Abstract
Objectives:
The present study investigated whether a maladaptive family environment would moderate the strength of the relations of Sluggish Cognitive Tempo (SCT) to attention-deficit/hyperactivity disorder inattention (ADHD-IN) and to depressive symptoms in a large sample of college students.
Method:
Participants (N = 3,172), between the ages of 18 to 29 (M±SDage = 19.24±1.52; 69.8% women; 80.4% White) and enrolled in five universities in the United States completed self-report measures of symptomatology, interparental conflict, and family expressiveness of emotions.
Results:
A negative emotional climate strengthened relations of SCT with ADHD-IN and depressive symptoms. Moreover, the lack of a positive emotional climate strengthened the co-occurrence of SCT with depressive symptoms, though not with ADHD-IN.
Conclusions:
The present study is the first to demonstrate that the family environment moderates the association between SCT and co-occurring symptomatology in young adults.
Keywords: sluggish cognitive tempo, psychopathology, transdiagnostic, family environment
Sluggish cognitive tempo (SCT), characterized by a constellation of symptoms including excessive daydreaming, mind wandering, and slowed thinking/behaviors, is uniquely associated with various forms of psychopathology and considerable functional impairment (Becker et al., 2017). Recently, some have argued for conceptualizing SCT as a meaningful construct that influences the phenomenology of other psychopathologies (Becker et al., 2016). It is likely that SCT symptoms directly influence the severity of commonly co-occurring symptomologies, specifically attention-deficit/hyperactivity disorder inattentive symptoms (ADHD-IN) and depressive symptoms. Moreover, SCT may interact with contextual influences to strengthen the co-occurrence of SCT with these symptom domains. In a large sample of young adults, the current study is the first to examine whether the family environment moderates the relations of SCT to ADHD-IN and to depressive symptoms.
SCT as a Distinct Construct
SCT was initially conceptualized as potentially redundant with symptoms of ADHD-IN, but evidence suggests that SCT symptoms are distinct from ADHD-IN (Barkley, 2014; Becker et al., 2014). The preponderance of SCT research has been conducted in child and adolescent populations and has consistently found support, including meta-analytic evidence, that SCT symptoms are empirically distinct from ADHD-IN (for review, see Becker et al., 2016). Though fewer in number, studies with adults also indicate that SCT is distinct from ADHD-IN symptoms (Barkley, 2012; Becker et al., 2014). SCT symptoms are also strongly related to, yet empirically distinct from, depression in adults (Becker et al., 2017). In fact, some studies find stronger associations between SCT and internalizing symptoms (particularly depression) than between SCT and ADHD-IN (Becker et al., 2014; Kamradt, Momany, & Nikolas, 2017).
As the literature on SCT has advanced, attention has shifted from whether this constellation of symptoms is distinct from ADHD-IN and depression, to a focus on the unique outcomes associated with SCT and how the presence of SCT may influence the presentation and associated impairments among co-occurring symptoms (Becker & Willcutt, 2018). Clearly, SCT is robustly associated with both ADHD-IN and depression (Becker et al., 2016; Becker et al., 2017). SCT, however, is also uniquely associated with academic, social, and emotional adjustment in young adults while controlling for ADHD-IN and depressive symptomatology (Flannery, Luebbe, & Becker, 2016; Jarrett et al., 2017; Wood, Lewandowski, Lovett, & Antshel, 2017). Most importantly, adults with SCT symptoms and clinically elevated ADHD-IN symptoms experience greater impairment compared to those with only ADHD-IN symptomatology (Barkley, 2012). A similar exacerbation might be expected for depressive symptoms as well. In sum, the extant research underscores how SCT symptoms may exacerbate functional outcomes of experiencing ADHD-IN or depressive symptomatology. These studies support previous research demonstrating that the presence of one constellation of symptoms can influence the presentation and severity of other symptom clusters (Connor et al., 2003). However, not all individuals with ADHD-IN or depression show elevated rates of SCT. Because co-occurring SCT may be associated with greater impairment among those with ADHD-IN or depressive symptomatology, it is important to understand under which conditions the co-occurrence of SCT with ADHD-IN and depressive symptoms is particularly strong.
Family Emotional Climate as a Moderator Linking SCT with ADHD-IN and Depression
Previous theoretical work suggests that the environment may influence the presence and magnitude of co-occurring symptoms (Caron & Rutter, 1991). In support of this, the presence of a maladaptive family environment has been found to influence the co-occurrence of ADHD with depressive symptomology (Drabick, Gadow, & Sprafkin, 2006). Potentially, environmental factors may also alter relations of SCT with ADHD-IN and depressive symptomatology (Barkley 2014). Specifically, the emotional climate of the family, characterized by the quality of relationships (e.g., interparental relationship, parent-child relationship) and the emotion expressivity in a family, may function as moderators that strengthen the association of SCT with ADHD-IN and depression.
Negative Emotional Climate and SCT.
A negative emotional climate, as evidenced through frequent interparental conflict and negative emotional expressivity, is indirectly linked with ADHD-IN symptoms. Research demonstrates that frequent conflict disrupts family cohesion and undermines the parent-child relationship (Krishnakumar & Buehler, 2000), and disruptions in family cohesion have been specifically related to more severe presentations of ADHD-IN symptoms (Cussen et al., 2012; Pheula, Rohde, & Schmitz, 2011). A negative emotional climate may also strengthen the relation between SCT and ADHD-IN. Indeed, according to a developmental psychopathological framework of ADHD, the family environment functions as a risk or protective factor by interacting with child predispositions to exacerbate or reduce the co-occurrence of ADHD with related conditions (Johnstone & Mash, 2001). Because a negative emotional climate may lack structure and organization, thereby hindering cognitive control and on-task behavior (Ellis & Nigg, 2009), individual tendencies towards daydreaming and mind-wandering (e.g., SCT symptoms) may exacerbate inattentive symptoms. On the other hand, a family environment with fewer negative exchanges may facilitate appropriate self-regulation, which may reduce the co-occurrence of SCT with ADHD-IN.
A negative emotional climate also strongly relates to depressive symptomatology in young adults (Cusimano & Riggs, 2013; Schiff et al., 2014). Frequent exposure to conflict and negative emotional expressiveness throughout childhood and adolescence likely elevates experiences of negative affect, resulting in heightened depressive symptoms in young adulthood (Schwartz et al., 2012). Moreover, young adults raised in these environments are likely to exhibit disrupted social interaction patterns, such as social isolation and withdrawal, which have been prospectively linked to depression (Katz et al., 2011). Because SCT is uniquely associated with dysfunctional social behaviors (Rondon, Hilton, Jarrett, & Ollendick, 2018; Willcutt et al., 2014), relations with depression may be strengthened in a negative emotional environment that models ineffective interpersonal relations. On the other hand, an environment that models conflict resolution and appropriate social interactions may buffer against individual tendencies toward isolation and withdrawal, likely reducing associations with depression.
Positive Emotional Family Climate and SCT.
A positive emotional climate, indicated through frequent verbal and non-verbal expressions of positive affect (PA), does not represent the opposite end of the same continuum with the negative emotional climate (Luebbe & Bell, 2014). Low PA is a feature unique to adolescents’ and young adults’ depressive symptoms that separates depression from highly comorbid disorders (Luebbe & Bell, 2014; Moffit et al., 2007; Schwartz et al., 2012). The relation between SCT and depressive symptoms may be strengthened in an environment with infrequent modeling and reinforcement of PA. Researchers contend that SCT and depression may have shared core aspects such as underactivity and drowsiness that may explain the substantial overlap between these symptom domains (Becker, Luebbe, et al., 2014; Kamradt; Momany, & Nikolas, 2017). Therefore, an individual’s tendency towards these behaviors may exacerbate depressive symptomatology in an environment that does not specifically socialize and encourage PA.
It is possible that the lack of a positive environment would strengthen relations of SCT with ADHD-IN symptom. Positive parenting behaviors, such as parental involvement and sensitivity, are associated with less severe inattentive symptomatology for those with ADHD (Ellis & Nigg, 2009; Keown, 2012). However, these studies included younger children, and there are notably fewer studies to propose specific hypotheses regarding associations between inattentive symptoms and a positive environmental climate compared to a negative climate. Further, the lack of a negative climate does not merely represent the presence of a positive emotional climate (Luebbe & Bell, 2014). Given the current state of the literature, we do not make specific claims regarding whether the lack of a positive climate strengthens relations of SCT with ADHD-IN symptoms.
Present Study
The present study utilized a large sample of young adults to test whether the emotional climate of the family would strengthen relations of SCT to ADHD-IN and to depressive symptoms. Examining a young adult sample is important, given heightened rates of SCT in college students (Flannery et al., 2016; Wood et al., 2014). First, we tested whether a negative family emotional climate moderated the associations of SCT to ADHD-IN and to depressive symptoms. It was anticipated that the strength of the co-occurrence between SCT and these related conditions would increase in the presence of an aversive environment. Second, we assessed whether the lack of a positive emotional climate would moderate the associations of SCT with ADHD-IN and of SCT with depression. We hypothesized that the lack of a positive emotional climate would strengthen the relation between SCT and depression, though we did not anticipate positive emotional climate to moderate the relation between SCT and ADHD-IN.
Methods
Participants
Participants included 3,172 undergraduate students enrolled in five universities in the United States. The universities (four of the five were public) are located in the Midwestern, Southeastern and Pacific Northwestern areas of the United States. Participants ranged in age from 18 to 29 years (Mage = 19.24, SD = 1.52, 69.8% female). The majority of participants identified as White (80.4%), while the remaining individuals identified as Asian/Asian American (6.4%), Black/African American (6.3%), Biracial/Multiracial (5.6%), Native Hawaiian/Other Pacific Islander (0.7%), and American Indian/Alaska Native (0.6%). Approximately seven percent of the participants identified as Hispanic or Latino. More than half of participants (59.5%) were in their freshman year of college, while the remaining were in their second (20.4%), third (12.1%), fourth (7.5%), and other (0.4%) year of college. The majority of participants reported that their parents were still married (68.9%), while 23.6% indicated that their parents were separated/divorced. Participants self-reported lifetime diagnoses of an anxiety disorder (12.6%, n = 401), depressive disorder (12.3%, n = 390), ADD/ADHD (9.4%, n = 298), a learning disorder (2.5%, n = 78), bipolar disorder (0.8%, n = 25), and an alcohol abuse/disorder (0.3%, n = 9).
Procedure
The present study was approved by the Institutional Review Board at each of the five universities. At four of the sites, participants provided consent and completed the survey anonymously entirely online using the Qualtrics platform. At the fifth university, participants selected individual time-slots to complete the consent form in-person and then completed the survey online on their own time. All participants were provided contact information of the primary investigator and student counseling center associated with each university. Participants received course credit for completion of the study, which on average lasted an hour.
Measures
SCT symptoms.
SCT symptoms were assessed with the recently validated 10-item Adult Concentration Inventory (ACI; Becker et al., 2017) developed following a meta-analysis that identified a constellation of SCT symptoms that were distinct from ADHD-IN (Becker et al., 2016). Factor analyses resulted in 10 SCT items that represented convergent and discriminative validity from internalizing symptoms and ADHD-IN symptoms (Becker et al., 2017). Participants responded to each item on a four-point scale (0 = not at all, 3 = very often) in regards to the past six months. Sample items include, “I stare off into space” and “I get tired easy.” In the present study, internal consistency was .89.
ADHD symptoms.
The Barkley Adult ADHD Rating Scale- IV (BAARS-IV; Barkley, 2011a) was used to evaluate ADHD symptoms. The 18 items correspond with recent changes to ADHD reflected in the DSM – 5 (American Psychiatric Association, 2013). Participants reported on each item on a four-point scale (0 = not at all, 3 = very often), in regards to how each statement describes their behavior during the past six months. Sample items on the ADHD-IN scale include “Fail to give attention to details” and “difficulty sustaining my attention in tasks or fun activities,” and on the ADHD hyperactivity-impulsivity (HI) include “fidget with hands or feet” and “talk excessively.” The BAARS-IV has demonstrated validity in adult samples with ADHD and has satisfactory test-retest reliability (Barkley, 2011a). In the present study, internal consistency for ADHD-IN (α = .89) and ADHD-hyperactivity-impulsivity (ADHD-HI; (α = .83) were acceptable.
Depressive symptoms.
The depression subscale of the Depression Anxiety Stress Scale-21 (DASS; Antony, Bieling, Cox, Enns, Swinson, 1998; Lovibond & Lovibond, 1995) assessed depressive symptomatology. This subscale entails seven items that assesses low self-esteem, sadness, low PA, and inability to experience pleasure, with higher scores representing greater symptomatology. Participants respond to each item in regards to the previous week on a four-point scale (0 = did not apply to me at all, 3 = applied to me very much or most of the time). The DASS-21 has shown good reliability estimates in clinical and nonclinical populations (Antony et al., 1998). In the present study, internal consistency was good (α = .89).
Interparental Conflict.
Perceptions of interparental conflict were assessed using the Children’s Perception of Interparental Conflict Scale (CPIC; Grych, Seid, & Fincham, 1992). The scale was adapted for young adult participants to retrospectively report on their perceptions of interparental conflict during childhood and adolescence. Initially a 48-item scale with nine subscales, only four subscales (frequency, intensity, resolution, and perceived threat; 26 items) were administered in the current sample to reduce participant burden. For analyses, however, the perceived threat subscale was omitted given that past research indicates this subscale functions differently than the other three that load together on single factor, labeled interparental conflict, in past factor analytic work (Bickham & Fiese, 1997; Grych et al., 1992;). Participants were asked to answer whether each item is “True,” “Sort of True,” or “False” regarding their experiences of the frequency (6 items; “I often saw or heard my parents arguing”), intensity (7 items; “My parents got really mad when they argued”), and resolution (6 items; “When my parents argued they usually made it up right away”) of interparental conflict. Items were re-coded when necessary to reflect a higher level of conflict, including complete reversal of the resolution subscale. Previous research has utilized retrospective accounts of these subscales, with acceptable internal consistency and reliability in young adult samples (Bickham & Fiese, 1997; Rodrigues & Kitzman, 2007). Internal consistency in the present study for frequency (α = .86), intensity (α = .87), and resolution (α = .90) was acceptable.
Family Emotion Expressiveness.
The Family Expressiveness Questionnaire-Short Form (FEQ; Halberstadt, Cassidy, Stifter, Parke, & Fox, 1995) is a 24-item retrospective measure that assesses the frequency of emotions expressed in the family and has been used with young adults (Kring & Gordon, 1998). Participants indicated on a 1 (not at all frequently) to 9 (very frequently) scale the frequency of a given item occurring in the family. The FEQ-S contains two subscales; negative family expressiveness (12 items; e.g., “Expressing dissatisfaction with someone else’s behavior” and “Showing dislike for someone”) and positive family expressiveness (12 items; e.g., “Praising someone for good work” and “Telling family members how happy you are”), that were included in the present study. The FEQ-Short Form has demonstrated acceptable internal consistency (Halberstadt et al., 1995). In the present study, internal consistency for the negative family expressiveness subscale (α = .90) and positive family expressiveness subscale (α = .94) were acceptable.
Analytic Approach
Data Quality Check.
To ensure quality responses, we applied an instructional manipulation check (IMC; Oppenheimer, Meyvis, & Davidenko, 2009), trap questions (e.g., “If you are paying attention, please click on the response ‘sometimes’), and a question at the conclusion of the battery to measure participants’ effort during the study. The IMC instructed the participant to select a specific answer, which they were required to answer correctly in order to proceed with the survey. We designated a threshold of 50% accuracy or higher for the trap questions and an effort rating of 5 or higher on a 0 to 10 scale (0 = not much effort, 10 = my best effort). Overall, 3,172 of the original 3,307 participants (95.9%) met the criteria for both the trap questions and self-reported effort.1
Structure of Family Climate.
Before testing primary hypotheses, confirmatory factor analyses were conducted in Mplus 7.0 (Muthen & Muthen, 1996–2014) to test how family climate should be best empirically modeled. Four competing models were tested, and all models were estimated using robust maximum likelihood estimation. The first model assumed that all indicators of family climate (i.e., the three subscales of the CPIC, the negative and positive subscales of the FEQ) loaded on a single factor (Model 1). The second model specified separate, but correlated, emotional climate factors differentiated by valences. Specifically, the two factors were: (1) a negative emotional climate factor composed of the intensity, frequency, and resolution (reverse-scored) subscales of the CPIC and the negative expressiveness subscale of the FEQ, and (2) a positive emotion climate factor composed of the positive expressiveness subscale of the FEQ modeled as three randomly generated parcels to improve factor stability (Little et al., 2002; Model 2). Given the potential that resolution of interparental conflict may operate uniquely, and more positively, for youth adjustment compared to intensity and frequency of conflict (McCoy, Cummings, & Davies, 2009), a third model was tested that was similar to Model 2 with the exception that the resolution subscale of the CPIC was placed on the positive emotion climate factor rather than the negative emotion climate factor (Model 3). Finally, a fourth model was tested that modeled unique subsystems in the family. Specifically, one factor was composed of the items from the CPIC purportedly assessing the marital subsystem, and a second factor was composed of the subscales of the FEQ purportedly assessing the larger family system.
Although Model 2, 3, and 4 are nested versions of Model 1, given that the former three models are non-nested, model comparison was based on considering fit indices and information criterion values across models. Across all indices, Model 2 with the separate positive and negative emotion climate factors (with resolution loading on negative) best fit the data (see Table 2), with all relative fit indices suggesting excellent fit (Hu & Bentler, 1999). This model was used for primary analyses.
Table 2.
Comparison of Model Fit for Family Emotional Climate
| MODEL | χ2 (df) | RMSEA (90% CI) |
CFI | TLI | SRMR | AIC | BIC |
|---|---|---|---|---|---|---|---|
| 1. One Factor | 7842.94(14)** | .42 (.41, .43) | .39 | .08 | .24 | 59887.47 | 59948.01 |
|
2. Two Factor: Neg. / Pos. Climate |
57.33 (13)** | .03 (.02, .04) | .99 | .99 | .01 | 50353.91 | 50417.34 |
| 3. Two Factor – Neg. / Pos. with Res. |
1811.09(13)** | .21(.20, .22) | .86 | .77 | .16 | 52362.02 | 52425.49 |
| 4. Two-Factor – Subsystems |
473.61 (13)** | .11 (.10, .11) | .96 | .94 | .10 | 50808.66 | 50872.08 |
Note. Neg. = Negative. Pos. = Positive. Res. = Resolution. The bolded row indicates the model retained for primary analyses given the indices of model fit.
p < .05.
p < .01.
Primary Analyses.
To test if family climate moderated the relation of SCT to ADHD- IN and depression, respectively, structural equation modeling in Mplus 7.0 was used. Specifically, models tested whether the interaction between manifest SCT scores and separate latent negative family climate and positive family climate scores predicted the outcome of interest. All models controlled for other forms of symptomatology. For example, in models where depressive symptoms were the outcome of interest, models controlled for ADHD-IN and ADHD-HI (and vice versa in models where ADHD-IN was the dependent variable). Given that the interactions in question were continuous manifest variable by continuous latent variable interactions, the XWITH command was used in Mplus. This command uses a quasi-maximum likelihood method to estimate interactions (Klein & Muthen, 2007) based on a latent moderated structural equation method (Klein & Moosbrugger, 2000). This approach is desirable in that it does not require separate manifest indicators to model interactions as do other methods for estimating interactions that involve latent variables (e.g., Kenny & Judd, 1984). Models were estimated using maximum likelihood with robust standard errors and numerical integration. Missing data were estimated using full-information maximum likelihood. To account for potential effects due to the site of data collection, a set of four dummy codes indicating site were included as covariates.
Results
Table 1 shows correlations among all study measures. No significant relations emerged between outcomes of interest (i.e., ADHD inattention symptoms, depression symptoms) and demographic variables such as age, gender, ethnic/racial identity (dummy-coded as White vs. ethnic/racial minority), or time since separation for those whose parents were divorced/separated. There was a very small (r = .04, p = .048), albeit significant, relation between depression and living in a one- versus two-parent home growing up, such that participants living in a one-parent home reported higher depressive symptoms compared to those living in a two-parent home. Models (described below) were calculated with and without this variable as a covariate. Effects were identical. As such, no demographic covariates were considered further in analyses.
Table 1.
Interrcorrelations among Demographics, Family Emotional Climate, and Psychopathology Symptoms
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | -- | ||||||||||||||||
| 2. Sex | −.09** | -- | |||||||||||||||
| 3. Race | .06** | −.01 | -- | ||||||||||||||
| 4. Bio/Non-Bio | −.04** | −.08** | −.01 | -- | |||||||||||||
| 5. Time Since | .15** | −.03 | .05 | .01 | -- | ||||||||||||
| 6. Pos. Exp. | −.06** | .20** | −.01 | .05** | −.06 | -- | |||||||||||
| 7. Pos. 1 | −.06** | .21** | −.01 | .05** | −.05 | .95** | -- | ||||||||||
| 8. Pos. 2 | −.07** | .21** | −.01 | .05** | −.06 | .96** | .88** | -- | |||||||||
| 9. Pos. 3 | −.05** | .16** | −.00 | .05** | −.06 | .96** | .87** | .89** | -- | ||||||||
| 10. Neg. Exp. | −.02 | .09** | −.01 | −.09** | .03 | −.11** | −.11** | −.07** | −.13** | -- | |||||||
| 11. Freq. | .04* | .09** | .02 | −.30** | −.11** | −.21** | −.21** | −.20** | −.21** | .37** | -- | ||||||
| 12. Int. | .04* | .07** | .01 | −.27** | .01 | −.19** | −.18** | −.17** | −.19** | .36** | .83** | -- | |||||
| 13. Res. | .06* | .07** | .01 | −.40** | −.05 | −.26** | −.25** | −.24** | −.26** | .34** | .79** | .74** | -- | ||||
| 14. Hyp/Imp | −.02 | .02 | −.03 | −.03 | −.00 | −.03 | −.04* | −.03 | −.02 | .25** | .15** | .13** | .10** | -- | |||
| 15. SCT | −.06** | .16** | −.02 | −.02 | .00 | −.06** | −.06** | −.05** | −.05** | .27** | .15** | .13** | .12** | .49** | -- | ||
| 16. Inattention | .00 | .01 | −.03 | −.02 | .01 | −.13** | −.14** | −.12** | −.12** | .30** | .18** | .17** | .16** | .61** | .65** | -- | |
| 17. Dep. | −.00 | .03 | −.02 | −.04* | −.01 | −.17** | −.18** | −.15** | −.15** | .29** | .18** | .15** | .17** | .35** | .49** | .53** | -- |
Note. For Sex, male = 0, female = 1. For Race, non-white = 0, white = 1. Bio/Non-Bio = two parent or one parent family of origin. For Bio/Non-Bio, 0 = one biological parent, 1 = both biological parent. Time Since = Time since parent separation, n = 786. Pos Exp. = Family Expressiveness of Positive Emotions. Pos. 1, 2, & 3 = Parcels for Family Expressiveness of Positive Emotions. Neg Exp. = Family Expressiveness of Negative Emotions. Freq. = Children’s Perception of Interparental Conflict (CPIC) Frequency Subscale. Int. = CPIC Intensity Subscale. Res. = CPIC Resolution Subscale Reverse Scored. Hyp/Imp. = ADHD Hyperactivity/Impulsivity. SCT = Sluggish Cognitive Tempo. Inattention = ADHD Inattentive. Dep. = Depression.
p < .05,
p < .01.
ADHD-IN Symptoms.
As a first step, we estimated a structural regression model that regressed ADHD-IN symptoms on the main effects of separate positive and negative family emotional climate factors (modeled as latent variables), SCT symptoms, and the two interaction terms (i.e., positive family climate by SCT; negative family climate by SCT). This model also included the covariates of ADHD-HI symptoms and depressive symptoms as well as the dummy codes for site. In this model, there was a marginally significant two-way interaction between negative family climate and SCT predicting ADHD-IN symptoms (b = .03, SE = .01, t = 1.90, p = .057). The interaction between positive family climate and SCT was non-significant. Given the non-significant interaction between positive family climate and SCT, we dropped this variable from the model and re-ran the analysis. In this new model, the path between the negative family climate by SCT interaction and ADHD-IN symptoms was significantly different than zero (b = .03, SE = .01, t = 2.27, p = .03). Notably, comparing this model to a model without the interaction indicated that the isolated effect size of the interaction was very small, accounting for just under 1% of variance in ADHD-IN symptoms. All other paths can be found in Figure 1.
Figure 1.
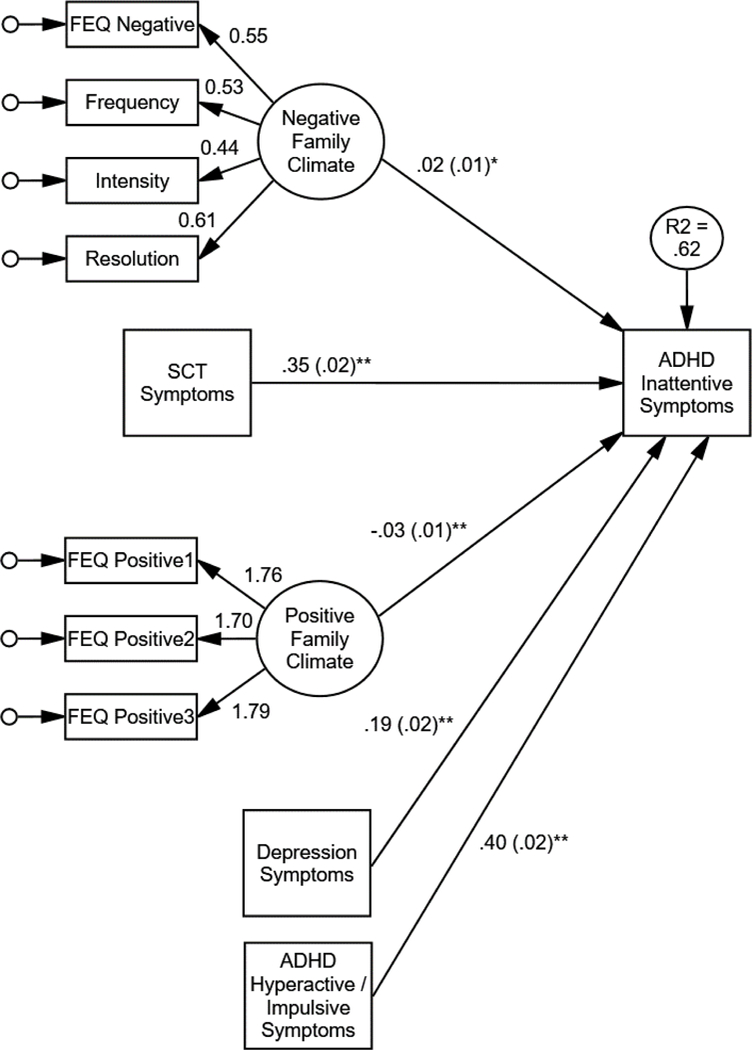
Structural equation model showing interactions of family negative emotional climate and of positive emotional climate with sluggish cognitive tempo (SCT) symptoms predicting ADHD-Inattentive symptoms. Unstandardized betas shown. The interaction of negative emotional climate with SCT predicting ADHD-Inattentive symptoms was marginal (p = .057). For ease, dummy codes representing site of data collection, covariances among independent variables, and residual variances of factor indicators not shown. FEQ = Family expressiveness questionnaire. * p < .05, ** p < .01.
To probe the interaction, we used the model constraint option in Mplus to test the slope of the relation between SCT and ADHD-IN at values of −1 SD, the mean, and +1 SD of the latent construct of negative family climate. All other continuous variables in the model were centered, so simple slopes represent effects at the mean of all covariates in the model (and 0 values on the dummy-coded site variables). Although significant at all three levels, the relation became increasingly stronger between SCT and ADHD-IN symptoms as family climate became more negative (see Figure 2). Thus, regardless of the environment, SCT symptoms and ADHD-IN are correlated. But, SCT symptoms and ADHD-IN symptoms more strongly co-occur in the presence of a negative family climate.
Figure 2.
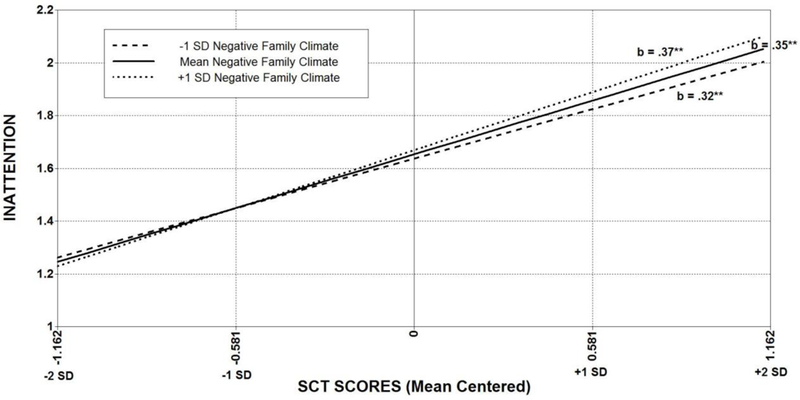
Interactions of family negative emotional climate with sluggish cognitive tempo (SCT) symptoms predicting ADHD-Inattentive symptoms. Unstandardized betas shown. Values are plotted at the mean of other covariates in the model. * p < .05, ** p < .01.
Depressive Symptoms.
Following the same modeling process as above, we next estimated a structural regression model that regressed depressive symptoms on the main effects of separate positive and negative family emotional climate factors (modeled as latent variables), SCT symptoms, and the two interaction terms (i.e., positive family climate by SCT; negative family climate by SCT), over and above the effects of ADHD-IN and ADHD-HI symptoms, and the dummy codes for site. In this model, there was a marginally significant two-way interaction between negative family climate and SCT predicting depressive symptoms (b = .04, SE = .02, t = 1.86, p = .063). In contrast, there was a significant interaction between positive family climate and SCT (b = −.06, SE = .02, t = −3.02, p = .003). Again, comparing this model to a model without the interactions indicated that the isolated effect size of the interactions (combined) was small, accounting for 1% of variance in depression symptoms. All other paths can be found in Figure 3.
Figure 3.
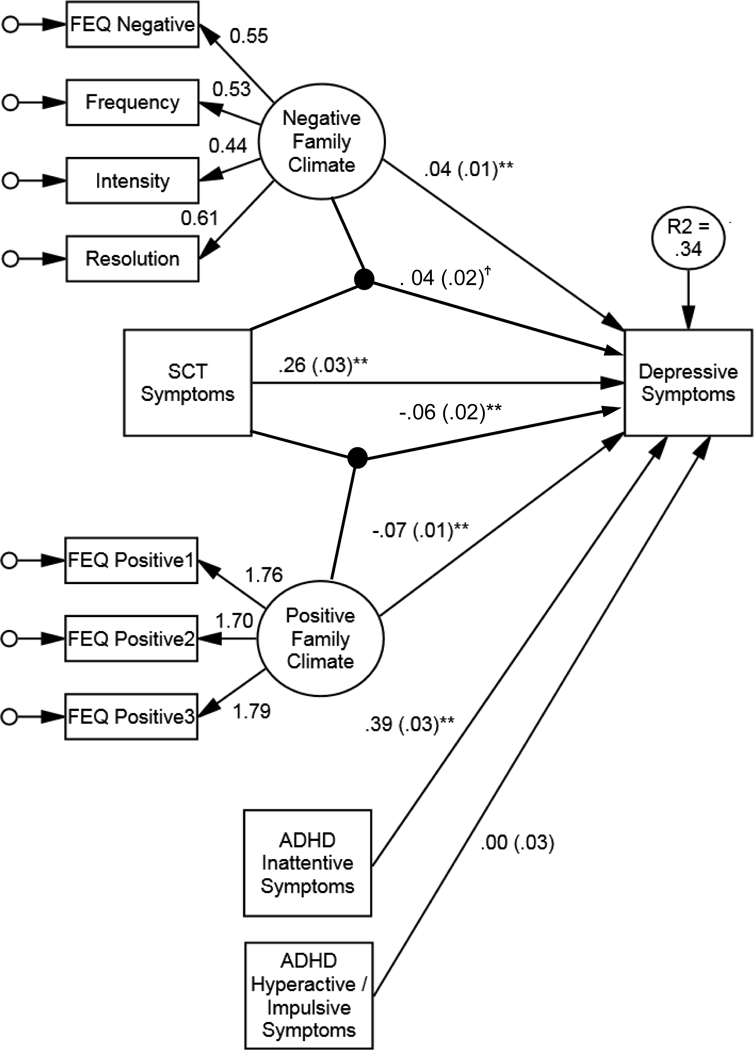
Structural equation model showing interactions of family negative emotional climate and of positive emotional climate with sluggish cognitive tempo (SCT) symptoms predicting depression symptoms. Unstandardized betas shown. For ease, dummy codes representing site of data collection, covariances among independent variables, and residual variances of factor indicators not shown. FEQ = Family expressiveness questionnaire. * p < .05, ** p < .01.
Although marginal, we opted to probe the interaction for family negative emotional climate in addition to the significant interaction for positive family emotional climate. Again, we probed the relation between SCT and depressive symptoms at values of −1 SD, the mean, and +1 SD of the latent construct of interest. Relations were significant at all values. All other continuous variables in the model were centered, so simple slopes represent effects at the mean of all covariates in the model (and 0 values on the dummy-coded site variables). For negative family climate, the relation became increasingly stronger between SCT and depressive symptoms as family climate became more negative (see Figure 4 top panel). Thus, SCT symptoms and depressive symptoms appear to more strongly co-occur in the presence of a negative family climate. For positive family climate, the relation became increasingly weaker between SCT and depressive symptoms as family climate became more positive. In other words, the strength of the co-occurrence between SCT and depressive intensified as the family climate became less positive (see Figure 4 bottom panel).
Figure 4.
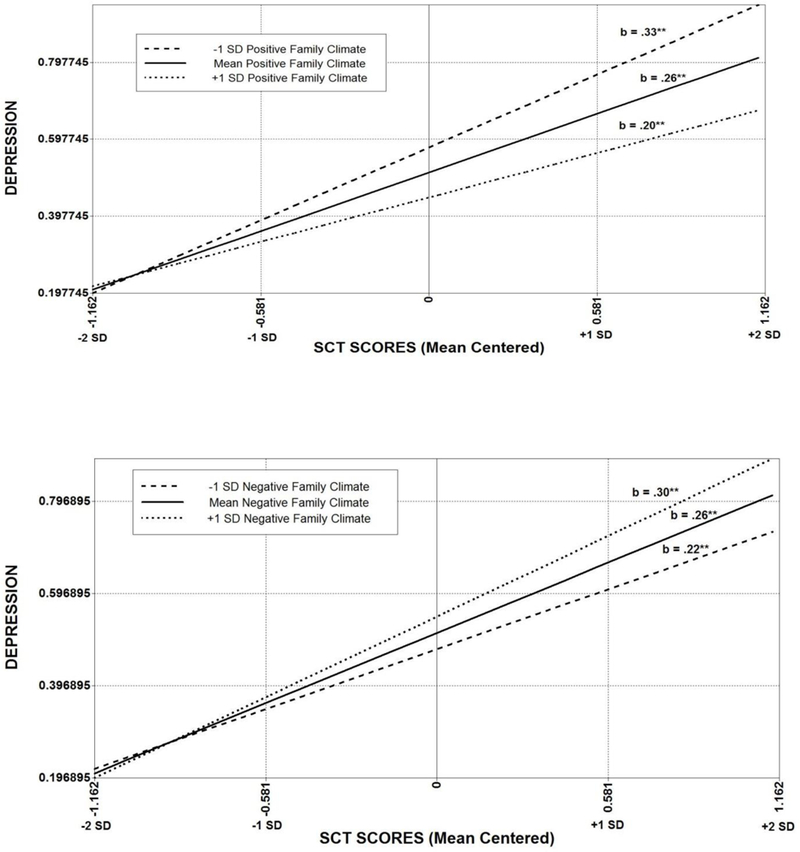
Interactions of family positive emotional climate (top panel) and of negative emotional climate (bottom panel) with sluggish cognitive tempo (SCT) symptoms predicting depression symptoms. Unstandardized betas shown. Values are plotted at the mean of other covariates in the model. Note. * p < .05, ** p < .01.
Discussion
Previous research suggests that SCT may influence the presentation and associated impairments among commonly co-occurring syndromes (Becker & Willcutt, 2018). The present study extends the literature on SCT by investigating under which conditions the co-occurrence of SCT with ADHD-IN and with depressive symptoms is strengthened. Findings demonstrated that the family emotional climate strengthened the relation between SCT and ADHD-IN and depressive symptomatology. Specifically, a negative emotional climate, as measured by interparental conflict and negative family emotional expressiveness, strengthened relations of SCT with ADHD-IN and depressive symptomatology. On the other hand, the lack of a positive emotional environment, as measured by positive emotional expressiveness, strengthened the co-occurrence of SCT with depressive symptoms, but not with ADHD-IN. This pattern of findings is consistent with models of co-occurrence that posit that environmental factors strengthen relations among symptomatologies (Caron & Rutter, 1991).
Negative Family Environment Moderates the Relation between SCT with ADHD-IN and Depressive Symptoms
In support of our hypotheses, current findings using structural equation modeling demonstrated that a negative family emotional climate strengthened the relation between SCT with ADHD-IN symptoms in young adults. We note that this was a small effect, potentially given the strong main effect of a large relation between SCT and ADHD-IN. Despite a multitude of studies identifying relations between the emotional climate of the family and youth symptomatology (Cusimano & Riggs, 2013), no study has examined these processes in relation to SCT. Still, our findings are in line with some previous work regarding ADHD-IN symptomatology, demonstrating that a family environment characterized by frequent conflict and a lack of cohesiveness is associated with more severe presentations of inattentive symptoms (e.g., Krishnakumar & Buehler, 2000; Pheula et al., 2011). It is possible that inconsistency and lack of structure in the environment strengthened the relation between SCT with ADHD-IN. For instance, inattentive symptoms are associated with deficits in self-regulation (cognitive control) that are malleable to a structured environment (Ellis & Nigg, 2009). An individual’s tendency toward mind-wandering and daydreaming (poor cognitive control associated with SCT), may be strongly linked with inattentive symptoms in an environment during childhood and adolescence that does not provide appropriate structure. On the other hand, an environment with healthy interpersonal relations is likely able to exert energy on fostering structure and self-regulatory abilities, which may protect against the worsening of inattentive symptoms in an individual prone to SCT-related behaviors.
Findings also showed that a negative emotional climate heightened the co-occurrence of SCT and depressive symptoms in young adults. This finding is in accordance with previous research demonstrating associations between exposure to interparental conflict and negative family expressiveness with depressive symptoms (e.g., Schiff et al., 2014; Stocker et al., 2007; Turner & Kopiec, 2006). It is possible that exposure to a negative emotional climate strengthens relations between SCT and depressive symptoms through modeling ineffective social interaction patterns. Previous research indicates that SCT is uniquely associated with social isolation/withdrawal behaviors while controlling for ADHD and/or depressive symptoms (Becker, Garner, Tamm, Antonini, & Epstein, 2017; Rondon et al., 2018; Willcutt et al., 2014), potentially as a result of challenges processing social cues and information. Young adults who were exposed to frequent negative emotional expressiveness and interparental conflict are more likely to experience loneliness and social isolation (Johnson, Lavoie, & Malhoney, 2001), and these behaviors are linked to depressive symptoms (Katz et al., 2011). Therefore, an environment that does not model appropriate social interactions likely heightens relations between tendencies towards daydreaming/absent-mindedness and depressive symptomatology.
Lack of Positive Family Environment Strengthens the Co-Occurrence of SCT with Depression but not with ADHD-IN
Previous work underscores that family negative and positive emotional climates are not merely opposite ends of the same continuum (Luebbe & Bell, 2014). Empirically, our structural equation modeling data suggested a similar distinction as a two-factor model of family climate (i.e., positive and negative) emerged. Because previous research shows that a positive climate may differentially influence depressive symptoms compared to other types of internalizing symptoms (Schwartz et al., 2012), we hypothesized that the lack of a positive emotional climate would heighten the relation between SCT and depressive symptoms. As expected, findings showed that the lack of frequent positive emotional expressiveness during childhood and adolescence strengthened the co-occurrence of SCT and depressive symptoms in young adults (albeit a small effect).
Though limited, research demonstrates that infrequent positive expressiveness and reduced positive parenting behaviors are associated with the development of depressive symptoms (Schwartz et al., 2012), potentially by specifically targeting youth’s experience of PA (Luebbe & Bell, 2014). In the present study, the lack of a positive emotional climate exclusively heightened the relation between SCT and depression, potentially through the lack of PA socialization. Previous research suggests that SCT underactive behaviors (e.g., drowsiness, sluggishness) are likely implicated in the development of depression (Becker et al., 2014). Although no study to our knowledge has tested whether these specific symptoms of SCT are associated with PA deficits, it is possible that these characteristics strengthen relations with depressive symptoms in an environment that does not provide sufficient rewarding opportunities and experiences. Conversely, an environment that provides frequent verbal and non-verbal PA (e.g., praising one another, encouraging positive conversations) likely protects individual predispositions toward underactive behaviors from experiencing even more depressive symptomatology. In other words, this environment may serve a form of behavioral activation for individuals with SCT prone to depressive symptoms through specifically modeling and reinforcing rewarding activities in the environment.
Finally, findings showed that a positive emotional climate did not moderate the relation between SCT and ADHD-IN symptoms. That is, the relation of SCT to ADHD-IN seems to be robust even in the presence of putative contextual factors that might alter these relations. If a positive climate uniquely effects PA regulatory systems as we surmise above, perhaps it is then unsurprising that the co-occurrence between SCT and ADHD-IN is not impacted by the positive emotional climate given that these two symptomatologies are more likely to share cognitive deficits (e.g., attentional control issues) than deficits in PA-related domains. Indeed, previous research contends that a positive climate relates to symptomology through specifically targeting positive affective processes (Luebbe & Bell, 2014), and that SCT and depression may share features of underactivity (Becker et al., 2014). Therefore, the lack of a positive emotional climate may not alter relations between SCT and ADHD-IN given the absence of behaviors characterized by disrupted positive affect in the latter, such as underactivity. Taken together, findings provide further evidence of the unique relation between a positive family climate and depressive symptomatology compared to other types of symptoms (Luebbe & Bell, 2014).
Although speculative, our findings may support previous suggestions of conceptualizing SCT as a meaningful transdiagnostic construct (Becker & Willcutt, 2018). Updated transdiagnostic models (Nolen-Hoeksema & Watkins, 2011) outline processes in which proximal factors influence psychological disorders. Proximal factors are characterized by intrapersonal mechanisms that are closely linked to psychopathologies and directly influence these conditions. According to Nolen-Hoesksema and Watkins (2011), proximal risk factors can be either “risk factors that (a) directly precede symptoms (relative to distal risk factors), and/or (b) directly influence symptoms” (p. 594). In this model, moderators determine which particular symptoms or psychopathologies a particular proximal factor will influence. If one considers SCT as fulfilling criterion “b” above, in our study it is possible that SCT functioned as a transdiagnostic construct in which relations with symptomatology were strengthened in the presence of a maladaptive family environment. On the other hand, it is equally possible that SCT merely functioned as a constellation of symptoms that correlated more highly with other symptoms in the presence of certain family environments. Our cross-sectional design limits our ability to fully answer these questions, in addition to whether SCT directly precedes symptoms, but does raise important questions about how SCT functions in conjunction with not only other syndromes, but also the environmental context. An imperative next step to advance SCT research is prospective designs that permit testing under which conditions SCT prospectively influences the developmental course of co-occurring symptomatologies.
Limitations and Future Directions
Despite the strengths of the present study, several limitations warrant further discussion. First, we reiterate that the cross-sectional nature of the data limits inferences regarding causality and prevents establishing the predictive validity of the interaction between SCT and the family environment in relation to related psychopathologies. For instance, although our findings showed that SCT symptoms exacerbated the presentation of symptomology under certain environmental contexts, our findings cannot allude to important questions regarding temporality. It is possible that the presence of SCT and co-occurring symptomatology influenced the family environment. Future research is therefore needed to understand whether the family environment influences the prospective association between SCT, ADHD-IN, and depression. This may also provide further research on whether SCT symptoms directly precede other psychopathology symptoms, or worsen the presentation of certain existing conditions.
The present study also relied on self-report measures which may have inflated relations among symptomatology and the family environment. Although research on SCT and self-reporting bias of symptoms is nonexistent, research has shown that college students may overreport ADHD symptoms to obtain secondary educational gains (Sollman, Reanseen, & Berry, 2010). Moreover, college students’ retrospective accounts of family functioning may be influenced by current psychological functioning (Turner & Kopiec, 2006), and there may be differences in college students’ reporting based on whether students still live at home or how long students have lived away from home. An important area of future research is to incorporate multimethod, multi-informant reports to augment confidence in our understanding of family functioning in relation to symptomatology.
Third, although the present study utilized a large sample size recruited across five universities, the sample consisted of primarily college-age youth, females, and European American/White individuals. Therefore, generalizing findings across all young adults is not supported. Including a sample of college students was important given evidence that SCT symptoms are higher in college students compared to the general population (Jarrett et al., 2017; Wood et al., 2017). Future research should examine these research questions using samples of young adults of different ages (e.g., mid to late twenties) and of varying ethnic/racial backgrounds to better understand whether these relations differ across this developmental period and/or across different cultures or contexts.
Findings showed that family emotional expressiveness and interparental conflict encompass a subset of environmental conditions that may strengthen comorbidities. Future research should include other aspects of the family environment (e.g., parenting behaviors, maternal warmth, psychological control) to understand which specific factors of the family emotional climate particularly impact SCT symptoms. Further, given not only small effects, but also the non-significant moderation for positive emotional climate on the association of SCT to ADHD-IN, several other non-familial (e.g., peers relationships) or non-environmental factors (e.g., biology) might be considered in future research examining potential moderating influences on the relations of SCT with ADHD-IN and depression. Finally, we assumed that stronger associations of SCT with depression and ADHD-IN would worsen impairment given preliminary research showing that adults with ADHD combined with SCT symptoms have more impairment compared to adults with fewer SCT symptoms (Kamradt, Momany, & Nikolas, 2017). Although beyond the scope of the present paper, testing the three-way interaction of family environment, SCT, and co-occurring symptomatology as predictors of specific domains of functional impairment would be a needed and exciting next step.
Conclusion
Our findings are the first to empirically demonstrate that environmental conditions moderate the co-occurrence of SCT symptoms with ADHD-IN and depression. Specifically, findings showed that a negative emotional climate (interparental conflict and negative family expressiveness) strengthened the co-occurrence of SCT with ADHD-IN and SCT with depression in young adults. Findings also showed that the absence of a positive emotional climate (positive family expressiveness) heightened the overlap of SCT and depressive symptoms, though not with ADHD-IN. In sum, the present study is particularly informative given research demonstrating that the co-occurrence of symptomologies worsens functional impairment (Drabick, Gadow, & Sprafkin, 2006). Although these results cannot support SCT as prospectively increasing risk for ADHD-IN and depressive symptomatology, the family environment is clearly a contextual factor influencing the co-occurrence of these symptom domains. Future research examining the family environment in relation to SCT may contribute to potential prevention and intervention treatments to minimize the negative impact of these symptomologies (Becker et al., 2016).
Acknowledgments
Funding information: National Institute of Mental Health (NIMH), Grant/Award Number: K23MH108603
Footnotes
All primary analyses described below were conducted with the full sample as well as a sample that had 100% accuracy on all trap questions. Coefficients remained nearly identical to those presented in text, with no changes in significance.
References
- Antony MM, Bieling PJ, Cox BJ, Enns MW, & Swinson RP (1998). Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment, 10(2), 176–181. [Google Scholar]
- Barkley RA (2011). Barkley Adult ADHD Rating Scale-IV (BAARS-IV). Guilford Press. [Google Scholar]
- Barkley RA (2012). Distinguishing sluggish cognitive tempo from attention-deficit/hyperactivity disorder in adults. Journal of Abnormal Psychology, 121(4), 978–990. [DOI] [PubMed] [Google Scholar]
- Barkley RA (2014). Sluggish cognitive tempo (concentration deficit disorder?): current status, future directions, and a plea to change the name. Journal of Abnormal Child Psychology, 42(1), 117–125. [DOI] [PubMed] [Google Scholar]
- Becker SP, Burns GL, Garner AA, Jarrett MA, Luebbe AM, Epstein JN, & Willcutt EG (2017). Sluggish cognitive tempo in adults: psychometric validation of the adult concentration inventory. Psychological Assessment. Advance online publication. doi: 10.1037/pas0000476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Garner AA, Tamm L, Antonini TN, & Epstein JN (2017). Honing in on the social difficulties associated with sluggish cognitive tempo in children: Withdrawal, peer ignoring, and low engagement. Journal of Clinical Child & Adolescent Psychology, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Langberg JM, Luebbe AM, Dvorsky MR, & Flannery AJ (2014). Sluggish cognitive tempo is associated with academic functioning and internalizing symptoms in college students with and without attention‐deficit/hyperactivity disorder. Journal of Clinical Psychology, 70(4), 388–403. [DOI] [PubMed] [Google Scholar]
- Becker SP, Leopold DR, Burns GL, Jarrett MA, Langberg JM, Marshall SA, ... & Willcutt EG (2016). The internal, external, and diagnostic validity of sluggish cognitive tempo: A meta-analysis and critical review. Journal of the American Academy of Child & Adolescent Psychiatry, 55(3), 163–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SP, Luebbe AM, Fite PJ, Stoppelbein L, & Greening L (2014). Sluggish cognitive tempo in psychiatrically hospitalized children: Factor structure and relations to internalizing symptoms, social problems, and observed behavioral dysregulation. Journal of Abnormal Child Psychology, 42(1), 49–62. [DOI] [PubMed] [Google Scholar]
- Becker SP, & Willcutt EG (2018). Advancing the study of sluggish cognitive tempo via DSM, RDoC, and hierarchical models of psychopathology. European Child & Adolescent Psychiatry, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickham NL, & Fiese BH (1997). Extension of the Children’s Perceptions of Interparental Conflict Scale for use with late adolescents. Journal of Family Psychology, 11(2), 246–250. [Google Scholar]
- Connor DF, Edwards G, Fletcher KE, Baird J, Barkley RA, & Steingard RJ (2003). Correlates of comorbid psychopathology in children with ADHD. Journal of the American Academy of Child & Adolescent Psychiatry, 42(2), 193–200. [DOI] [PubMed] [Google Scholar]
- Cusimano AM, & Riggs SA (2013). Perceptions of interparental conflict, romantic attachment, and psychological distress in college students. Couple and Family Psychology: Research and Practice, 2(1), 45–59. [Google Scholar]
- Cussen A, Sciberras E, Ukoumunne OC, & Efron D (2012). Relationship between symptoms of attention-deficit/hyperactivity disorder and family functioning: a community-based study. European Journal of Pediatrics, 171(2), 271–280. [DOI] [PubMed] [Google Scholar]
- Drabick DA, Gadow KD, & Sprafkin J (2006). Co‐occurrence of conduct disorder and depression in a clinic‐based sample of boys with ADHD. Journal of Child Psychology and Psychiatry, 47(8), 766–774. [DOI] [PubMed] [Google Scholar]
- Ellis B, & Nigg J (2009). Parenting practices and attention-deficit/hyperactivity disorder: new findings suggest partial specificity of effects. Journal of the American Academy of Child & Adolescent Psychiatry, 48(2), 146–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flannery AJ, Becker SP, & Luebbe AM (2016). Does emotion dysregulation mediate the association between sluggish cognitive tempo and college students’ social impairment? Journal of Attention Disorders, 20(9), 802–812. [DOI] [PubMed] [Google Scholar]
- Grych JH, Seid M, & Fincham FD (1992). Assessing marital conflict from the child’s perspective: The Children’s Perception of Interparental Conflict Scale. Child Development, 63(3), 558–572. [DOI] [PubMed] [Google Scholar]
- Halberstadt AG, Cassidy J, Stifter CA, Parke RD, & Fox NA (1995). Self-expressiveness within the family context: Psychometric support for a new measure. Psychological Assessment, 7(1), 93–103. [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal, 6(1), 1–55. [Google Scholar]
- Jarrett MA, Rapport HF, Rondon AT, & Becker SP (2017). ADHD dimensions and sluggish cognitive tempo symptoms in relation to self-report and laboratory measures of neuropsychological functioning in college students. Journal of Attention Disorders, 21(8), 673–683. [DOI] [PubMed] [Google Scholar]
- Johnston C, & Mash EJ (2001). Families of children with attention-deficit/hyperactivity disorder: review and recommendations for future research. Clinical Child and Family Psychology Review, 4(3), 183–207. [DOI] [PubMed] [Google Scholar]
- Johnson HD, Lavoie JC, & Mahoney M (2001). Interparental conflict and family cohesion: Predictors of loneliness, social anxiety, and social avoidance in late adolescence. Journal of Adolescent Research, 16(3), 304–318. [Google Scholar]
- Kamradt JM, Momany AM, & Nikolas MA (2017). Sluggish Cognitive Tempo Symptoms Contribute to Heterogeneity in Adult Attention-Deficit Hyperactivity Disorder. Journal of Psychopathology and Behavioral Assessment, 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz SJ, Conway CC, Hammen CL, Brennan PA, & Najman JM (2011). Childhood social withdrawal, interpersonal impairment, and young adult depression: a mediational model. Journal of Abnormal Child Psychology, 39(8), 1227–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA, & Judd CM (1984). Estimating the nonlinear and interactive effects of latent variables. Psychological Bulletin, 96(1), 201–210. [Google Scholar]
- Keown LJ (2012). Predictors of boys’ ADHD symptoms from early to middle childhood: The role of father–child and mother–child interactions. Journal of Abnormal Child Psychology, 40(4), 569–581. [DOI] [PubMed] [Google Scholar]
- Klein AG, & Muthén BO (2007). Quasi-maximum likelihood estimation of structural equation models with multiple interaction and quadratic effects. Multivariate Behavioral Research, 42(4), 647–673. [Google Scholar]
- Klein A, & Moosbrugger H (2000). Maximum likelihood estimation of latent interaction effects with the LMS method. Psychometrika, 65(4), 457–474. [Google Scholar]
- Kring AM, & Gordon AH (1998). Sex differences in emotion: expression, experience, and physiology. Journal of personality and social psychology, 74(3), 686. [DOI] [PubMed] [Google Scholar]
- Krishnakumar A, & Buehler C (2000). Interparental conflict and parenting behaviors: A meta‐analytic review. Family Relations, 49(1), 25–44. [Google Scholar]
- Little TD (2013). Longitudinal structural equation modeling. Guilford Press; Chicago, IL. [Google Scholar]
- Little TD, Cunningham WA, Shahar G, & Widaman KF (2002). To parcel or not to parcel: Exploring the question, weighing the merits. Structural equation modeling, 9(2), 151–173. [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. [DOI] [PubMed] [Google Scholar]
- Luebbe AM, & Bell DJ (2014). Positive and negative family emotional climate differentially predict youth anxiety and depression via distinct affective pathways. Journal of Abnormal Child Psychology, 42(6), 897–911. [DOI] [PubMed] [Google Scholar]
- McCoy K, Cummings EM, & Davies PT (2009). Constructive and destructive marital conflict, emotional security and children’s prosocial behavior. Journal of Child Psychology and Psychiatry, 50(3), 270–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2007). Mplus. Statistical analysis with latent variables. Version, 3. [Google Scholar]
- Nolen-Hoeksema S, & Watkins ER (2011). A heuristic for developing transdiagnostic models of psychopathology: Explaining multifinality and divergent trajectories. Perspectives on Psychological Science, 6(6), 589–609. [DOI] [PubMed] [Google Scholar]
- Oppenheimer DM, Meyvis T, Davidenko N, 2009. Instructional manipulation checks: Detecting satisficing to increase statistical power. Journal of Experimental Social Psychology 45, 867–872. [Google Scholar]
- Pheula GF, Rohde LA, & Schmitz M (2011). Are family variables associated with ADHD, inattentive type? A case–control study in schools. European Child & Adolescent Psychiatry, 20(3), 137–145. [DOI] [PubMed] [Google Scholar]
- Rondon AT, Hilton DC, Jarrett MA, & Ollendick TH (2018). Sleep, internalizing problems, and social withdrawal: Unique associations with elevated sluggish cognitive tempo symptoms. Journal of Attention Disorders. Advance online publication. doi: 10.1177/1087054718756197. [DOI] [PubMed] [Google Scholar]
- Rodrigues LN, & Kitzmann KM (2007). Coping as a mediator between interparental conflict and adolescents’ romantic attachment. Journal of Social and Personal Relationships, 24(3), 423–439. [Google Scholar]
- Schiff M, Plotnikova M, Dingle K, Williams GM, Najman J, & Clavarino A (2014). Does adolescent’s exposure to parental intimate partner conflict and violence predict psychological distress and substance use in young adulthood? A longitudinal study. Child Abuse & Neglect, 38(12), 1945–1954. [DOI] [PubMed] [Google Scholar]
- Schwartz OS, Dudgeon P, Sheeber LB, Yap MB, Simmons JG, & Allen NB (2012). Parental behaviors during family interactions predict changes in depression and anxiety symptoms during adolescence. Journal of Abnormal Child Psychology, 40(1), 59–71. [DOI] [PubMed] [Google Scholar]
- Sollman MJ, Ranseen JD, & Berry DT (2010). Detection of feigned ADHD in college students. Psychological Assessment, 22(2), 325–335. [DOI] [PubMed] [Google Scholar]
- Turner HA, & Kopiec K (2006). Exposure to interparental conflict and psychological disorder among young adults. Journal of Family Issues, 27(2), 131–158. [Google Scholar]
- Wood WL, Lewandowski LJ, Lovett BJ, & Antshel KM (2017). Executive dysfunction and functional impairment associated with sluggish cognitive tempo in emerging adulthood. Journal of Attention Disorders, 21(8), 691–700. [DOI] [PubMed] [Google Scholar]


