Abstract
Background:
Research is critical for developing HIV and tuberculosis (TB) programming for U.S. African-born communities, and depends on successful recruitment of African-born people.
Methods:
From January 2014- June 2016, we recruited African-born people for HIV and TB research in King County, Washington. We compared the characteristics of study participants and the underlying populations of interest, and assessed recruitment strategies.
Results:
Target enrollment for the HIV study was 167 participants; 51 participants (31%) were enrolled. Target enrollment for the TB study was 218 participants; 38 (17%) were successfully recruited. Of 249 prior TB patients we attempted to contact by phone, we reached 72 (33%). Multiple recruitment strategies were employed with variable impact. Study participants differed from the underlying populations in terms of gender, country of origin and language.
Conclusions:
Inequities in research participation and in meaningful opportunities for such participation may exacerbate existing health disparities.
Keywords: African, immigrant, HIV, tuberculosis, recruitment
Introduction
King County, Washington (WA) is home to a well-established technology industry and a large public university, is a major port of entry for new immigrants arriving in the U.S., and has been a center for refugee resettlement for many years. As a result of these and other forces, the county population is very diverse, with foreign-born individuals representing 21% of the county population, compared to 13% of the national population.1,2 In particular, the Seattle metropolitan statistical area is home to one of the largest African immigrant communities in the U.S.3
Notably, the substantial presence of immigrant populations has influenced the epidemiology of infectious diseases in King County, including HIV, tuberculosis (TB), and hepatitis B.4–7 While African immigrants comprised only 1.8% of the total county population in 2016, African-born people accounted for roughly 10% of newly reported HIV cases from 2010–2013.8 Similarly, 18% of reported cases of active tuberculosis in King County from 2012–2015 were among African immigrants (M. Pecha, unpublished data).
Research is critical for developing effective HIV and TB prevention programs for African-born communities, and is dependent on successful recruitment of African-born people. However, previous episodes of significant research misconduct and human subjects abuses have left many communities of diverse ethnic and cultural backgrounds distrustful and/or fearful of research.9 Additionally, immigrants may have other concerns about participating in research, including concerns about confidentiality and the potential for information sharing with immigration officials, particularly for research around sensitive topics such as drug use or HIV. Recruitment for research of stigmatized conditions may also be particularly difficult for small or tightly knit communities given that a breach of confidentiality could have serious deleterious social or economic consequences.
In order to address the disproportionate impact of HIV and TB on the African immigrant population, we undertook two studies to examine access to and uptake of HIV and TB screening, and to identify missed opportunities for screening, among African-born people reported with HIV or active TB in King County. Recruitment was challenging in both of these studies. In this paper, we document our recruitment goals and actual enrollment, as well as steps taken to increase recruitment.
Methods
We conducted two cross-sectional studies to assess the epidemiology of HIV and TB among African-born people living in King County. The objectives of the HIV study included estimating the proportion of African-born people living with HIV (PLWH) residing in four US metropolitan areas who likely acquired HIV in the U.S., and assessing experiences with HIV testing in this population. The TB study sought to document missed opportunities for TB screening, diagnosis and treatment in the African-born population and was limited to King County; while all participants in the TB study had been diagnosed with active TB, we were interested in learning whether these diagnoses were delayed. A secondary goal for both studies was to develop feasible methods for enrolling African-born people in such studies, with the goal of carrying out similar, larger studies in the future. For the HIV study, we recruited participants at four sites (King County, New York City, Chicago, and Philadelphia) with large African immigrant populations, but for the purposes of this analysis, we included data only for King County, where recruitment was in progress for the longest period. Both studies were funded via the same grant. Because describing post-migration acquisition of HIV was the primary aim of the grant supporting the studies, and given limited resources, we limited recruitment for the TB study to King County.
Eligibility criteria for both studies included birth in an African country, age 18 years or older, and diagnosis with HIV (for the HIV study) or active TB (for the TB study) in 2005 or later. Initially, for both studies, eligibility was limited to English speakers. After consent documents were translated, we also began recruiting participants who spoke French, Oromo, Swahili, Amharic, or Tigrinya, or, for the TB study only, Somali. Eventually, after we obtained approval to do so from the University of Washington (UW) Institutional Review Board (IRB), we began recruiting participants regardless of language spoken.
Additional differences in strategies for the two studies were as follows: PLWH were recruited via a variety of mechanisms which evolved over time. We initially began recruiting participants who were contacted regarding HIV partner services by the Public Health – Seattle and King County (PHSKC) HIV/STD Program staff at the time of HIV diagnosis. We eventually expanded recruitment efforts to include recruitment in the UW Madison Clinic (for HIV infection, housed in the local county medical center); the UW Medical Center’s high risk pregnancy clinic, a UW General Internal Medicine Clinic; through two community-based organizations; and through another UW research study and an ongoing PHSKC HIV surveillance project. Recruitment was carried out by PHSKC staff and UW staff involved in this study.
For our study involving people with active TB diagnoses, we obtained a list of all persons who were diagnosed with active TB and had an African country of birth, along with contact information at the time of diagnosis, from the PHSKC TB Control Program. Staff from the TB Program, the Principle Investigator, or a UW research assistant attempted to contact potential participants who were not currently being treated for TB by phone and letter; letters were translated into Amharic, French, Somali, and Tigrinya. Patients who were currently being treated for active TB at the PHSKC TB Clinic were approached by TB Program staff who were trained in recruitment procedures by the Principle Investigator.
For both studies potential participants were offered 3 options for participating: 1) an in-person interview (with interpreter if needed/desired), 2) a phone interview (with interpreter if needed/desired), and 3) an online survey (limited to English speakers only). Data collection instruments for both studies included questions regarding demographics, the immigration process (year of arrival, visa status at arrival, medical exam as part of the immigration process, medical exam to change visa status in the U.S.), access to medical care, history of TB and HIV screening, and assessment of previous known or suspected exposures to HIV and/or TB.
Both data collection instruments included questions regarding medical care use and access, developed by the TB Epidemiologic Studies Consortium (TBESC) for a study of missed TB prevention opportunities among foreign-born residents of the U.S. and Canada; we utilized questions from this instrument regarding TB symptom seeking behavior for the TB study.10 To measure stigma related to these two infections, we incorporated a stigma scale (previously validated for use measuring HIV stigma in an African American population) for the HIV study, and adapted it for TB for the TB study.11,12 The HIV interview incorporated questions that were either taken from or similar to questions used in a study in the UK to determine whether HIV acquisition among African immigrants was pre- or post-migration.13 We used questions on HIV disclosure originally developed and used with women living in rural communities in the southeastern U.S.14 We examined experiences with sexual violence by adapting four questions used in the National Violence Against Women Survey, adapting them for use with both genders.15 We also asked patients for permission to access their medical or PHSKC surveillance records to record limited amounts of clinical data, including date of diagnosis, HIV and/or TB lab results at diagnosis, and for HIV patients, history of AIDS diagnosis, current viral load, and antiretroviral therapy use. We piloted the HIV interview, which contained many of the questions in the TB interview, with a group of 16 African immigrants living with HIV prior to the beginning of the study. In the pilot interview, we asked participants whether they would be more likely to participate in the study if the study interviewer was similar to the participant in age, gender, language or country of birth. The great majority of participants reported that they had no preferences around interviewer characteristics. Patients received a gift card for participating in the study; the incentive was initially $30 and $35 for the TB and HIV studies, respectively, but after unexpectedly low initial enrollment, the incentive was raised to $50.
We actively recruited patients for the TB study from January 15, 2014 through January, 2016. Recruitment for the HIV study began April 1, 2014 and is ongoing; we included recruitment data through June 30, 2016. We present descriptive analyses, including our recruitment goals and numbers of participants enrolled over time. We compared the characteristics of study participants and all African-born individuals reported with either TB or HIV using PHSKC HIV and TB surveillance data from 2010–2013 and 2004–2011, respectively. All study procedures were approved by the UW IRB.
Results
TB Study Enrollment
Our enrollment goal for our assessment of missed opportunities for TB screening and diagnosis was 218 participants. We actively recruited participants from January, 2014– January, 2016, and during this time we enrolled 38 participants. We attempted to contact all 249 potentially eligible individuals who had been diagnosed with active TB since 2005 by telephone. We were unable to contact 167 (67%). Of these, we had incorrect phone numbers for 74 (44%), the remaining 93 (56%) either did not answer our calls or did not return messages. We also sent letters to people whom we were unable to contact, describing the study and signed by the principle investigator and the director of the PHSKC TB Program. The letters asked the recipients to expect a call from study staff, and provided a study phone number for those who were interested in participating immediately. Of 121 letters sent to English speakers, 56 (46%) were returned as undeliverable. We sent an additional 125 letters translated into Tigrinya, Amharic, and Somali, but were unable to track returns of these letters. Of the total 246 letters sent, we received only 2 phone calls in response.
HIV Study Enrollment
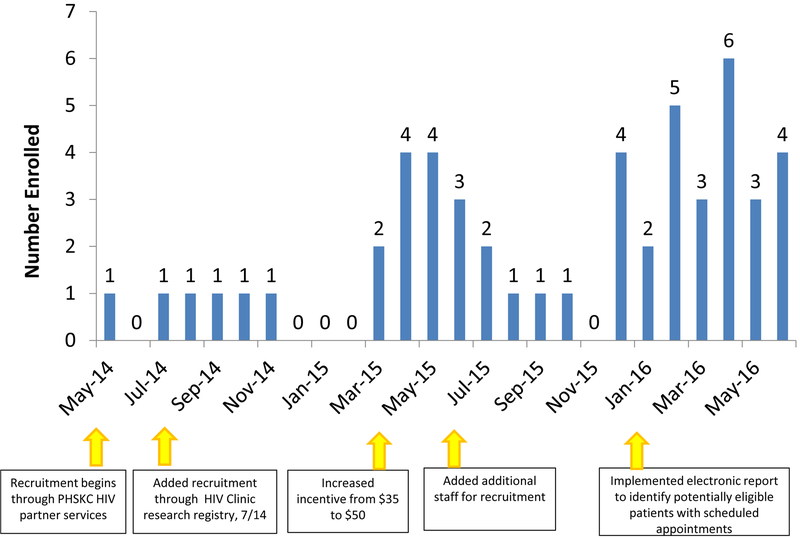
Our recruitment goal for the HIV study was 167; from February, 2014 through June 30, 2016, we enrolled 51 participants. Multiple strategies were employed to improve recruitment over the study period. Figure 1 displays the timing of these strategies along with enrollment over time. Although we initially began recruiting patients only through PHSKC HIV partner services, we subsequently changed strategies to include recruitment through the research registry at the UW Madison Clinic, the largest HIV clinic in King County. Typically, research registry staff explain the importance of clinical research and solicit written consent from new clinic patients with HIV at the time of presentation to the clinic, or soon thereafter. We increased the incentive from $35 to $50, added additional staff recruiting time, and finally, we began recruiting patients directly through providers at the Madison Clinic, rather than through the research registry. We were able to do this through a daily report developed for the study and based on the clinic’s electronic medical record. Of note, after our patient report was implemented (Dec 1, 2015), of 168 potentially eligible patients who presented to the clinic and had not been previously interviewed, only 34 (20%) were enrolled in the clinic’s research registry; in comparison, 80% of the overall clinic population enrolls in this registry.16 Of the 168 potentially eligible participants, 14 were found to be ineligible for our study after we approached the patient or provider. Of the remaining 154, 103 (67%) were approached about participation in the study; of these, 44 (43%) were interviewed, and 27 (26% of the 103 approached) declined. An additional 32 (31%) were uncertain about participating, and asked for future follow up or time to consider.
Figure 1:
HIV Study Enrollment by Month, King County, WA, May, 2014 - June, 2016
Interview Language and Modality
Of the 51 total participants interviewed for the HIV study, 37 (73%) were interviewed in English, 4 (11%) completed an online survey, 25 (68%) completed a face-to-face interview, and 8 (22%) participated via a telephone interview (Table I). Of the 47 people who initially enrolled in the TB study, 19 (40%) agreed to take the online survey but 9 (49%) of these did not complete the survey. Of the remaining 38 participants who completed the TB study, 15 (40%) completed a face to face interview, 13 (34%) completed a phone interview, and 10 (26%) participated via the online survey.
Table I:
| TB Study Participants, N=38 |
HIV Study Participants, N=51 |
||||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Sex | Male | 21 | 55 | 25 | 49 |
| Female | 17 | 45 | 26 | 51 | |
| Age** | 18–29 years | 10 | 27 | 3 | 6 |
| 30–39 years | 17 | 46 | 17 | 35 | |
| 40–49 years | 4 | 11 | 12 | 24 | |
| 50 years and older | 6 | 16 | 17 | 35 | |
| Interview language | English | 30 | 79 | 37 | 73 |
| Amharic | 4 | 11 | 6 | 12 | |
| French | 1 | 3 | 4 | 8 | |
| Other | 3 | 8 | 3 | 6 | |
| Country of birth | East Africa | 34 | 89 | 38 | 75 |
| Other regions of Africa | 4 | 11 | 13 | 25 | |
Recruitment for the TB study occurred January, 2014-February 1, 2016
Three participants were missing age, one in the TB study and two in the HIV study
Participant representativeness
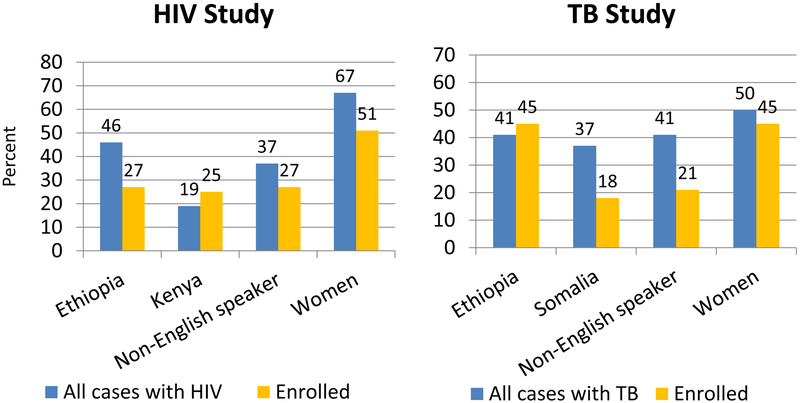
To assess whether our study participants were representative of all local African-born people with HIV or active TB, we compared the characteristics of study participants to all African-born people reported with HIV or active TB in King County using PHSKC surveillance data for 2010–2013 and 2005–2014, respectively. A larger proportion of HIV study participants were Kenyan and a smaller proportion were Ethiopian and/or female, compared to all African-born people reported with HIV from 2010–2013 (Figure 2). A smaller proportion of TB study participants were Somali when compared to all African persons reported with active TB, while there were smaller differences by gender and for people born in Ethiopia than we observed for HIV study participants. Interestingly, people with limited English proficiency (LEP) were more clearly underrepresented among our TB study participants than was the case for HIV study participants, with 41% of all persons reported with TB in King County having LEP, compared to only 21% of TB study participants.
Figure 2:
Study participant characteristics and characteristics of all African-born people reported with active HIV* or TB** in King County, WA
*Public Health – Seattle and King County (PHSKC) HIV surveillance data, 2010–2013 (N= 101)
**PHSKC TB surveillance data, 2005–2014 (N=249)
Discussion
We encountered significant challenges in recruiting African-born study participants. Among persons previously treated for active TB whom we attempted to contact and recruit by phone, we were unable to reach 67%. Over a two year period we were able to enroll only 38 out of 249 potentially eligible people with current or prior active TB. While we were more successful at recruiting participants into our study of PLWH, enrollment was lower than expected. We found that the existing infrastructure in place to recruit patients to participate in HIV research in our local HIV clinic did not function well with this African-born patient population; only 20% of the potentially eligible participants identified through the clinic’s electronic medical record were part of the clinic’s pre-existing research registry, compared to 80% of the clinic’s overall patient population.16 Of the persons living with HIV who we were able to speak with, approximately one-quarter declined to participate in our study, while an additional 30% requested additional time to consider participation. While we attempted to provide additional options to make potential participants feel more comfortable with participating in the studies, including translating consent forms, providing interpreters, and offering the interview as an online survey, meeting our recruitment goals was a challenge, and study participants were not representative of the population of African-born people living with HIV or active TB in our county.
Investigators have documented a variety of challenges of recruiting vulnerable populations such as immigrants and refugees. These include concerns about privacy, language barriers, a lack of belief in the benefit of research to community, research procedures such as informed consent process which are unfamiliar or culturally inappropriate, and study working hours or locations which are inconvenient for participants.9,17–23 There are additional structural level barriers to participation in research that likely also hinder research participation among marginalized populations, including differential access to health care or other services where recruitment might take place, the legacy of research misconduct and human rights abuses associated with studies such as the Tuskegee Syphilis Study, power imbalances between researchers and participants, including beliefs researchers gain more from research than the communities that participate in their studies, and specific to immigrants, fear that uptake of health services or research participation might have negative immigration-related consequences.9,17,19,22,24–31
Some of these barriers have been successfully addressed by engaging community advisory boards, undertaking other forms of community engagement such as health fairs or working with community leaders, ethnic and linguistic “matching” of recruiters to the population of interest, making the consent process transparent and straightforward, providing hours and locations that are convenient, providing translated information and interpreters for those with low English proficiency, and ensuring that research participants are adequately compensated for their time.9,20,21,23,32 Recruitment practices to address some of the more structural-level barriers have been less well documented in the literature. Recruiting participants in the community or via community-based organizations that serve specific populations rather than at facilities has been successful in many instances.29 Community-based participatory research (CBPR) is a research framework that incorporates many of these individual strategies, and has been successfully used to recruit immigrant and refugee populations.31,32 Finally, providing support to junior investigators or otherwise improving the “pipeline” to bring individuals who represent marginalized populations into research fields may also be a way to ensure that researchers understand the needs of the community and to build trust between communities and academic institutions.
While all of the strategies described above have been used effectively to recruit vulnerable populations for research, a further challenge to investigators is that racial/ethnic minority and other marginalized populations are not homogenous, and strategies that are successful for one community may be less so for others.21,33,34 Similarly, the topic of research and the degree to which researchers are seeking information about sensitive or stigmatized conditions or behaviors may also affect the effectiveness of recruitment strategies.19 For example, others studying very sensitive topics found that when offered a choice, participants often did not want to meet with research staff from their country of birth.18,35 Both HIV and TB are highly stigmatized in many African communities,18,36–39 and this led us to adapt recruitment strategies that do not necessarily conform to processes that may otherwise be recognized as best practices when recruiting participants from vulnerable populations.
We undertook recruitment of African immigrant participants after consultation with social workers, and community based organization, research, and public health staff, all of whom work with African immigrants with HIV and or TB, and some of whom are African immigrants themselves. Based on their input, and the shared concern that the stigma around HIV and TB in the African immigrant community would make recruitment difficult, we believed that our recruitment would be most successful at facilities or agencies that serve people who are seeking care or services related to HIV or TB, rather than in the community or through more passive means such as advertising. We did attempt to make participation as convenient as possible, including conducting interviews in the evenings or on weekends as needed, providing an option for phone interviews, and offering to conduct interviews in participant’s homes or other private locations. In retrospect, we believe that the most effective approach would have been to have trusted providers, or clinic or community-based organization staff carry out recruitment and the interviews. We attempted to provide support for a community-based organization staff member to recruit PLWH receiving HIV case management services, which was a successful model for our pilot interviews. Unfortunately, staff turnover resulted in this strategy being unsuccessful beyond the pilot phase.
We hope that others who intend to recruit immigrant and refugee populations will find these results useful in developing recruitment plans. However, there are some limitations to our analyses. First, as a result of relying on other organizations to recruit some participants for our HIV study, we were unable document how many total potential participants were approached and how many refused to participate among all those approached. Second, while we had information about many of the potential participants who declined participation or whom we could not contact (such as language and COB), our IRB did not allow us to use this information to compare those who agreed to participate with those who did not, without first obtaining permission to use those data from each individual. While we attempted to do this for a time, we ultimately abandoned this strategy; most people who declined to participate in our studies chose not to allow us to use their data for any research purpose. Finally, certain instruments used in this study (e.g. measures of sexual violence and HIV status disclosure), while employed by previous studies, have not been validated for use with African immigrants. Future research is needed to better understand the psychometric properties of these instruments with this specific population.
Inequities in research participation may result in some populations not benefitting from the positive impacts of research, particularly if groups are systematically excluded from participation because of barriers such as language or literacy. As such, research that excludes populations most impacted by the health condition may serve to exacerbate existing health disparities. Successful recruitment of immigrant populations may require resources not usually needed for studies with U.S.-born people, including support for translation, interpreters, and increased staff time to provide more intensive outreach, resources which should be taken into consideration both by investigators and funders. Finally, the same barriers to research participation that we and others have observed may also make immigrant populations difficult to reach with prevention programs or public health messages; as such, identifying and implementing methods to reach immigrant communities may be important not only to the success of individual studies, but also in developing ways to most effectively deliver programs or interventions resulting from such studies.
Acknowledgements:
RK was supported by NAID K01 AI095060. This research was further supported by the UW Center for AIDS Research (NIH AI027757), NCATS/NIH for REDCap (UL1 TR002319), and the Firland Foundation (201108). The study authors wish to thank the community partners who provided support for this project.
References
- 1.U.S. Census Bureau. Profile of Selected Social Characteristics: 2000. American Fact Finder, Census 2000 Summary File 2003 (SF 2003) - Sample Data. Available at: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=CF. Accessed July 20, 2017.
- 2.Census Bureau US. United States Quick Facts. 2016; http://www.census.gov/quickfacts/table/PST045215/00. Accessed June 29, 2016.
- 3.Gambino CP TEN, Fitzwater JT The Foreign-Born Population from Africa: 2008–2012. U.S. Census Bureau;2014. [Google Scholar]
- 4.Kent JB. Impact of foreign-born persons on HIV diagnosis rates among Blacks in King County, Washington. AIDS Educ Prev. 2005;17(6 Suppl B):60–67. [DOI] [PubMed] [Google Scholar]
- 5.Kerani R, Bennett AB, Golden M, Castillo J, Buskin SE. Foreign-Born Individuals with HIV in King County, WA: A Glimpse of the Future of HIV? AIDS Behav. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kerani RP, Herbeck JT, Buskin SE, et al. Evidence of Local HIV Transmission in the African Community of King County, Washington. Journal of immigrant and minority health / Center for Minority Public Health. 2017;19(4):891–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Public Health - Seattle & King County. Tuberculosis, Seattle & King County, Washington, 2016 March, 2017. [Google Scholar]
- 8.Kerani RP, Herbeck JT, Buskin SE, et al. Evidence of Local HIV Transmission in the African Community of King County, Washington. Journal of Immigrant and Minority Health. 2016:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blanchet R, Sanou D, Nana CP, Pauze E, Batal M, Giroux I. Strategies and Challenges in Recruiting Black Immigrant Mothers for a Community-Based Study on Child Nutritional Health in Ottawa, Canada. Journal of immigrant and minority health / Center for Minority Public Health. 2017;19(2):367–372. [DOI] [PubMed] [Google Scholar]
- 10.Davidow AL, Katz D, Reves R, Bethel J, Ngong L, Tuberculosis Epidemiologic Studies C. The challenge of multisite epidemiologic studies in diverse populations: design and implementation of a 22-site study of tuberculosis in foreign-born people. Public Health Rep. 2009;124(3):391–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rao D, Choi SW, Victorson D, et al. Measuring stigma across neurological conditions: the development of the stigma scale for chronic illness (SSCI). Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2009;18(5):585–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rao D, Molina Y, Lambert N, Cohn SE. Assessing Stigma among African Americans Living with HIV. Stigma Health. 2016;1(3):146–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burns FM, Arthur G, Johnson AM, Nazroo J, Fenton KA. United Kingdom acquisition of HIV infection in African residents in London: more than previously thought. AIDS. 2009;23(2):262–266. [DOI] [PubMed] [Google Scholar]
- 14.Sowell RL, Lowenstein A, Moneyham L, Demi A, Mizuno Y, Seals BF. Resources, stigma, and patterns of disclosure in rural women with HIV infection. Public Health Nurs. 1997;14(5):302–312. [DOI] [PubMed] [Google Scholar]
- 15.Tjaden PTN. Extent, nature and consequences of intimate partner violence: findings from the National Violence Against Women Survey. Washington, DC: Department of Justice, National Institute of Justice;2000. NCJ 181867. [Google Scholar]
- 16.Oster NV, Jackson SL, Dhanireddy S, et al. Patient Access to Online Visit Notes: Perceptions of Doctors and Patients at an Urban HIV/AIDS Clinic. J Int Assoc Provid AIDS Care. 2015;14(4):306–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loutfy MR V LK, Mohammed S, et al. Recruitment of HIV-Positive Women in Research: Discussing Barriers, Facilitators, and Research Personnel’s Knowledge. Open AIDS J. 2014;8:58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Othieno J Understanding how contextual realities affect African born immigrants and refugees living with HIV in accessing care in the Twin Cities. Journal of health care for the poor and underserved. 2007;18(3 Suppl):170–188. [DOI] [PubMed] [Google Scholar]
- 19.Shedlin MG, Decena CU, Mangadu T, Martinez A. Research participant recruitment in Hispanic communities: lessons learned. Journal of immigrant and minority health / Center for Minority Public Health. 2011;13(2):352–360. [DOI] [PubMed] [Google Scholar]
- 20.Craig SR, Lahey T, Dixit A, Fordham von Reyn C. Altruism, Scepticism, and collective decision-making in foreign-born U.S. residents in a tuberculosis vaccine trial. BMC Public Health. 2018;18(1):535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lu YG MW The Qualitative Report. 2014;19:1–16. [Google Scholar]
- 22.Barata PC, Gucciardi E, Ahmad F, Stewart DE. Cross-cultural perspectives on research participation and informed consent. Soc Sci Med. 2006;62(2):479–490. [DOI] [PubMed] [Google Scholar]
- 23.Salman A, Nguyen C, Lee YH, Cooksey-James T. A Review of Barriers to Minorities’ Participation in Cancer Clinical Trials: Implications for Future Cancer Research. Journal of immigrant and minority health / Center for Minority Public Health. 2016;18(2):447–453. [DOI] [PubMed] [Google Scholar]
- 24.Deren S, Shedlin M, Decena CU, Mino M. Research challenges to the study of HIV/AIDS among migrant and immigrant Hispanic populations in the United States. J Urban Health. 2005;82(2 Suppl 3):iii13–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Asch S, Leake B, Anderson R, Gelberg L. Why do symptomatic patients delay obtaining care for tuberculosis? Am J Respir Crit Care Med. 1998;157(4 Pt 1):1244–1248. [DOI] [PubMed] [Google Scholar]
- 26.Berk ML, Schur CL. The effect of fear on access to care among undocumented Latino immigrants. J Immigr Health. 2001;3(3):151–156. [DOI] [PubMed] [Google Scholar]
- 27.Gilbert PA, Barrington C, Rhodes SD, Eng E. Saliendo Adelante: Stressors and Coping Strategies Among Immigrant Latino Men Who Have Sex With Men in a Nontraditional Settlement State. Am J Mens Health. 2016;10(6):515–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Corbie-Smith G, Thomas SB, Williams MV, Moody-Ayers S. Attitudes and beliefs of African Americans toward participation in medical research. J Gen Intern Med. 1999;14(9):537–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rugkasa J, Canvin K. Researching mental health in minority ethnic communities: reflections on recruitment. Qual Health Res. 2011;21(1):132–143. [DOI] [PubMed] [Google Scholar]
- 30.Mays VM, Coles CN, Cochran SD. Is there a legacy of the U.S. Public Health Syphilis Study at Tuskegee in HIV/AIDS-related beliefs among heterosexual African-Americans and Latinos? Ethics Behav. 2012;22(6):461–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carina K, Meghan F, Lauren R, Katherine HM. Experiences and Lessons Learned in Using Community-Based Participatory Research to Recruit Asian American Immigrant Research Participants. Journal of Nursing Scholarship. 2016;48(2):210–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hanza MM, Goodson M, Osman A, et al. Lessons Learned from Community-Led Recruitment of Immigrants and Refugee Participants for a Randomized, Community-Based Participatory Research Study. Journal of immigrant and minority health / Center for Minority Public Health. 2016;18(5):1241–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McLean CA, Campbell CM. Locating research informants in a multi-ethnic community: ethnic identities, social networks and recruitment methods. Ethn Health. 2003;8(1):41–61. [DOI] [PubMed] [Google Scholar]
- 34.Shaghaghi A, Bhopal RS, Sheikh A. Approaches to Recruiting ‘Hard-To-Reach’ Populations into Re-search: A Review of the Literature. Health Promot Perspect. 2011;1(2):86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kwakwa HA, Wahome R, Goines DS, et al. Engaging African and Caribbean Immigrants in HIV Testing and Care in a Large US City: Lessons Learned from the African Diaspora Health Initiative. Journal of immigrant and minority health / Center for Minority Public Health. 2017;19(4):818–824. [DOI] [PubMed] [Google Scholar]
- 36.Bova C, Nnaji C, Woyah A, Duah A. HIV Stigma, Testing Attitudes and Health Care Access Among African-Born Men Living in the United States. Journal of immigrant and minority health / Center for Minority Public Health. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Koku EF. HIV-related stigma among African immigrants living with HIV/AIDS in the USA. Sociological Research Online. 2010;15(3). [Google Scholar]
- 38.Nnoaham KE, Pool R, Bothamley G, Grant AD. Perceptions and experiences of tuberculosis among African patients attending a tuberculosis clinic in London. Int J Tuberc Lung Dis. 2006;10(9):1013–1017. [PubMed] [Google Scholar]
- 39.Chinouya MJ, Adeyanju O. A disease called stigma: the experience of stigma among African men with TB diagnosis in London. Public Health. 2017;145:45–50. [DOI] [PubMed] [Google Scholar]