Abstract
Thyroid dysfunctions, particularly hypothyroidism, predispose to cardiovascular diseases, such as atherosclerotic coronary artery disease. However, thyroid functions are not always assessed in such patients. In this report, we studied the cases with pathologically evident ischemic heart disease (IHD) at autopsy and correlated with the absence or presence of thyroid disease. In a 5-year retrospective autopsy-based study, cases with IHD in whom the thyroid gland was dissected at autopsy were analyzed. The thyroid gland was available for assessment in 181 of the 255 autopsied cases with IHD. The majority were males with a mean age of 59.9 years. Thyroid pathology was noted in 58 patients (32.0%) in the form of uninodular or multinodular goiter (56.9%), lymphocytic thyroiditis (37.9%), and Hashimoto's thyroiditis (5.2%). Based on our experience, we feel it may be worthwhile to assess the thyroid by simple inspection and palpation followed by ultrasonographic imaging and estimations of hormones, thyroid-stimulating hormone and antithyroidal antibodies, in all patients presenting with IHD.
Keywords: Ischemic heart disease, Thyroid, Hypothyroidism, Autopsy
1. Introduction
The Indian subcontinent, home to 20% of the world's population, is estimated to have one of the highest burdens of cardiovascular disease (CVD) in the world and majority of the cases have been attributed to ischemic heart disease (IHD), related mainly to atherosclerotic coronary artery disease (CAD). This has assumed an epidemic proportion in India as a fall-out of rapid urbanization (in the form of increased intake of energy-dense foods, usage of tobacco, a decrease in physical activity, and a heightened level of psychosocial stress) and a high prevalence of genetically mediated factors (such as elevated levels of Lp (a), homocysteine, fibrinogen, and plasminogen activator inhibitor). These factors sooner or later lead to development of dysglycemia, hypertension, and dyslipidemia, which are the major atherosclerotic risk factors.1 Similarly, diseases of the thyroid (both hypothyroidism and hyperthyroidism), which are also very common worldwide, predispose to CVD in general and CAD in particular.2 This becomes more relevant in patients with hypothyroidism (often associated with dyslipidemia), which is the most common of thyroid disorders in India, affecting one in 10 adults.3 However, as a routine, investigations for thyroid functions are not always requested for in a setting of CAD. Furthermore, autopsy studies on the thyroid have also not focused on the relationship between thyroid disease and CAD. In this report, we studied the cases with clinically and/or pathologically evident IHD at autopsy and correlated with the absence or presence of thyroid disease.
2. Materials and methods
In a 5-year retrospective autopsy-based study, cases with IHD that caused death or was identified as a comorbid condition were selected. Among these patients, the cases in whom the thyroid gland was dissected at autopsy were further analyzed. The demographic details, duration of admission, clinical presentation, and diagnosis were noted from the available clinical records. The hearts had been fixed by coronary arterial perfusion and were dissected by the inflow-outflow technique. The major epicardial arteries had been studied by serial cross-sections. Depending on the morphology of the myocardium, IHD was classified as acute coronary insufficiency (critical coronary stenosis devoid of visible ischemic changes), acute myocardial infarction (MI), acute-on-chronic MI, and chronic MI. When available, the thyroid was serially sectioned after overnight formalin fixation and two or more sections were processed for histopathological study. The thyroid was labeled as normal or showing features of nodular/multinodular goiter, lymphocytic thyroiditis, or Hashimoto's thyroiditis. The results of this study were then compared, at autopsy, to an age- and sex-matched control group viz. adult patients (age ≥ 18 years) who died without IHD to find the burden of thyroid disease in them. Appropriate descriptive and comparative statistics viz. odds ratio and Fisher exact probably test were used.
3. Results
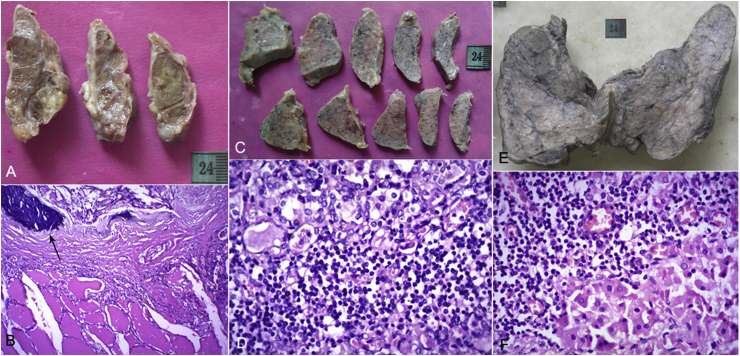
In a span of 5 years, IHD was identified in 255 patients at autopsy. Among these cases, the thyroid gland was available for assessment in 181 patients. There were 137 males and 44 females with an age range of 28–90 years (mean age of 59.9 years). Hypertension and diabetes mellitus were present in 38 and 28 patients, respectively; an additional 56 patients had both the risk factors. A history of smoking and/or alcoholism was elicited in 32 patients. The categories of IHD noted in these patients were as follows: acute coronary insufficiency, 91 (50.3%) patients; acute MI, 13 (7.2%) patients; acute-on-chronic MI, 13 (7.2%) patients; and chronic MI, 64 (35.3%) patients. A thyroid pathology was noted in 58 patients (32.0%, Fig. 1), affecting 32 males and 26 females, in the form of uninodular or multinodular goiter (33 cases, 56.9%), lymphocytic thyroiditis (22 cases, 37.9%), and Hashimoto's thyroiditis (3 cases, 5.2%). One case each of lymphocytic thyroiditis and Hashimoto's thyroiditis was associated with papillary carcinoma and sarcoidosis, respectively. None of the thyroids studied were associated with pathological features of hyperthyroidism. Mild-to-moderate thyromegaly (not noted on clinical examination in any patient) was present in 41 cases, which included all cases of goiter, Hashimoto's thyroiditis, and 14 cases of lymphocytic thyroiditis.
Fig. 1.
Multinodular goiter: (A) the right lobe of the thyroid has been serially sectioned to show multinodularity. Note the absence of enlargement; (B) one of the nodules is well delineated and shows the presence of calcification (arrow, H&E 400×); lymphocytic thyroiditis: (C) Both the lobes of the thyroid have lost their normal pale brown honey-combed appearance and are fleshy and whitish; (D) the whitish appearance was because of the presence of aggregates and infiltrates of lymphocytes (H&E 400×); Hashimoto's thyroiditis: (E) the thyroid is uniformly enlarged and shows a fleshy, lobulated, gray-white cut surface; (F) apart from lymphocytic aggregates, the follicles show oncocytic metaplasia (Hurthle cell change, H&E 400×). H&E, hemotoxylin and eosin.
During the same period, thyroids were available for study in an additional 500 adult patients, with similar age and gender distribution and who died without CAD. It was normal in 373 patients (74.6%). The remaining 127 patients (25.4%) showed thyroidal abnormalities. Multinodular goiter, lymphocytic thyroiditis, and Hashimoto's thyroiditis had been present in 34 (6.8%), 73 (14.6%), and 10 (2%) patients, respectively. The other uncommon pathologies noted were miliary tuberculosis (04, 0.8%), Graves' disease (02, 0.4%), hemosiderosis (01, 0.2%), oncocytoma (01, 0.2%), Hurthle cell carcinoma (01, 0.2%), and metastatic disease (01, 0.2%).
In this study, thyroid abnormalities were seen in 58 of 181 cases of IHD (32%) and 127 of 500 cases of the control group (25.4%). The odds of a patient having thyroid disease in cases of IHD were 1.38 times that of the control group. The one-tailed p-value using Fisher exact probability test was 0.053 indicating an important tendency.
4. Discussion
It is a well-known fact that the thyroid hormones play a crucial role over the development and function of the cardiovascular system. The hormones thyroxine (T4) and tri-iodothyronine (T3) exert their effects through cellular receptors and nongenomic pathways on myocardial contractility and oxygen consumption, cardiac output and rhythm, systemic vascular resistance, and blood pressure.2, 4 Hence, when thyroid dysfunction is known or clinically suspected, a CVD or risk should be investigated. The Clinical Management Guidelines for Coronary Artery Disease for National Program for Prevention and Control of Diabetes, Cardiovascular Disease and Stroke5 recommends that blood samples should be sent for analyzing cardiac enzymes for the diagnosis of acute coronary syndromes, hemogram, fasting blood glucose, blood urea, creatinine, and electrolytes for monitoring, and fasting lipid profile for secondary prevention. Despite the known correlation and high prevalence of thyroid diseases in India, the thyroid functions are not specifically assessed.
Clinical hypothyroidism is characterized by decreased levels of T3 and T4, and compensatory elevated levels of thyroid-stimulating hormone (TSH). Apart from classical clinical symptomatology, hypothyroidism induces diastolic hypertension, bradyarrhythmias, increased atherogenicity, systemic inflammation, endothelial dysfunction, and hypercoagulability. A similar clinical scenario can also occur to a lesser or greater extent with subclinical hypothyroidism, wherein the thyroid hormones are within normal range with high levels of TSH.6 Both would require hormonal supplementation.2, 6 In our cohort of 681 autopsied patients who had the thyroid available for study, 185 thyroids (27.2%) showed thyroidal disease, majority of which fell into the spectrum of diseases seen in India in the form of uninodular or multinodular goiters, lymphocytic thyroiditis, and Hashimoto's thyroiditis.7 Simple goiters that develop mainly because of iodine deficiency involve the entire gland without producing nodularity, but following repeated stimulation and involution may result in uninodular or multinodular goiters. Such patients are generally euthyroid, but in due course of time can become hypothyroid. About 40% of the remaining patients had thyroiditis, a condition which has an autoimmune basis, and such antibodies can also have effects independent of the thyroid function.4 In such patients, there is a transient phase of hyperthyroidism, before lapsing into a hypothyroid state. In this study, we found increased odds of a patient having thyroid disease in cases of IHD as compared with the control group. The limitation of this study was that there was no correlation with lipid profile or thyroid hormonal profiles because of short stay in the hospital, and assessment of thyroid functions was also not present in the protocols followed. However, our main objective was to demonstrate the high prevalence of thyroid abnormalities among patients with IHD, warranting more careful evaluation for thyroid dysfunction in clinical practice by simple inspection and palpation followed by ultrasonographic imaging and estimations of the hormones, TSH, and antithyroidal antibodies.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There is no conflict of interest.
References
- 1.Prabhakaran D., Jeemon P., Roy A. Cardiovascular diseases in India: current epidemiology and future directions. Circulation. 2016;133:1605–1620. doi: 10.1161/CIRCULATIONAHA.114.008729. [DOI] [PubMed] [Google Scholar]
- 2.Coceani M. Heart disease in patients with thyroid dysfunction: hyperthyroidism, hypothyroidism and beyond. Anadolu Kardiyol Derg. 2013;13:62–66. doi: 10.5152/akd.2013.008. [DOI] [PubMed] [Google Scholar]
- 3.Bagcchi S. Hypothyroidism in India: more to be done. Lancet Diabetes Endocrinol. 2014;2:778. doi: 10.1016/S2213-8587(14)70208-6. [DOI] [PubMed] [Google Scholar]
- 4.Grais M., Sowers J.R. Thyroid and the heart. Am J Med. 2014;127:691–698. doi: 10.1016/j.amjmed.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clinical Management Guidelines for Coronary Artery Disease . A manual for medical officer; 2008. National Program for Prevention and Control of Diabetes, Cardiovascular Disease and Stroke. 42p. [Google Scholar]
- 6.Abreu I.M., Lau E., de Sousa Pinto B., Carvallo D. Subclincial hypothyroidism: to treat or not to treat, that is the question! A systematic review with meta-analysis on lipid profile. Endocr Connect. 2017;6:188–189. doi: 10.1530/EC-17-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Unnikrishnan A.G., Menon U.V. Thyroid disorders in India: an epidemiological perspective. Indian J Endocr Metabol. 2011;15:S78–S81. doi: 10.4103/2230-8210.83329. [DOI] [PMC free article] [PubMed] [Google Scholar]