Abstract
Background
Depression in congestive heart failure (CHF) patients can increase morbidity and mortality. Given the ever-rising prevalence of CHF patients with depression, it is vital that we understand the predictors of depression in these patients to identify and better manage these patients. The main objective of this study was to evaluate the frequency and predictors of depression in CHF patients.
Methods
A cross-sectional study was conducted in a tertiary care hospital. Patients with a diagnosis of CHF for more than 6 months based on signs and left ventricular ejection fraction <40% were included. Patients were interviewed with the Patient Health Questionnaire-9 (PHQ-9) consisting of nine items in line with the Diagnostic and Statistical Manual (DSM) - IV criteria to assess depression. Each item was scored from 0 to 3, and a PHQ-9 score of 10 or greater suggested clinical depression. Data were analyzed on SPSS, v22, and a p < 0.05 was considered significant.
Results
Of 170 participants, 102 (60%) had depression. Among these 102 patients, 42% (n = 43) had mild depression, and the rest (n = 59) had moderate-to-severe depression. Predictors of depression were New York Heart Association stage 3 or 4 (p = 0.001), previous myocardial infarction (p = 0.001), living without a partner (p = 0.001), lack of a joint family system (p = 0.001), sedentary lifestyle (p = 0.001), aged 70 years or more (p = 0.01), and having been admitted in a hospital at least once in the past two months (p = 0.002).
Conclusion
Depression is common among patients with CHF. It is associated with multiple factors and needs to be addressed and targeted urgently.
Keywords: Depression, Congestive heart failure, NYHA classification
1. Introduction
Depression is five times more prevalent in heart failure patients than in the general population.1, 2 Depressive symptoms contribute to increased health-care costs,3 hospitalizations,4 worsening of heart failure symptoms,4 and deaths.2, 5, 6 Moreover, it has been reported that depression in heart failure patients is related to diminished quality of life,4, 7 functional decline,8 physical and social limitations,4 and worsening of New York Heart Association (NYHA) functional classification.1, 8 The worldwide prevalence is variable, although data is scarce from developing countries. A study from Pakistan reported that 30% of patients had depression in chronic heart failure.9
Such data suggest that by understanding the predictors of depressive symptoms, we may be able to identify CHF patients who are at higher risk of morbidity and establish interventions targeted at improving and/or preventing further depression. In Pakistan, hospitalizations due to CHF are increasing at an alarming rate.10
Considering the increasing prevalence of cardiovascular diseases, determining the risk factors for developing depression in patients with heart failure is vital. The aim of the present study was to identify the factors associated with depressive symptoms in CHF patients. Furthermore, we sought to determine the prevalence of depression among patients with CHF.
2. Materials and methods
This cross-sectional study was conducted during February 2017 after approval from the Institutional Review Board of Dow University of Health Sciences. Recruited participants were heart failure patients who visited the clinics for follow-up of CHF in Karachi. The patients diagnosed with CHF for more than 6 months as documented in their medical records by echocardiography with the left ventricular ejection fraction (LVEF) < 40% were included. Exclusion criteria were as follows: having an implantable cardioverter-defibrillator (ICD), suicidal ideations, end-stage liver disease, severe debilitating conditions, recent major surgeries, current hospitalization, and pregnancy.
Face-to-face interviews were conducted by interns or medical students who were specially trained before the formal start of this investigation. To check inter-rater reliability, randomly selected participants were interviewed for the second time by a different or the same interviewer, and the scores were compared and analyzed ensuring no significant difference existed in the ratings. Questionnaires were read to participants, and their answers were recorded, although no assistance was provided in deciding which response was to be given. Each participant signed a consent form before data collection. Information on age, sex, marital status, income level in Pakistani rupees, education level, number of hospital readmissions, and mean time since diagnoses were collected. Patients earning less than 10,000 Pakistani rupees monthly were categorized as having a low socioeconomic status. Hospital readmission was specified for exacerbation of symptoms of CHF within the last two months.
All interviewers used standard questions and were blinded to the aforementioned data. Apart from this, recall bias was reduced by asking questions in the questionnaire about an easily recallable time period. Furthermore, imputation method was avoided, and incomplete questionnaires were discarded. Unhealthy eating behaviors (≥3 times/week) were defined based on a standard lifestyle questionnaire,11 which was developed by the Japan Ministry of Health, Labor and Welfare and is widely used for specific health checkups (Tokutei Kenshin) in Japan.
Sedentary behavior was assessed using the Past-day Adults' Sedentary Time (PAST) questionnaire.12 The PAST is a seven-item instrument that uses past-day recall of sedentary time. It asks about time spent sitting or lying (while awake) on the previous day with questions about time spent sitting or lying while at work, traveling, watching television, using the computer (excluding work), reading (excluding work), hobbies, and any other purposes not reported in the previous items. The PAST questionnaire has been found to have acceptable reliability and validity.13
The NYHA functional classification14 was carried out based on participants' severity of limitation. It ranges from I (no limitation of physical activity) to II (slight limitation in physical activity; comfortable at rest, but moderate physical activity results in limitation) to III (marked limitation of physical activity; symptoms are caused by less than ordinary activities) to IV (unable to carry on any physical activity without discomfort). Total scores were calculated using a weighted score for each activity; lower total scores indicate worse functional status.
Depressive symptoms were assessed with the Patient Health Questionnaire-9 (PHQ-9).15 The PHQ-9 consists of nine items in line with the DSM-IV criteria for major depression (i.e. loss of interest, feeling down, sleeping problems, loss of energy, appetite change, feelings of failure, trouble concentrating, psychomotor change, and suicidal ideations).16 Each item is scored on a scale from 0 (not at all) to 3 (nearly every day) with a total score ranging from 0 to 27. PHQ-9 scores suggest mild (less than 5), moderate (5–9), moderately severe (10–14), and severe (15 or more) depression.
Data were analyzed using International Business Machines Corporation's Statistical Package for the Social Sciences (IBM-SPSS), version 22. Patient characteristics were represented using means and standard deviations (SD) for continuous variables and frequency distributions for categorical variables. Independent t-tests and chi-square tests were used as the primary statistical tests. A p value of less than 0.05 was considered significant at a 95% confidence level for all cases.
3. Results
Out of the 170 patients, 133 (78.2%) had ischemia as the primary cause of CHF. Around one-fourth of the patients (n = 44, 25.9%) were hospitalized at least once within the last two months. Mean duration of CHF was 4.6 years (SD = 3.3). The mean age of the sample was 64.3 years (SD = 9.6) with 125 being (73.5%) men. Nearly one-third (n = 53, 31.2%) of the sample had no education. About half (n = 73, 43%) of the sample reported being current smokers, whereas a very small percentage of the sample drank alcohol (n = 13, 7.6%). Most (n = 67, 39.4%) of the patients had moderate NYHA symptom severity scores. History of diabetes, hypertension, hyperlipidemia, previous stroke and previous myocardial infarction (MI) along with other baseline demographic and clinical characteristics are shown in Table 1.
Table 1.
Baseline characteristics.
| Characteristics | Frequency (n = 170) |
|---|---|
| Age, mean ± SD (years) | 64.3 ± 9.6 |
| Males | 125 (73.5) |
| Married | 136 (80.0) |
| Joint family system | 87 (51.2) |
| Low socioeconomic status | 104 (61.2) |
| No education | 53 (31.2) |
| NYHA class 3 or 4 | 67 (39.4) |
| Hypertensive | 103 (60.5) |
| Diabetic | 98 (57.6) |
| Smoking | 73 (42.9) |
| Alcoholic | 13 (7.6) |
| Previous myocardial infarction | 79 (46.4) |
| Ischemic cause of congestive heart failure | 133 (78.2) |
| Previous stroke | 24 (14.1) |
| Taking ACE inhibitors | 149 (87.6) |
| Taking beta blockers | 102 (60.0) |
| Hyperlipidemia | 92 (54.1) |
| Mean duration of CHF ± SD (years) | 4.6 ± 3.3 |
| At least 1 hospital readmission for HF in the past 2 months | 44 (25.9) |
| Unhealthy dietary habits | 52 (30.6) |
| Sedentary lifestyle | 91 (53.5) |
SD, standard deviation; NYHA, New York Heart Association; ACE, angiotensin converting enzyme.
Continuous variables are reported as mean ± SD.
Categorical variables are reported as n (%).
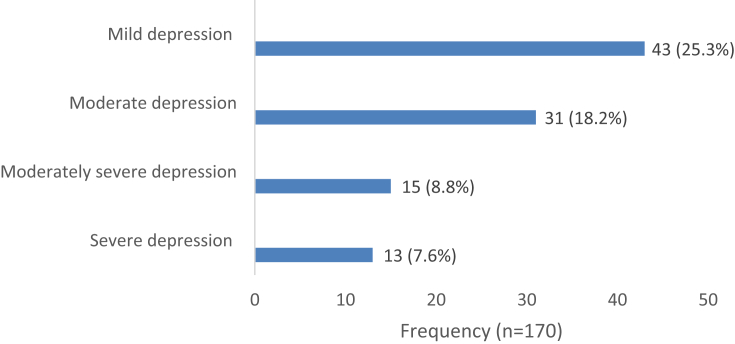
Fig. 1 shows the proportion of the CHF patients with mild depression (n = 43, 42.2%), moderate depression (n = 31, 30.4%), moderately severe depression (n = 15, 14.7%), and severe depression (n = 13, 12.7%) as per the PHQ-9 scoring scale.
Fig. 1.
Frequency of depression.
Table 2 shows the predictors of depression. NYHA stage 3 or 4 (p = 0.001), previous MI (p = 0.001), living without a partner (p = 0.001), lack of a joint family system (p = 0.001), and sedentary lifestyle (p = 0.001) were significantly associated with depression. Older than 70 years (p = 0.01) and hospitalization (p = 0.002) within the past 2 months were also predictors of depression. Furthermore, low socioeconomic status (p = 0.84), no education (p = 0.78), smoking (p = 0.48), and unhealthy dietary habits (p = 0.78) were not significantly related with depression.
Table 2.
Comparison of characteristics between patients with depression and without depression.
| Characteristics | Depression (n = 102, %) | No depression (n = 68, %) | p-value |
|---|---|---|---|
| Age > 70 years | 38 (37.3) | 11 (16.2) | 0.01 |
| Males | 75 (73.5) | 50 (73.5) | 0.99 |
| NYHA Class 3 or 4 | 51 (50.0) | 16 (23.5) | ∗0.001 |
| Previous myocardial infarction | 65 (63.7) | 14 (20.6) | ∗0.001 |
| Hyperlipidemia | 56 (54.9) | 36 (52.9) | 0.8 |
| Diabetes mellitus | 73 (71.6) | 45 (66.2) | 0.45 |
| Single/divorced/widowed | 31 (30.4) | 3 (4.4) | ∗0.001 |
| Low socioeconomic status | 63 (61.8) | 41 (60.3) | 0.84 |
| Joint family system | 33 (32.4) | 54 (79.4) | ∗0.001 |
| Hospital readmission | 35 (34.3) | 9 (13.2) | 0.002 |
| No education | 31 (30.4) | 22 (32.4) | 0.78 |
| Hypertension | 65 (63.7) | 38 (55.9) | 0.3 |
| Smoking | 46 (45.1) | 27 (39.7) | 0.48 |
| Unhealthy dietary habits | 32 (31.4) | 20 (29.4) | 0.78 |
| Sedentary lifestyle | 67 (65.7) | 24 (35.3) | ∗0.001 |
NYHA, New York Heart Association.
∗p value < 0.001.
To further examine the relationship between the severities of depression, we divided the sample into subgroups namely moderately severe/severe depression and mild/moderate depression as shown in Table 3. Most significant associations observed did not remain significant for the greater severity of depression, except for associations of NYHA stage 3 or 4 (p = 0.001) and hospital readmission (p = 0.001). Specifically, associations with severe depression were nonsignificant in patients older than 70 years and those living in a joint family system.
Table 3.
Predictors of severe depression.
| Variable | Moderately severe/severe depression (n = 28) | Mild/moderate depression (n = 74) | p-value |
|---|---|---|---|
| Age >70 years | 9 (32.1) | 29 (39.2) | 0.51 |
| NYHA 3 or 4 | 23 (82.1) | 28 (37.8) | 0.001* |
| Previous MI | 22 (78.6) | 43 (58.1) | 0.05 |
| Joint family system | 7 (25.0) | 26 (35.1) | 0.32 |
| Hospital readmission | 25 (89.3) | 10 (13.5) | 0.001* |
| Sedentary lifestyle | 15 (53.6) | 52 (70.3) | 0.11 |
NYHA, New York Heart Association; MI, myocardial infarction.
Categorical variables are reported as n (%).
*p value < 0.001.
4. Discussion
The growing recognition of depression as a potential cause of morbidity and mortality in heart failure patients has led to the increasing assessment of prevalence of depression in such patients. The prevalence of depression has been shown to be extremely high in the present study, with 60% of the participants being labeled as depressed. Previous studies have recorded varying prevalence ranging from 9% to 60%17 in small studies; however, to the best of our knowledge, this is the largest study to include postdischarge patients (n = 170).
Co-morbidities such as depression make treatment more difficult and worsen the prognosis-increasing NYHA class, hospitalization, and mortality rate.18, 19 The prevalence of depression is three-fold higher in CHF patients than in the healthy population.18, 19 A previous study demonstrated how depressive symptoms developed in 22% of CHF patients without depression at discharge20 which partly explains that depression is more common in CHF patients. The definite mechanism which causes depression in CHF patients is not exactly known, yet the raised levels of catecholamines, cortisol, and inflammatory cytokines (IL-6, IL-1β, and TNF-α) in both the diseases might somewhat explain the pathophysiology.18
Four different mechanisms have been proposed for the progression of CHF in depressed patients: first, hypersecretion of cortisol and sympathetic hyperactivity in response to hypothalamic stimulation; second, reduced parasympathetic response leading to increased chances of arrhythmias; third, rise in proinflammatory cytokines causing inflammation; and fourth, hypercoagulability due to defective platelet activation.21 CHF is a multiorgan disorder involving skeletal, renal, neuroendocrine, and immune systems along with the heart. Cytokines such as TNF-α, IL-1, IL-6, and macrophage chemo-attractant protein (MCP)-1 play a significant role in its development.22 Similarly, depression and emotional distress have also been linked to abnormal immune responses peripherally and increased expression of proinflammatory cytokines which profoundly affects the brain and peripheral serotonin-mediated systems.23
There were eight risk factors associated with depression in CHF patients that were identified: age, previous MI, NYHA stage 3 or 4, living without a partner, absence of a joint family system, sedentary lifestyle, hospitalization within the past 2 months, and hospital readmission. The results were in line with a similar study which found a significant relation of previous ischemic heart disease, participation restriction, and lack of satisfaction with social support with depression.20 The study predicted that the presence of these three risk factors alone increases the risk of developing depressive symptoms by 70%, and patients are likely to develop such symptoms in one year.20 Unlike other studies on heart failure patients, our cross-sectional study evaluated patients in their postdischarge period of greater than 6 months, with different clinical, social, and economic settings.
The consideration of living without a partner and social isolation has been associated with depression in the senior age group.24 However, data in relation to heart failure patients is limited.21 Our study found that being single and not living in a joint family is significantly associated with depression. This was corroborated by a study which found that living alone is a significant predictor of depressive symptoms in heart failure patients who followed up after a year.25 Nonetheless, a study by Shimizu et al in 201420 did not find the same relation to be significant. Although some individuals might be depressed due to lack of support because of being single or not living with family, other individuals find it positive to live alone, which explains how depression is a subjective phase which develops when level of relationship does not meet one's desire to bond.26
Although social isolation, poor health and decreased strength, and demise of friends might be contemplated as a cause of depression in the elderly, more individuals in the younger age group (<70 years) were found to have depression. This is in line with a study by Gottlieb et al27 which found similar results. A possible explanation is that heart failure (HF) affects their quality of life physically and emotionally, as it is harder for the younger ones to accept those restraints. As far as gender is concerned, literature reveals that women are more likely to be depressed than men be it general population28, 29, 30, 31 or HF patients.17, 27, 32 On the contrary, our study found depression to be more prevalent in men.
NYHA class, which is consistent with the severity of disease, is another factor that was significantly associated with depression in the study participants, and this was consistent with the findings of a meta-analysis performed in 2006.2 Moreover, it has been demonstrated that patients with NYHA class 3 and 4 are more likely to be depressed.27 Our study is analogous as it shows this group as having moderate to severe depression rather than mild to moderate depression, and the difference is significant. Smoking33, 34 and hypertension27 have previously been shown to be strongly associated with depression implying reduced desire for self-care and drug compliance, but it was not a significant predictor of depression in the heart failure patients studied in this study.
Feola et al, in one of the largest clinical studies in this area, found a significantly positive correlation between mini-mental state examination (MMSE), age, and brain natriuretic peptide (BNP), concluding that older CHF patients with a higher BNP plasma level had significant cognitive impairment.35 It also found a significant association of depression in the elderly with increasing NYHA class in heart failure patients.35 The pathophysiology behind cognitive dysfunction, however, remains unclear; it might be related to pump failure36 or decreased blood supply to the brain.37 On the other hand, depressive mood with higher NYHA class reflects how severe CHF causes functional impairment resulting in depression, and depression in turn might worsen the symptoms of CHF improving the severity of functional impairment.35
The consequences of depression cannot be overlooked. It has been found to lower the quality of life and the survival rate.18 All-cause mortality increases in patients with ejection fraction ≤35%,38 and depression is found to be the most important risk factor for HF symptoms, physical and social functions, quality of life, and short-term worsening in health status.4 Depression also adversely affects the autonomic system; the sympathetic system becomes overactive, causing tachycardia, decreasing heart rate variability, and lowering the threshold for ischemic attack.39, 40 As proven experimentally, heart failure causes a rise in the natriuretic peptides in brain41 which antagonizes blood pressure regulation and fluid neurotransmission in HF and thus are responsible for mental and emotional changes.42, 43 Furthermore, depression increases hospital readmission and mortality in HF patients.44
Accordingly, studies have suggested that treatment of depression can decrease morbidity and mortality in patients of HF.27 There is evidence indicating that medical costs are higher for depressed HF patients than their nondepressed HF counterparts.3 Hence, not just improving quality of life, treating depression also reduces health expenses incurred by these patients. However, it is still not known what the best pharmacological treatment of depression in HF patients should be. Variable pathogenesis of concomitant depression with inconstant predominance is a possible explanation why different treatment strategies have been irregularly unsuccessful. Depression, in turn, is associated with noncompliant attitude of patients with regard to pharmacologic and behavioral therapy.45
This study has several important clinical implications. Owing to the high prevalence of depression, screening of CHF patients for depression in the postdischarge phase is required. Identification and treatment of depression in such patients improves patient's compliance to the corresponding treatment. Literature proposes that programs for psychiatric management in CHF patients to treat depression after discharge can help improve the consequences on health.46, 47 Further multicenter studies are required on a larger scale and for a longer duration to assess the prevalence of depression in HF patients, the risk factors associated with it, and the effectiveness of screening and behavioral therapy programs in improving the health of patients.
4.1. Limitations
There are a few limitations in this study which need to be considered. Participants enrolled were from a single medical center. Different methods of assessing depression and the type of questionnaire used can create variations in the reported prevalence of depression. More studies are needed to clarify the extent to which these findings are generalizable to patients treated in other settings. In addition, this study was on CHF patients, who were diagnosed 6 months before; hence, the more acute CHF patients and their risk factors of depression could not be determined on the basis of this study. Additional research with a longer follow-up period is also needed to confirm our findings and to better evaluate the results. In addition, dependence of variation in each predictor through equal representation of each gender would have given a better picture and would have pointed out toward gender-specific interventions.
5. Conclusions
Depression is a common condition affecting CHF patients with NYHA stage 3 or 4, previous MI, living without a partner, sedentary lifestyle and age of 70 years or older as well as having been admitted in a hospital at least once in the past two months serving to be significant predictors of this condition.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
All authors have none to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ihj.2018.10.410.
Contributor Information
Ibrahim Zahid, Email: ibrahim_zahid@hotmail.com.
Mishall Ahmed Baig, Email: mishaalbaig@hotmail.com.
Jaleed Ahmed Gilani, Email: jaleedahmedgi16@gmail.com.
Nageen Waseem, Email: nageenwsm@gmail.com.
Shumaila Ather, Email: shumailaather14@gmail.com.
Aishath Shausha Farooq, Email: shaushafarooq@gmail.com.
Amna Ghouri, Email: amnaghouri@gmail.com.
Simra Nadeem Siddiqui, Email: simrasiddiqui1993@gmail.com.
Ram Kumar, Email: Ramlulla3553@gmail.com.
Sahil, Email: sahil200748@gmail.com.
Suman, Email: Sumandr632@gmail.com.
Raj Kumar, Email: Raj_karira@yahoo.com.
Ravi kumar, Email: ravi2671995@gmail.com.
Awais Ahmed Mulla, Email: awais.ahmed@gmail.com.
Rabbia Siddiqi, Email: rabbiasiddiqi@hotmail.com.
Kaneez Fatima, Email: kaneezfatima344@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Ghaemian A., Mohammadpour R.A., Hosseini S.H., Emadi S.H. Depression in heart failure patients and the influence of age, gender and severity of depression on heart failure patients. J Tehran Univ Heart Cent. 2007;2(1):31–34. [Google Scholar]
- 2.Rutledge T., Reis V.A., Linke S.E., Greenberg B.H., Mills P.J. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48(8):1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 3.Sullivan M., Simon G., Spertus J., Russo J. Depression-related costs in heart failure care. Arch Intern Med. 2002;162(16):1860–1866. doi: 10.1001/archinte.162.16.1860. [DOI] [PubMed] [Google Scholar]
- 4.Rumsfeld J.S., Havranek E., Masoudi F.A. Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J Am Coll Cardiol. 2003;42(10):1811–1817. doi: 10.1016/j.jacc.2003.07.013. [DOI] [PubMed] [Google Scholar]
- 5.Jiang W., Alexander J., Christopher E. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161(15):1849–1856. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- 6.Sherwood A., Blumenthal J.A., Trivedi R. Relationship of depression to death or hospitalization in patients with heart failure. Arch Intern Med. 2007;167(4):367–373. doi: 10.1001/archinte.167.4.367. [DOI] [PubMed] [Google Scholar]
- 7.Carels R.A. The association between disease severity, functional status, depression and daily quality of life in congestive heart failure patients. Qual Life Res. 2004;13(1):63–72. doi: 10.1023/B:QURE.0000015301.58054.51. [DOI] [PubMed] [Google Scholar]
- 8.Vaccarino V., Kasl S.V., Abramson J., Krumholz H.M. Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol. 2001;38(1):199–205. doi: 10.1016/s0735-1097(01)01334-1. [DOI] [PubMed] [Google Scholar]
- 9.Khan S., Khan A., Ghaffar R., Awan Z.A. Frequency of depression in patients with chronic heart failure. J Ayub Med Coll Abbottabad. 2012;24(2):26–29. [PubMed] [Google Scholar]
- 10.Noor L., Adnan Y., Khan S.B. Inpatient burden of heart failure in the cardiology units of tertiary care hospitals in Peshawar. Pak J Physiol. 2012;8(1) [Google Scholar]
- 11.Huang C., Momma H., Cui Y. Independent and combined relationship of habitual unhealthy eating behaviors with depressive symptoms: a prospective study. J Epidemiol. 2017;27(1):42–47. doi: 10.1016/j.je.2016.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clark B.K., Winkler E., Healy G.N. Adults' past-day recall of sedentary time: reliability, validity, and responsiveness. Med Sci Sports Exerc. 2013;45(6):1198–1207. doi: 10.1249/MSS.0b013e3182837f57. [DOI] [PubMed] [Google Scholar]
- 13.Sylvia L.G., Bernstein E.E., Hubbard J.L., Keating L., Anderson E.J. Practical guide to measuring physical activity. J Acad Nutr Diet. 2014;114(2):199–208. doi: 10.1016/j.jand.2013.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kubo S.H., Schulman S., Starling R.C., Jessup M., Wentworth D., Burkhoff D. Development and validation of a patient questionnaire to determine New York Heart Association classification. J Card Fail. 2004;10(3):228–235. doi: 10.1016/j.cardfail.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 15.Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kohlmann S., Gierk B., Murray A.M., Scholl A., Lehmann M., Lowe B. Base rates of depressive symptoms in patients with coronary heart disease: an individual symptom analysis. PLoS One. 2016;11(5):e0156167. doi: 10.1371/journal.pone.0156167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Metra M., Gheorghiade M., Bonow R.O., Dei Cas L. Postdischarge assessment after a heart failure hospitalization: the next step forward. Circulation. 2010;122(18):1782–1785. doi: 10.1161/CIRCULATIONAHA.110.982207. [DOI] [PubMed] [Google Scholar]
- 18.DeJongh B., Birkeland K., Brenner M. Managing comorbidities in patients with chronic heart failure: first, do no harm. Am J Cardiovasc Drugs. 2015;15(3):171–184. doi: 10.1007/s40256-015-0115-6. [DOI] [PubMed] [Google Scholar]
- 19.Vongmany J., Hickman L.D., Lewis J., Newton P.J., Phillips J.L. Anxiety in chronic heart failure and the risk of increased hospitalisations and mortality: a systematic review. Eur J Cardiovasc Nurs. 2016;15(7):478–485. doi: 10.1177/1474515116635923. [DOI] [PubMed] [Google Scholar]
- 20.Shimizu Y., Suzuki M., Okumura H., Yamada S. Risk factors for onset of depression after heart failure hospitalization. J Cardiol. 2014;64(1):37–42. doi: 10.1016/j.jjcc.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Joynt K.E., Whellan D.J., O'Connor C.M. Why is depression bad for the failing heart? A review of the mechanistic relationship between depression and heart failure. J Card Fail. 2004;10(3):258–271. doi: 10.1016/j.cardfail.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 22.Anker S.D., von Haehling S. Inflammatory mediators in chronic heart failure: an overview. Heart. 2004;90(4):464–470. doi: 10.1136/hrt.2002.007005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pasic J., Levy W.C., Sullivan M.D. Cytokines in depression and heart failure. Psychosom Med. 2003;65(2):181–193. doi: 10.1097/01.psy.0000058372.50240.38. [DOI] [PubMed] [Google Scholar]
- 24.Djernes J.K. Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatr Scand. 2006;113(5):372–387. doi: 10.1111/j.1600-0447.2006.00770.x. [DOI] [PubMed] [Google Scholar]
- 25.Havranek E.P., Spertus J.A., Masoudi F.A., Jones P.G., Rumsfeld J.S. Predictors of the onset of depressive symptoms in patients with heart failure. J Am Coll Cardiol. 2004;44(12):2333–2338. doi: 10.1016/j.jacc.2004.09.034. [DOI] [PubMed] [Google Scholar]
- 26.Teo A.R., Choi H., Valenstein M. Social relationships and depression: ten-year follow-up from a nationally representative study. PLoS One. 2013;8(4):e62396. doi: 10.1371/journal.pone.0062396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gottlieb S.S., Khatta M., Friedmann E. The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol. 2004;43(9):1542–1549. doi: 10.1016/j.jacc.2003.10.064. [DOI] [PubMed] [Google Scholar]
- 28.Ernst C., Angst J. The Zurich Study. XII. Sex differences in depression. Evidence from longitudinal epidemiological data. Eur Arch Psychiatr Clin Neurosci. 1992;241(4):222–230. doi: 10.1007/BF02190257. [DOI] [PubMed] [Google Scholar]
- 29.Kornstein S.G. Gender differences in depression: implications for treatment. J Clin Psychiatr. 1997;58(Suppl 15):12–18. [PubMed] [Google Scholar]
- 30.Kornstein S.G., Schatzberg A.F., Yonkers K.A. Gender differences in presentation of chronic major depression. Psychopharmacol Bull. 1995;31(4):711–718. [PubMed] [Google Scholar]
- 31.Weissman M.M., Klerman G.L. Sex differences and the epidemiology of depression. Arch Gen Psychiatr. 1977;34(1):98–111. doi: 10.1001/archpsyc.1977.01770130100011. [DOI] [PubMed] [Google Scholar]
- 32.Angermann C.E., Gelbrich G., Stork S. Somatic correlates of comorbid major depression in patients with systolic heart failure. Int J Cardiol. 2011;147(1):66–73. doi: 10.1016/j.ijcard.2009.07.044. [DOI] [PubMed] [Google Scholar]
- 33.Cole M.G., Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. 2003;160(6):1147–1156. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- 34.Vink D., Aartsen M.J., Schoevers R.A. Risk factors for anxiety and depression in the elderly: a review. J Affect Disord. 2008;106(1-2):29–44. doi: 10.1016/j.jad.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 35.Feola M., Garnero S., Vallauri P. Relationship between cognitive function, depression/anxiety and functional parameters in patients admitted for congestive heart failure. Open Cardiovasc Med J. 2013;7:54–60. doi: 10.2174/1874192401307010054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Staniforth A.D., Kinnear W.J., Cowley A.J. Cognitive impairment in heart failure with Cheyne-Stokes respiration. Heart. 2001;85(1):18–22. doi: 10.1136/heart.85.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zuccala G., Cattel C., Manes-Gravina E., Di Niro M.G., Cocchi A., Bernabei R. Left ventricular dysfunction: a clue to cognitive impairment in older patients with heart failure. J Neurol Neurosurg Psychiatry. 1997;63(4):509–512. doi: 10.1136/jnnp.63.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Adelborg K., Schmidt M., Sundbøll J. Mortality risk among heart failure patients with depression: a nationwide population-based cohort study. J Am Heart Assoc Cardiovasc Cerebrovasc Dis. 2016;5(9):e004137. doi: 10.1161/JAHA.116.004137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carney R.M., Freedland K.E., Veith R.C. Depression, the autonomic nervous system, and coronary heart disease. Psychosom Med. 2005;67(Suppl 1):S29–S33. doi: 10.1097/01.psy.0000162254.61556.d5. [DOI] [PubMed] [Google Scholar]
- 40.Hughes J.W., Watkins L., Blumenthal J.A., Kuhn C., Sherwood A. Depression and anxiety symptoms are related to increased 24-hour urinary norepinephrine excretion among healthy middle-aged women. J Psychosom Res. 2004;57(4):353–358. doi: 10.1016/j.jpsychores.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 41.Hu K., Gaudron P., Bahner U., Palkovits M., Ertl G. Changes of atrial natriuretic peptide in brain areas of rats with chronic myocardial infarction. Am J Physiol. 1996;270(1 Pt 2):H312–H316. doi: 10.1152/ajpheart.1996.270.1.H312. [DOI] [PubMed] [Google Scholar]
- 42.Ertl G., Hu K., Gaudron P., Palkovits M., Bahner U. Remodeling of the brain post myocardial infarction: focus on central ANF. Basic Res Cardiol. 1997;92(2):82–84. doi: 10.1007/BF00805567. [DOI] [PubMed] [Google Scholar]
- 43.Herrmann-Lingen C., Binder L., Klinge M. High plasma levels of N-terminal pro-atrial natriuretic peptide associated with low anxiety in severe heart failure. Psychosom Med. 2003;65(4):517–522. doi: 10.1097/01.psy.0000073870.93003.c4. [DOI] [PubMed] [Google Scholar]
- 44.Faris R., Purcell H., Henein M.Y., Coats A.J. Clinical depression is common and significantly associated with reduced survival in patients with non-ischaemic heart failure. Eur J Heart Fail. 2002;4(4):541–551. doi: 10.1016/s1388-9842(02)00101-0. [DOI] [PubMed] [Google Scholar]
- 45.Sherwood A., Blumenthal J.A., Hinderliter A.L. Worsening depressive symptoms are associated with adverse clinical outcomes in patients with heart failure. J Am Coll Cardiol. 2011;57(4):418–423. doi: 10.1016/j.jacc.2010.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gary R.A., Dunbar S.B., Higgins M.K., Musselman D.L., Smith A.L. Combined exercise and cognitive behavioral therapy improves outcomes in patients with heart failure. J Psychosom Res. 2010;69(2):119–131. doi: 10.1016/j.jpsychores.2010.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Phillips C.O., Wright S.M., Kern D.E., Singa R.M., Shepperd S., Rubin H.R. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta-analysis. JAMA. 2004;291(11):1358–1367. doi: 10.1001/jama.291.11.1358. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.