Abstract
Anti-angiogenic agents that block Vascular Endothelial Growth Factor (VEGF) signaling are important components of current cancer treatment modalities but are limited by alternative ill-defined angiogenesis mechanisms that allow persistent tumor vascularization in the face of continued VEGF pathway blockade. Here, we identify prostaglandin E2 (PGE2) as a soluble tumor-derived angiogenic factor associated with VEGF-independent angiogenesis. PGE2 production in preclinical breast and colon cancer models was tightly controlled by cyclooxygenase-2 (COX-2) expression, and COX-2 inhibition augmented VEGF pathway blockade to suppress angiogenesis and tumor growth, prevent metastasis, and increase overall survival. These results demonstrate the importance of the COX-2/PGE2 pathway in mediating resistance to VEGF pathway blockade and could aid in the rapid development of more efficacious anti-cancer therapies.
Summary
One Sentence Summary: COX-2 Blockade Potentiates Anti-Angiogenic Therapy
INTRODUCTION
The ability to evoke new blood vessel formation, or angiogenesis, is a critical hallmark of malignant tumors. The newly formed tumor vasculature provides not only a lifeline of nourishment for expansive tumor growth, but also a key escape route for metastatic spread. Vascular endothelial growth factor-A (hereafter VEGF), the most widely recognized stimulator of angiogenesis, promotes tumor neovascularization upon binding to VEGF receptors on the endothelial cells (ECs) that line blood vessels. Over the past decade, VEGF pathway blockers have become a vital component of cancer therapy (1). In 2004, an anti-VEGF neutralizing antibody, bevacizumab, became the first antiangiogenic agent approved for cancer therapy and is currently used in combination with chemotherapy to treat colon, lung, brain and kidney cancer. Seven small-molecule tyrosine kinase inhibitors (TKIs) with anti-angiogenic activity, namely axitinib, cabozantinib, pazopanib, regorafenib, sorafenib, sunitinib, and vandetanib, are also clinically approved for treatment of various malignancies. In addition to targeting VEGFRs, most TKIs also potently inhibit other tyrosine kinases such as PDGFR, KIT, or RAF. However, axitinib is highly selective for the VEGFR family, targeting VEGFR-1, VEGFR-2 and VEGFR-3 at clinically used doses (2).
Although VEGF pathway blockade has shown clinical activity against some cancers, enduring cures are rare, and extension of overall survival is usually measured in weeks or months. In both clinical and preclinical settings, tumor angiogenesis and tumor growth can persist in the face of VEGF/VEGFR2 pathway blockade. Several alternative angiogenesis-promoting factors have been proposed for this refractoriness to VEGF-pathway blockade, including PlGF, FGF, BV8, IL8, PDGF-C, and TEM8/ATRXR1 (3–4) but the therapeutic value of targeting these factors awaits clinical validation.
It is apparent that blockade of the VEGF pathway alone is insufficient to block the outgrowth of microscopic metastatic disease, based on the failure of several recent clinical studies involving VEGF inhibitors in the neoadjuvant (before primary tumor removal) or adjuvant (after primary removal) setting (5). Even more disconcerting is the possibility that in certain cases VEGF pathway inhibitors may fuel the development of more invasive and metastatic disease, thereby counteracting any beneficial anti-tumor responses these agents may have elicited earlier in the course of treatment (6). These concerns, provoked largely by two preclinical studies (7–8), could help explain why in several clinical trials anti-angiogenic therapy extended progression-free survival, but then failed to significantly impact overall survival in subsequent large randomized clinical trials (6). Concordant with this idea, angiogenesis inhibition can promote tumor hypoxia, which in turn can promote the selection of more invasive and metastatically-competent tumor cells (9). Whether or not anti-angiogenic therapy can promote the evolution of more aggressive disease in the clinic is currently unclear, challenging to assess, and a matter of ongoing debate (6, 10). Nevertheless, with glioblastoma, there is clinical evidence to support the idea that VEGF blockade may evoke a more invasive disease (6, 11). Regardless of whether or not anti-VEGF therapy can accelerate tumor metastasis in the clinic, there is a clear need to identify key agents that work effectively with VEGF-pathway blockers to inhibit VEGF-independent angiogenesis and simultaneously prevent the emergence and growth of aggressive metastatic disease. Here, we set out to identify key mediators of VEGF-independent tumor angiogenesis and identified cyclooxygenase-2 [COX-2; prostaglandin-endoperoxide synthase 2 (Ptgs2)] as a potential facilitator of both VEGF-refractory tumor angiogenesis and metastatic disease.
RESULTS
CT26 colon tumors exploit VEGF-independent angiogenesis
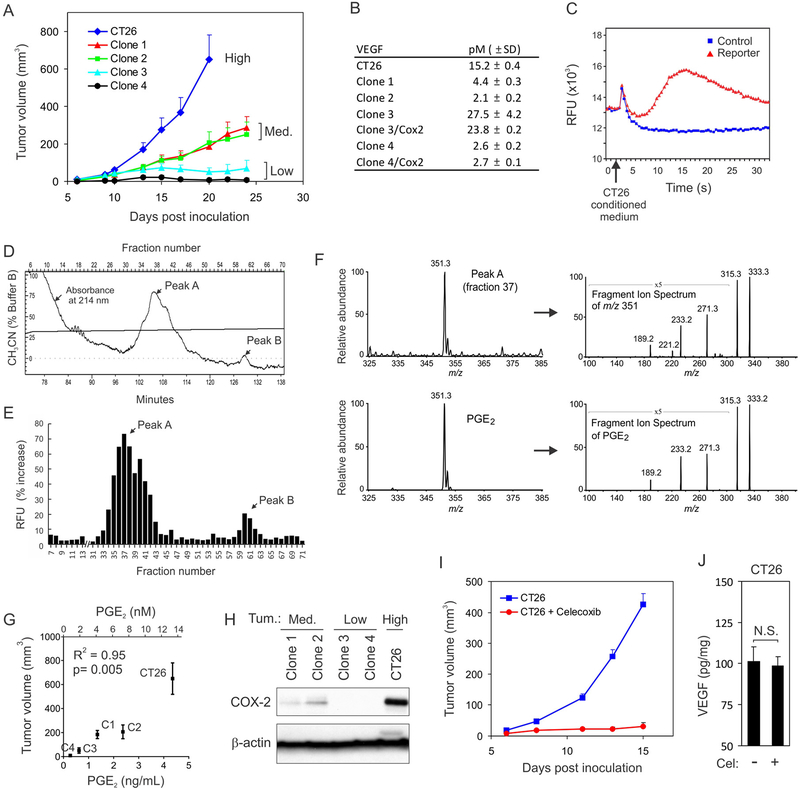
Previous studies revealed a wide variation in the response of tumors to VEGF pathway blockade (12). While examining the sensitivity of various preclinical tumor cell lines to VEGF pathway inhibitors in vivo, we (see below) and others (12) found that the growth of murine CT26 colon tumors in syngeneic immunocompetent mice is resistant to VEGFR2 inhibitors, suggesting that this cell line may be a useful tool for identifying VEGF-independent angiogenesis mechanisms. We therefore cloned the CT26 cell line by limiting dilution and compared the VEGF expression of the clones with their tumorigenic potential in vivo after subcutaneous inoculation. These studies revealed a range of tumorigenicity that was categorized as low (clone 1 and 2), medium (clone 3 and 4), or high (CT26 parent) (Fig. 1A and table S1). However, the tumorigenicity index displayed no direct correlation with VEGF expression in the tumors in vivo or in the conditioned medium of cultured cells (Fig. 1B and fig. S1). For example, clone 3 had the highest concentration of VEGF but was poorly tumorigenic, whereas clone 2 had an extremely low concentration of VEGF and intermediate tumorigenic potential. These studies suggest that tumor-derived VEGF is not the major angiogenesis-stimulating factor in CT26 tumors.
Figure 1. PGE2 is a major tumor-promoting factor produced by CT26 cells.
(A) Subcutaneous tumor growth rates for the CT26 parent cell line and its clonally derived sublines were categorized as high (CT26), medium (Med.; Clone 1, Clone 2) or low (Clone 3, Clone 4).
(B) VEGF concentrations in the conditioned media of CT26-derived cell lines as measured by ELISA.
(c) Conditioned medium from CT26 cells induced a robust calcium flux in reporter cells. The flux could be rapidly measured in a 96-well format using a calcium-sensitive dye. This assay was used to guide biochemical fractionation.
(D) Two separate molecular entities (Peaks A and B) were visualized at 214 nm in the final HPLC column.
(E) The fractions corresponding to Peak A and Peak B in (D) stimulated the highest activity in the calcium mobilization assay.
(F) Electrospray ionization mass spectrometry (ESI-MS) of Fraction 37 from Peak A revealed a molecular ion (m/z 351) and corresponding fragment ion spectrum (top panel) that was identical to pure PGE2 (bottom panel).
(G) Correlation between PGE2 concentration and tumor volume of CT26-derived cell lines 20 days after inoculation.
(H) COX-2 protein in the CT26-derived cell lines as measured by Western blotting.
(I) CT26 tumor growth with or without celecoxib treatment. P < 0.0001.
(J) The amount of VEGF in CT26 tumors with or without celecoxib. N.S.: nonsignificant.
Data in A, I, and J are presented as mean ± SEM.
Tumors can recruit infiltrating immune cells, such as myeloid cells, which are known to promote angiogenesis (13), raising the possibility that CT26 tumor angiogenesis may be initiated indirectly by VEGF-producing inflammatory cells. We therefore generated ~0.5 mm diameter CT26 tumor spheroids in cell culture, implanted the spheroids into the avascular mouse cornea, and assessed the timing of immune cell infiltration and angiogenesis. CT26 tumor cells were able to evoke a rapid angiogenic response that was unaffected by VEGF blockade at the earliest stage of angiogenesis induction. Immunofluorescence staining with the pan-leukocyte marker CD45 revealed that the infiltrating host cells arrived via the newly formed blood vessel loops that originated from the limbal vasculature (fig. S2). These studies raised the possibility that CT26 tumor cells secrete a VEGF-independent factor that stimulates angiogenesis followed by host cell infiltration.
PGE2 production correlates with the tumorigenicity of CT26 cell clones
We set out to biochemically purify the putative VEGF-independent angiogenesis factor from the conditioned medium of CT26 cells with high performance liquid chromatography (HPLC). Although various angiogenesis assays could potentially be used to follow biological activity during fractionation, current angiogenesis assays are impractical for high-throughput screening and/or only recapitulate certain aspects of the complex angiogenesis process in vivo. While searching for an alternative in vitro assay we discovered that conditioned medium from the CT26 parent line or its tumorigenic clones (clone 1 and 2), but not the low-tumorigenic clones (clone 3 and 4), selectively stimulated a robust calcium flux in reporter cells stably transfected with Gα16 (Fig. 1C). This particular assay was tested because many extracellular ligands signal through G-protein coupled receptors (GPCRs), and forced expression of the so-called “promiscuous” Gα16 protein can couple GPCR stimulation with the PLC/DAG signaling pathway that culminates in calcium release from cytosolic stores (14). During our initial characterization of the soluble CT26-derived factor, we determined it was stable at high temperatures (95°C) and could be extracted with butanol, suggesting that the tumor-derived factor may be a lipid.
We biochemically purified the factor to homogeneity from 10 liters of CT26 conditioned medium using a protocol involving filtration and multiple cycles of solid phase extraction and reverse phase HPLC (for details see Supplementary Methods). After the final HPLC column, we detected two separate chromatographic peaks correlated with reporter activity, one major (peak A) and one minor (peak B), subsequently identified by electrospray ionization mass spectrometry as prostaglandins E2 (PGE2) and PGA2, respectively (Fig. 1, D to F and fig. S3A). Chemically synthesized PGE2 and PGA2 both induced Ca2+ mobilization in the reporter cells, confirming the identity of the purified factors (fig. S3, B and C). PGE2 can undergo spontaneous dehydration to form PGA2, which was presumably responsible for the minor “PGA2” peak on the HPLC columns. Next, we measured PGE2 concentration in the conditioned medium of the parent CT26 cell line and its subclones, and found that it correlated with the tumorigenic properties of the cells (R2 = 0.95, Fig. 1G and table S1). Thus, PGE2 is the physiologic Ca2+-mobilizing factor selectively produced by CT26 pro-tumorigenic clones, and its production correlates with tumorigenic proficiency.
The COX-2/PGE2 pathway mediates refractoriness to VEGF/VEGFR2 inhibition
PGE2 is derived from arachidonic acid though a series of enzymatic reactions, of which COX-2 is usually rate-limiting. Western blot analysis revealed that high levels of COX-2 expression were associated with high concentrations of PGE2 and high tumorigenicity (Fig. 1G and 1H). Treatment of fast-growing CT26 tumors with celecoxib, a selective inhibitor of COX-2, reduced tumor growth to a rate similar to that of PGE2 low-producing clones (Fig. 1I and table S1). However, VEGF protein expression in CT26 tumors in vivo was unaltered in response to celecoxib treatment, suggesting that COX-2 activity does not regulate VEGF in this model (Fig. 1J and table S1).
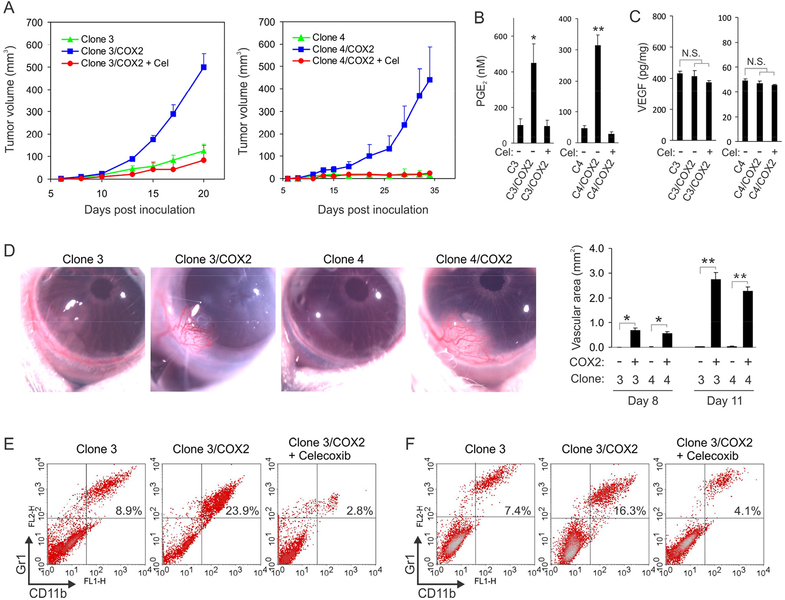
To directly test the importance of COX-2 for tumor growth, we stably transfected exogenous COX-2 into CT26 clones that expressed low amounts of endogenous COX-2 (Clone 3 and 4), so their COX-2 and PGE2 production were similar to the CT26 parent cell line (fig. S4, fig. S5A, and table S1). Forced COX-2 expression in the poorly tumorigenic CT26 clones made them highly tumorigenic in vivo, and their pro-tumorigenic phenotype could be completely reversed by treatment with celecoxib (Fig. 2A and table S1). PGE2 concentration was also increased in the blood of mice bearing Clone 3/COX-2 or Clone 4/COX-2 tumors compared to control tumors (Clone 3 or Clone 4), and the elevated PGE2 concentration was reversed after treatment with Celecoxib (Fig. 2B and table S1). VEGF concentrations in both clones were unaltered by COX-2, both in vitro (Fig. 1B) and in tumors in vivo (Fig. 2C and table S1).
Figure 2. Forced COX-2 expression promotes angiogenesis and tumorigenesis.
(A) CT26 Clone 3 and Clone 4 tumor growth rates were compared with their corresponding COX-2 stable transfectants (Clone 3/COX-2 and Clone 4/COX-2). The tumorigenic proficiencies of the COX-2-transfected cell lines were reversed by treatment with Celecoxib (Cel).
(B) Serum PGE2 concentrations in vivo were measured in mice bearing subcutaneous tumors from CT26 Clone 3 (C3) and Clone 4 (C4) and corresponding COX-2 transfected cell lines. The impact of Celecoxib (Cel) treatment was also assessed. *p=0.007, **p<0.0001 vs. parent group, ANOVA.
(C) The amount of tumor VEGF in vivo as determined by ELISA. N.S.: Non-significant.)
(D) Tumor spheroids were implanted into the cornea to evaluate the role of COX-2 in tumor angiogenesis. Right panel: Quantification of corneal angiogenesis at day 8 and 11. *p=0.008, **p=0.002 versus parent group, Mann-Whitney.
(E) Flow cytometry was used to quantify the percentage of Gr1+CDllb+ myeloid cells in the spleens of CT26 Clone 3 tumor-bearing mice (n=4).
(F) Flow cytometry was used to quantify the percentage of Gr1+CDllb+ myeloid cells in subcutaneous CT26 Clone 3 tumors (n=4).
Data are presented as mean ± SEM.
COX-2 converts arachidonic acid to PGH2, which can be enzymatically converted to five major prostanoids: PGE2, PGD2, PGI2 (prostacyclin), PGF2α, and thromboxane A2 (TXA2). To evaluate the potential contribution of prostanoids other than PGE2, first we used RT-PCR to analyze the expression of prostanoid synthases in CT26 cells. Although each of the three PGE2 synthases (Ptges, Ptges2, and Ptges3) was constitutively expressed in the CT26 clones, PGD2 synthase (Ptgds), PGI2 synthase (Ptgis), PGF synthase (Fam213b) and TXA2 synthase (Tbxas1) were undetectable after 30 cycles of PCR (fig. S5B). An analysis of prostanoid concentrations in the conditioned medium of CT26 clones or the corresponding tumors in vivo (figs. S5A, S6 and table S1) revealed that PGE2 was the only prostanoid that increased in response to COX-2 overexpression and decreased after celecoxib treatment, whereas other prostanoids were expressed in low or undetectable amounts. Together, these results indicate that all three PGE2 synthases are expressed in the CT26 cell clones and COX-2 is rate-limiting for PGE2 production.
COX-2 and PGE2 have previously been shown to induce angiogenesis in a number of systems, but most studies point towards an indirect role through stimulation of other pro-angiogenic growth factors from tumor-infiltrating host cells (15). In addition to indirect effects, we hypothesized that the COX-2/PGE2 pathway may play a more immediate role in stimulating angiogenesis through a VEGF-independent paracrine mechanism that acts directly on endothelial cells. To assess this possibility, we evaluated angiogenesis in the immune privileged cornea. Stable COX-2 expression in poorly tumorigenic CT26 clones converted them from an angiogenic-deficient to an angiogenicproficient phenotype (Fig. 2D and table S1). Chemically synthesized PGE2 or conditioned medium from COX-2 overexpressing cells could also stimulate a robust angiogenic response in the Matrigel plug or the ex vivo mouse aortic ring assays, but antiVEGFR2 antibodies were unable to block angiogenesis induced by COX-2 overexpressing cells (figs. S7, S8 and table S1). Although we cannot rule out the possibility that PGE2 induced the production of other angiogenic growth factors, nevertheless, these results demonstrate the importance of the COX-2/PGE2 pathway in meditating VEGF-independent angiogenesis.
The COX-2/PGE2 pathway has been shown to be important for stimulating the production of myeloid derived suppressor cells (MDSCs) (16). Myeloid cells, upon reaching the tumor via newly formed vasculature, can promote tumor growth by suppressing immune functions and promoting further tumor angiogenesis (13). To determine if myeloid cells could also be involved in the later stages of COX-2 induced tumor growth in the CT26 model, we used flow cytometry to measure the number of Gr1+ CD11b+ myeloid cells in Clone 3 or Clone 3/COX-2 tumor-bearing mice. These studies revealed a COX-2 dependent increase in myeloid cells both in the spleen and in the tumor, which was reversed by celecoxib treatment (Fig. 2, E and F). Thus, the PGE2/COX-2 pathway likely promotes tumor growth through multiple mechanisms, beginning with the induction of new blood vessel growth followed by the recruitment of pro-angiogenic Gr1+ CD11b+ myeloid cells.
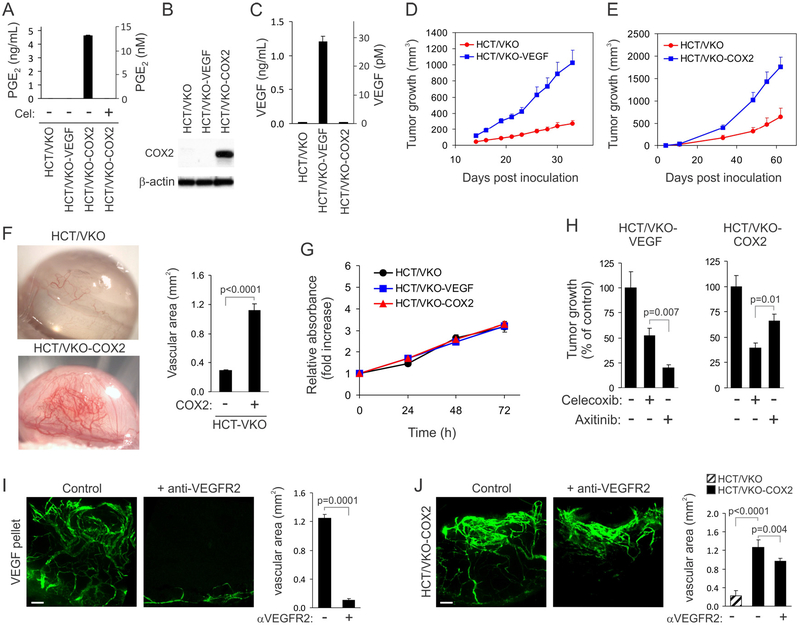
The COX-2 and VEGF pathways independently modulate angiogenesis and human tumor xenograft growth
To further explore the relationship between the VEGF pathway, COX-2/PGE2 pathway, and angiogenesis, we utilized a human colon cancer VEGF knockout (KO) cell line, HCT/VKO, wherein both alleles of the VEGF gene were disrupted by homologous recombination (17). The HCT/VKO cell line produces no detectable VEGF, COX-2 or PGE2 (Fig. 3, A to C and table S1) and forms slow-growing poorly angiogenic tumor xenografts in immunodeficient mice compared to its HCT116 parental VEGF wildtype counterpart (17–18). These results indicate that human tumor-derived VEGF is a major factor driving angiogenesis and tumor growth in HCT116 xenografts. As expected, reintroduction of VEGF into the HCT/VKO cell line by stable transfection (HCT/VKOVEGF) rescued VEGF expression and the in vivo tumor growth properties of the VEGFnull cell line (Fig. 3, C and D and table S1). Stable transfection of HCT/VKO cells with COX-2 (HCT/VKO-COX2) also made the cell line highly tumorigenic in vivo and highly angiogenic in the corneal assay (Figs. 3E, 3F and table S1). Although COX-2 and PGE2 were highly expressed only in HCT/VKO-COX2 cells (Fig. 3, A and B), where PGE2 concentration was similar to endogenous PGE2 concentration in in the conditioned medium of CT26 (compare Fig. 3A with 1G), COX-2 overexpression had no effect on VEGF concentration in vitro (Fig. 3C) or in vivo (fig. S9 and table S1). Similar to the CT26 model, PGE2 was the only prostanoid selectively elevated in response to COX-2 overexpression (fig. S10 and table S1). The growth rate of this tumor cell line in vitro was unaltered by overexpression of either COX-2 or VEGF (Fig. 3G and table S1), suggesting that the enhanced tumor growth in vivo may be mediated through proangiogenic effects on host vascular cells.
Figure 3. Expression of VEGF or COX-2 in HCT/VKO cells promotes tumorigenesis.
(A) PGE2 concentration in the conditioned media of HCT/VKO-derived cell lines as measured by ELISA. PGE2 was below the detection limit in the HCT/VKO, HCT/VKOVEGF, and celecoxib-treated HCT/VKO-COX2 cell lines.
(B) COX-2 protein in HCT/VKO-derived cell lines as measured by Immunoblotting. β-actin was used as a loading control.
(C) VEGF concentration in the conditioned media of HCT/VKO-derived cell lines as measured by ELISA. VEGF was not detected in the HCT/VKO and HCT/VKO-COX2 cell lines.
(D) Tumor growth rates of HCT/VKO and HCT/VKO-VEGF subcutaneous xenografts.(E) Tumor growth rates of HCT/VKO and HCT/VKO-COX2 subcutaneous xenografts.
(F) Tumor spheroids were implanted into the cornea to evaluate the role of COX-2 in tumor angiogenesis. Right panel: Quantification of corneal angiogenesis. P < 0.0001.
(G) An Alamar blue assay was used to measure the relative growth of HCT/VKO-derived cell lines in vitro.
(H) The response of HCT/VKO-VEGF (left panel) or HCT/VKO-COX2 (right panel) subcutaneous xenografts to celecoxib and axitinib was evaluated in vivo.
(I) The corneal assay was used to measure the effect of systemic DC101 anti-VEGFR2 antibody treatment on VEGF-induced vascular sprouting in vivo. Bar: 100 μm.
(J) The corneal assay was used to measure the effect of systemic DC101 anti-VEGFR2 antibody treatment on angiogenesis induced by HCT/VKO-COX2 spheroids. Bar: 100 μm.
Data are presented as mean ± SD (A, C, and G) or mean ± SEM (D, E, F, H-J).
Previous studies have shown that COX-2 controls VEGF-induced angiogenesis and VEGF controls COX-2-induced angiogenesis, highlighting reciprocal cross-talk between the COX-2 and VEGF pathways (19–20). However, it is less clear if either of these two pathways can also operate independently to promote tumorigenesis when the other pathway is blocked. To assess this, we used our HCT/VKO-VEGF and HCT/VKO-COX2 xenograft models to evaluate the impact of celecoxib and axitinib on tumor growth. Axitinib was most potent against HCT/VKO-VEGF tumors, causing an 80% reduction in tumor growth, whereas celecoxib only caused a 48% reduction in tumor growth. Celecoxib, on the other hand, was most potent against HCT/VKO-COX2 tumors, causing a 60% reduction in tumor growth compared to only 34% for axitinib (Fig. 3H and table S1).
Next, we evaluated the impact of VEGF pathway blockade on corneal angiogenesis induced by HCT/VKO-COX2 spheroids. In this assay, FITC-dextran was injected intravenously to assess the functional vasculature in the eye. Although DC101 anti-VEGFR2 antibodies completely blocked corneal angiogenesis induced by VEGF, DC101 only reduced angiogenesis induced by HCT/VKO-COX2 spheroids by 20% (Figs. 3I, 3J and table S1). These data suggest that the COX-2/PGE2 pathway promotes VEGF-independent angiogenesis through direct effects on the vasculature. The 20% reduction caused by DC101 may be the result of angiogenesis induced by VEGF-positive host stromal cells that infiltrate the tumor spheroid in the later stages of the angiogenesis assay.
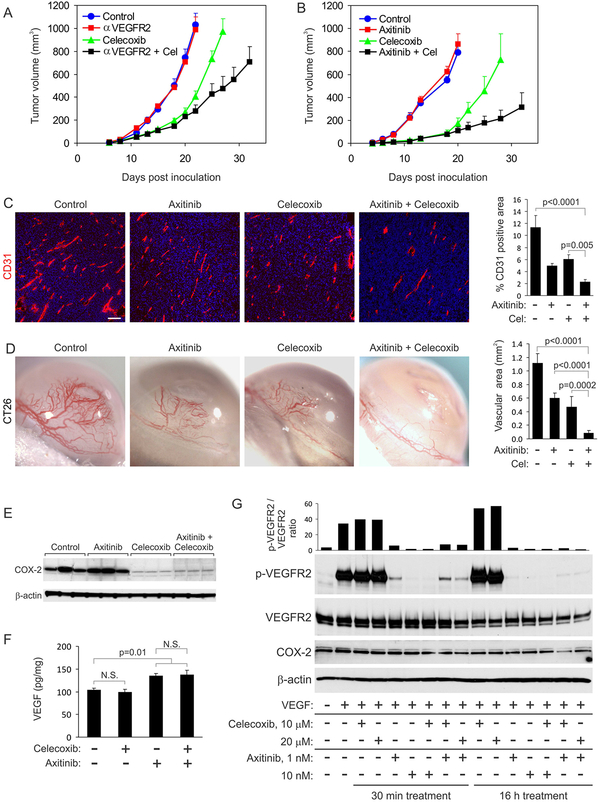
Dual VEGF/COX-2 pathway blockade improves anti-angiogenic activity
The ability of the COX-2/PGE2 pathway to evoke VEGF-independent angiogenesis suggests this pathway may contribute to evasive angiogenesis when the VEGF pathway is blocked. To address this possibility, we challenged mice with CT26 tumors and then treated them with DC101 anti-VEGFR2 antibodies alone, celecoxib alone, or both agents combined. Although CT26 was resistant to DC101 antibody therapy, as previously reported (12), DC101 slowed tumor growth when combined with celecoxib, indicating that the VEGF pathway can contribute to evasive tumor growth in this model when the predominant COX-2/PGE2 pathway is blocked (Fig. 4A and table S1). Similarly, axitinib had no detectable activity on its own in this model, but augmented the anti-tumor activity of celecoxib (Fig. 4B and table S1). To assess the impact of these agents on angiogenesis, we evaluated blood vessel densities and found that celecoxib, anti-VEGFR2 antibody, and axitinib each decreased the vascular density to ~50% of normal. Moreover, the combination of celecoxib with either of the VEGFR2 blockers reduced blood vessel density even further, to ~20% of controls (Fig. 4C, fig. S11A and table S1). Evaluation of angiogenic responses in the corneal assay again revealed increased inhibition with the combination compared to the monotherapies (Fig. 4D, fig. S11B and table S1).
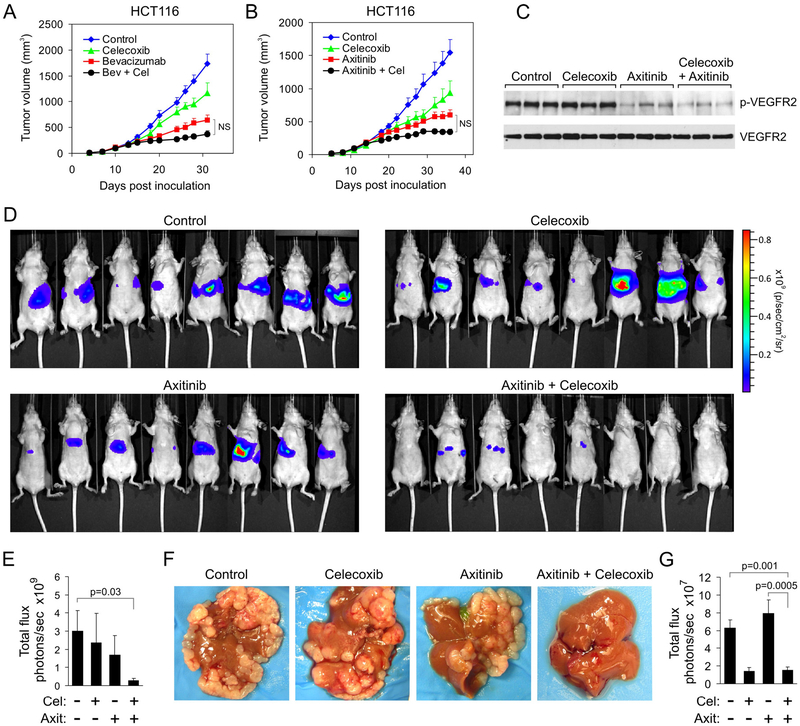
Figure 4. Celecoxib and axitinib modulate independent downstream signaling pathways.
(A) CT26 tumor growth rates in response to celecoxib (Cel) and DC101 (αVEGFR2). Celecoxib therapy was initiated one day after tumor cell inoculation, and DC101 therapy was initiated when tumors reached a size of ~50 mm3.(B) CT26 tumor growth rates in response to celecoxib (Cel) and axitinib. Treatments were initiated as outlined in (A).
(C) Immunofluorescence staining for CD31 (red) was used to assess blood vessel densities in CT26 tumors after treatment with axitinib and celecoxib. Bar: 100 μm. Right panel: quantification of CD31 vessel staining.
(D) The corneal assay was used to measure the effect of systemic axitinib and celecoxib treatment on angiogenesis induced by CT26 tumor spheroids. Right panel: quantification of the corneal angiogenesis.
(E) Western blotting was used to evaluate COX-2 expression in CT26 tumors in vivo in response to axitinib and/or celecoxib (n=3 tumors per group). β-actin was used as a loading control.
(E) An ELISA was used to measure the amount of VEGF in CT26 tumors after treatment with celecoxib and axitinib.
(F) Western blotting was used to assess the impact of celecoxib and axitinib treatment on VEGFR2 phosphorylation and COX-2 expression in HMECs. The top bar graph displays the ratio of phosphorylated VEGFR2 to total VEGFR2.
Data are presented as mean ± SEM.
Next we set out to measure changes in COX-2 and VEGF pathway activity in response to the mono- or combined therapies. Pharmacologic inhibition of COX-2 enzymatic activity has previously been shown to result in decreased COX-2 protein expression in certain tumor types, suggesting a positive feedback loop and providing a convenient way to measure COX-2 inhibition (21). Western blot analysis revealed that celecoxib reduced COX-2 in CT26 tumors, whereas axitinib had no impact on COX-2 (Fig. 4E). Although the amount of VEGF in CT26 tumors increased 30% in response to axitinib, tumor VEGF expression was unaffected by celecoxib treatment (Fig. 4F and table S1). Stimulation of cultured human microvascular endothelial cells (HMECs) with VEGF resulted in a striking phosphorylation of VEGFR2 that was blocked by treatment with axitinib. However, treatment with celecoxib had no impact on VEGFR2 expression or phosphorylation (Fig. 4G). Taken together, these studies highlight the ability of each of these agents to work independently to target the vasculature of tumors.
Next, we tested celecoxib and bevacizumab, an anti-human VEGF neutralizing antibody, against HCT116 human colon cancer xenografts grown subcutaneously in athymic nude mice. Although bevacizumab neutralizes human VEGF and displays minimal cross-reactivity with mouse VEGF, HCT116 tumors xenografts rely mostly on human VEGF produced by the tumor cells (17). Both bevacizumab and celecoxib displayed anti-tumor activity on their own, but the two in combination did not show a significant increase in efficacy (Fig. 5A and table S1). Celecoxib combined with axitinib also did not show a significant additive effect on tumor volume, but blood vessel densities were significantly decreased compared to the monotherapies (p< 0.0001, Fig. 5B, fig. S12, A and B and table S1). An analysis of the VEGFR2 phosphorylation status in tumor tissues revealed that axitinib was able to effectively block VEGFR2 phosphorylation in vivo (Fig. 5C), whereas celecoxib had no effect on VEGFR2 phosphorylation.
Figure 5. Dual COX-2/VEGF pathway blockade suppresses colon cancer liver metastasis.
(A) HCT116 tumor growth rates in response to bevacizumab (Bev) and celecoxib (Cel). All treatments were initiated when tumors reached a size of ~100 mm3. N.S: Nonsignificant. P values for the other comparisons are provided in table S1.
(B) HCT116 tumor growth rates in response to axitinib and celecoxib (Cel). All treatments were initiated when tumors reached a size of ~100 mm3. N.S: Non-significant. P values for the other comparisons are provided in table S1.
(C) VEGFR2 immunoprecipitation followed by western blotting was used to assess the amount of phosphorylated VEGFR2 (p-VEGFR2) in tumors in vivo after treatment with celecoxib or axitinib.
(D) Bioluminescent imaging of tumor burden 14 days after intrasplenic injection of HCT116-luc cells, applying a maximum luminescence threshold of 1×1010.
(E) Quantification of tumor burden shown in (D). Celecoxib (Cel); Axitinib (Axit).
(F) Physical appearance of HCT116 tumor burden in the liver.
(G) Whole body bioluminescent quantification 14 days after intrasplenic injection of CT26-luc cells. The whole body data are comparable to bioluminescent quantification of ex vivo livers (see fig. S12C). Cel: Celecoxib; Axit: Axitinib.
Data are presented as mean ± SEM.
The COX-2 and VEGF pathways cooperate to regulate metastasis
Most cancer-related mortality is a consequence of metastatic spread. To determine if dual VEGF/COX-2 pathway blockade could inhibit metastasis, we used bioluminescence imaging to quantify tumor burden in the liver after intrasplenic injection of luciferasetagged human HCT116 or murine CT26 colon cancer cells. In the HCT116 model, celecoxib treatment alone had a minimal effect on liver metastasis and so did axitinib. However, the combination of the two agents caused a striking decrease in metastasis (Fig. 5, D to F and table S1). In the CT26 syngeneic immunocompetent model, celecoxib displayed potent anti-metastatic activity on its own, whereas axitinib did not have any detectable anti-metastatic activity either alone or in combination with celecoxib (Fig. 5G, fig. S12C and table S1). However, in this model the activity of axitinib in the combination group may have been masked by the strong anti-tumor activity of celecoxib.
To determine if dual VEGF/COX-2 blockade could impact tumor progression in other tumor types, we injected luciferase-tagged murine 4T1-luc breast cancer cells orthotopically into the mammary fat pad of immunocompetent syngeneic mice and monitored tumorigenesis and metastasis. Both primary tumor growth and blood vessel densities were decreased after treatment with either celecoxib or axitinib, but there was no significant increase inefficacy when the agents were combined (Fig. 6, A and B and table S1). The amount of PGE2 in the conditioned media of cultured 4T1-luc cells was reduced in response to celecoxib but not axitinib (fig. S13 and table S1).
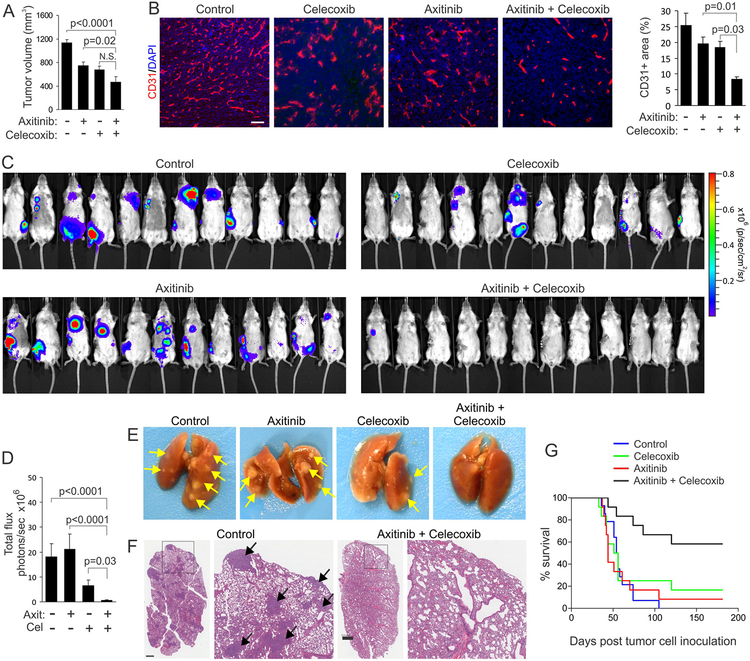
Figure 6. Dual celecoxib/axitinib therapy blocks spontaneous metastasis and extends survival.
(A) The orthotopic growth of 4T1-luc breast tumors in the mammary fat pad was evaluated after treatment with axitinib and celecoxib.
(B) CD31 immunofluorescent staining (red) was used to assess blood vessel densities in 4T1-luc primary tumors after treatment with axitinib and celecoxib. Bar: 100 μm. Right panel: quantification of CD31 vessel staining.
(C) Bioluminescent imaging of metastasis 35 days after injection of 4T1-luc cells into the mammary fat pad. Primary tumors were resected when they reached a size of ~1000 mm3.
(D) Quantification of tumor burden shown in (C) applying a maximum luminescence threshold of 3×107. N.S.: non-significant (n=12/group).
(E) Macroscopic appearance of 4T1-luc tumor burden in the lung. Arrows: tumor nodules.
(F) Microscopic appearance of 4T1-luc tumor burden in the lung after H&E staining. Arrows: tumor nodules. Bar =1 mm.
(G) Kaplan-Meier survival curves were used to asses the impact of celecoxib and axitinib treatment on overall survival of the mice imaged in (C) and (D). Treatments began one day after tumor cell inoculation and continued for the duration of the study. Log-rank analysis: p=0.0001 combination vs. control, p=0.02 combination vs. celecoxib, p=0.001 combination vs. axitinib. All other comparisons were non-significant.
Data are presented as mean ± SEM.
Next, we used bioluminescence imaging to measure the ability of these agents to inhibit spontaneous metastasis of 4T1-luc from the mammary fat. Treatments were initiated 1 day after tumor cell inoculation. Because the 4T1-luc primary tumors grew slower in the treated versus untreated groups (Fig. 6A) and larger tumors could potentially promote more metastasis due to their increased size and/or altered microenvironment, primary tumors were surgically removed once they reached a size of approximately 1000 mm3. Axitinib alone had no significant effect on 4T1-luc metastasis and neither did celecoxib. However, the combination of these two agents significantly reduced metastasis (p<0.0001; Fig. 6, C and D and table S1). Histopathological analysis confirmed that the luminescence signals originated from the metastatic tumor burden (fig. S14). The lung was the most common site of metastasis (Fig. 6, E and F), but metastases were also found in the lymph nodes, kidney, bone, and occasionally the brain, mimicking the major sites of metastasis observed in human breast cancer. To evaluate the impact of this therapy on long-term survival, treatments were continued for an additional 6 months. These studies revealed a significant improvement in survival only in the axitinib/celecoxib combination group, where 60% of mice were alive at 6 months (p=0.0001 vs. control). Only 8% (axitinib) or 17% (celecoxib) survival was found in the monotherapy arms, and no survivors in the control arm (Fig. 6G).
Many cancer patients already have microscopic metastatic disease at the time their primary tumor is removed. To model this difficult-to-treat population and determine if the combination therapy could block the outgrowth of pre-established (initially undetectable) tumor metastasis, we injected 4T1 tumors orthotopically into the mammary fat pad, surgically removed the primary tumors 3 weeks later, randomized the mice into treatment groups, and then began therapy. Four weeks after the initiation of therapy, we could detect widespread metastasis in the untreated control, the celecoxib and the axitinib groups (Fig. 7, A and B and table S1). However, metastases were undetectable in 10 out of 11 mice on the combination therapy. To assess potential toxicity of the treatments, we monitored body weights and food consumption, but found no significant alterations in the monotherapy or combination groups (Fig. 7C, fig. S15 and table S1). By 100 days, overall survival was significantly improved only in the combination group (p=0.007 vs. control; Fig. 7D). At that time, the survivors failed to show any bioluminescence signals above background (fig. S16). 83% of the mice were still alive in the combination group, 58% in the celecoxib group, and 28% and 25% in the control and axitinib groups respectively. Thus, simultaneous COX-2/VEGF pathway blockade prolonged overall survival, despite the presence of pre-established metastatic disease prior to the onset of therapy.
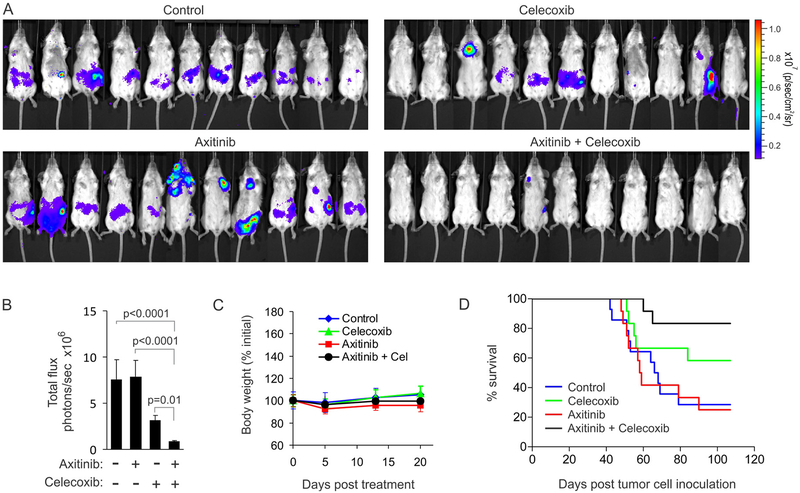
Figure 7. Dual adjuvant therapy blocks pre-established breast cancer metastasis.
(A) Bioluminescent imaging of 4T1-luc metastasis in vivo 50 days after mammary fat pad injection and 27 days after primary tumor resection. Treatments were initiated at the time of tumor resection.
(B) Quantification of tumor burden shown in (A) applying a maximum luminescence threshold of 5×107. Data represent mean ± SEM.
(C) Body weights were monitored for 20 days after tumor resection. Data represent mean ± SD.
(D) Kaplan-Meier survival curves were used to asses the impact of celecoxib and axitinib treatment on overall survival of the mice in (A-C). Log-rank analysis: p=0.007 combination vs. control, p=0.003 combination vs. axitinib, celecoxib vs. control was nonsignificant.
DISCUSSION
Non-selective anti-inflammatory drugs (NSAIDs) that inhibit both COX-1 and COX-2, such as aspirin, have been widely used to prevent fever, pain and inflammation since the late 1800’s (22). Although COX-1 is a constitutively expressed housekeeping enzyme in most tissues, COX-2 levels are normally low but induced during inflammation and cancer. COX-2 expression is elevated in up to 90% of colorectal carcinomas, 70% of lung cancers, and 37% of breast cancers and is correlated with poor prognosis (23–25). For cancer therapy, NSAIDs and selective COX-2 inhibitors (COXIBs) have been tested mostly as preventative agents, and large epidemiologic studies have revealed that regular use of NSAIDs reduces the risk of developing colon, breast, lung and prostate cancer (26). Our study predicts that NSAIDs and COXIBs may also enhance the activity of conventional anti-angiogenic agents against pre-established metastasis, and could potentially improve overall survival of patients with COX-2 positive tumors.
Multiple mechanisms have been proposed to explain the tumor-promoting activity of the COX-2/PGE2 pathway in cancer, including promotion of tumor cell proliferation, recruitment of myeloid-derived suppressor cells and inducing angiogenesis (15). In our study, tumor-derived PGE2 appeared to promote tumor growth through multiple independent mechanisms. First, PGE2 was able to stimulate angiogenesis. Second, COX-2 expression in tumor cells resulted in an elevated number of Gr1+ CD11b+ myeloid cells in tumors, which likely fueled tumor growth once the blood vessel network had been established. Some reciprocal cross-talk between the COX-2/PGE2 and VEGF pathways was also observed in our study, as reported by others (19–20). However, VEGF expression and VEGFR2 phosphorylation were unaltered in celecoxib-treated tumors, suggesting that the mechanisms responsible for crosstalk are likely complex and require further study.
More than 300 ongoing or planned clinical trials of anti-angiogenic agents in the adjuvant or neoadjuvant setting (6) (see also www.clinicaltrials.gov) have been initiated based on the successes of anti-angiogenic agents in the treatment of patients with advanced metastatic disease. However, results from the initial adjuvant trials involving VEGF pathway inhibitors have so far been uniformly disappointing (5, 27–29). In hindsight, these discouraging results are not unexpected, at least based on empirical data from preclinical studies. Historically, few preclinical studies have evaluated the impact of anti-angiogenic agents as adjuvant therapy to prevent the outgrowth of microscopic (minimal residual) metastatic disease after removal of the primary tumor (30–31). One study that evaluated the activity of a VEGFR inhibitor (sunitinib) found anti-tumor activity only against the primary tumor, but the same agent caused accelerated metastasis in the adjuvant setting (7). Another study showed that two VEGFR inhibitors could slow the growth rate of primary tumors, but neither agent was able to prevent lymphatic metastasis when given after tumor cells had seeded the lymph node (32). Similarly, in each of our preclinical colon (CT26 and HCT116) and breast (4T1) cancer models, VEGF pathway blockade alone had no discernable impact on metastasis in the adjuvant setting. Celecoxib, on the other hand, did show some anti-metastatic activity as a monotherapy, but the extent of this activity was tumor model dependent: CT26 showed a strong response, 4T1 an intermediate response, and HCT116 no response. However, in every case, the combination of celecoxib and a VEGF pathway inhibitor was much more effective at blocking metastasis. For example, in the case of HCT116, neither celecoxib nor axitinib showed any tumoricidal activity against liver metastases as a monotherapy, but the combination showed potent anti-metastatic activity. 4T1 also responded much better to axitinib/celecoxib combined therapy than to celecoxib alone, and this translated into an enhanced overall survival only in the combination group.
A major limitation of current anti-angiogenic therapy is the lack of suitable biomarkers that would allow clinicians to predict which patients are likely to respond to VEGF pathway blockers (33). Our data suggest that when COX-2 expression is high, blockade of the VEGF pathway may have only modest anti-tumor activity. Thus, COX-2 expression analysis may aid in determining which patients are most likely to respond to VEGF pathway inhibitors. Screening for mutations in PIK3CA or other genes that lead to elevated COX-2 activity and PGE2 synthesis in tumors (34) may also aid in identifying patients most likely to respond to COX-2/PGE2 and VEGF/VEGFR2 pathway inhibitors.
One limitation of this study is that our work was conducted exclusively in preclinical models. Controlled clinical trials will be required to determine if the combination of COXIBs or NSAIDs with VEGF pathway inhibitors can also aid in the prevention or treatment of advanced metastatic disease in humans. Another potential limitation of our study is that the combination of COXIBs or NSAIDs with VEGF pathway blockers could lead to increased toxicities. Indeed, the gastrointestinal toxicities of traditional NSAIDs and the cardiovascular side effects of selective COX-2 inhibitors, including celecoxib, have dampened the initial excitement for these agents in cancer prevention (35). Recently, a detailed analysis of the Adenoma Prevention with Celecoxib (APC) trial revealed that a history of atherosclerotic heart disease was the only specific risk factor associated with celecoxib-related cardiovascular toxicities (36). Furthermore, a pooled analysis of the data from 6 large randomized placebo-controlled clinical trials, a meta-analysis of 72 epidemiological studies, and an analysis of the cardiovascular outcomes of ~1.4 million patients all failed to demonstrate any increased risk of cardiovascular events due to celecoxib in people with a low baseline cardiovascular risk (26, 37–38). Taken together, these results indicate that celecoxib is relatively safe to use in people with a low cardiovascular risk. In individuals at high risk for cardiovascular disease, long term aspirin may provide a suitable alternative in combination with other procedures to control gastrotoxicity (39).
Three of the agents used in our studies, bevacizumab, axitinib, and celecoxib are clinically approved by the US FDA, and ramucirumab, the fully human anti-VEGFR2 counterpart to DC101, is in late stage (Phase III) clinical development (40). Combination of selective COX-2 inhibitors with VEGF-pathway blockers could lead to the control of metastasis in patients with colon cancer, breast cancer and other tumor types that overexpress COX-2. Alternatively, inhibitors of PGE2 synthases or PGE2 receptors EP1 to EP4 may eventually provide even safer agents to use in combination with VEGF-pathway blockers. However, additional studies will be required to determine which targets are the most suitable, because their expression patterns vary widely among normal tissues. In summary, our study suggests that agents that block the COX2/PGE2 pathway may help reduce tumor burden and enhance survival when judiciously combined with anti-angiogenic agents to treat patients with established metastatic disease.
Supplementary Material
Table S1. Original data for graphs that show composite results.
Materials and Methods
Fig. S1. Tumor volume does not correlate with VEGF levels in CT26 clones.
Fig. S2. CD45-positive inflammatory cells enter the cornea via newly formed vascular loops.
Fig. S3. PGE2 and PGA2 are the CT26 produced factors responsible for the calcium flux in reporter cells.
Fig. S4. Stable expression of COX-2 in Clone 3 and Clone 4 results in elevated COX-2 levels.
Fig. S5. COX-2 selectively upregulates PGE2 levels without affecting prostanoid mRNA expression levels.
Fig. S6. COX-2 regulates PGE2 levels in CT26 tumors in vivo.
Fig. S7. PGE2 stimulates angiogenesis in vivo.
Fig. S8. Anti-VEGFR2 antibodies can not block COX-2 induced angiogenesis.
Fig. S9. HCT/VKO-VEGF tumors express high VEGF levels in vivo.
Fig. S10. COX-2 selectively regulates PGE2 levels in HCT116 tumors in vivo.
Fig. S11. Anti-VEGFR2 antibodies and celecoxib both reduce CT26-induced tumor angiogenesis.
Fig. S12. VEGFR and COX-2 inhibition reduces tumor angiogenesis and blocks colon cancer metastasis.
Fig. S13. PGE2 levels are reduced in 4T1-luc cells following treatment with celecoxib.
Fig. S14. Whole body luciferase imaging predicts tumor burden in mice.
Fig. S15. Food consumption is unaltered in mice treated with axitinib and celecoxib.
Fig. S16. Metastases are undetectable in long term survivors treated with combined axitinib/celecoxib therapy.
Table S2. List of primers.
Acknowledgements:
We thank Drs. Bert Vogelstein and Lino Tessarollo for critical reading of the manuscript, Dr. P. Charles Lin for providing 4T1-luc cells and Dr. Long Dang for HCT116 and HCT116/VKO cells.
Funding: Supported by the Center for Cancer Research Intramural Program, NCI, NIH, a part of the U.S. Department of Health and Human Services (DHHS), and with federal funds from the NCI under contract nos. HHSN261200800001E and NIH HL34788. The content of this publication does not necessarily reflect the views or policies of the DHHS.
Footnotes
Competing interests: The authors declare that they have no competing interests.
REFERENCES AND NOTES
- 1.Kerbel RS, Tumor angiogenesis. N Engl J Med 358, 2039–2049 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patson B, C.R B, Olszanski AJ, Pharmacokinetic evaluation of axitinib. Expert Opin Drug Metab Toxicol 8, 259–270 (2012). [DOI] [PubMed] [Google Scholar]
- 3.Bergers G, Hanahan D, Modes of resistance to anti-angiogenic therapy. Nat Rev Cancer 8, 592–603 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaudhary A, Hilton MB, Seaman S, Haines DC, Stevenson S, Lemotte PK, Tschantz WR, Zhang XM, Saha S, Fleming T, St Croix B, TEM8/ANTXR1 Blockade Inhibits Pathological Angiogenesis and Potentiates Tumoricidal Responses against Multiple Cancer Types. Cancer Cell 21, 212–226 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bagri A, Kouros-Mehr H, Leong KG, Plowman GD, Use of anti-VEGF adjuvant therapy in cancer: challenges and rationale. Trends Mol Med 16, 122132 (2010). [DOI] [PubMed] [Google Scholar]
- 6.Ebos JM, Kerbel RS, Antiangiogenic therapy: impact on invasion, disease progression, and metastasis. Nat Rev Clin Oncol 8, 210–221 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ebos JM, Lee CR, Cruz-Munoz W, Bjarnason GA, Christensen JG, Kerbel RS, Accelerated metastasis after short-term treatment with a potent inhibitor of tumor angiogenesis. Cancer Cell 15, 232–239 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paez-Ribes M, Allen E, Hudock J, Takeda T, Okuyama H, Vinals F, Inoue M, Bergers G, Hanahan D, Casanovas O, Antiangiogenic therapy elicits malignant progression of tumors to increased local invasion and distant metastasis. Cancer Cell 15, 220–231 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steeg PS, Angiogenesis inhibitors: motivators of metastasis? Nat Med 9, 822823 (2003). [DOI] [PubMed] [Google Scholar]
- 10.Ellis LM, Reardon DA, Cancer: The nuances of therapy. Nature 458, 290–292 (2009). [DOI] [PubMed] [Google Scholar]
- 11.de Groot JF, Fuller G, Kumar AJ, Piao Y, Eterovic K, Ji Y, Conrad CA, Tumor invasion after treatment of glioblastoma with bevacizumab: radiographic and pathologic correlation in humans and mice. Neuro Oncol 12, 233–242 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fischer C, Jonckx B, Mazzone M, Zacchigna S, Loges S, Pattarini L, Chorianopoulos E, Liesenborghs L, Koch M, De Mol M, Autiero M, Wyns S, Plaisance S, Moons L, van Rooijen N, Giacca M, Stassen JM, Dewerchin M, Collen D, Carmeliet P, Anti-PlGF inhibits growth of VEGF(R)-inhibitor-resistant tumors without affecting healthy vessels. Cell 131, 463–475 (2007). [DOI] [PubMed] [Google Scholar]
- 13.Yang L, DeBusk LM, Fukuda K, Fingleton B, Green-Jarvis B, Shyr Y, Matrisian LM, Carbone DP, Lin PC, Expansion of myeloid immune suppressor Gr+CD11b+ cells in tumor-bearing host directly promotes tumor angiogenesis. Cancer Cell 6, 409–421 (2004). [DOI] [PubMed] [Google Scholar]
- 14.Milligan G, Marshall F, Rees S, G16 as a universal G protein adapter: implications for agonist screening strategies. Trends Pharmacol Sci 17, 235–237 (1996). [DOI] [PubMed] [Google Scholar]
- 15.Sahin M, Sahin E, Gumuslu S, Cyclooxygenase-2 in cancer and angiogenesis. Angiology 60, 242–253 (2009). [DOI] [PubMed] [Google Scholar]
- 16.Sinha P, Clements VK, Fulton AM, Ostrand-Rosenberg S, Prostaglandin E2 promotes tumor progression by inducing myeloid-derived suppressor cells. Cancer Res 67, 4507–4513 (2007). [DOI] [PubMed] [Google Scholar]
- 17.Dang DT, Chen F, Gardner LB, Cummins JM, Rago C, Bunz F, Kantsevoy SV, Dang LH, Hypoxia-inducible factor-1alpha promotes nonhypoxiamediated proliferation in colon cancer cells and xenografts. Cancer Res 66, 16841936 (2006). [DOI] [PubMed] [Google Scholar]
- 18.Dang DT, Chun SY, Burkitt K, Abe M, Chen S, Havre P, Mabjeesh NJ, Heath EI, Vogelzang NJ, Cruz-Correa M, Blayney DW, Ensminger WD, St Croix B, Dang NH, Dang LH, Hypoxia-inducible factor-1 target genes as indicators of tumor vessel response to vascular endothelial growth factor inhibition. Cancer Res 68, 1872–1880 (2008). [DOI] [PubMed] [Google Scholar]
- 19.Wu G, Luo J, Rana JS, Laham R, Sellke FW, Li J, Involvement of COX-2 in VEGF-induced angiogenesis via P38 and JNK pathways in vascular endothelial cells. Cardiovasc Res 69, 512–519 (2006). [DOI] [PubMed] [Google Scholar]
- 20.Fukuda R, Kelly B, Semenza GL, Vascular endothelial growth factor gene expression in colon cancer cells exposed to prostaglandin E2 is mediated by hypoxia-inducible factor 1. Cancer Res 63, 2330–2334 (2003). [PubMed] [Google Scholar]
- 21.Wu R, Abramson AL, Shikowitz MJ, Dannenberg AJ, Steinberg BM, Epidermal growth factor-induced cyclooxygenase-2 expression is mediated through phosphatidylinositol-3 kinase, not mitogen-activated protein/extracellular signal-regulated kinase kinase, in recurrent respiratory papillomas. Clin Cancer Res 11, 6155–6161 (2005). [DOI] [PubMed] [Google Scholar]
- 22.Vane JR, Botting RM, The mechanism of action of aspirin. Thromb Res 110, 255–258 (2003). [DOI] [PubMed] [Google Scholar]
- 23.Ristimaki A, Sivula A, Lundin J, Lundin M, Salminen T, Haglund C, Joensuu H, Isola J, Prognostic significance of elevated cyclooxygenase-2 expression in breast cancer. Cancer Res 62, 632–635 (2002). [PubMed] [Google Scholar]
- 24.Eberhart CE, Coffey RJ, Radhika A, Giardiello FM, Ferrenbach S, DuBois RN, Up-regulation of cyclooxygenase 2 gene expression in human colorectal adenomas and adenocarcinomas. Gastroenterology 107, 1183–1188 (1994). [DOI] [PubMed] [Google Scholar]
- 25.Krysan K, Reckamp KL, Sharma S, Dubinett SM, The potential and rationale for COX-2 inhibitors in lung cancer. Anticancer Agents Med Chem 6, 209–220 (2006). [DOI] [PubMed] [Google Scholar]
- 26.Harris RE, Cyclooxygenase-2 (cox-2) blockade in the chemoprevention of cancers of the colon, breast, prostate, and lung. Inflammopharmacology 17, 55–67 (2009). [DOI] [PubMed] [Google Scholar]
- 27.Van Cutsem E, Lambrechts D, Prenen H, Jain RK, Carmeliet P, Lessons from the adjuvant bevacizumab trial on colon cancer: what next? J Clin Oncol 29, 1–4 (2011). [DOI] [PubMed] [Google Scholar]
- 28.Oyan B, Why do targeted agents not work in the adjuvant setting in colon cancer? Expert Rev Anticancer Ther 12, 1337–1345 (2012). [DOI] [PubMed] [Google Scholar]
- 29.Allegra CJ, Yothers G, O’Connell MJ, Sharif S, Petrelli NJ, Lopa SH, Wolmark N, Bevacizumab in stage II-III colon cancer: 5-year update of the National Surgical Adjuvant Breast and Bowel Project C-08 trial. J Clin Oncol 31, 359–364 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Francia G, Cruz-Munoz W, Man S, Xu P, Kerbel RS, Mouse models of advanced spontaneous metastasis for experimental therapeutics. Nat Rev Cancer 11, 135–141 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Day CP, Carter J, Bonomi C, Hollingshead M, Merlino G, Preclinical therapeutic response of residual metastatic disease is distinct from its primary tumor of origin. Int J Cancer 130, 190–199 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Padera TP, Kuo AH, Hoshida T, Liao S, Lobo J, Kozak KR, Fukumura D, Jain RK, Differential response of primary tumor versus lymphatic metastasis to VEGFR-2 and VEGFR-3 kinase inhibitors cediranib and vandetanib. Mol Cancer Ther 7, 2272–2279 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jayson GC, Hicklin DJ, Ellis LM, Antiangiogenic therapy--evolving view based on clinical trial results. Nat Rev Clin Oncol 9, 297–303 (2012). [DOI] [PubMed] [Google Scholar]
- 34.Liao X, Lochhead P, Nishihara R, Morikawa T, Kuchiba A, Yamauchi M, Imamura Y, Qian ZR, Baba Y, Shima K, Sun R, Nosho K, Meyerhardt JA, Giovannucci E, Fuchs CS, Chan AT, Ogino S, Aspirin use, tumor PIK3CA mutation, and colorectal-cancer survival. N Engl J Med 367, 1596–1606 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grosser T, Yu Y, Fitzgerald GA, Emotion recollected in tranquility: lessons learned from the COX-2 saga. Annu Rev Med 61, 17–33 (2010). [DOI] [PubMed] [Google Scholar]
- 36.Bertagnolli MM, Eagle CJ, Zauber AG, Redston M, Breazna A, Kim K, Tang J, Rosenstein RB, Umar A, Bagheri D, Collins NT, Burn J, Chung DC, Dewar T, Foley TR, Hoffman N, Macrae F, Pruitt RE, Saltzman JR, Salzberg B, Sylwestrowicz T, Hawk ET, Five-year efficacy and safety analysis of the Adenoma Prevention with Celecoxib Trial. Cancer Prev Res (Phila) 2, 310321 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Solomon SD, Wittes J, Finn PV, Fowler R, Viner J, Bertagnolli MM, Arber N, Levin B, Meinert CL, Martin B, Pater JL, Goss PE, Lance P, Obara S, Chew EY, Kim J, Arndt G, Hawk E, Cardiovascular risk of celecoxib in 6 randomized placebo-controlled trials: the cross trial safety analysis. Circulation 117, 2104–2113 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Graham DJ, Campen D, Hui R, Spence M, Cheetham C, Levy G, Shoor S, Ray WA, Risk of acute myocardial infarction and sudden cardiac death in patients treated with cyclo-oxygenase 2 selective and non-selective non-steroidal anti-inflammatory drugs: nested case-control study. Lancet 365, 475–481 (2005). [DOI] [PubMed] [Google Scholar]
- 39.Wang D, DuBois RN, The role of anti-inflammatory drugs in colorectal cancer. Annu Rev Med 64, 131–144 (2013). [DOI] [PubMed] [Google Scholar]
- 40.Reichert JM, Antibodies to watch in 2013: Mid-year update. MAbs 5, 513–517 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Original data for graphs that show composite results.
Materials and Methods
Fig. S1. Tumor volume does not correlate with VEGF levels in CT26 clones.
Fig. S2. CD45-positive inflammatory cells enter the cornea via newly formed vascular loops.
Fig. S3. PGE2 and PGA2 are the CT26 produced factors responsible for the calcium flux in reporter cells.
Fig. S4. Stable expression of COX-2 in Clone 3 and Clone 4 results in elevated COX-2 levels.
Fig. S5. COX-2 selectively upregulates PGE2 levels without affecting prostanoid mRNA expression levels.
Fig. S6. COX-2 regulates PGE2 levels in CT26 tumors in vivo.
Fig. S7. PGE2 stimulates angiogenesis in vivo.
Fig. S8. Anti-VEGFR2 antibodies can not block COX-2 induced angiogenesis.
Fig. S9. HCT/VKO-VEGF tumors express high VEGF levels in vivo.
Fig. S10. COX-2 selectively regulates PGE2 levels in HCT116 tumors in vivo.
Fig. S11. Anti-VEGFR2 antibodies and celecoxib both reduce CT26-induced tumor angiogenesis.
Fig. S12. VEGFR and COX-2 inhibition reduces tumor angiogenesis and blocks colon cancer metastasis.
Fig. S13. PGE2 levels are reduced in 4T1-luc cells following treatment with celecoxib.
Fig. S14. Whole body luciferase imaging predicts tumor burden in mice.
Fig. S15. Food consumption is unaltered in mice treated with axitinib and celecoxib.
Fig. S16. Metastases are undetectable in long term survivors treated with combined axitinib/celecoxib therapy.
Table S2. List of primers.