Abstract
Objectives:
To predict the duration of any breastfeeding using the duration of exclusive breastfeeding in a socioeconomically heterogeneous sample of mothers using Receiver Operator Characteristic (ROC) analysis.
Study design:
The Mother Baby Health Survey, a birth certificate-linked cross-sectional survey was sent at 4–5 months postpartum to a stratified random sample of socioeconomically and racially diverse women in upstate New York; 797 mothers who initiated exclusive breastfeeding were included in this study. Split-sample validation was employed; eligible subjects were divided into training or test samples at random (80% and 20%, respectively). ROC curves were constructed using the training sample and optimal exclusive breastfeeding duration thresholds were tested using the remaining test sample. Logistic regression using the training sample provided estimates of the predictive ability (sensitivity, specificity, positive predictive value) of thresholds in both unadjusted and adjusted analyses (covariates: age, education, parity, marital status, race).
Results:
The ROC analysis in this sample demonstrated that 9 weeks of exclusivity was required for maintenance of breastfeeding at 3 months, and 14.9 weeks of exclusivity was required for maintenance at 20 weeks. Unadjusted and adjusted models yielded similar results; women who exclusively breastfed for at least 9 weeks had 2.2 times the risk (95%CI:1.7–2.8) of maintaining any breastfeeding at 3 months.
Conclusions:
These results are similar to our previous results, from a less diverse cohort, and support that these thresholds may be useful in clinical settings for helping mothers achieve breastfeeding duration goals.
Keywords: Exclusive breastfeeding, Breastfeeding duration, Receiver Operating Characteristic (ROC) curves, Healthy People 2020 Breastfeeding Targets
Breastfeeding has numerous short- and long-term health benefits for both mother and infant (1–4). In light of these benefits, exclusive breastfeeding has been broadly recommended for the first 6 months after birth (5–8). The Healthy People 2020 breastfeeding objectives include increasing the proportion of infants who ever breastfed (initiation), are exclusively breastfed at 3 and 6 months postpartum, and continue to receive human milk at 6 months and 1 year (9). As of 2016, the targets for these objectives are currently unmet in the vast majority of states (10). National rates for exclusive breastfeeding at 3 and 6 months are increasing but remain suboptimal (9, 10). In the United States, initiation, exclusivity, and duration of breastfeeding vary by maternal demographic factors including income, educational attainment, insurance status, race, and ethnicity (11–14). Lower income mothers, those with fewer years of education, those with public insurance and those who identify as a racial or ethnic minority are less likely to meet breastfeeding recommendations, indicating the need for continued efforts aimed at helping women breastfeed longer, especially those at risk of not meeting targets (14–17).
A positive association between the duration of exclusive breastfeeding and the duration of any breastfeeding has been repeatedly demonstrated in the literature (19–23). Our previous study demonstrated showed that the duration of exclusive breastfeeding can be used to predict the duration of any breastfeeding out to 12 months using ROC curves (24). These models allowed for the determination of the optimal length of exclusive breastfeeding that predicted any breastfeeding at 12 months postpartum and were proposed for use in helping mothers meet their breastfeeding duration goals. The participants were predominantly white, educated, partnered and primarily multiparous women, therefore, in order to determine if this type of analysis would be broadly applicable, a similar methodology was applied to a more diverse group of mothers. We hypothesized that despite differences in demographic make-up of the samples, the optimal length of exclusive breastfeeding that predicts any breastfeeding would be similar in both samples.
METHODS
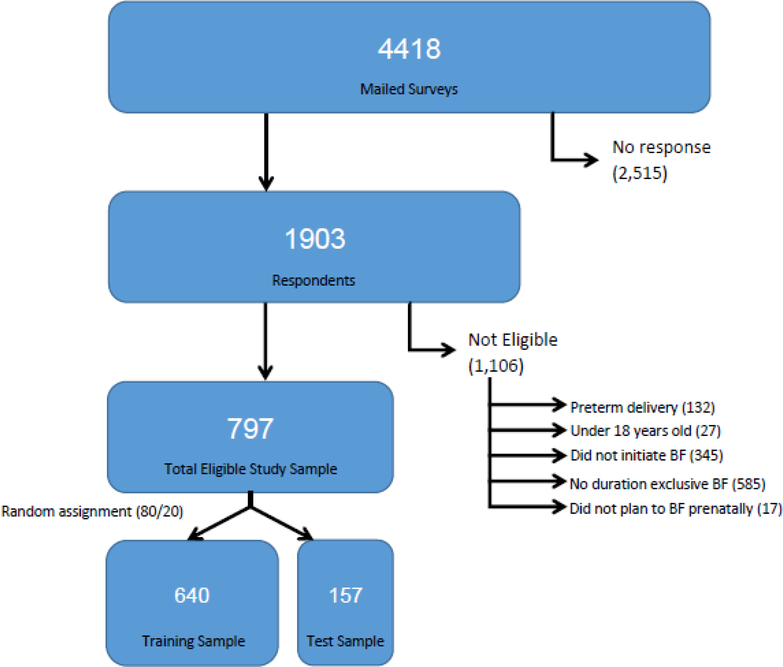
Eligible mothers who responded to the Mother and Baby Health Survey (MBHS) were included in the analysis. The cross-sectional survey was administered to a stratified randomized sample of women who had a live birth in Monroe County, New York between 2009 and 2011. Low income mothers were oversampled to ensure adequate representation in the study sample. Surveys were mailed to mothers between 4–5 months postpartum, and non-responders were contacted by phone. As shown in Figure 1 (available at www.jpeds.com), 1903/4418 surveys were returned, resulting in a 43% response rate. Details regarding the survey methodology can be found in a previous publication (25). MBHS survey respondents were excluded from the current analysis if they delivered the infant before 37 weeks gestation (n=132), were < 18 years of age (n=27), did not initiate breastfeeding (n=345), did not have at least one day of exclusive breastfeeding (n=585), or did not plan to breastfeed during pregnancy (n=17). Breastfeeding duration and exclusivity metrics were based on maternal self-report in the MBHS. The initiation of exclusive breastfeeding was confirmed using birth certificate data. Demographic information also was obtained from the birth certificate, including maternal age group, education level, income status (defined as having a Medicaid funded delivery and/or being on WIC prenatally), race and parity. Additional potential confounders included in the analysis were infant age at survey completion (source: MBHS), and exclusive breastfeeding plan (source: MBHS). For these secondary analyses, responses were not weighted. Detailed information about survey materials, data collection and handling is described in a previous publication (25). Consistent with the analysis conducted by Brownell et al (24), exclusive breastfeeding was considered the exposure variable, and was defined as the amount of time that elapsed between breastfeeding initiation and the last day of exclusive breastfeeding. The outcome of interest, maintenance of any breastfeeding, was defined as the time between breastfeeding initiation and the last day of any breastfeeding or date of survey completion, if still breastfeeding.
Fig 1.
Flow diagram of participants.
Split-sample validation methodology was adopted as described by Brownell et al (24). Subjects were divided into either training and test samples (80% and 20%, respectively) at random, and chi-square tests were used to compare maternal demographics, exclusive breastfeeding plan, and breastfeeding duration and exclusivity metrics between the training (80%) and test (20%) samples. For mothers in this sample, the actual duration of breastfeeding is likely longer than captured by the survey, thus the predicted duration of any breastfeeding is a conservative estimate.
This split sample method was utilized in order to avoid the overly optimistic estimates of model performance generated when models are evaluated using the same data used to build the model (26), and the 80%-20% split was modeled after a prior publication (24). The training sample was used for optimal threshold determination, and the test sample was used to evaluate the predictive ability of these thresholds.
The training sample was used to determine exclusive breastfeeding duration thresholds based on optimized model predictive ability. The training sample was used to create ROC curves for each time point in order to estimate the minimum duration of exclusive breastfeeding associated with continuation of any breastfeeding at that point in time. Optimal thresholds were determined by minimizing the difference between sensitivity (the percent of mothers for which the exclusive breastfeeding threshold correctly predicted duration of any breastfeeding through at least the specified maintenance time point) and specificity (the percent of mothers for which the exclusive breastfeeding threshold correctly predicted duration of any breastfeeding ending before the specified maintenance time point) for each time point from 4 weeks extending through 20 weeks postpartum (based on the proportion of survey responses through this duration).
After optimization, the test sample was used to assess the performance (sensitivity and specificity) of these thresholds in a demographically similar, but distinct set of subjects. The positive predictive value of each threshold was calculated to determine the percentage of women maintaining any breastfeeding at the next time point. The attributable risk reduction of each threshold estimated the difference in risk of any breastfeeding between women who exclusively breastfed and those who did not exclusively breastfeed at a given time point. Potential confounders were identified a priori and included maternal age, maternal education, parity, marital status, race, baby age at survey completion and exclusive breastfeeding plan. Bivariate associations between these potential confounders and the predictor variables (exclusivity thresholds) and outcomes (any breastfeeding duration estimates) were assessed to evaluate potential confounding using Chi-Square tests for all categorical variables. T-tests were used for baby age at survey completion, the only continuous covariate. Covariates associated with both the predictor and outcome variables (p < 0.10) were considered potential confounders. Logistic regression applied to the test sample provided estimates of the predictive ability of thresholds in both an unadjusted analysis and an analysis adjusted for age, maternal education, parity, marital status, and race. Thresholds from a previous publication (24) were tested using the methods described above using the full sample. In addition to the methods outlined by Brownell et al (24), Poisson regression was implemented evaluate the risk (rather than odds) of breastfeeding maintenance using the newly calculated thresholds, along with the thresholds from Brownell’s 2015 publication.
Analyses were conducted in SAS v. 9.4. Significance was set at an alpha level < 0.05 and all P values were 2 sided. These secondary analyses were approved by the University of Rochester Research Subjects Review Board.
RESULTS
Women who initiated exclusive breastfeeding and met additional inclusion criteria (n = 797) were included in this study. All but one mother had stopped exclusive breastfeeding by the time the survey was returned and 98% reported any current breastfeeding on the date of survey completion. There were no significant differences between training and test samples in terms of maternal demographics, exclusive breastfeeding plan, breastfeeding duration and exclusivity metrics, or infant age at survey completion (Table 1).
Table 1:
Sample Demographics
| Total study sample N = 797 | 80% training sample N = 640 | 20% test sample N = 157 | ||
|---|---|---|---|---|
| Maternal Demographics | N (%) | N (%) | N (%) | P-value |
| Age* | ||||
| 18–24 | 134 (16.8) | 105 (16.4) | 29 (18.5) | 0.37 |
| 25–34 | 516 (64.7) | 411 (64.2) | 105 (66.9) | |
| 35 | 147 (18.4) | 124 (19.4) | 23 (14.6) | |
| Education* | ||||
| High school or less | 175 (22.0) | 134 (20.9) | 41 (26.1) | 0.38 |
| Some college | 201 (25.2) | 163 (25.5) | 38 (24.2) | |
| Completed college | 420 (52.7) | 342 (53.4) | 78 (49.7) | |
| Race Non-white | 135 (16.9) | 106 (16.6) | 29 (18.5) | 0.57 |
| White | 662 (83.1) | 534 (83.4) | 128 (81.5) | |
| Parity | ||||
| No prior pregnancy | 362 (46.0) | 289 (45.8) | 73 (46.8) | 0.82 |
| Prior pregnancy | 425 (54.0) | 342 (54.2) | 83 (53.2) | |
| Missing | 10 | 9 | 1 | |
| Marital Status | ||||
| Single (no support) | 226 (28.4) | 180 (28.1) | 46 (29.3) | 0.77 |
| Married | 571 (71.6) | 460 (71.9) | 111 (70.7) | |
| Income | ||||
| Low Income | 291(36.5) | 226(35.3) | 65(41.4) | 0.16 |
| Non-Low Income | 506(63.5) | 414(64.7) | 92(58.6) | |
| Exclusive Breastfeeding Plan | ||||
| Not exclusive BF | 66 (8.3) | 53 (8.3) | 13 (8.3) | 1.00 |
| Exclusive BF | 731 (91.7) | 587 (91.7) | 144 (91.7) | |
| Infant age at survey date (weeks) | Mean (sd) | Mean (sd) | Mean (sd) | |
| 21.0 (3.7) | 21.0 (3.8) | 21.0 (3.6) | 0.99 | |
| Any Breastfeeding at 12 weeks | ||||
| No | 189 (23.7) | 154 (24.1) | 35 (22.3) | 0.64 |
| Yes | 608 (76.3) | 486 (75.9) | 122 (77.7) | |
| Any Breastfeeding at 3 months (13 weeks)a | ||||
| No | 238 (29.9) | 189 (29.5) | 49 (31.2) | 0.68 |
| Yes | 559 (70.1) | 451 (70.5) | 108 (68.8) | |
| Any Breastfeeding at 20 weeks | ||||
| No | 695 (87.2) | 564 (88.1) | 131 (83.4) | 0.12 |
| Yes | 102 (12.8) | 76 (11.9) | 26 (16.6) |
Categories do not sum to 100% due to rounding error
This additional timeframe was provided as Brownell et al’s23 analysis used 3 months.
The average time surveys were returned was 21 weeks postpartum (SD = 3.7 weeks). In the 80% training sample, 45% of respondents reported continuation of breastfeeding through at least 20 weeks postpartum, allowing for statistical estimation of the optimal period of exclusive breastfeeding needed to maintain any breastfeeding at this time point. Threshold estimates were not reported for time points beyond 20 weeks, as the majority of women returned the survey at or before 21 weeks, and the number of women maintaining breastfeeding in the training sample beyond this time was too small to be useful for prediction purposes (fewer than 20 women in the training sample with available data at 24 weeks or later were continuing to breastfeed).
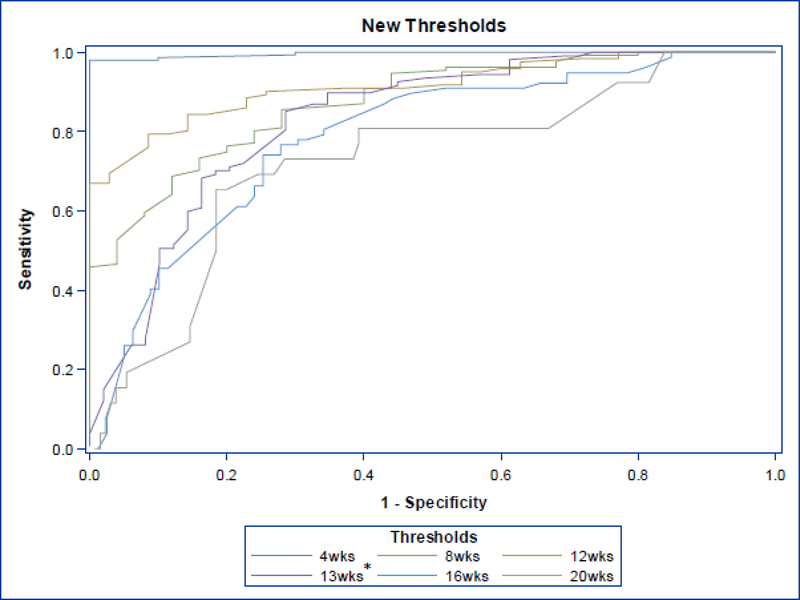
The training sample (n = 640) was used to determine the optimal minimum threshold durations of exclusive breastfeeding to predict maintenance of breastfeeding at 6 time points throughout the first 20 weeks of life beginning at 4 weeks by minimizing the difference between sensitivity and specificity of these models, resulting in the largest area under the ROC curve. The minimum duration of exclusive breastfeeding required for maintenance of any breastfeeding at these time points was 3 weeks of exclusivity for maintenance of any breastfeeding at 4 weeks, and 14.9 weeks of exclusivity for maintenance of any breastfeeding at 20 weeks. The test sample was used to determine the sensitivity and specificity of the selected exclusivity thresholds. The sensitivity and specificity of the 3-week exclusive breastfeeding threshold were 88.6% and 82.0% respectively, and the 14.9 week exclusivity threshold predicted any breastfeeding at 20 weeks with a sensitivity and specificity of 64.5% (Table 2). Figure 2 (available at www.jpeds.com) contains ROC curves generated in the test sample. The respective thresholds had moderate ability to correctly predict breastfeeding maintenance through 20 weeks, with positive likelihood ratios ranging from 1.8 – 5.5 (Table 2). The estimates had positive predictive values of 100% at 4 weeks, and 28.6% at 20 weeks. The attributable risk estimates indicate that the risk of any breastfeeding at 4 weeks was 32.3% greater among those women who exclusively breastfed through 3 weeks, compared with women who did not meet this exclusivity threshold. Similarly, breastfeeding exclusively through 14.9 weeks resulted in an attributable risk estimate of 65.3%, indicating that maintenance through this threshold increased the likelihood of maintaining any breastfeeding at 20 weeks by 65.3%.
Table 2:
Maintenance of Any Breastfeeding Predicted by Exclusive Breastfeeding Threshold Estimates and Threshold Diagnostic Statistics
| N (% of training sample) | Maintenance of any BF | Exclusive BF threshold (weeks) | Sensitivitya (%) | Specificityb (%) | Positive Likelihood Ratioc | Positive predictive valued (%) | Attributable risk reductione (%) |
|---|---|---|---|---|---|---|---|
| 590 (92.2) | 4 weeks | 3.0 | 88.6 | 82.0 | 4.9 | 100.0% | 32.3% |
| 541 (84.5) | 8 weeks | 5.0 | 83.2 | 84.8 | 5.5 | 93.7% | 35.0% |
| 486 (75.9) | 12 weeks | 8.6 | 77.4 | 76.6 | 3.3 | 97.7% | 45.9% |
| 451 (70.5) | 3 monthsf | 9.0 | 72.7 | 83.5 | 4.4 | 88.5% | 50.0% |
| 323 (50.5) | 16 weeks | 12.9 | 71.5 | 66.6 | 2.1 | 74.2% | 58.6% |
| 76 (11.9) | 20 weeks | 14.9 | 64.5 | 64.5 | 1.8 | 28.6% | 65.3% |
Sensitivity: The percent of mothers in the test sample for which the exclusive breastfeeding threshold (calculated in the training sample) correctly predicted duration of any breastfeeding through at least the specified maintenance time point.
Specificity: The percent of mothers in the test sample for which the exclusive breastfeeding threshold correctly predicted duration of any breastfeeding ending before the specified maintenance time point.
Positive Likelihood Ratio: The probability that someone who met the exclusivity threshold, also met the predicted duration
Positive Predictive Value: The percentage of mothers in the test sample who were predicted to have maintained any breastfeeding through a given time point based on the duration of their exclusivity, and truly did breastfeed to or beyond that maintenance point.
Attributable Risk Reduction: The percentage reduction in risk of failing to maintain any breastfeeding at a maintenance time point among mothers who met or exceeded the exclusivity threshold, compared to women who did not meet this exclusivity threshold. The inverse yields the number needed to treat (1/ARR).
This additional timeframe was provided as Brownell et al’s23 analysis used 3 months.
Fig 2.
ROC curves (1 for each threshold 4- to 20-week) generated using test sample of the MBHS data set (n = 157) to evaluate the thresholds presented calculated in the current analysis. *13 weeks = 3-month threshold.
Confounding assessment demonstrated that maternal age, maternal education, and marital status were associated with both the maintenance of any breastfeeding (outcome) and exclusivity threshold achievement (predictor) in the majority of time points. Crude and adjusted odds ratios were calculated using the training sample to allow for direct comparison with prior findings (24) (Table 3), however, given that the outcomes (breastfeeding maintenance) are common in this sample (>10%), risk ratios also are reported in Table 3. The training sample was used to calculate crude and adjusted risk ratios for maintenance of any breastfeeding from 4–20 weeks based on the duration of breastfeeding exclusivity. Unadjusted and adjusted relative risk of maintaining any breastfeeding associated with maintenance through the respective exclusivity threshold are reported for each time point (Table 3). Maternal age, maternal education, parity, marital status, and race-adjusted estimates were similar to corresponding unadjusted estimates at all time points evaluated (Table 3).The threshold estimates were significantly associated with maintenance of breastfeeding from the 4 – 20 week time points in both unadjusted and adjusted models (Table 3). In adjusted models, none of the covariates included in multivariable models were consistently associated with the outcome (only maternal race was significantly associated with the outcome, and only in the 20 week duration model, p = 0.03; all others p > 0.05), and the effect estimates in all adjusted models changed less than 10% from the respective crude estimates.
Table 3:
Unadjusted and Adjusted RRs – adjusted for age, maternal education, parity, partner support, and race
| N (% of training sample) | Maintenance of any BF | Exclusive BF threshold (weeks) | Unadjusted model RR (95% CI) | Adjusted model RR (95% CI) | Unadjusted model OR (95% CI) | Adjusted model OR (95% CI) |
|---|---|---|---|---|---|---|
| 590 (92.2) | 4 weeks | 3.0 | 1.9 (1.5, 2.3) | 1.8 (1.4, 2.3) | 35.6 (16.5, 76.4) | 41.6 (18.2, 95.2) |
| 541 (84.5) | 8 weeks | 5.0 | 1.9 (1.5, 2.3) | 1.8 (1.5, 2.3) | 27.7 (15.3, 50.1) | 28.5 (15.3, 53.1) |
| 486 (75.9) | 12 weeks | 8.6 | 2.1 (1.7, 2.6) | 2.0 (1.6, 2.4) | 11.2 (7.3, 17.2) | 11.8 (7.4, 18.8) |
| 451 (70.5) | 3 monthsa | 9.0 | 2.3 (1.8, 2.9) | 2.2 (1.7, 2.8) | 13.6 (8.8, 21.0) | 13.9 (8.7, 22.3) |
| 323 (50.5) | 16 weeks | 12.9 | 2.8 (1.8, 4.6) | 2.9 (1.8, 4.8) | 5.0 (3.6, 7.0) | 4.7 (3.3, 6.7) |
| 76 (11.9) | 20 weeks | 14.9 | 1.9 (1.5, 2.3) | 1.8 (1.4, 2.3) | 3.3 (2.0, 5.4) | 3.5 (2.1, 5.9) |
This additional timeframe was provided as Brownell et al’s23 analysis used 3 months.
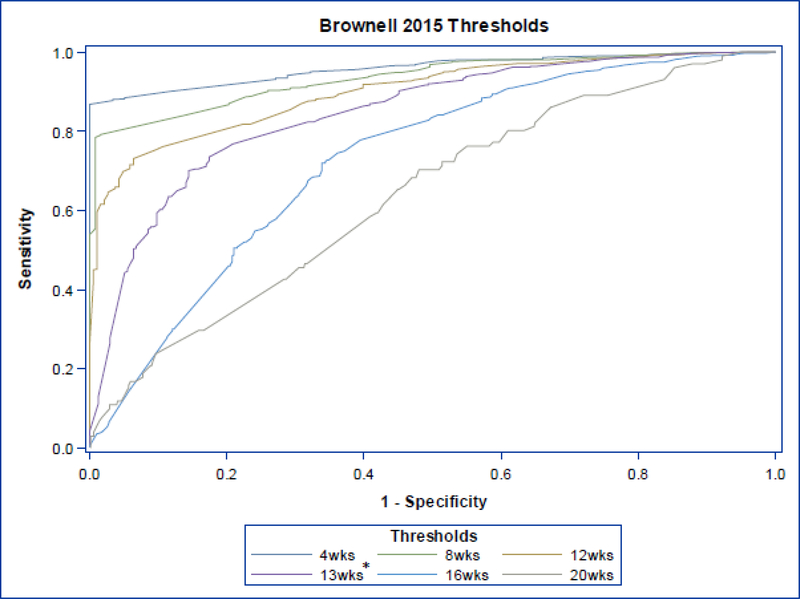
The full sample (N = 797) was used to test the threshold estimates (24), and results demonstrated similar performance (Table 4). Figure 3 (available at www.jpeds.com) contains ROC curves generated using the 2015 publication’s thresholds with the full current data set.
Table 4:
Validation of Brownell’s Previously Published Exclusivity Thresholds: Maintenance of Any Breastfeeding Predicted by Exclusive Breastfeeding Threshold Estimates and Threshold Diagnostic Statistics
| Maintenance of any BF | Brownell’s Exclusive BF threshold (weeks) | Sensitivitya (%) | Specificityb (%) | Positive predictive valuec (%) | Attributable risk reductiond (%) | Adjusted RR (95%CI) | Adjusted OR (95%CI) |
|---|---|---|---|---|---|---|---|
| 4 weeks | 4.0 | 86.0 | 100.0 | 100.0 | 36.8 | 1.6 (1.3 – 1.9) | 755.2(52.9 - >999)* |
| 8 weeks | 7.0 | 78.2 | 99.2 | 99.8 | 45.4 | 1.8 (1.5 – 2.2) | 301.8 (61.6 - >999) * |
| 12 weeks | 8.7 | 71.5 | 94.2 | 97.5 | 48.2 | 1.9 (1.6 – 2.3) | 39.7 (20.8 – 75.7) |
| 3 monthse | 9.6 | 71.9 | 83.2 | 91.0 | 46.7 | 1.9 (1.6 – 2.4) | 12.0 (8.0 – 18.1) |
| 16 weeks | 11.1 | 72.0 | 65.7 | 67.9 | 37.9% | 2.2 (1.7 – 2.7) | 4.6 (3.3 – 6.3) |
| 20 weeks | 12.1 | 69.6 | 50.4 | 17.1 | 8.9 | 2.1 (1.4 – 3.3) | 2.4 (1.5 – 3.7) |
Sensitivity: The percent of mothers in the test sample for which the exclusive breastfeeding threshold (calculated in the training sample) correctly predicted duration of any breastfeeding through at least the specified maintenance time point.
Specificity: The percent of mothers in the test sample for which the exclusive breastfeeding threshold correctly predicted duration of any breastfeeding ending before the specified maintenance time point.
Positive Predictive Value: The percentage of mothers in the test sample who were predicted to have maintained any breastfeeding through a given time point based on the duration of their exclusivity, and truly did breastfeed to or beyond that maintenance point.
Attributable Risk Reduction: The percentage reduction in risk of failing to maintain any breastfeeding at a maintenance time point among mothers who met or exceeded the exclusivity threshold, compared to women who did not meet this exclusivity threshold. The inverse yields the number needed to treat (1/ARR).
This additional timeframe was provided as Brownell et al’s23 analysis used 3 months.
Due to zero cells, OR and 95% CI calculated using Firth’s Penalized Likelihood (1)
Fig 3.
ROC curves (1 for each threshold 4- to 20-week) generated using full MBHS data set (n = 797) to evaluate the thresholds presented in Brownell et al.23 *13 weeks = 3-month threshold.
DISCUSSION
Data from the MBHS sample were used to determine the optimal minimum length of exclusive breastfeeding associated with continuation of breastfeeding out to 20 weeks postpartum. This study is a modified replication of our previous study (24), and was conducted among women in upstate New York. This strategy for estimating the optimal minimum length of exclusive breastfeeding is a tool that can be used in meeting Healthy People 2020 breastfeeding targets. Increasing the number of mother-infant dyads achieving longer durations of exclusive and any breastfeeding is a critical goal for the improvement of health on a national scale.
Mothers who exclusively breastfeed for at least 9 weeks were more likely to continue any breastfeeding at 3 months. Longer maintenance of exclusive breastfeeding (14.9 weeks) was associated with increased duration of any breastfeeding through 20 weeks. Because surveys were sent out between 4 and 5 months postpartum, the data set implemented for this analysis did not have a sufficient number of mothers who reported long enough breastfeeding durations to determine if early exclusive breastfeeding could predict maintenance of breastfeeding at the Healthy People 2020 duration target of 6 months or longer. Testing this hypothesis will require a larger sample with longer duration breastfeeding.
Our results are consistent with our priror report (24), a study that was conducted in a relatively homogeneous sample across race, parity, partner status and post high school education, and with higher than national average breastfeeding duration (27, 28). Our respondents from upstate New York had lower than national average duration for that year (29). The fact that we obtained similar results despite breastfeeding duration differences and data from a more socio-economically heterogeneous sample indicates that the threshold estimates may be generalizable across other populations. The previous study reported exclusivity of a minimum of 8.7 weeks predicted maintenance at 12 weeks, and 12.1 weeks of exclusivity as predicted breastfeeding maintenance at 20 weeks (24). These findings are similar to the results of our analysis (Table 2)m which included a large number of low income mothers, along with a larger proportion of non-white women.
Additionally, the adjusted and unadjusted predicted duration estimates (Table 3) were similar, indicating that confounding by included covariates was minimal, and further highlighting the robustness of these analyses. The variables included in the adjusted analysis have been consistently associated with breastfeeding duration and continuation in prior literature, but in this analysis, only maternal education was a confounder of the relationship of interest (15–17). The magnitude of confounding was very small, yielding similar crude and adjusted odds ratios.
There are several limitations of this study. The MBHS was mailed to mothers between 4 and 5 months after giving birth, and included questions asking mothers to recall information about their pre-pregnancy experience, during pregnancy, and the postpartum period up until the time the survey was returned. There was concern that mothers may not have been able to accurately recall pre-pregnancy behavior if asked too late in the postpartum period. For this reason, the 4 to 5 month time period was selected for survey distribution. Due to these constraints, we did not have infant feeding outcome data out to 6 months. Given that this dataset was collected through a surveillance methodology, it was not possible to collect follow-up information from mothers who were currently breastfeeding at the time of survey completion. Furthermore, it is difficult to collect breastfeeding data at extended time points because many mothers stop breastfeeding well before reaching these targets. A larger sample will be required in order to provide adequate statistical power at 6 and 12 month time points.
Confounders that were not evaluated include maternal medical conditions (depression, polycystic ovarian syndrome), obesity, delivery method, breastfeeding support practices in institutional and community settings, return to work, and utilization of child care may have resulted in residually confounded effect estimates based on their association with breastfeeding outcomes (30–32). Maternal return to work status was not available in the data set utilized from the MBHS and birth certificate, and although several of the other potential confounders could have been extracted (delivery method, obesity, and some medical conditions), we did not include these variables in our analysis to ensure direct comparability with the publication that this replication is based on. Additionally, the expected degree of confounding by these unmeasured confounders is relatively small; we anticipate that these factors would also be associated with the demographic variables included in multivariate models and with the same directionality. For example, low socioeconomic status is associated with increased risk of overweight/obesity (33), and is associated with poor breastfeeding outcomes. Maternal obesity is also associated with poor breastfeeding outcomes (30). Excluding confounders (e.g. obesity) with this pattern of association results in a small degree of residual confounding (34). Similar relationships are expected with the other confounders that were not included in multivariable analyses.
As with all survey-based methodologies, the data used in this project is subject to nonresponse bias, however these concerns are offset by the relatively high response rate (43%) and oversampling of low income women to increase their representation. Further reducing concern about non-response bias, Dozier et al. (25) demonstrated that the MBHS respondents from which this study sample was drawn were representative of the general population with few differences; white respondents, those aged 30–39 and those who had completed high school were slightly over-represented before weighting. Additionally, this study utilized self-report survey data linked to the birth certificate to provide data on key covariates for adjusted analyses and allowed for validation of key survey questions (breastfeeding initiation), as well as allowing for accurate replacement of missing survey data.
Replication of our methodology in a more heterogeneous sample demonstrates the robust nature of this novel application of ROC curves for prediction of breastfeeding duration using early exclusivity. Despite the different demographics between these two samples, the fact that the threshold estimates calculated in these separate samples were very similar and demonstrate consistency (35). This consistency may be explained by one or a combination of two hypotheses; a psychosocial mechanism and physiological mechanism. From a psychosocial perspective, women who breastfeed exclusively early in the postpartum period are likely to have enabling environmental and motivational factors in combination with normal physiology that underlie this behavior. These factors that enable exclusive breastfeeding in the early postpartum period may also foster continued breastfeeding in the following weeks. However, even after adjustment for several demographic proxies of these environmental factors (maternal age, maternal education, parity, marital status, and race) and evaluation in a sample of women who all shared prenatal intent to breastfeed (over 90% of whom intended to exclusively breastfeed), exclusivity thresholds significantly predicted breastfeeding duration. From a biological perspective, prolactin levels play a critical role in the establishment of breastmilk in the first weeks following delivery. Prolactin levels are increased with increased nipple stimulation and lead to establishment of a milk supply that is based on the number of feeds the child receives (36). Given that the first weeks are particularly important for establishing this supply, it is plausible that early exclusivity is helpful for maintaining a milk supply at later time points. This theory is consistent with our finding that there was limited confounding by demographic factors as evidenced by very similar point estimates resulting from adjusted and unadjusted models.
Future, prospective studies evaluating the physiological response to early exclusive breastfeeding and its impact on duration of breastfeeding continuation should be completed to better understand this proposed biological link, and additional studies evaluating the role of psychosocial and motivating factors that facilitate early exclusivity and continued duration are warranted.
The utility of exclusivity threshold estimates has not been evaluated in a clinical setting, the applicability is evident. In the clinical setting, providing mothers with concrete targets for exclusive breastfeeding duration that may encourage mothers who are facing breastfeeding difficulties to continue or dissuade them from supplementing with formula early on. Using this as a discussion point with additional encouragement and support (e.g. appropriate referrals to peer counselors, lactation consultants, breastfeeding medicine providers, and community support groups) may help mothers meet their breastfeeding duration goals, and in turn, extending their duration of exclusivity. Future studies should evaluate the clinical utility of utilizing exclusivity targets for helping mothers achieve their breastfeeding duration goals.
Acknowledgements:
The authors would like to acknowledge the invaluable efforts of the following individuals: Gyuhyeong Goh PhD1, Mary Lussier BSN, IBLCL2, and Trudy Lerer MS2 whose work on the original study provided the foundation for this work.
1University of Kansas, Lawrence, KS USA, 2Connecticut Children’s Medical Center, Hartford, CT USA
Supported by National Institutes of Health funding from PHS (RO1-HD055191), Community Partnership for Breastfeeding Promotion and Support (NICHD). The funder had no role in the design, collection, analysis and interpretation of data, the writing of the report, or the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors declare no conflicts of interest.
Abbreviations and Acronyms:
- ROC
Receiver Operator Characteristic
- MBHS
Mother Baby Health Survey
Footnotes
Portions of this study were presented as a poster at International Society for Research in Human Milk and Lactation meeting, << >>, 2016, Stellenbosch, South Africa.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ann M. Dozier, Department of Public Health Sciences, University of Rochester Medical Center, 265 Crittenden Blvd. CU 420644, Rochester, NY 14642.
Elizabeth A. Brownell, The Connecticut Human Milk Research Center, Division of Neonatology, Connecticut Children's Medical Center, Hartford, CT; Department of Pediatrics, University of Connecticut School of Medicine, Farmington, CT.
Kelly Thevenet-Morrison, Department of Public Health Sciences, University of Rochester Medical Center, Rochester, NY, Hayley Martin, BS, Department of Public Health Sciences, University of Rochester Medical Center, Rochester, NY.
James I Hagadorn, The Connecticut Human Milk Research Center, Division of Neonatology, Connecticut Children's Medical Center, Hartford, CT; Department of Pediatrics, University of Connecticut School of Medicine, Farmington, CT.
Cynthia Howard, Department of Public Health Sciences, Department of Pediatrics, University of Rochester, Rochester, NY; Rochester General Hospital, Rochester, NY.
References
- 1.Lawrence RM, Lawrence RA. Breastfeeding: More than just good nutrition. Pediatrics in Review. 2011;32(7):267–80. [DOI] [PubMed] [Google Scholar]
- 2.Ip S, Chung M, Raman G, Trikalinos TA, Lau J. A summary of the agency for healthcare research and quality's evidence report on breastfeeding in developed countries. Breastfeeding Medicine. 2009;4(Supplement 1):S-17–S-30. Available from: http://online.liebertpub.com/doi/pdfplus/10.1089/bfm.2009.0050. [DOI] [PubMed] [Google Scholar]
- 3.Godfrey JR, Lawrence RA. Toward optimal health: The maternal benefits of breastfeeding. Journal of Women's Health. 2010;19(9):1597–602. [DOI] [PubMed] [Google Scholar]
- 4.Schwarz EB, Ray RM, Stuebe AM, Allison MA, Ness RB, Freiberg MS, et al. Duration of lactation and risk factors for maternal cardiovascular disease. Obstetrics and Gynecology. 2009;113(5):974–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics. Policy statement: Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827–41. [DOI] [PubMed] [Google Scholar]
- 6.American College of Obstetricians and Gynecologists. Breastfeeding: Maternal and infant aspects. Obstetrics & Gynecology. 2007;109:479–80. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. The optimal duration of exclusive breastfeeding: Report of an expert consultation. Geneva, Switzerland: World Health Organization; 2001. Report No.: 01.09. [Google Scholar]
- 8.World Health Organization. Exclusive breastfeeding [homepage on the Internet]. 2018. Available from: http://www.who.int/nutrition/topics/exclusive_breastfeeding/en/
- 9.Centers for Disease Control and Prevention (CDC). Healthy people 2020 objectives for the nation [homepage on the Internet]. 2016. Available from: https://www.cdc.gov/breastfeeding/policy/hp2020.htm
- 10.Centers for Disease Control and Prevention (CDC). Breastfeeding report card [homepage on the Internet]. 2016. Available from: https://www.cdc.gov/breastfeeding/pdf/2016breastfeedingreportcard.pdf.
- 11.Joyce T, Reeder J. Changes in breastfeeding among WIC participants following implementation of the new food package. Matern Child Health J. 2015. April;19(4):868–76. [DOI] [PubMed] [Google Scholar]
- 12.Anstey EH, Chen J, Elam-Evans LD, Perrine CG. Racial and geographic differences in breastfeeding - united states, 2011–2015. MMWR Morb Mortal Wkly Rep. 2017. July 14;66(27):723–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henninger ML, Irving SA, Kauffman TL, Kurosky SK, Rompala K, Thompson MG, et al. Predictors of breastfeeding initiation and maintenance in an integrated healthcare setting. J Hum Lact. 2017. May;33(2):256–66. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention (CDC). Rates of any and exclusive breastfeeding by socio-demographics among children born in 2014 [homepage on the Internet]. 2017. Available from: https://www.cdc.gov/breastfeeding/data/nis_data/rates-any-exclusive-bf-socio-dem-2014.htm
- 15.Linares AM, Rayens MK, Dozier A, Wiggins A, Dignan MB. Factors influencing exclusive breastfeeding at 4 months postpartum in a sample of urban hispanic mothers in kentucky. J Hum Lact. 2015. May;31(2):307–14. [DOI] [PubMed] [Google Scholar]
- 16.Brand E, Kothari C, Stark MA. Factors related to breastfeeding discontinuation between hospital discharge and 2 weeks postpartum. J Perinat Educ. 2011. Winter;20(1):36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thulier D, Mercer J. Variables associated with breastfeeding duration. J Obstet Gynecol Neonatal Nurs. 2009. May-Jun;38(3):259–68. [DOI] [PubMed] [Google Scholar]
- 18.Rosen-Carole C, Hartman S, Academy of Breastfeeding Medicine. ABM clinical protocol #19: Breastfeeding promotion in the prenatal setting, revision 2015. Breastfeed Med. 2015. December;10(10):451–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ekstrom A, Widstrom AM, Nissen E. Duration of breastfeeding in swedish primiparous and multiparous women. J Hum Lact. 2003. May;19(2):172–8. [DOI] [PubMed] [Google Scholar]
- 20.Chantry CJ, Dewey KG, Peerson JM, Wagner EA, Nommsen-Rivers LA. In-hospital formula use increases early breastfeeding cessation among first-time mothers intending to exclusively breastfeed. J Pediatr. 2014. June;164(6):1339–45.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howel D, Ball H. Association between length of exclusive breastfeeding and subsequent breastfeeding continuation. J Hum Lact. 2013. November;29(4):579–85. [DOI] [PubMed] [Google Scholar]
- 22.Haggkvist AP, Brantsaeter AL, Grjibovski AM, Helsing E, Meltzer HM, Haugen M. Prevalence of breast-feeding in the norwegian mother and child cohort study and health service-related correlates of cessation of full breast-feeding. Public Health Nutr. 2010. December;13(12):2076–86. [DOI] [PubMed] [Google Scholar]
- 23.Bolton TA, Chow T, Benton PA, Olson BH. Characteristics associated with longer breastfeeding duration: An analysis of a peer counseling support program. J Hum Lact. 2009. February;25(1):18–27. [DOI] [PubMed] [Google Scholar]
- 24.Brownell EA, Hagadorn JI, Lussier MM, Goh G, Thevenet-Morrison KN, Lerer TJ, et al. Optimal periods of exclusive breastfeeding associated with any breastfeeding duration through one year. J Pediatr. 2015. 3;166(3):566–570.e1. [DOI] [PubMed] [Google Scholar]
- 25.Dozier AM, Brownell EA, Guido J, Yang H, Howard CR, Doniger A, et al. Adapting the pregnancy risk assessment monitoring survey to enhance locally available data: Methods. Maternal and Child Health Journal. 2014;18(5):1196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steyerberg EW, Harrell FE Jr, Borsboom GJ, Eijkemans MJ, Vergouwe Y, Habbema JD. Internal validation of predictive models: Efficiency of some procedures for logistic regression analysis. J Clin Epidemiol. 2001. August;54(8):774–81. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention (CDC). Breastfeeding report card 2009 [homepage on the Internet]. 2009. Available from: https://www.cdc.gov/breastfeeding/pdf/2009BreastfeedingReportCard.pdf
- 28.Grummer-Strawn LM, Scanlon KS, Fein SB. Infant feeding and feeding transitions during the first year of life. Pediatrics. 2008. October;122 Suppl 2:S36–42. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention (CDC). Breastfeeding report card 2013 [homepage on the Internet]. 2013. Available from: https://www.cdc.gov/breastfeeding/pdf/2013breastfeedingreportcard.pdf
- 30.Amir LH, Donath S. A systematic review of maternal obesity and breastfeeding intention, initiation and duration. BMC Pregnancy Childbirth. 2007. July 4;7:9,2393–7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li R, Fein SB, Chen J, Grummer-Strawn LM. Why mothers stop breastfeeding: Mothers' self-reported reasons for stopping during the first year. Pediatrics. 2008. October;122 Suppl 2:S69–76. [DOI] [PubMed] [Google Scholar]
- 32.Dewey KG, Nommsen-Rivers LA, Heinig MJ, Cohen RJ. Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss. Pediatrics. 2003. September;112(3 Pt 1):607–19. [DOI] [PubMed] [Google Scholar]
- 33.Everson SA, Maty SC, Lynch JW, Kaplan GA. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity, and diabetes. J Psychosom Res. 2002. October;53(4):891–5. [DOI] [PubMed] [Google Scholar]
- 34.Groenwold RHH, Sterne JAC, Lawlor DA, Moons KGM, Hoes AW, Tilling K. Sensitivity analysis for the effects of multiple unmeasured confounders. Annals of Epidemiology. 2016. September 2016;26(9):605–11. [DOI] [PubMed] [Google Scholar]
- 35.Hill AB. Association or causation? Proc R Soc Med. 1965;58:295–300. [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization. Infant and young child feeding: Model chapter for textbooks for medical students and allied health professionals. Infant and young child feeding: model chapter for textbooks for medical students and allied health professionals. 2009. [PubMed]