Abstract
Prescription opioid misuse is a serious public health concern, yet antecedent factors are poorly described. Using data from the National Longitudinal Study of Adolescent to Adult Health (N = 14,784), we examined the longitudinal relationship between a history of adolescent chronic pain and the odds of misusing prescription opioids in adulthood. The primary predictor variable was chronic pain status during adolescence. The primary outcome variables were prescription opioid misuse during early adulthood and adulthood. Multivariate models controlled for known risk factors of opioid misuse, including sociodemo-graphics (sex, race, and ethnicity), adolescent mental health symptoms (anxiety, depression), adolescent self-reported physical health status, adolescent substance use/abuse, childhood trauma, and adult legitimate opioid use. We found that adults with a history of adolescent chronic pain were more likely to misuse opioids than those without history of chronic pain, even after controlling for other known risk factors. Further, we found that among individuals with history of adolescent chronic pain that race (white), other substance use, and exposure to trauma were risk factors for later opioid misuse. Longitudinal associations between adolescent chronic pain and subsequent adult prescription opioid misuse highlight the need for early targeted screening and prevention efforts that may reduce later opioid misuse.
Keywords: Adolescent, chronic pain, opioid misuse
Prescription opioid misuse is defined as the consumption of opioids in manner or dose other than prescribed, consuming others’ prescriptions, or consuming opioids for feelings that are elicited (ie, to get high).31 Prescription opioid misuse is a serious public health epidemic in the United States. In 2013, almost 10 million Americans (4.9% of the adult population) reported prescription opioid misuse.15 Prescription opioid misuse was found to be most prevalent among young adults 18 to 26 years of age, of whom 7.1% reported opioid misuse over the previous 12 months in 2016 in the United States.4 Cumulatively, by age 28, almost 23 to 30% of Americans report misusing opioids at some point during their lifetime according to data from the 2008 National Longitudinal Study of Adolescent Health (Add Health) and the 2014 National Survey on Drug Use and Health.3,45
Prescription opioid misuse among young adults is associated with severe consequences including decreased employment,1 sexual victimization,19 and driving under the influence.52 Furthermore, opioid misuse is a key antecedent for opioid use disorder, which may be characterized as a problematic pattern of opioid use that causes significant impairment or distress.5 Indeed, opioids accounts for >50% of drug-related emergency department visits,30 and unintentional opioid overdose deaths now exceed those for all other illicit drugs in the United States.40 In 2016, 2.1 million Americans reported having an opioid use disorder.4
Risk factors for opioid misuse remain poorly understood, yet many of the risk factors identified thus far are already present during adolescence, including a history of substance abuse25; anxiety and depressive symptoms9; a history of childhood trauma37; higher socioeconomic status45; female sex28; and white, non-Hispanic race.26 Better identification of risk factors would allow targeted screening and prevention efforts during childhood, decreasing the incidence and negative impact of later opioid misuse.
Chronic pain in adolescence is a potentially important individual difference factor that may help explain risk of prescription opioid misuse. Chronic pain affects 15 to 25% of adolescents,21 and adolescents with chronic pain share some similar characteristics with those who develop prescription opioid misuse, including an increased prevalence of exposure to childhood trauma16 and increased rates of anxiety and depression.32 Furthermore, a recent meta-analysis found that 25% of adults with chronic pain misuse prescription opioids.50 However, studies have not yet identified whether having chronic pain during adolescence is associated with an increased risk for future prescription opioid misuse in adulthood.
Thus, the primary aim of this study was to determine the associations between adolescent chronic pain and subsequent prescription opioid misuse in adulthood in a large, nationally representative sample of individuals in the United States. We hypothesized that adults with a history of chronic pain during adolescence were more likely to misuse prescribed opioids, over and above other known risk factors of opioid misuse, including sociodemographic variables (sex, race, ethnicity, and income), adolescent mental health symptoms (anxiety and depression), adolescent substance use/abuse, history of childhood trauma, and legitimate opioid use during adulthood. Our second aim was to explore specific risk factors associated with subsequent prescription opioid misuse in adulthood among individuals with a history of adolescent chronic pain. We hypothesized that the following risk factors in adolescence would predict increased risk for prescription opioid misuse in adulthood: higher household income, greater anxiety and depressive symptoms, higher substance use scores, and a greater number of traumatic experiences in childhood. Findings from these analyses will provide health care providers with a better understanding about which of their adolescent patients with chronic pain are at increased risk for future problematic opioid use.
Methods
Participants and Procedure
For this cross-sectional analysis, we used data from Add Health.29 Add Health is a nationally representative, stratified, random sample of 20,745 U.S. participants starting in 1995 when participants were 11 to 21 years of age (mean age = 16 years, standard deviation = 1.7 years). Add Health combines longitudinal survey data on respondents′ sociodemographic factors, physical and mental health, and substance use, providing unique opportunities to study how risk factors in adolescence are linked to health outcomes in adulthood.
Add Health uses a complex, multistage sample design and oversamples minorities. By applying survey weights, estimates are representative of the U.S. population. Thus far, participants have completed 4 subsequent waves of in-home interviews, the most recent of which was in 2008 when participants were between the ages of 24 and 34 years (mean age = 29 years, standard deviation = 1.7 years). Waves include wave I (adolescents 11–21 years of age, assessed in 1995), wave II (adolescents 12–22 years of age, assessed in 1996), wave III (early adulthood, 18–28 years of age, assessed in 2002), and wave IV (adulthood, 24–34 years of age, assessed in 2008). We extracted data from all 4 waves. The sample size included participants who completed all of the relevant items and waves (n = 14,784). Participant characteristics are presented in Table 1. Additional information on Add Health is available at http://www.cpc.unc.edu/projects/addhealth. Add Health data are publicly available, and therefore the institutional review board at Seattle Children’s Hospital deemed this study exempt from review.
Table 1.
Wave I Sociodemographic and Baseline Characteristics of Individuals With and Without a History of Adolescent Chronic Pain
| Characteristic | Full Sample | No Adolescent Chronic Pain | Adolescent Chronic Pain | P Value |
|---|---|---|---|---|
| Sample, n | 14,784 | 11,610 | 3,174 | |
| Estimated population, millions | 21.9 | 17.1 | 4.8 | |
| Mean age at wave I, y | 16.0 | 16.0 | 16.0 | .94 |
| Mean age at wave IV, y | 28.9 | 28.9 | 28.9 | .76 |
| Sex, female % | 49.3 | 47.1 | 57.4 | <.0001 |
| Race and ethnicity, % | .25 | |||
| White, non-Hispanic | 65.6 | 65.2 | 67.5 | |
| Black, non-Hispanic | 15.5 | 15.5 | 15.5 | |
| Hispanic | 12.0 | 12.4 | 10.6 | |
| Other | 6.8 | 7.0 | 6.4 | |
| Mean income, $ | 45,665 | 46,182 | 43,994 | .11 |
| Mean depressive symptoms (range = 0–60) | 11.4 | 10.4 | 14.9 | <.0001 |
| Mean anxiety symptoms (range = 0–20) | 2.3 | 2.0 | 3.5 | <.0001 |
| General health rated as fair or poor, % | 7.0 | 5.6 | 12.1 | <.0001 |
| Substance use (range = 0–6) | 1.1 | 1.0 | 1.4 | <.0001 |
| Childhood trauma exposures (range = 0–9) | .4 | .4 | .6 | <.0001 |
| Legitimate opioid use during wave IV, % | 5.2 | 4.7 | 6.9 | <.001 |
| Prescription opioid misuse, wave III (early adulthood), % | 19.9 | 18.8 | 24.0 | <.0001 |
| Prescription opioid misuse, wave IV (adulthood), % | 28.3 | 27.0 | 33.0 | <.0001 |
Data source: Longitudinal Study of Adolescent to Adult Health.
Measures
Fig 1 outlines Add Health waves and measures assessed at each time point.
Figure 1.
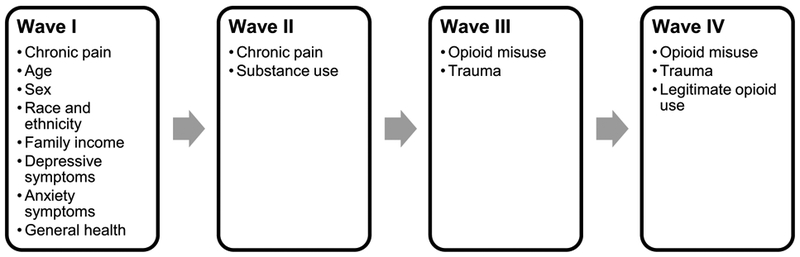
National Longitudinal Study of Adolescent to Adult Health (Add Health) waves and measures assessed at each wave.
Chronic Pain
Adolescents completed a general health survey during waves I and II, which assessed pain location and frequency. Adolescents were asked to rate the frequency of common types of pain conditions over the previous 12 months (headache; stomachache; and aches, pain, or soreness in the muscles or joints). Adolescents reported whether they experienced each pain never, just a few times, about once a week, almost every day, or every day. We dichotomized pain as chronic or not chronic. To avoid overinflating rates and keeping consistent with the definitions of high-frequency pain used in previous literature, we used a conservative classification of chronic pain to include pain occurring almost every day or every day, consistent with previous publications using data from Add Health.32,47 Moreover, the prevalence rates of chronic pain within this dataset (21.9%) were similar to those cited in previous research.21
Prescription Opioid Misuse
Prescription opioid misuse was measured in the waves after chronic pain measurement. Thus, whereas chronic pain was measured at waves I and II, prescription opioid misuse was measured in waves III and IV. Specifically in the Add Health study, assessments were conducted to identify which participants initiated prescription opioid misuse between waves II and III and again between waves III and IV. This design allowed us to determine which individuals had chronic pain in adolescence before reporting prescription opioid misuse in adulthood.
We used self-report data from waves III and IV to measure cumulative prescription opioid misuse. The exact item stems varied slightly across waves, reflecting different opioids available in the United States between waves. Wave III prescription opioid misuse was identified by the following question: “Since June 1995 (Wave II), have you taken any of the following drugs without a doctor’s permission: pain killers such as Darvon, Demerol, Percodan or Tylenol with codeine?” with a binary response option of yes or no. Wave IV prescription opioid misuse was identified by the following question: “Which of the following prescription drugs have you taken that were not prescribed for you, taken in larger amounts than prescribed, for longer periods than prescribed, or that you only took for the feeling or experience they caused: pain killers or opioids such as Vicodin, OxyContin, Percocet, Demerol, Percodan or Tylenol with codeine not prescribed?” with a binary response option of yes or no. For analyses, responses at each wave were coded as a binary variable (no opioid misuse = 0, any opioid misuse = 1).
Sociodemographics
During wave I, adolescents reported their age, sex, race, and ethnicity. Parents reported their household income.
Anxiety Symptoms
Adolescents completed a questionnaire assessing 5 physiological anxiety symptoms during wave I. This approach has been used in previous Add Health studies18 to access anxiety symptoms. Specifically, adolescents were asked the frequency of each of the following symptoms over the previous 12 months: 1) felt hot all over suddenly, for no reason; 2) cold sweats; 3) chest pains; 4) fearfulness; and 5) trouble relaxing. Responses to each item were measured using a 5-point Likert scale (anchors, 0 [never] to 4 [every day]). Similar to previously published research using this variable in the Add Health database, total anxiety symptom scores were calculated as a sum of the 5 items, with a possible range from 0 (no anxiety symptoms) to 20 (frequent/severe anxiety symptoms).18
Depressive Symptoms
Adolescents completed the 20-item Center for Epidemiologic Studies Depression Scale at wave I. Items were scored based on the frequency at which depressive symptoms were experienced in the previous week using a 4-point Likert scale (anchors, never/rarely and most/all of the time). Similar to previously published Add Health studies, total scores were calculated as a sum of the 20 items and could range from 0 (no depressive symptoms) to 60 (frequent/severe depressive symptoms).41
General Health
Adolescents responded to the question “In general, how is your health?” with 5 response options ranging from excellent to poor in wave I. For analyses, response options were dichotomized as either good (responses of excellent, very good, or good) or fair or poor (responses of fair or poor). For analyses, the referent of fair or poor was coded as 0 and good was coded as 1.
Other Substance Use in Adolescence
At wave 2, adolescents responded to the following 6 items assessing other substance use behaviors: 1) “Have you ever regularly smoked one or more cigarettes per day”; 2) “Have you had 5 or more drinks in a row over the past 12 months”; 3) “Have you ever tried marijuana”; 4) “Have you ever tried cocaine”; 5) “Have you ever tried inhalants, such as glue”; and 6) “Have you ever tried any other illegal drugs such as LSD, PCP, heroin, pills, etc.” Response options for all 6 items were binary (yes vs no). Prior Add Health publications have used these items to characterize substance use behaviors during adolescence.45 For analyses, we summed these 6 dichotomous variables (yes = 1, no = 0) to create a continuous variable representing 0 to 6 total substances used, where higher scores indicate a greater number of substances used.
Childhood Trauma
Using data from waves I, III, and IV, adolescents responded to 9 items assessing exposure to childhood trauma. Specifically, adolescents were asked how often the following happened: 1) “being left alone when an adult should have been present >6 times”; 2) “not having adults taking care of their basic needs >6 times”; 3) “being slapped, kicked, or hit by an adult caregiver >6 times”; 4) “being touched in a sexual way or being forced to touch an adult in a sexual way”; 5) “having Social Services investigate or try to take them out of their living situation”; 6) “witnessed or threatened with physical violence”; 7) “someone stabbed you”; 8) “someone shot at you”; or 9) “someone physically assaulted/beaten you up.” Response options for all 9 items were binary (yes vs no), Consistent with previously published Add Health studies,13 we summed these 9 dichotomous variables (yes = 1, no= 0) to create a continuous variable representing 0 to 9 total individual traumas experienced during childhood.37
Legitimate Opioid Use During Adulthood
During wave IV, interviewers asked participants to provide information on all prescription medications consumed in the previous 4 weeks. These medications were categorized into therapeutic classes using the Multum Lexicon database. We identified all participants who reported taking a prescribed opioid.
Statistical Analysis
All analyses were conducted using the survey package contained in Stata version 12.1 (StataCorp, College Station, TX); a was set at .05. We adjusted for the complex sample design of Add Health by using sampling weights, regional stratification, and primary sampling unit information to provide nationally representative estimates of the U.S. population.
To address our primary aim, we directly compared rates of prescription opioid misuse at both waves III and IV between adults who had chronic pain as adolescents with those who did not have chronic pain as adolescents. Next, we performed a multivariate logistic regression analysis to determine the association between adolescent chronic pain status and adult prescription opioid misuse after controlling for other known risk factors, including sociodemographic factors (sex, race and ethnicity, income), mental health (anxiety and depressive symptoms), physical health, other adolescent substance use/abuse, and exposure to childhood trauma. We also included legitimate opioid use during wave IV as a covariate in our model assessing associations between history of adolescent chronic pain and opioid misuse at wave IV. However, we should note that the inclusion versus exclusion of this covariate did not affect the size or direction of our estimated odds ratios (ORs).
To address our second aim, we used multivariate logistic regression analyses selecting only participants with a history of chronic pain during adolescence to determine the association between hypothesized risk factors and subsequent prescription opioid misuse during adulthood among individuals with history of adolescent chronic pain. The dependent variable used in our second aim was cumulative opioid misuse at wave IV.
Results
Sample Description
Our sample included 14,784 participants weighted represent 21.93 million individuals nationally. Of 3,174 (weighted percentage = 21.9%) reported chronic pain during adolescence. Sample characteristics, subdivided by chronic pain status, are presented Table 1. Females reported chronic pain more frequently than males: although females represented 49.3% of entire sample, they represented 57.4% of those chronic pain. Adolescents with chronic pain, on reported higher depressive and anxious symptoms were more likely to rate their general health as fair poor compared with adolescents without chronic We also found that adolescents with chronic reported higher scores on both substance use and hood trauma exposure variables than those chronic pain.
Aim 1: Association Between Adolescent Chronic Pain History and Prescription Opioid Misuse During Early Adulthood (Wave III) and Adulthood (Wave IV)
In the full sample, 19.9% of individuals reported ation of prescription opioid misuse between wave (12–22 years of age; 1996) and wave III (18–28 years age; 2002; Table 1). Furthermore, an additional 8.4% individuals reported initiation of prescription misuse between waves III and IV (24–34 years of 2008). Thus, we found that by wave IV 28.3% of pants endorsed prescription opioid misuse. The rate reported prescription opioid misuse in early adulthood was higher among individuals with a history of adolescent chronic pain versus those without pain (24% vs 18.8%, P < .001). Similarly, the rate reported prescription opioid misuse in adulthood also higher among individuals with a history of cent chronic pain versus those without (33% vs 27%, P < .001). After controlling for multiple factors as fied in our logistic regression models, individuals with history of adolescent chronic pain had significantly increased odds of reported prescription opioid misuse both early adulthood (adjusted odds ratio [AOR] = 95% confidence interval [CI] = 1.05–1.46, P = 0.13; Table 2) and adulthood (AOR = 1.19, 95% CI =1.04–1.36, P = .01). We also found that younger participants were more likely to report opioid misuse than older ticipants and that females were less likely to report oid misuse. In addition, black and Hispanic participants were less likely to report opioid misuse than white ticipants. Having a history of adolescent substance and childhood trauma was associated with an odds of reported opioid misuse. Legitimate opioid in the preceding 4 weeks was associated with increased odds of opioid misuse. Self-reported sive and anxiety symptoms and overall physical reported as fair or poor were not associated with scription opioid misuse.
Table 2.
Multivariate Logistic Regression Analyses Testing the Association Between Adolescent Chronic Pain History and Prescription Opioid Misuse in Adulthood at Waves III and IV
| Characteristic | Early Adulthood (Wave III) | Adulthood (Wave IV) | ||||
|---|---|---|---|---|---|---|
| AOR | 95% CI | P Value | AOR | 95% CI | P Value | |
| Adolescent chronic pain | ||||||
| No | Reference | Reference | ||||
| Yes | 1.24 | 1.05–1.46 | .013 | 1.19 | 1.04–1.36 | .013 |
| Age | .90 | .86–.95 | <.0001 | .88 | .85–.92 | <.0001 |
| Sex | ||||||
| Male | Reference | Reference | ||||
| Female | .81 | .70–.94 | .006 | .76 | .66–.86 | <.0001 |
| Race and ethnicity | ||||||
| White, non-Hispanic | Reference | Reference | ||||
| Black, non-Hispanic | .52 | .38–.72 | <.0001 | .39 | .29–.51 | <.0001 |
| Hispanic | .53 | .41–.69 | <.0001 | .50 | .40–.62 | <.0001 |
| Other | .87 | .65–1.17 | .349 | .88 | .69–1.13 | .311 |
| Income | 1.00 | 1.00–1.00 | .092 | 1.00 | 1.00–1.00 | .416 |
| Depression | 1.00 | .99–1.01 | .911 | 1.00 | .99–1.01 | .588 |
| Anxiety | .99 | .95–1.03 | .704 | .99 | .95–1.03 | .487 |
| Health reported as fair or poor | ||||||
| No | Reference | Reference | ||||
| Yes | .96 | .71 −1.32 | .815 | 1.18 | .90–1.56 | .223 |
| Substance use | 1.21 | 1.16–1.27 | <.0001 | 1.27 | 1.22–1.33 | <.0001 |
| Childhood trauma exposures | 1.32 | 1.23–1.42 | <.0001 | 1.31 | 1.21 −1.41 | <.0001 |
| Legitimate opioid use during wave IV | - | - | - | 1.95 | 1.53–2.48 | <.0001 |
Aim 2: Predictors of Prescription Opioid Misuse Within Adults With a History of Adolescent Chronic Pain
Table 3 presents results from our multivariate logistic regression analysis examining the associations between adolescent risk factors and subsequent adult prescription opioid misuse among participants who had a history of adolescent chronic pain. Our findings partially supported our hypotheses. When investigating race, white adolescents were more likely to misuse opioids in adulthood than black adolescents (AOR = .40, 95% CI = .23–.69) and Hispanic adolescents (AOR = .42, 95% CI = .25–.71). Females were less likely to misuse opioids than males (AOR = .67, 95% CI = .52–.86). Contrary to our hypotheses, we did not find that higher depressive (AOR = .99, 95% CI = .98–1.01) or anxiety symptoms (AOR = 1.02, 95% CI = .96–1.08) were associated with prescription opioid misuse. However, higher scores on adolescent substance use (AOR = 1.27, 95% CI = 1.17–1.39) and childhood trauma exposure (AOR = 1.38, 95% CI = 1.21–1.58) were significantly associated with an increased likelihood of misusing opioids in adulthood.
Table 3.
Multivariate Logistic Regression Analyses Testing Associations Between Hypothesized Risk Factors and Prescription Opioid Misuse Among Participants With a History of Chronic Pain During Adolescence
| Characteristic | AOR | 95% CI | P Value |
|---|---|---|---|
| Age | .93 | .87–1.00 | .065 |
| Sex | |||
| Male | Reference | ||
| Female | .67 | .52–.86 | .002 |
| Race and ethnicity | |||
| White, non-Hispanic | Reference | ||
| Black, non-Hispanic | .40 | .23–.69 | .001 |
| Hispanic | .42 | .25–.71 | .001 |
| Other | 1.40 | .86–2.29 | .17 |
| Income | 1.00 | 1.00–1.00 | .284 |
| Depression | .99 | .98–1.01 | .473 |
| Anxiety | 1.02 | .96–1.08 | .563 |
| Health reported as fair or poor | |||
| No | Reference | ||
| Yes | 1.01 | .65–1.57 | .967 |
| Substance use | 1.27 | 1.17–1.39 | <.0001 |
| Childhood trauma exposures | 1.38 | 1.21–1.58 | <.0001 |
Discussion
In this secondary analysis of an ongoing longitudinal survey, we examined whether adolescent chronic pain increases the risk for subsequent prescription opioid misuse in adulthood using a nationally representative sample of individuals in the United States. As we hypothesized, chronic pain status in adolescence was associated with an increased risk for prescription opioid misuse in early adulthood and adulthood over and above other known demographic and clinical covariates. Specifically, we found that the rate of opioid misuse in early adulthood was higher among individuals with a history of adolescent chronic pain (24%) than those without a chronic pain history (19%). Similarly, the rate of opioid misuse in adulthood was higher among individuals with a history of adolescent chronic pain (33%) than those without a chronic pain history (27%). Our finding that 19.9% of 18- to 26-year-olds misused opioids is similar to a previous report from the National Survey on Drug Use and Health, which found that 20.2% of 18- to 25-year-old Americans had misused pain relievers in 2014.3
Among the subsample of individuals with a history of adolescent chronic pain, we also sought to identify risk factors for later prescription opioid misuse. Consistent with our hypothesis, we found that youth who were white, female, used other substances, and had a history of exposure to childhood trauma were particularly vulnerable to opioid misuse in adulthood. This pattern of results is generally consistent with prior research, which has also found that opioid misuse is more likely among white children (as compared with racial and ethnic minority youth),26 youth who use marijuana or engage in binge drinking,28 and youth with a history of physical abuse or assault.37 Our finding that adolescent females may be at higher risk for later opioid misuse than males is somewhat difficult to interpret owing to mixed findings in prior literature. For example, some epidemio-logic studies have also identified a higher risk for opioid misuse among females,4,3 whereas others have found females to be at either lower risk20 or equivalent risk compared with males.26 The etiology of the racial and ethnic differences in opioid misuse identified in our study and others is also poorly understood. For example, a recent study examining racial and ethnic differences in opioid use between Mexican American adults versus non-Hispanic white and black American adults indicated that patient preferences and cultural values may influence differential rates of opioid use between racial and ethnic groups.17 To our knowledge, similar research has not yet been conducted in pediatric populations.
Contrary to our hypothesis, symptoms of depression and anxiety among adolescents with chronic pain were not associated with a later risk for opioid misuse. Psychological factors have been implicated in the persistence of chronic pain from adolescence to adulthood, including negative affect and pain catastrophizing,51 yet the precise role of psychological functioning in the development of opioid misuse remains unclear. For example, Grattan et al12 found that depression was associated with opioid misuse among adults with chronic pain, whereas Hah et al14 found that depression and anxiety were not associated with opioid misuse among adults with chronic pain in multivariate models. In contrast, Quinn et al38 recently found strong associations between mental health diagnoses, including anxiety and depression, and long-term opioid use in adolescents, although opioid misuse was not examined in that study. Potential shared biological mechanisms between chronic pain and opioid use in childhood are also largely unexplored, although there has been some work in this area in animal models and adult populations that may be informative. In a recent review, Finan et al8 proposed that chronic pain states may lead to changes in dopaminergic neurotransmission and the mesolimbic system functions involved in the perception of pain, reward, and pain relief. An increased risk for problematic opioid use is proposed to result directly from these neurobiological changes or may occur indirectly via changes in psychological functioning (ie, increased negative affect, pain catastrophizing, pain-related fear).8 Limited available research suggests that, similar to their adult counterparts, youth with chronic pain also experience alterations in brain regions involved in pain processing, reward, and pain-related fear, with the amygdala being of particular importance.44 Furthermore, both chronic pain and opioid misuse are associated with genetic polymorphisms in dopaminergic pathways. For example, dopamine D2 receptors36 and dopamine active transporters have been shown to alter pain perception and response to experimental pain in animal models and in adults with chronic pain conditions.53 Dopamine has also been identified as an important contributor to the opioid reward system, as evidenced by associations between opioid addiction and decreased expression of dopamine D2 receptors in the brain.11,46
In addition to potential shared biological and psychological mechanisms, it is also important to consider social factors driving opioid use and the subsequent opioid epidemic in the United States. For example, recent nationwide increases in opioid prescribing to children and adolescents10 may be attributed to the confluence of several societal changes, including an increasing understanding of pediatric pain21 and its negative consequences,39 increased vigilance toward pain management by regulatory agencies, and increased marketing of opioid medications to patients and providers by pharmaceutical companies. Treating pain with opioids is associated with increased risky opioid behaviors later in life.2 For example, Miech et al28 found that legitimate opioid use during adolescence was associated with a 33% increased risk for opioid misuse before age 23 years, and McCabe et al24 also found that that legitimate opioid use during adolescence was associated with opioid misuse at age 35 years. The next steps in this line of work should account for broader societal factors that may influence opioid prescribing practices and subsequent community-level and nationwide risks for opioid misuse and abuse across the lifespan. Our findings also suggest that a history of trauma and other substance use in adolescence may increase risk for opioid misuse later in life.
For youth with chronic pain conditions who may benefit from opioid medications, an important clinical consideration is ensuring adequate pain relief while minimizing risks of opioid misuse, overdose, and opioid use disorder. This step is of particular importance for pediatric populations, because untreated or under-treated pain in childhood has the potential to substantially disrupt neurobiological42 and psychosocial development34 and persist into adulthood.51 It is important to recognize that even for youth with chronic pain conditions who have a legitimate need for opioid medication, the gold standard for the management of pediatric chronic pain is interdisciplinary pain care, which may include pharmacotherapy but emphasizes the important role of behavioral pain management interventions, physical and occupational therapy, and complementary and alternative modalities.23 Although we did not examine legitimate opioid use among adolescents in this study, our findings support the need for development of guidelines aimed at decreasing the risk for opioid misuse among children and adolescents with chronic pain.7
Consistent with prior research, our findings indicate that most prescription opioid misuse was initiated between adolescence and early adulthood.4 This finding suggests that adolescence may be a critical time for clinicians to identify risk for later opioid misuse and, potentially, to deploy preventive interventions directed at substance use behaviors. For example, adolescents often have unrestricted access to opioid medications at home,27 and a recent survey found that 1 in 4 adolescents did not consider prescription opioid misuse to be a risky behavior.35 Our findings support existing recommendations for health care providers, parents, and adolescents receiving an opioid prescription to receive education about 1) the impact of prescription drug misuse on the developing brain, 2) safe storage and disposal of opioid medications in the home, and 3) prescription drug monitoring.33 Our findings suggest that adolescents at increased risk for later opioid misuse (eg, presence of chronic pain, other substance use, history of exposure to childhood trauma) may require closer monitoring to ensure appropriate use of opioid medications.
Findings from this secondary data analysis should be interpreted in the context of several limitations. First, chronic pain status in adulthood was not assessed in the Add Health survey; as a result, we cannot distinguish rates of opioid misuse between adults with versus without concurrent chronic pain. Second, the legitimate use of prescription opioids during adolescence was not assessed in the Add Health survey. Therefore, we are not able to determine rates of co-occurring opioid use and chronic pain in our sample before early adulthood, and we are unable to make conclusions about associations between opioid use and misuse in our sample. Third, opioid misuse was assessed using a single self-report item, and other factors related to patterns and drivers of opioid misuse were not assessed (eg, frequency, motivation for misuse). As a result, we were not able to evaluate potentially relevant nuances such as differences by opioid type and the impact of motivation on the initiation of opioid use and misuse behaviors. To our knowledge, this limitation is not unique to our study; more comprehensive self-report measures of opioid misuse risk have not yet been validated for adolescent populations. Furthermore, existing measures developed for adult populations have demonstrated poor psychometric properties and limited clinical usefulness (Voon et al49 provide a comprehensive listing).6 Finally, different questions were used to assess opioid misuse in wave III versus wave IV, which may have impacted our findings. Specifically, wave IV asks about oxycodone, hydrocodone/paracetamol (Vicodin), and acetaminophen/oxycodone (Percocet), whereas wave IV also included greater detail on opioid misuse behaviors. The less comprehensive approach in wave III may have led to an underestimation of opioid misuse prevalence at that time point. Despite these limitations, the results from this study contribute to the limited evidence on the association between pediatric chronic pain and prescription opioid misuse.
In conclusion, this is the first nationally representative study to examine whether chronic pain in adolescence is associated with opioid misuse in adulthood. Chronic pain affects 15 to 25% of adolescents and is associated with increased risk for poor clinical outcomes in adulthood, including mental48 and physical health symptoms51 and alcohol and tobacco use.22 Our study extends knowledge of the long-term outcomes associated with adolescent chronic pain by investigating subsequent prescription opioid misuse in adulthood. Our findings provide evidence that opioid misuse is more likely for adults with versus without a history of adolescent chronic pain. This longitudinal association is of high public health importance, because the prescription opioid epidemic severely affects individuals in the United States across the lifespan. Early identification of at-risk individuals may minimize later prescription drug misuse. In our study, several risk factors for opioid misuse later in life were identified, including white race, female sex, other substance use, and history of childhood trauma.
Perspective:
Using a large, nationally representative sample, we found that chronic pain during adolescence was an independent risk factor for opioid misuse in adulthood, over and above other known risk factors. Furthermore, among those individuals with adolescent chronic pain, substance use, exposure to trauma, and race were associated with opioid misuse.
Acknowledgments
Supported by an early career grant from the International Association for the Study of Pain (PI: C.B.G.) and the National Institutes of Health (grant nos. K24HD060068 [PI: T.M.P.] and K23NS089966 [PI: E.F.L.])
Footnotes
The authors have no conflicts of interest to declare.
References
- 1.Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL: Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med 12:657–667, 2011 [DOI] [PubMed] [Google Scholar]
- 2.Boyd CJ, Young A, Grey M, McCabe SE: Adolescents’ nonmedical use of prescription medications and other problem behaviors. J Adolesc Health 45:543–550, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Center for Behavioral Health Statistics and Quality: 2014 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD, Substance Abuse and Mental Health Services Administration, 2015 [Google Scholar]
- 4.Center for Behavioral Health Statistics and Quality: 2016 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD, Substance Abuse and Mental Health Services Administration, 2017 [Google Scholar]
- 5.Centers for Disease Control and Prevention: Opioid overdose: Commonly used terms. Available at: https://www.cdc.gov/drugoverdose/opioids/terms.html. Accessed February 10, 2018
- 6.Chou R, Fanciullo GJ, Fine PG, Miaskowski C, Passik SD, Portenoy RK: Opioids for chronic noncancer pain: Prediction and identification of aberrant drug-related behaviors: A review of the evidence for an American Pain Society and American Academy of Pain Medicine clinical practice guideline. J Pain 10:131–146, 2009 [DOI] [PubMed] [Google Scholar]
- 7.Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic pain: United States, 2016. JAMA 315:1624–1645, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Finan PH, Remeniuk B, Dunn KE: The risk for problematic opioid use in chronic pain: What can we learn from studies of pain and reward. Prog Neuropsychopharmacol Biol Psychiatry, 2017. August 1 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fink DS, Hu R, Cerda M, Keyes KM, Marshall BD, Galea S, Martins SS: Patterns of major depression and nonmedical use of prescription opioids in the United States. Drug Alcohol Depend 153:258–264, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fortuna RJ, Robbins BW, Caiola E, Joynt M, Halterman JS: Prescribing of controlled medications to adolescents and young adults in the United States. Pediatrics 126:1108–1116, 2010 [DOI] [PubMed] [Google Scholar]
- 11.Gardner EL: Addiction and brain reward and antire-ward pathways. Adv Psychosom Med 30:22–60, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grattan A, Sullivan MD, Saunders KW, Campbell CI, Von Korff MR: Depression and prescription opioid misuse among chronic opioid therapy recipients with no history of substance abuse. Ann Fam Med 10:304–311, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haberstick BC, Boardman JD, Wagner B, Smolen A, Hewitt JK, Killeya-Jones LA, Tabor J, Halpern CT, Brummett BH, Williams RB, Siegler IC, Hopfer CJ, Mullan Harris K: Depression, stressful life events, and the impact of variation in the serotonin transporter: Findings from the National Longitudinal Study of Adolescent to Adult Health (Add Health). PLoS One 11, 2016:e0148373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hah JM, Sturgeon JA, Zocca J, Sharifzadeh Y, Mackey SC: Factors associated with prescription opioid misuse in a cross-sectional cohort of patients with chronic non-cancer pain. J Pain Res 10:979–987, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Han B, Compton WM, Jones CM, Cai R: Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003–2013. JAMA 314:1468–1478, 2015 [DOI] [PubMed] [Google Scholar]
- 16.Holley AL, Wilson AC, Noel M, Palermo TM: Post-traumatic stress symptoms in children and adolescents with chronic pain: A topical review of the literature and a proposed framework for future research. Eur J Pain 20:1371–1383, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hollingshead NA, Vrany EA, Stewart JC, Hirsh AT: Differences in Mexican Americans’ prevalence of chronic pain and co-occurring analgesic medication and substance use relative to non-Hispanic white and black Americans: Results from NHANES 1999–2004. Pain Med 17:1001–1009, 2016 [DOI] [PubMed] [Google Scholar]
- 18.Jacobson NC, Newman MG: Avoidance mediates the relationship between anxiety and depression over a decade later. J Anxiety Disord 28:437–445, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jessell L, Mateu-Gelabert P, Guarino H, Vakharia SP, Syckes C, Goodbody E, Ruggles KV, Friedman S: Sexual violence in the context of drug use among young adult opioid users in New York City. J Interpers Violence, 2015. August 3 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kelly BC, Wells BE, Leclair A, Tracy D, Parsons JT, Golub SA: Prevalence and correlates of prescription drug misuse among socially active young adults. Int J Drug Policy 24:297–303, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, MacDonald AJ: The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain 152:2729–2738, 2011 [DOI] [PubMed] [Google Scholar]
- 22.Law EF, Bromberg MH, Noel M, Groenewald C, Murphy LK, Palermo TM: Alcohol and tobacco use in youth with and without chronic pain. J Pediatr Psychol 40:509–516, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin SR, Zeltzer LK: Prioritizing pediatric chronic pain and comprehensive pain treatment in the context of the opioid epidemic. Pain Manag 8:67–70, 2018 [DOI] [PubMed] [Google Scholar]
- 24.McCabe SE, Veliz P, Schulenberg JE: Adolescent context of exposure to prescription opioids and substance use disorder symptoms at age 35: A national longitudinal study. Pain 157:2173–2178, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCabe SE, West BT, Teter CJ, Boyd CJ: Co-ingestion of prescription opioids and other drugs among high school seniors: Results from a national study. Drug Alcohol Depend 126:65–70, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCabe SE, West BT, Veliz P, McCabe VV, Stoddard SA, Boyd CJ: Trends in medical and nonmedical use of prescription opioids among US adolescents: 1976–2015. Pediatrics 139:e20162387, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McDonald EM, Kennedy-Hendricks A, McGinty EE, Shields WC, Barry CL, Gielen AC: Safe storage of opioid pain relievers among adults living in households with children. Pediatrics 139:e20162161, 2017 [DOI] [PubMed] [Google Scholar]
- 28.Miech R, Johnston L, O’Malley PM, Keyes KM, Heard K: Prescription opioids in adolescence and future opioid misuse. Pediatrics 136:e1169–e1177, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Institutes of Health: The National Longitudinal Study of Adolescent to Adult Health: Social, behavioral, and biological linkages across the life course. Available at: http://www.cpc.unc.edu/projects/addhealth. Accessed February 11, 2018
- 30.National Institute on Drug Abuse: Drug-related hospital emergency room visits Available at https://www.drugabuse.gov/publications/drugfacts/drug-related-hospital-emergency-room-visits; 2011. Accessed February 12, 2018
- 31.National Institute on Drug Abuse: Misuse of prescription drugs Available at https://www.drugabuse.gov/publications/research-reports/misuse-prescription-drugs/summary. 2016. Accessed February 2, 2017
- 32.Noel M, Groenewald CB, Beals-Erickson SE, Gebert JT, Palermo TM: Chronic pain in adolescence and internalizing mental health disorders: A nationally representative study. Pain 157:1333–1338, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.United States Department of Health and Human Services, Office of Adolescent Health: Opioids and adolescents. Available at: https://www.hhs.gov/ash/oah/adolescent-development/substance-use/drugs/opioids/index.html#prevention. Accessed January 10, 2018
- 34.Palermo TM, Valrie CR, Karlson CW: Family and parent influences on pediatric chronic pain: A developmental perspective. Am Psychol 69:142–152, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Partnership for Drug-Free Kids (formerly known as The Partnership at DrugFree.org) 2012 partnership attitude tracking study: Teens and parents. Available at: https://drugfree.org/wp-content/uploads/2013/04/PATS-2012-FULL-REPORT2.pdf. Accessed December 18, 2017
- 36.Qadri YJ, Bortsov AV, Orrey DC, Swor RA, Peak DA, Jones JS, Rathlev NK, Lee DC, Domeier RM, Hendry PL, McLean SA: Genetic polymorphisms in the dopamine receptor 2 predict acute pain severity after motor vehicle collision. Clin J Pain 31:768–775, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quinn K, Boone L, Scheidell JD, Mateu-Gelabert P, McGorray SP, Beharie N, Cottler LB, Khan MR: The relationships of childhood trauma and adulthood prescription pain reliever misuse and injection drug use. Drug Alcohol Depend 169:190–198, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Quinn PD, Hur K, Chang Z, Krebs EE, Bair MJ, Scott EL, Rickert ME, Gibbons RD, Kroenke K, D’Onofrio BM: Incident and long-term opioid therapy among patients with psychiatric conditions and medications: A national study of commercial health care claims. Pain 158:140–148, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rabbitts JA, Zhou C, Groenewald CB, Durkin L, Palermo TM: Trajectories of postsurgical pain in children: Risk factors and impact of late pain recovery on long-term health outcomes after major surgery. Pain 156:2383–2389, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rudd RA, Seth P, David F, Scholl L: Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR Morb Mortal Wkly Rep 65:1445–1452, 2016 [DOI] [PubMed] [Google Scholar]
- 41.Rushton JL, Forcier M, Schectman RM: Epidemiology of depressive symptoms in the National Longitudinal Study of Adolescent Health. J Am Acad Child Adolesc Psychiatry 41:199–205, 2002 [DOI] [PubMed] [Google Scholar]
- 42.Schwaller F, Fitzgerald M: The consequences of pain in early life: Injury-induced plasticity in developing pain pathways. Eur J Neurosci 39:344–352, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Simoni-Wastila L, Ritter G, Strickler G: Gender and other factors associated with the nonmedical use of abusable prescription drugs. Subst Use Misuse 39:1–23, 2004 [DOI] [PubMed] [Google Scholar]
- 44.Simons LE, Erpelding N, Hernandez JM, Serrano P, Zhang K, Lebel AA, Sethna NF, Berde CB, Prabhu SP, Becerra L, Borsook D: Fear and reward circuit alterations in pediatric CRPS. Front Hum Neurosci 9:703, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stewart TD, Reed MB: Lifetime nonmedical use of prescription medications and socioeconomic status among young adults in the United States. Am J Drug Alcohol Abuse 41:458–464, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tacelosky DM, Alexander DN, Morse M, Hajnal A, Berg A, Levenson R, Grigson PS: Low expression of D2R and Wntless correlates with high motivation for heroin. Behav Neurosci 129:744–755, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van Tilburg MA, Spence NJ, Whitehead WE, Bangdiwala S, Goldston DB: Chronic pain in adolescents is associated with suicidal thoughts and behaviors. J Pain 12:1032–1039, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vinall J, Pavlova M, Asmundson GJ, Rasic N, Noel M: Mental health comorbidities in pediatric chronic pain: A narrative review of epidemiology, models, neurobiological mechanisms and treatment. Children (Basel) 3:E40, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Voon P, Karamouzian M, Kerr T: Chronic pain and opioid misuse: A review of reviews. Subst Abuse Treat Prev Policy 12:36, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP, van der Goes DN: Rates of opioid misuse, abuse, and addiction in chronic pain: A systematic review and data synthesis. Pain 156:569–576, 2015 [DOI] [PubMed] [Google Scholar]
- 51.Walker LS, Sherman AL, Bruehl S, Garber J, Smith CA: Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. Pain 153:1798–1806, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wilson FA, Stimpson JP, Pagan JA: Fatal crashes from drivers testing positive for drugs in the U.S, 1993–2010. Public Health Rep 129:342–350, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wood PB, Glabus MF, Simpson R, Patterson JC 2nd: Changes in gray matter density in fibromyalgia: Correlation with dopamine metabolism. J Pain 10:609–618, 2009 [DOI] [PubMed] [Google Scholar]


