Abstract
Background
In ST-elevation myocardial infarction (STEMI), prehospital delay is a significant factor, decreasing likelihood of revascularization and increasing mortality. Prehospital delays are substantive in Indian patients with STEMI. Our study aimed to investigate factors associated with prehospital delay in patients with STEMI.
Methods
A multicentric prospective analysis was conducted at five major cardiac care referral centers in Punjab including a tertiary care teaching hospital over a period of 1 year from January 2015 to December 2015. Patients presenting with STEMI were included in the study. A structured questionnaire was used to gather patient characteristics and factors responsible for prehospital delay.
Results
Of the 619 patients included in the study, 42% presented with more than 6 h of prehospital delay. On univariate analysis, delay was significantly higher among elderly (p = 0.01), illiterate patients (p = 0.02), and patients residing in rural areas (p = 0.04). Recognizing symptoms as cardiac in origin (p < 0.001), hospital as initial medical contact, and availability of prehospital electrocardiogram (ECG) (p = 0.001) were associated with shorter delays. On multivariate analysis, prehospital delay was significant in elderly patients, initial point of care as outpatient clinic, and patients without access to prehospital ECG.
Conclusion
Our study concludes that demographic and socioeconomic barriers exist that impede rapid care seeking and highlights the need for utilization of prehospital ECG to decrease prehospital delay. Possibilities include, educating the public on the importance of early emergency medical services contact or creating emergency stations in rural areas with ECG capabilities. Our study also invites further research, regarding role of telemedicine to triage patients derived from prehospital ECGs to decrease prehospital delay. Keywords: STEMI, Pre-hospital ECG, Pre-hospital delay, Factors, Telemedicine.
Keywords: STEMI, Pre-hospital ECG, Pre-hospital delay, Factors, Telemedicine
1. Introduction
Cardiovascular diseases are a major cause of morbidity and mortality globally, with an estimated 17.7 million deaths in 2015, representing 31% of the total global deaths.1 India has one of the highest burden of acute coronary syndrome in the world2 constituting approximately 60% of the world's heart disease. Among the Indian population, outcomes in patients with ST-elevation myocardial infarction (STEMI) demonstrate higher in-hospital mortality. A significant contributory factor for this is the unacceptably high prehospital delay, consistently seen in Indian patients.3, 4 This results in several patients unable to receive timely life-saving revascularization therapy and a reduced efficacy of revascularization among those who receive it.
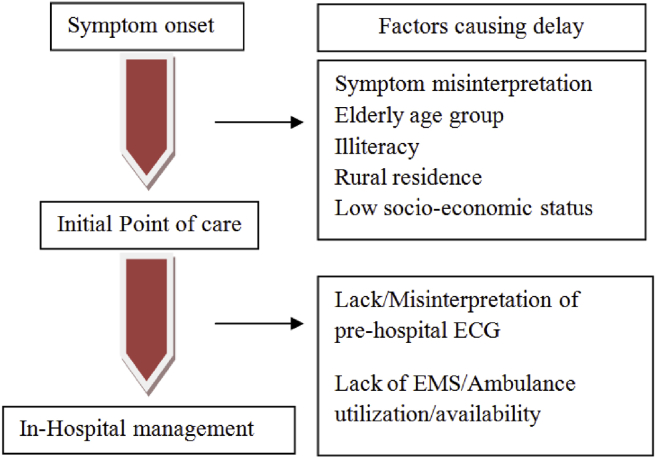
Potential periods of delays in treatment of STEMI for patients include symptom onset to initial point of care; initial point of care to hospital arrival delays, and in-hospital management delays including obtaining a diagnostic electrocardiogram (ECG) and administering reperfusion therapy (Fig. 1).
Fig. 1.
Variables affecting prehospital delay. ECG, electrocardiogram; EMS, emergency medical services.
Few studies in developing countries have identified factors that might play a significant role in prehospital delay.5, 6, 7, 8 A greater understanding of the contributing factors may be a key element in designing simple and economical strategies to enable faster access to revascularization in patients, thereby improving their prognosis. Our study was, thus, conducted to determine factors delaying interval to hospital presentation in patients with STEMI.
2. Materials and methods
A multicentric prospective analysis was conducted over a period of 1 year (January 2015 to December 2015) at five major primary reperfusion-capable cardiac care referral centers in Punjab, including a tertiary care teaching hospital.
This study included patients with STEMI if they met any two of the following three criteria: (1) typical symptoms of STEMI; (2) ECG findings compatible with STEMI; (3) elevated cardiac markers. Patients without recall of exact time of symptom onset or with any psychiatric, cognitive or communication problems were excluded from the study.
Prehospital delay was defined as the time elapsed from symptom onset to arrival at a reperfusion-capable hospital on the basis of which patients were categorized into two groups: group I, delay <6 h and group II, delay >6 h. These time periods were chosen considering the predominant uses of fibrinolytic therapy in developing countries,4 and given its greatest benefit within 1 h of symptom onset, with a sharp drop off after 6 h and almost no benefit after 12 h of symptom onset.9, 10, 11
After an informed consent, a questionnaire was administered, which contained information about various demographic factors, educational background, socioeconomic status, type of nearest medical facility, availability of prehospital ECG and medical aid, health history of the patient, and the time from symptom onset to hospital arrival. Socioeconomic status was categorized using the Modified Kuppuswamy scale. The questionnaire was designed and tested for reliability and validity. Pilot testing of the questionnaire was carried out on a small number of patients not included in the study.
Subsequently, univariate and multivariate analysis was performed on collected data using Statistical Package for the Social Sciences (IBM SPSS Statistics for Windows, version 21.0, IBM Corp., Armonk, NY), and various factors leading to prehospital delay were identified. Multivariate analysis was performed using binary logistic regression on variables significant on univariate analysis. A p-value of <0.05 was considered significant when comparing the effect of variables on prehospital delay.
3. Results
A total of 619 patients with acute STEMI met our study criteria and were included in the study, of which 58% of the patients presented within 6 h to the hospital, whereas 42% of the patients presented after 6 h. Of the 619 patients, 487 patients (78.6%) were males and 132 patients (21.3%) were females. The patient population covered patients both from urban and rural areas with a majority from the urban areas (67%).
In our study, on comparing prehospital time with various variables (Table 1), we found that prehospital delay was significant in the elderly population (p = 0.01), rural population (p = 0.014) and illiterate population (p = 0.005). No significant prehospital delay was seen associated with patient gender, patient socioeconomic status, patient's family type, or the availability of health insurance.
Table 1.
Prehospital delay in relation to various sociodemographic variables (values in percentage).
| Variable | Time in reaching hospital |
Total (in %) | p-value | ||
|---|---|---|---|---|---|
| <6 h, n = 360 (in %) | >6 h, n = 259 (in %) | ||||
| Age group (years) | <60 | 62.4 | 37.6 | 59.3 | 0.01 |
| >60 | 52.0 | 48.0 | 40.7 | ||
| Gender | Male | 58.5 | 41.5 | 78.6 | 0.725 |
| Female | 56.8 | 43.2 | 21.4 | ||
| Residence | Rural | 51.2 | 48.8 | 33.1 | 0.014 |
| Urban | 61.5 | 38.4 | 66.9 | ||
| Education | Illiterate | 51.1 | 48.9 | 37.6 | 0.005 |
| Literate | 62.4 | 37.6 | 62.4 | ||
| Type of family | Joint | 53.3 | 46.6 | 35.7 | 0.073 |
| Nuclear | 60.8 | 39.2 | 64.3 | ||
| Health insurance | No | 57.8 | 42.2 | 92 | 0.566 |
| Yes | 62.0 | 38.0 | 8.0 | ||
| Socioeconomic status | Low | 54.0 | 46.0 | 8.0 | 0.121 |
| Middle | 57.1 | 42.8 | 83.0 | ||
| High | 70.9 | 29.1 | 8.8 | ||
| Time of symptoms | 6 am To 6 pm | 55.6 | 44.4 | 70.3 | 0.050 |
| 6 pm To 6 am | 64.1 | 35.9 | 29.7 | ||
| Symptom perception | Cardiac | 75.5 | 24.5 | 62.66 | <0.001 |
| Gastrointestinal | 26.7 | 73.3 | 23.6 | <0.001 | |
| Musculoskeletal | 29.2 | 70.8 | 7.8 | 0.01 | |
| Others | 37.8 | 62.2 | 6.0 | <0.001 | |
| Comorbidities | Diabetes | 52.6 | 47.4 | 33.7 | 0.047 |
| Hypertension | 54.2 | 45.8 | 34.6 | 0.147 | |
| CAD | 48.0 | 52.0 | 8.1 | 0.129 | |
| Smoking | 60.0 | 40.0 | 4.0 | 0.849 | |
| Alcohol | 49.0 | 50.9 | 8.5 | 0.160 | |
| Initial medical contact | Hospital (nonreperfusion capable) | 62.5 | 37.5 | 54.8 | 0.015 |
| Outpatient clinic | 52.9 | 47.1 | 45.2 | ||
| Distance to initial medical contact | <5 km | 60.3 | 39.7 | 42.3 | 0.354 |
| 6–10 km | 53.2 | 46.8 | 24.9 | 0.154 | |
| >10 km | 59.1 | 40.9 | 32.8 | 0.737 | |
| ECG at initial medical contact | No | 36.7 | 63.3 | 9.7 | 0.001 |
| Yes | 60.5 | 39.5 | 90.3 | ||
| Treatment received | Reperfusion therapy | 79.4 | 20.6 | 66.7 | <0.001 |
| Nonreperfusion therapy | 15.5 | 84.5 | 33.3 | ||
| Conveyance used | Ambulance | 54.5 | 45.5 | 5.3 | 0.665 |
| Personal | 58.4 | 41.6 | 94.7 | ||
CAD, coronary artery disease; ECG, electrocardiogram.
The most common chief complaint in the presenting patients was chest pain (91.1%); however, only 62.7% of the patients perceived it as a cardiac symptom with others perceiving it to be from a noncardiac source most commonly gastrointestinal or musculoskeletal pain. Recognizing symptoms as cardiac in origin resulted in decreased prehospital delay (p < 0.001), whereas perceiving symptoms as gastrointestinal or musculoskeletal resulted in a significant prehospital delay (p < 0.001 and p = 0.01).
Seventy percent of the patients had symptom onset between 6 am and 6 pm and had a marginally significant delay in reaching the hospital as compared to 30% of the patients having symptom onset between 6 pm and 6 am (p = 0.050). The most common comorbidities present were diabetes (33.7%) and hypertension (34.6%). Patients with diabetes had a decreased prehospital delay (p = 0.047), whereas no significant association was seen between other comorbidities and prehospital delay.
Nearest medical aid available to most of the patients was either a hospital (nonreperfusion capable) (54.8%) or an outpatient clinic (45.2%). Significant prehospital delay was observed if the patients' point of initial medical contact was an outpatient clinic as compared to a hospital (nonreperfusion capable). Availability of a nearby nonreperfusion capable hospital significantly decreased prehospital delay and enabled patients to report earlier to hospitals equipped with primary reperfusion capabilities (p = 0.015).
On assessing prehospital delay with distance to initial medical care, no statistically significant difference was seen. Although ambulance awareness was present in 96% of patients, ambulance services were used by only 5.3% of patients.
ECG availability and utilization, when analyzed with the point of initial medical contact, demonstrated that ECG availability was predominantly seen in 96.4% of hospitals (nonreperfusion capable), whereas only 83% of outpatient facilities had this capability. Availability and utilization of ECG at initial medical contact (prehospital ECG) resulted in a significant decrease in prehospital delay (p = 0.001) (Table 1).
On multivariate analysis, factors that significantly increased prehospital delay included age group >60 years, initial medical contact of an outpatient clinic, and nonavailability of ECG at initial medical contact (Table 2).
Table 2.
Multivariate analysis (factors influencing prehospital delay > 6 h).
| Factors | Exp(B) [95% CI] | p-value |
|---|---|---|
| Age group > 60 years | 1.614 [1.048–2.487] | 0.030 |
| Residence—rural | 1.075 [0.680–1.698] | 0.758 |
| Education—illiterate | 1.470 [0.937–2.305] | 0.094 |
| Time of symptoms—6 am to 6 pm | 0.837 [0.530–1.321] | 0.445 |
| Symptom perception | ||
| Cardiac | 0.492 [0.214–1.132] | 0.095 |
| Gastrointestinal | 1.247 [0.522–2.982] | 0.619 |
| Other | 0.747 [0.241–2.320] | 0.614 |
| Comorbidities diabetes | 1.254 [0.805–1.952] | 0.317 |
| Nearest medical aid—outpatient clinic | 0.615 [0.389–0.971] | 0.037 |
| ECG availability at nearest medical aid—no | 2.198 [1.061–4.554] | 0.034 |
CI, confidence interval; ECG, electrocardiogram.
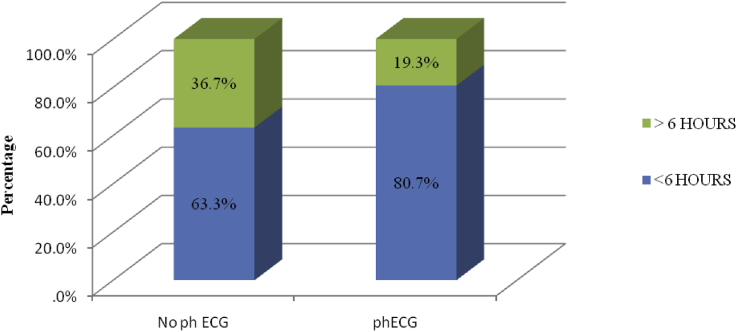
On analyzing ECG utilization with early reperfusion therapy, it was seen that in cases where prehospital ECG was performed, approximately 80.7% of the patients received early reperfusion therapy, whereas cases where prehospital ECG was not performed, only 63.3% of the patients received early reperfusion therapy (p = 0.026) (Fig. 2).
Fig. 2.
Proportion of patients receiving reperfusion therapy within 6 h and >6 h of hospital arrival phECG, prehospital electrocardiogram.
4. Discussion
In our study, age more than 60 years, rural residence, illiteracy, symptom misperception, outpatient clinic as initial point of contact, and nonutilization of prehospital ECG led to a significant prehospital delay of more than 6 h in patients with STEMI.
Our findings are consistent with other published reports showing increased prehospital delay in elderly compared with younger population,12, 13 reasons for which may include limited access to and use of medical care, failure to recognize symptoms of STEMI that may be more nonspecific in this age group, lack of access to transport, or emergency medical services (EMS) to the hospital. Similar studies have also shown that prehospital delay was significantly more in females as compared to male counterparts attributing the difference to greater frequency nonspecific symptoms in females and socioeconomic barriers.13, 14 Our study failed to show any significant difference in prehospital delay when comparing male patients with female patients.
A significant difference in hospital reporting time was also seen among patients residing in urban population compared with their rural counterparts and literate population compared to illiterate populations. These two factors were also seen in univariate analysis in our study; however, they were not significant in multivariate analysis. Various factors play a role in this difference including increased illiteracy rates in rural areas, decreased awareness of medical symptoms, lack of access to transportation, distant nearby medical aids, and nonavailability of standard treatment in remote health-care facilities.
In our study, no significant difference in prehospital delay was seen with patients' marital status, coresiding family members, or history of prior comorbidities. It is unclear why patients with a history of coronary artery disease fail to present earlier to the hospital given abundant counseling and education provided to them. Strangely enough, studies such as the Worcester study has reported that a history of MI may possibly be associated with prolonged prehospital delay.15
In addition to sociodemographic factors, prehospital delay in STEMI is also influenced by factors such as recognition of signs and symptoms by the patients and ability to access emergency medical care. In the present study, although STEMI presented most commonly with chest pain, only 62.7% of the patients perceived it as a cardiac symptom, whereas 24% of our study population perceived it as gastritis and 6% perceived it to be a muscular pain. In our study, prehospital delay was significantly less when patients perceived their symptoms as cardiac related. Attributing the symptoms to noncardiac source such as gastrointestinal or muscular resulted in significant prehospital delay, an observation also supported by other similar studies.6, 8
When comparing our observational data with similar studies performed in different regions of India, similar factors affecting prehospital delay have been established based on demographics (old age and rural background) and symptomatic profile of the patients with a general consensus that awareness about the typical symptoms of heart attack are necessary for the prevention of prehospital delay (Table 3). A number of studies have sought to answer whether prehospital delays might be shortened by public education regarding symptoms of acute MI. A recent systematic review of 10 studies aiming to reduce prehospital delay times concluded that there was little evidence that public education interventions reduced prehospital delay.16 Similarly, the REACT study carried out from 1995 to 1997 in 20 American cities concluded that although persons living in the target areas of the public information campaigns were demonstrably better informed about the subject afterward; however, the prehospital times in the target areas were not shortened significantly in comparison to control areas.17 Despite contradicting evidence, population education might be a promising intervention in developing countries to reduce prehospital delay.
Table 3.
Factors affecting delay in Indian population.
| Study | Factors increasing delay |
|---|---|
| Rajagopalan et al5 | Initial point of contact—general practitioner |
| Age >65 years | |
| Khan et al6 | Misinterpretation of symptoms |
| Transportation delay/no help available | |
| Financial reasons | |
| Initial misdiagnosis | |
| Beig et al7 | Initial misdiagnosis/referral delay |
| Transport delay | |
| Rural residence | |
| Absence of prior CAD | |
| Choudhary et al25 | Old age |
| Female sex | |
| Rural residence | |
| H/o diabetes | |
| Symptom perception | |
| Our study | Age > 60 years |
| Rural residence | |
| Illiteracy | |
| Noncardiac symptom perception | |
| Initial point of contact—outpatient clinic | |
| Nonavailability of prehospital ECG |
CAD, coronary artery disease; ECG, electrocardiogram.
Other common variables elucidated by different Indian studies show that initial misdiagnosis, referral delay, and transport delay are important factors increasing prehospital delay (Table 3). Emergent interventions are needed to reduce delay during this prehospital phase. Utilization of prehospital ECG is one of the major interventions which may help reduce this delay, by increasing physician confidence of STEMI diagnosis and guide diagnosis in cases of atypical symptoms with a possible link with telemedicine for early referral and patient transport.
One of the major findings in our study showed that. ECG utilization at initial medical contact resulted in a statistically significant decrease in prehospital delay (Table 1, Table 2) and significantly increased myocardial reperfusion therapy rates. In cases where prehospital ECG was carried out, 80.7% of the patients received early reperfusion therapy compared with 63.3% of the patients without prehospital ECG (Fig. 2). ECG obtained before hospital arrival, leads to an early STEMI diagnosis eliminating the need for in-hospital ECG and increased hospital preparedness for a possible emergent reperfusion, thus resulting in markedly reduced time to reperfusion therapy.
In consensus with various studies18 highlighting the importance of prehospital ECG, the American Heart Association national guidelines recommend that EMS acquire and use prehospital ECGs to evaluate patients with suspected acute coronary syndrome.
With significant evidence in favor of prehospital ECG, we present a significant opportunity to reduce prehospital delay in our country.
In our study, we observed that was that 25% of our study population had basic medical care facilities located farther than 10 km. Also in our study population, ambulance services were used in only 5.3% of patients, reflecting poor knowledge of the importance of early EMS contact.
Thus, in support of our findings, we recommend efforts to increase both availability and use of prehospital ECG to reduce time to reperfusion in STEMI patients. Possibilities include equipping ambulance services with ECG or creating emergency stations in rural areas with ECG capabilities and educating the public on the importance of early EMS contact when the symptoms of MI are observed. The central challenge for health-care providers is not to simply perform a prehospital ECG but to use and integrate the diagnostic with systems of care. A hub-and-spoke model similar to the system of care in the TN-STEMI program,19 relying on an integrated health-care network based on clusters of primary health-care clinics and small hospitals built around large tertiary care facilities can be followed, which has successfully demonstrated significant reduction in prehospital delay by reducing time to first medical contact (FMC), FMC to ECG time, and total ischemic time.20
In our study, prehospital times were delayed in about 39% of the patients who had an ECG at the first point of contact. This delay includes various factors including transportation time or time spent in cases of misinterpreted ECG. Use of telemedicine in the prehospital triage of STEMI patients has been shown to be associated with a reduced mean prehospital delay and lower patient mortality rates both in observational studies21, 22 and in meta-analyses.23 Thus, in consensus with international guidelines, the use of telemedicine is further recommended in the diagnosis and management of STEMI.24
5. Limitations
Our study was primarily conducted in the setting of a private health-care system, thus excluding patients dependent on public health care. Further studies are needed in the public sector to further ascertain overall population characteristics. Patients who received thrombolysis outside the study centers were excluded from the study and although every effort was made to interview patients soon after admission, data may have been affected by recall bias.
6. Conclusion
The results of this large multihospital study provide evidence that demographic and socioeconomic barriers exist that impede rapid care seeking. Old age, rural residence, and symptom misinterpretation resulted in a significant delay in reaching hospital, while ECG availability at the point of first contact resulted in less prehospital delay and earlier reperfusion. The present study highlights that there is an increasing need to educate the general public regarding symptoms of STEMI and increase the availability of ECG in remote areas for decreasing the prehospital delay. Our study also invites further research, regarding the role of telemedicine to triage patients derived from prehospital ECGs to further decrease prehospital delay.
Conflicts of interest
All authors have none to declare.
Acknowledgment
The authors acknowledge Madan Mohan Bansal (Guru Nanak Hospital, Muktsar) and N S Balian (Balian Heart Centre, Dhuri).
References
- 1.World health Organization. Factsheet Updated May 2017. available at: www.who.int/mediacentre/factsheets/fs317/en/ (last cited on 22.7.2017).
- 2.Ghaffar A., Reddy K.S., Singhi M. Burden of non-communicable diseases in South Asia. BMJ. 2004;328:807–810. doi: 10.1136/bmj.328.7443.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mohanan P.P., Mathew R., Harikrishnan S. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013;34:121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xavier D., Pais P., Devereaux P.J., Xie C., Prabhakaran D., Reddy K.S. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 5.Rajagopalan R.E., Chandrasekaran S., Pai M., Rajaram R., Mahendran S. Pre-hospital delay in acute myocardial infarction in an urban Indian hospital: a prospective study. Natl Med J India. 2001;14:8–12. [PubMed] [Google Scholar]
- 6.Khan A., Phadke M., Lokhandwala Y.Y., Nathani P.J. A study of pre-hospital delay patterns in acute myocardial infarction in an urban tertiary care Institute in Mumbai. J Assoc Phys India. 2017;65:24–27. [PubMed] [Google Scholar]
- 7.Beig J.R., Tramboo N.A., Kumar K. Components and determinants of therapeutic delay in patients with acute ST-elevation myocardial infarction: a tertiary care hospital-based study. J Saudi Heart Assoc. 2017;29:7–14. doi: 10.1016/j.jsha.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gao Y., Zhang H.-J. The effect of symptoms on prehospital delay time in patients with acute myocardial infarction. J Int Med Res. 2013;41:1724–1731. doi: 10.1177/0300060513488511. [DOI] [PubMed] [Google Scholar]
- 9.Taher T., Fu Y., Wagner G.S., Goodman S.G., Fresco C., Granger C.B. Aborted myocardial infarction in patients with ST-segment elevation: insights from the assessment of the safety and efficacy of a new thrombolytic regimen-3 trial electrocardiographic Substudy. J Am Coll Cardiol. 2004;44:38–43. doi: 10.1016/j.jacc.2004.03.041. [DOI] [PubMed] [Google Scholar]
- 10.LATE Study Group Late Assessment of Thrombolytic Efficacy (LATE) study with alteplase 6–24 hours after onset of acute myocardial infarction. Lancet. 1993;342:759–766. [PubMed] [Google Scholar]
- 11.EMERAS Collaborative Group Randomized trial of late thrombolysis in patients with suspected acute myocardial infarction. Lancet. 1993;342:767–772. [PubMed] [Google Scholar]
- 12.Goldberg R.J., Steg P.G., Sadiq I. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE registry) Am J Cardiol. 2002;89:791–796. doi: 10.1016/s0002-9149(02)02186-0. [DOI] [PubMed] [Google Scholar]
- 13.Nguyen H.L., Gore J.M., Saczynski J.S. Age and sex differences and 20-year trends (1986 to 2005) in prehospital delay in patients hospitalized with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2010;3:590–598. doi: 10.1161/CIRCOUTCOMES.110.957878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alshahrani H., McConkey R., Wilson J., Youssef M., Fitzsimons D. Female gender doubles pre-hospital delay times for patients experiencing ST segment elevation myocardial infarction in Saudi Arabia. Eur J Cardiovasc Nurs. 2014;13:399–407. doi: 10.1177/1474515113507159. [DOI] [PubMed] [Google Scholar]
- 15.Saczynski J.S., Yarzebski J., Lessard D. Trends in prehospital delay in patients with acute myocardial infarction (from the Worcester heart attack study) Am J Cardiol. 2008;102:1589–1594. doi: 10.1016/j.amjcard.2008.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kainth A., Hewitt A., Sowden A. Systematic review of interventions to reduce delay in patients with suspected heart attack. Emerg Med J. 2004;21:506–508. doi: 10.1136/emj.2003.013276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luepker R.V., Raczynski J.M., Osganian S. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease: the Rapid Early Action for Coronary Treatment (REACT) Trial. J Am Med Assoc. 2000;284:60–67. doi: 10.1001/jama.284.1.60. [DOI] [PubMed] [Google Scholar]
- 18.Scholz K.H., Hilgers R., Ahlersmann D. Contact-to-balloon time and door-to-balloon time after initiation of a formalized data feedback in patients with acute ST-elevation myocardial infarction. Am J Cardiol. 2008;101:46–52. doi: 10.1016/j.amjcard.2007.07.078. [DOI] [PubMed] [Google Scholar]
- 19.Alexander T., Victor S.M., Mullasari A.S. Protocol for a prospective, controlled study of assertive and timely reperfusion for patients with ST-segment elevation myocardial infarction in Tamil Nadu: the TN-STEMI programme. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-003850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raja D.C., Subban V., Victor S.M. The impact of systems-of-care on pharmacoinvasive management with streptokinase: the subgroup analysis of the TN-STEMI programme. Indian Heart J. 2017;69:573–579. doi: 10.1016/j.ihj.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brunetti N.D., Bisceglia L., Dellegrottaglie G. Lower mortality with pre-hospital electrocardiogram triage by telemedicine support in high risk acute myocardial infarction treated with primary angioplasty: preliminary data from the Bari-BAT public Emergency Medical Service 118 registry. Int J Cardiol. 2015;185:224–228. doi: 10.1016/j.ijcard.2015.03.138. [DOI] [PubMed] [Google Scholar]
- 22.Brunetti N.D., Amodio G., De Gennaro L. Telecardiology applied to a region-wide public emergency health-care service. J Thromb Thrombolysis. 2009;28:23–30. doi: 10.1007/s11239-008-0241-y. [DOI] [PubMed] [Google Scholar]
- 23.de Waure C., Cadeddu C., Gualano M.R., Ricciardi W. Telemedicine for the reduction of myocardial infarction mortality: a systematic review and a meta-analysis of published studies. Telemed J E Health. 2012;18:323–328. doi: 10.1089/tmj.2011.0158. [DOI] [PubMed] [Google Scholar]
- 24.Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC), Steg P.G., James S.K. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33:2569–2619. doi: 10.1093/eurheartj/ehs215. [DOI] [PubMed] [Google Scholar]
- 25.Choudhary R., Sharma S.M., Kumar V., Gautam D.K. An Observational study of prehospital and hospital delay in reperfusion for acute myocardial infarction at a University Hospital in India. J Pract Cardiovasc Sci. 2016;2:163–168. [Google Scholar]