PLoS Medicine 7(7):e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House James S., Landis Karl R., and Umberson Debra. 1988. “Social Relationships and Health.” Science 241(4865):540–45. [DOI] [PubMed] [Google Scholar]
- Howren MB, Lamkin DM, and Suls J. 2009. “Associations of Depression with C-reactive Protein, IL-1, and IL-6: A Meta-analysis.” Psychosomatic Medicine 71(2):171–86. [DOI] [PubMed] [Google Scholar]
- Hummer Robert A., and Chinn Juanita J.. 2011. “Race/Ethnicity and US Adult Mortality.” Du Bois Review: Social Science Research on Race 8(1):5–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson James S., Knight Katherine M., and Rafferty Jane A.. 2010. “Race and Unhealthy Behaviors: Chronic Stress, the HPA Axis, and Physical and Mental Health Disparities over the Life Course.” American Journal of Public Health 100(5):933–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landale Nancy S., Oropesa R. Salvador, and Bradatan Christina. 2006. Hispanic Families in the United States: Family Structure and Process in an Era of Family Change” Pp. 138–78 in Hispanics and the Future of America, edited by Tienda M and Mitchell F. Washington, DC: National Research Council of the National Academies. [Google Scholar]
- Li Jiong, Precht Dorthe Hansen, Mortensen Preben Bo, and Olsen Jorn. 2003. “Mortality in Parents after Death of a Child in Denmark: A Nationwide Follow-up Study.” The Lancet 361(9355):363–67. [DOI] [PubMed] [Google Scholar]
- Massey Douglas S. 2017. “Why Death Haunts Black Lives.” Proceedings of the National Academy of Sciences 114(5):800–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire Thomas G., and Miranda Jeanne. 2008. “New Evidence Regarding Racial and Ethnic Disparities in Mental Health: Policy Implications.” Health Affairs 27(2):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin Katie A., Sheridan Margaret A., and Lambert Hilary K.. 2014. “Childhood Adversity and Neural Development: Deprivation and Threat as Distinct Dimensions of Early Experience.” Neuroscience and Biobehavioral Reviews 47(November):578–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson Miller, Smith-Lovin Lynn, and Brashears Matthew E.. 2006. “Social Isolation in America: Changes in Core Discussion Networks over Two Decades.” American Sociological Review 71(3):353–75. [Google Scholar]
- Melhem Nadine M., Porta Giovanna, Shamseddeen Wael, Payne Monica Walker, and Brent David A.. 2011. “Grief in Children and Adolescents Bereaved by Sudden Parental Death.” Archives of General Psychiatry 68(9):911–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller Gregory E., Chen Edith, and Parker Karen J.. 2011. “Psychological Stress in Childhood and Susceptibility to the Chronic Diseases of Aging: Moving toward a Model of Behavioral and Biological Mechanisms.” Psychological Bulletin 137(6):959–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez Jennifer K., Hummer Robert A., Hayward Mark D., Woo Hyeyoung, and Rogers Richard G.. 2011. “Trends in the Educational Gradient of U.S. Adult Mortality from 1986 to 2006 by Race, Gender, and Age Group.” Research on Aging 33(2):145–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez Jennifer K., Zajacova Anna, and Hayward Mark D.. 2016. “Explaining Inequalities in Women’s Mortality between U.S. States.” Social Science & Medicine-Population Health 2:561–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. 2016. Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities. Hyattsville, MD: U.S. Government Printing Office. [PubMed] [Google Scholar]
- Norton Maria C., Ostbye Truls, Smith Ken R., Munger Ronald G., and Tschanz Joann T.. 2009. “Early Parental Death and Late-life Dementia Risk: Findings from the Cache County Study.” Age and Ageing 38(3):340–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson Julie Skalamera, and Umberson Debra. 2017. “Family Member Death and the Interplay of Race, Place, and Social Class” Presented at the annual conference of the Population Association of America, Chicago, IL. [Google Scholar]
- Pearlin Leonard I., Menaghan Elizabeth, Lieberman Morton A., and Mullan Joseph T.. 1981. The Stress Process. Journal of Health and Social Behavior 22(4):337–56. [PubMed] [Google Scholar]
- Pearlin Leonard I., Schieman Scott, Fazio Elena M., and Meersman Stephen C.. 2005. “Stress, Health, and the Life Course: Some Conceptual Perspectives.” Journal of Health and Social Behavior 46(2):205–19. [DOI] [PubMed] [Google Scholar]
- Phelan Jo C., and Link Bruce G.. 2015. “Is Racism a Fundamental Cause of Inequalities in Health?” Annual Review of Sociology 41:311–30. [Google Scholar]
- Pinquart Martin, and Sörensen Sylvia. 2006. “Gender Differences in Caregiver Stressors, Social Resources, and Health: An Updated Meta-analysis.” The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 61(1):33–45. [DOI] [PubMed] [Google Scholar]
- Repetti Rena L., Taylor Shelley E., and Seeman Teresa E.. 2002. “Risky Families: Family Social Environments and the Mental and Physical Health of Offspring.” Psychological Bulletin182(2):330–66. [PubMed] [Google Scholar]
- Rogers Catherine H., Floyd Frank J., Seltzer Marsha Malick, Greenberg Jan, and Hong Jinkuk. 2008. “Long-term Effects of the Death of a Child on Parents’ Adjustment in Midlife.” Journal of Family Psychology 22(2):203–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenfield Sarah, and Mouzon Dawne M.. 2013. Gender and Mental Health” Pp. 277–96 Handbook of the Sociology of Mental Health, edited by Aneshensel CS and Phelan JC (Eds.),. New York: Springer. [Google Scholar]
- Rostila Mikael, Saarela Jan, and Kawachi Ichiro. 2012. “The Forgotten Griever: A Nationwide Follow-up of Mortality Subsequent to the Death of a Sibling.” American Journal of Epidemiology 176(4):338–46. [DOI] [PubMed] [Google Scholar]
- Ross Catherine E. 2011. “Collective Threat, Trust, and the Sense of Personal Control.” Journal of Health and Social Behavior 52(3):287–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkisian Natalia, and Gerstel Naomi. 2004. “Kin Support among Blacks and Whites: Race and Family Organization.” American Sociological Review 69(6):812–37. [Google Scholar]
- Shiels Meredith S., Chernyavskiy Pavel, Anderson William F., Best Ana F.. Haozous Emily A., Hartge Patricia, Rosenberg Phillip S., Thomas David, Freedman Neil D., and de Gonzalez Amy Berrington. 2017. “Trends in Premature Mortality in the USA by Sex, Race, and Ethnicity from 1999 to 2014: An Analysis of Death Certificate Data.” The Lancet 389(10073):1043–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff Jack P., Garner Andrew S., Siegel Benjamin S., Dobbins Mary I., Earls MF, Garner AS, McGuinn L, Ascoe J, and Wood DL. 2012. “The Lifelong Effects of Early Childhood Adversity and Toxic Stress.” Pediatrics 129(1):232–46. [DOI] [PubMed] [Google Scholar]
- Shonkoff Jack P., Thomas Boyce W, and McEwen Bruce S.. 2009. “Neuroscience, Molecular Biology, and the Childhood Roots of Health Disparities.” JAMA: The Journal of the American Medical Association 301(21):2252–59. [DOI] [PubMed] [Google Scholar]
- Sharkey Patrick 2010. “The Acute Effect of Local Homicides on Children’s Cognitive Performance.” Proceedings of the National Academy of Sciences 107(26):11733–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith Jocelyn.R. 2015. “Unequal Burdens of Loss: Examining the Frequency and Timing of Homicide Deaths Experienced by Young Black Men across the Life Course. American Journal of Public Health 105(S3):S483–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer Carrie A., and Lease Suzanne H.. 2000. “The Impact of Multiple AIDS-related Bereavement in the Gay Male Population.” Journal of Counseling and Development 78(3):297–304. [Google Scholar]
- Stroebe Margaret, Schut Henk, and Stroebe Wolfgang. 2007. “Health Outcomes of Bereavement.” The Lancet 370(9603):1960–73. [DOI] [PubMed] [Google Scholar]
- Stroebe Margaret, Stroebe Wolfgang, and Abakoumkin Georgios. 2005. “The Broken Heart: Suicidal Ideation in Bereavement.” Archives of General Psychiatry 162(11):2178–80. [DOI] [PubMed] [Google Scholar]
- Taylor Shelley E., Klein Laura C., Lewis Brian P., Gruenewald Tara L., Gurung Regan A., and Updegraff John A.. 2000. “Biobehavioral Responses to Stress in Females: Tend-and-befriend, Not Fight-or-flight.” Psychological Review 107(3):411–29. [DOI] [PubMed] [Google Scholar]
- Toblin Robin L., Riviere Lyndon A., Thomas Jeffrey L., Adler Amy B., Kok Brian C., and Hoge Charles W.. 2012. “Grief and Physical Health Outcomes in U.S. Soldiers Returning from Combat.” Journal of Affective Disorders 136(3):469–75. [DOI] [PubMed] [Google Scholar]
- Uchino Bert N., Cacioppo John T., and Kiecolt-Glaser Janice K.. 1996. “The Relationship between Social Support and Physiological Processes: A Review with an Emphasis on Underlying Mechanisms and Implications for Health.” Psychological Bulletin 119(3):488–531. [DOI] [PubMed] [Google Scholar]
- Umberson Debra 2003. Death of a Parent: Transition to a New Adult Identity. Cambridge: Cambridge University Press. [Google Scholar]
- Umberson Debra, Liu Hui, and Reczek Corinne. 2008. “Stress and Health Behaviors” Pp. 19–44 in Advances in Life Course Research: Stress Processes Across the Life Course, edited by Turner HA and Schiemann S. Elsevier Science. [Google Scholar]
- Umberson Debra, and Montez Jennifer K.. 2005. “Social Relationships and Health: A Flashpoint for Public Policy.” Journal of Health and Social Behavior 51(S):S54–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson Debra, Olson Julie S., Crosnoe Robert, Liu Hui, Pudrovska Tetyana, and Donnelly Rachel. 2017. “Death of Family Members as an Overlooked Source of Racial Disadvantage in the United States.” Proceedings of the National Academy of Sciences 114(5):915–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson Debra, Thomeer Mieke B., Kroeger Rhiannon A., Reczek Corinne, and Donnelly Rachel. 2015. “Childhood Adversity and Men’s Relationships in Adulthood: Life Course Processes and Racial Disadvantage.” The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 72(3):498–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson Debra, Williams Kristi, Thomas Patricia A., Liu Hui, and Thomeer Mieke B.. 2014. “Race, Gender, and Chains of Disadvantage: Childhood Adversity, Social Relationships, and Health.” Journal of Health and Social Behavior 55(1):20–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vargas Joao H. Costa. 2008. Never Meant to Survive: Genocide and Utopias in Black Diaspora Communities. New York: Rowman & Littlefield Publishers. [Google Scholar]
- Williams David R., and Sternthal Michelle. 2010. “Understanding Racial-ethnic Disparities in Health: Sociological Contributions.” Journal of Health and Social Behavior 51(1):S15–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams David R., and Mohammed Selina A.. 2013. “Racism and Health I: Pathways and Scientific Evidence.” American Behavioral Scientist 57(8):1152–73. [DOI] [PMC free article] [PubMed] [Google Scholar]