Abstract
Background
Door-to-balloon (DTB) time of 90 min during primary angioplasty is considered as the benchmark duration. Shorter DTB time is preferable, and longer duration can have poor clinical outcomes.
Methods
A cross-sectional observational study of three months in Shahid Gangalal National Heart Center was conducted in which all patients undergoing primary angioplasty were included. The DTB time was calculated, and the different determining factors were studied.
Results
Seventy-nine patients undergoing primary percutaneous intervention were studied. The median DTB time was 79 minutes (Interquartile range [IQR] 59–115 min). Forty-six (58.2%) patients had a DTB time of less than 90 min. DTB time varied significantly with direct visit vs transfer (p = 0.029) and office time visit (9 am–5 pm) vs off time (5 pm–9 am) (p = 0.012). DTB time did not differ between any infarct-related vessels (p = 0.471), number of vessels involved (p = 0.638), and the added procedures (defibrillation, thrombosuction, and temporary pacemaker insertion) (p = 0.682) during angioplasty. No significant differences were recorded according to age (p = 0.330), gender (p = 0.254), hypertension (p = 0.073), diabetes (p = 0.487), heart failure (p = 0.316), and baseline left ventricular ejection fraction (LVEF) (p = 0.819).
Conclusion
The median DTB time in primary angioplasty was less than 90 minutes. The significant determining factors were timing of hospital visit (office vs off time) and type of visit (direct vs transfer). There can be improvement in factors determining DTB time to lower it further.
Keywords: Direct vs. transfer, Door-to-balloon time, Office time vs. off time, Radial vs. femoral
1. Introduction
Primary percutaneous coronary intervention (PCI) is the preferred treatment for the management of ST segment elevation acute myocardial infarction. The American Heart Association guidelines have introduced the concept of door-to-balloon (DTB) time emphasizing on the timely management of PCI. DTB time is the time required for ballooning after entry of patients to the hospital. The target DTB time as per the guidelines is 90 min or less.1, 2, 3
Different studies have reported various contributing factors responsible for varying DTB time. Reducing DTB time has been associated with lower in-hospital mortality,4, 5, 6 at 30 days7 and at 1 year.5, 8 Increased DTB time has been associated with increased mortality.9, 10
This is the first study conducted in Nepal for studying DTB time during PCI. Knowledge of the existing DTB time and its determinants can help us formulate new action plans to further lower the time enabling effective patient care and outcome after primary angioplasty.
2. Methodology
A cross-sectional hospital-based study was conducted at Shahid Gangalal National Heart Center, Bansbari. The study was approved by the institutional review committee and fulfills ethical principles according to the Declaration of Helsinki. All patients undergoing primary angioplasty from July 2017 to October 2017 were included. Patients who underwent rescue PCI and elective PCI were excluded. DTB time was defined as the difference in time from the time of ballooning to the time of patient arrival at the emergency room. Catheterization laboratory entry time was recorded in a catheterization laboratory, and the time of the first shot of contrast was recorded as the first shot time. First shot-to-ballooning time was recorded. Ballooning time was the time at which the balloon dilated the stenotic or blocked target lesion. The radial approach was the first approach used, and the femoral approach was used only when necessary or if the transradial approach failed. Data collection was performed in proforma after due consent. All data were tabulated using Excel. Continuous variables were expressed as mean with standard deviation or median and interquartile range, if data were skewed. Categorical variables were expressed in percentages and were compared using chi-square test. Nonparametric data were calculated using independent sample Mann–Whitney U test. Differences were considered to be statistically significant if p < 0.05.
3. Results
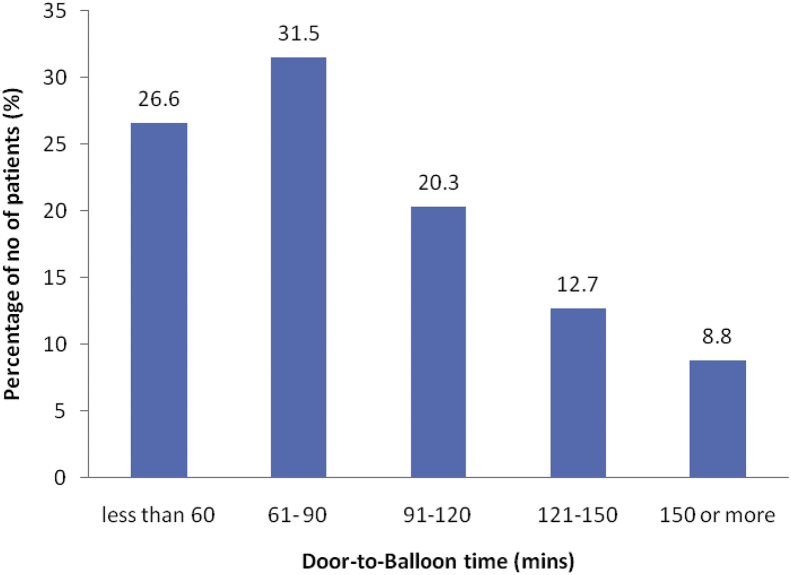
Seventy-nine patients undergoing primary percutaneous intervention were studied in 3 months time. The median DTB time was 79 min (interquartile range [IQR] 59–115 min). Forty-six (58.2%) patients had DTB time less than 90 min. The different time intervals of patients who had undergone primary angioplasty were recorded and are listed in Table 1. The distribution of percentage of patients according to DTB time is shown in Fig. 1.
Table 1.
Parameters of door-to-balloon time.
| Parameters | Median time (minutes) | Interquartile range (IQR)a |
|---|---|---|
| Median DTB time | 79 | 59–115 |
| Door-to-ECG time | 2 | 1–2 |
| Door-to-catheterization laboratory entry time | 55 | 38–83 |
| Catheterization laboratory entry time to first shot time | 6 | 4–9 |
| First shot-to-balloon time | 13 | 10–18 |
DTB, door-to-balloon; ECG, electrocardiogram.
IQR is 25th–50th percentile.
Fig. 1.
Distribution of patients according to door-to-balloon time.
No significant differences according to age, gender, hypertension, diabetes, and heart failure were seen between patients with DTB time less than or more than 90 min (Table 2). DTB time varied significantly for direct visit vs. transfer visit and office time (9 am–5 pm) vs. off time (5 pm–9 am). Fifty-six (70.9%) patients had radial access, and 23 (29.1%) patients had femoral access. The median DTB time during radial access was 73 (IQR 59–110) and during femoral access was 99 min (IQR 71–116). DTB time did not differ based on infarct-related vessels, number of vessels involved, and the added procedures (defibrillation, thrombosuction, and temporary pacemaker) during angioplasty (Table 3).
Table 2.
Baseline characteristics of patients.
| Baseline characteristics | Door-to-balloon < 90 min; n = 46 (58.2%) | Door-to-balloon ≥90 min; n = 33 (41.8%) | Overall median door-to-balloon time minutes (IQR) | p value* |
|---|---|---|---|---|
| Age (years) | ||||
| <50 | 12 (26) | 12 (36.3) | 94 (60–127) | 0.599 |
| ≥50 | 34 (73.9) | 21 (63.6) | 75 (59–109) | |
| Gender | ||||
| Male | 40 (86.9) | 26 (78.7) | 74.5 (58–115) | 0.254 |
| Female | 6 (13) | 7 (21.2) | 95 (73–120) | |
| Medical factors | ||||
| Diabetes | 14 (30.4) | 11 (33.3) | 85 (54–114) | 0.487 |
| Hypertension | 31 (67.3) | 16 (48.4) | 75 (59–105) | 0.073 |
| Heart failure | 8 (17.3) | 8 (24.2) | 91.5 (58–133) | 0.316 |
| ER visit time | ||||
| Office time | 21 (45.6) | 6 (18.1) | 64 (51–85) | 0.012∗ |
| Off time | 25 (54.3) | 27 (81.8) | 96 (67–128) | |
| Types of visit | ||||
| Direct | 4 (8.6) | 9 (27.2) | 109 (78–160) | 0.029∗ |
| Transfer | 42 (91.3) | 24 (72.7) | 73 (56–107) | |
IQR, interquartile range; ER, emergency room.
∗Significant (p < 0.05).
Table 3.
Procedural characteristics of the study population.
| Parameters | Door-to-balloon time <90 min; n = 46 (58.2%) | Door-to-balloon time ≥90 min; n = 33 (41.8%) | Overall median door-to-balloon time minutes (IQR) | p value* |
|---|---|---|---|---|
| No. of vessels | ||||
| SVD | 32 (69.6) | 25 (75.8) | 77 (59–113) | 0.638 |
| DVD | 13 (28.3) | 6 (18.2) | 79 (54–115) | |
| TVD | 1 (2.1) | 2 (6) | 97 (78–115) | |
| Infarct-related vessels | ||||
| RCA | 18 (39.1) | 16 (48.5) | 81.5 (58–126) | 0.471 |
| LCx | 4 (8.7) | 2 (6.0) | 72 (53–154) | |
| LAD | 24 (52.2) | 15 (45.5) | 79 (62–108) | |
| Additional procedure (TPI/defibrillator/thrombosuction) | 12 (26) | 10 (38.5) | 84 (55–126) | 0.682 |
IQR, interquartile range; DVD, double-vessel disease; LAD, left anterior descending artery; LCx, left circumflex artery; RCA, right coronary artery; SVD, single-vessel disease; TPI, temporary pacemaker insertion; TVD, triple-vessel disease.
*Significant (p < 0.05).
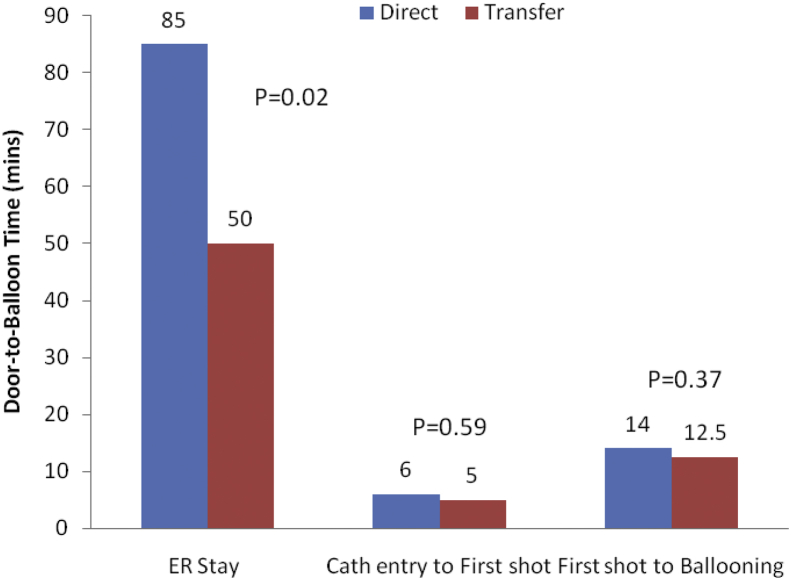
3.1. Direct vs. transfer patients
The median DTB time in patients directly coming to hospital was 109 min (IQR 78–160). Sixty-six (83.5%) patients visited as transfer patients from other centers. The median DTB time in transfer patients was 73 min (IQR 56–107). The time of emergency room stay, catheterization entry and first shot, and the first shot-to-ballooning is shown in Fig. 2.
Fig. 2.
Variations of door-to-balloon time in direct vs. transfer patients.
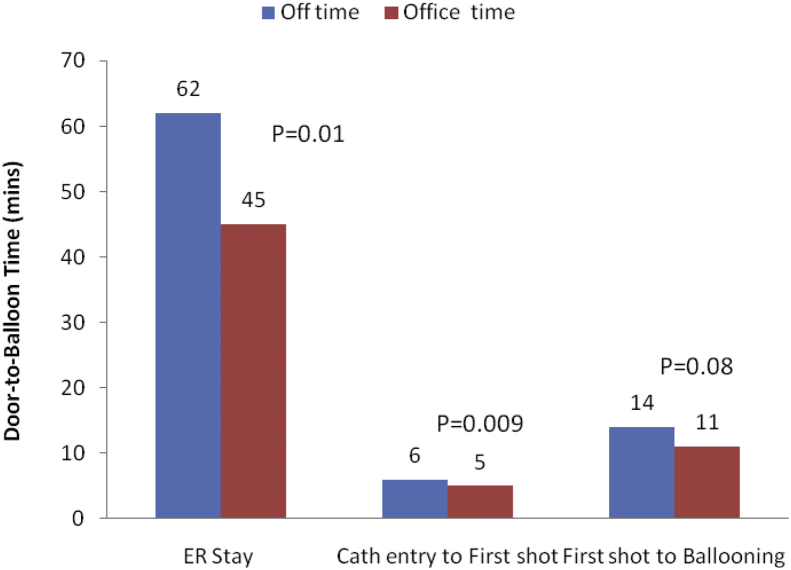
3.2. Office time (9 am–5 pm) vs. off time (5 pm–9 am)
Twenty-seven patients (34.1%) visited in office hours (9 am–5 pm), while 52 (65.8%) patients visited in off hours (5 pm–9 am). The median DTB time during office hours was 64 min (IQR 51–85) and during off hours was 96 min (IQR 67–128). The time of emergency room stay, catheterization entry and first shot, and the first shot to ballooning is shown in Fig. 3.
Fig. 3.
Variations of door-to-balloon time according to office hours vs. off hours.
4. Discussion
The median DTB time in our study was 79 min, which is as per the guidelines of the American College of Cardiology and American Heart Association stating the time should be 90 min or less.2, 3 The required time was similar to other contemporary studies describing the range between 67 and 110.3 min.5, 11, 12, 13 The percentage of patients meeting DTB time (<90 min) in this study was 58.2%, which was also within the range of 57.9%–83.1% as in other reported studies.5, 11, 12
The median DTB time for the transfer patients from clinics or other hospitals was less by 36 min when compared with those directly visiting the emergency room. Wang et al14 had reported the DTB time of 79 min vs. 36 min for such patients. Kim et al have also described the time for transfer patient to be less than the direct ER-attending patients (75 vs. 91 min).15 DTB in transfer patients had been taken from the door entry in our hospital and not from the door entry of the first contact of the referral doctor or hospital. Some other studies have calculated such time and had increased DTB time in transfer patient compared with the direct ER-visiting patients.16 The patients directly visiting the ER spent extra time in the ER for carrying out investigations, giving consent, and clearing financial bills for interventions. There was no significant difference in the procedure time calculated from catheterization laboratory entry to ballooning and first shot to ballooning between the two groups. Shorter DTB time in the transfer patients was because of shorter stay in the ER, which was because of prompt consent and early financial clearance. This might be because of the counseling of possibility of PCI and its cost by the primary physicians and the referring hospitals, so that patients and their family members had adequate time for required preparation.
DTB time was found to be less in the patients visiting during office hours than in those visiting during off time.17 Garceau et al observed a 16-min treatment delay in office on and off hours.16 Graham et al18 has described the median DTB time of 72 min in the working hours group while it was 80 min in the after-hours group (p = 0.007). This difference was primarily because of the availability of a primary operator in the office. Also, the excess working manpower during the office hours in catheterization laboratory, emergency room, and billing section could be the reasons. The time taken for the financial clearance and patient consent was also less during the day than at night. The ER stay, door-to-first shot, and the first shot-to-ballooning time were all shorter in office hours than in off time period.
Patients had to spend the median time of 6 min (IQR 4 to 9) in the catheterization laboratory before the first shot. This difference in the time of catheterization entry to first shot was less for the radial access compared with the femoral access, which in turn resulted in a significant difference in the overall DTB time. The approach in our catheterization laboratory was radial first followed by femoral approach if radial approach failed. The femoral approach first was used for heart block where temporary pacemaker was needed or in cardiogenic shock patients. The added procedure time because of any added intervention (thrombosuction, defibrillation, temporary pacemaker insertion) did not change the overall DTB time in the study. Tayeh and Ettori19 have reported nonsignificant differences (p = 0.522) in total DTB time and in catheterization entry to ballooning time between the two approaches. The procedure time in our study was nonsignificantly higher in the radial approach than in the femoral approach. This longer time for the radial approach has also been described by Karrowni et al.20
The DTB time did not vary with associated hypertension, diabetes, heart failure, left ventricular ejection fraction, and the type of infarct artery. The finding is similar to the study by Alla Lubovich et al.21 The finding by Rathore et al for relation of DTB with diabetes, hypertension, and left ventricular ejection fraction and for infarct-related vessel contradicts our finding.5
The knowledge of DTB time from the study will help the institution in auditing different delays by developing mechanism in delivering guideline-guided timely services, which include time to electrocardiogram (ECG), catheterization laboratory team activation, patients transfer time to catheterization laboratory, and procedure time. This highlights the importance of the active and mutual participation of the referring doctors and hospitals with the team of receiving hospitals to decrease the door in and out time, so the patient can receive early revascularization therapy. The communication between the referring doctors and the operating interventionists can activate the catheterization team and lessen the DTB time for angioplasty. Extensive campaigning about the knowledge and importance of symptoms of coronary artery disease, accessible ECG facilities in community, and affordable emergency revascularization therapy in hospitals can help in mitigating patient-induced decision delay in DTB time.
The limitations of the study were the outcome of the study with time had not been done. The time record if calculated electronically can alter any time bias of the observer. Similarly, only patients who undergo Primary PCI were enrolled as this can cause selection bias. The increase in size of the sample and the duration of the study can give a more accurate result.
5. Conclusion
The median DTB time in primary angioplasty was less than 90 min. The significant determining factors were the timing of hospital visit (office vs. off time) and the types of visit (direct vs. transfer). There can be improvement in factors determining DTB time to lower it further.
Conflict of interest
All authors have none to declare.
Acknowledgments
The authors would like to acknowledge other cardiologists, medical officers, catheterization laboratory technicians, nursing staffs, and attendants who worked day and night at Shahid Gangalal National Heart Center.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ihj.2018.07.011.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Keeley E.C., Boura J.A., Grines C.L. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet (Lond Engl) 2003;361(9351):13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 2.O'Gara P.T., Kushner F.G., Ascheim D.D. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2013;61:485–510. doi: 10.1016/j.jacc.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 3.Steg P.G., James S.K., Atar D. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33:2569–2619. doi: 10.1093/eurheartj/ehs215. [DOI] [PubMed] [Google Scholar]
- 4.Cannon C.P., Gibson C.M., Lambrew C.T. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283:2941–2947. doi: 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 5.Rathore S.S., Curtis J.P., Chen J. Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ (Clin Res Ed) 2009;338:b1807. doi: 10.1136/bmj.b1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McNamara R.L., Wang Y., Herrin J. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47:2180–2186. doi: 10.1016/j.jacc.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 7.Berger P.B., Ellis S.G., Holmes D.R., Jr. Relationship between delay in performing direct coronary angioplasty and early clinical outcome in patients with acute myocardial infarction: results from the global use of strategies to open occluded arteries in Acute Coronary Syndromes (GUSTO-IIb) trial. Circulation. 1999;100:14–20. doi: 10.1161/01.cir.100.1.14. [DOI] [PubMed] [Google Scholar]
- 8.Rathore S.S., Curtis J.P., Nallamothu B.K. Association of door-to-balloon time and mortality in patients ≥65 Years with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. J Am All Cardiol. 2009;104:1198–1203. doi: 10.1016/j.amjcard.2009.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Luca G., Suryapranata H., Ottervanger J.P., Antman E.M. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 10.Brodie B.R., Hansen C., Stuckey T.D. Door-to-Balloon time with primary percutaneous coronary intervention for acute myocardial infarction impacts late cardiac mortality in high-risk patients and patients presenting early after the onset of symptoms. J Am Coll Cardiol. 2006;47:289–295. doi: 10.1016/j.jacc.2005.08.065. [DOI] [PubMed] [Google Scholar]
- 11.Menees D.S., Peterson E.D., Wang Y. Door-to-balloon time and mortality among patients undergoing primary PCI. N Eng J Med. 2013;369:901–909. doi: 10.1056/NEJMoa1208200. [DOI] [PubMed] [Google Scholar]
- 12.Victor S.M., Gnanaraj A., V S., Pattabiram S., Mullasari A.S. Door-to-balloon: where do we lose time? Single centre experience in India. Indian Heart J. 2012;64:582–587. doi: 10.1016/j.ihj.2012.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Secco G.G., Marinucci L., Uguccioni L., Parisi R., Uguccioni S., Fattori R. Transradial versus transfemoral approach for primary percutaneous coronary interventions in elderly patients. J Invasive Cardiol. 2013;25(5):254–256. [PubMed] [Google Scholar]
- 14.Wang T.Y., Peterson E.D., Ou F.S., Nallamothu B.K., Rumsfeld J.S., Roe M.T. Door-to-balloon times for patients with ST-segment elevation myocardial infarction requiring interhospital transfer for primary percutaneous coronary intervention: a report from the national cardiovascular data registry. Am Heart J. 2011;161:76–83.e1. doi: 10.1016/j.ahj.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 15.Kim B.W., Cha K.S., Park M.J. The impact of transferring patients with ST-segment elevation myocardial infarction to percutaneous coronary intervention-capable hospitals on clinical outcomes. Cardiol J. 2016;23:289–295. doi: 10.5603/CJ.a2016.0003. [DOI] [PubMed] [Google Scholar]
- 16.Garceau P., Déry J.-P., Lachance P. Treatment delays in patients undergoing primary percutaneous coronary intervention for ST elevation myocardial infarction at the Quebec Heart and Lung Institute. Can J Cardiol. 2007;23(suppl B):53B–57B. doi: 10.1016/s0828-282x(07)71011-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abrich V.A., Rokey R., Bhupathi S.S.V., Mesa J.E. Variability of door-to-device times at a rural tertiary care center. J Clin Med Res. 2014;12:138–146. doi: 10.3121/cmr.2014.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Graham M.M., Ghali W.A., Southern D.A., Traboulsi M., Knudtson M.L. Outcomes of after-hours versus regular working hours primary percutaneous coronary intervention for acute myocardial infarction. BMJ Qual Safety Health Care. 2011;20:60–67. doi: 10.1136/bmjqs.2010.041137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tayeh O., Ettori F. Door-to-balloon time in radial versus femoral approach for primary percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction. EHJ. 2014;66:155–162. [Google Scholar]
- 20.Karrowni W., Vyas A., Giacomino B. Radial versus femoral access for primary percutaneous interventions in ST-segment elevation myocardial infarction patients: a meta-analysis of randomized controlled trials. JACC Cardiovasc Interv. 2013;6:814–823. doi: 10.1016/j.jcin.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 21.Lubovich A., Hamood H., Behar S., Rosenschein U. Bypassing the emergency room to reduce door-to-balloon time and improve outcomes of patients with ST elevation myocardial infarction: the Acute Coronary Syndrome Israeli Survey experience. Isr Med Assoc J. 2011;13:216–219. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.