Abstract
Background:
Analyses from the SAMMPRIS trial showed that good control of vascular risk factors (SBP, LDL, and exercise) was associated with fewer vascular events and exercise had the biggest impact on outcome. We sought to determine the type and duration of exercise performed by SAMMPRIS patients during the trial.
Methods:
SAMMPRIS aggressive medical management included a telephonic lifestyle modification program, INTERVENT, that was provided free of charge to all subjects during the study. We analyzed self-reported data collected by INTERVENT on the patients’ type and duration of exercise from baseline (n= 394) to 3 years (n=132). We calculated the mean duration for each exercise type at each time period and then compared the change in exercise duration from baseline using paired t-tests and Wilcoxon signed rank tests.
Results:
Walking was the most common form of exercise at all time points, as measured by both the duration of exercise and the number of patients performing the exercise. The mean duration of walking and other aerobic activities increased significantly from baseline to all other time points.
Conclusion:
The type of self-reported exercise performed by SAMMPRIS patients included mostly walking or other aerobic activity and increased significantly during follow-up.
Introduction:
Intracranial atherosclerotic stenosis (ICAS) is one of the most important causes of stroke worldwide1 and is associated with high risk of stroke recurrence2, 3. The Stenting and Aggressive Medical management for prevention of Recurrent Stroke in Intracranial Stenosis (SAMMPRIS) trial incorporated intensive risk factor control for all patients and showed that aggressive medical management is superior to stenting in patients with severe (70–99%) symptomatic intracranial atherosclerotic disease 4, 5. Post hoc analyses of patients in the medical arm of SAMMPRIS showed that physical activity was the strongest predictor of lower risk of recurrent stroke and vascular events6. The purpose of this study is to report the type and duration of physical activity in the SAMMPRIS trial.
Methods:
The overall design of SAMMPRIS and its aggressive medical management protocols have been described previously4, 7. In brief, SAMMPRIS was an NIH-funded, investigator-initiated and designed phase III randomized multicenter trial in which 451 patients were randomized at 50 sites in the USA to aggressive medical therapy alone vs. percutaneous transluminal angioplasty and stenting (PTAS) with the wingspan stent system plus aggressive medical therapy. Aggressive risk factor management primarily targeted systolic blood pressure (SBP) < 140 mm Hg, and low density lipoprotein (LDL) < 70 mg/dl. Secondary risk factors targeted included physical inactivity, diabetes mellitus, weight, and smoking. Using a commercially available lifestyle modification program (INTERVENT), all subjects received coaching on healthy lifestyle behaviors at regularly schedule times throughout the study at no charge. Lifestyle coaches provided individualized risk factor counseling (via telephone or internet) twice a month for 6 months and monthly thereafter. Risk factor values for each subject during follow-up were recorded at baseline, 30 days, 4 months, and every 4 months thereafter. Through INTERVENT, patients were provided with a health coach, who, after assessing the patient’s health, lifestyle and their readiness for change, develops a personal action plan and then follows up regularly with the patient to monitor their adherence to the plan. Physical activity was assessed at the sites using the 8-point Physician based Assessment and Counseling for Exercise (PACE) questionnaire, which the participants completed at each visit. INTERVENT also collected self-reported exercise type and duration of activity (see appendix for questionnaire).
We analyzed self-reported data collected by INTERVENT on the patients’ type and duration from baseline to close out. We calculated the mean duration of each exercise type at each time period and the compared the change in exercise duration from baseline using paired t-tests.
Results:
Of the 451 patients enrolled in SAMMPRIS, INTERVENT physical activity data from 394 patients was available at baseline.
As shown in the Figure, walking was the most common form of exercise reported by patients at all points in the study. The percentage of patients who reported walking for exercise increased from baseline 166 /394 (42%) to 1 year 167/264 (63%). In contrast, only 34/394 (8%) reported using a stationary cycle and 27/394 (6%) using a treadmill as their form of exercise at baseline. At 1 year, 28/264 (13%) reported stationary cycle and 28/264 (10%) reported treadmill use.
Figure:
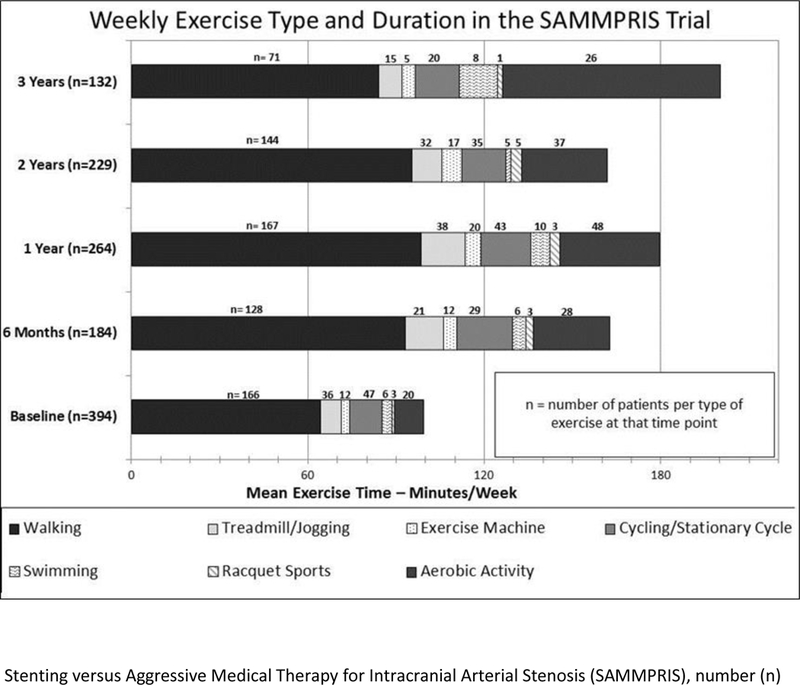
Weekly Exercise Type and Duration in the SAMMPRIS Trial Stenting versus Aggressive Medical Therapy for Intracranial Arterial Stenosis (SAMMPRIS), number (n)
Walking was the form of activity that also had the highest duration for the patients overall. The mean duration of walking was 64.3 (±131.7) minutes per week at baseline, 98.4 (±142.4) at 1 year, 95.5 (±138.9) at 2 years, and 84.0 (±117.0) at 3 years (table 1).
Table 1:
Weekly exercise types and duration (minutes) in the SAMMPRIS trial SAMMPRIS (Stenting versus Aggressive Medical Management for Intracranial Arterial Stenosis)
| Follow Up | Walking | Treadmill | Stationary Cycle |
Exercise Machine | Jogging | Cycling | Swimming | Racquet Sports | Aerobic Dance/ Floor Exercise |
Other Aerobic Activity |
Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | |||||||||||
| Mean | 64.3 | 4.7 | 7.4 | 2.8 | 1.8 | 3.6 | 3.5 | 0.8 | 0.9 | 9.0 | 98.9 |
| (sd) | (131.7) | (21.9) | (35.1) | (18.7) | (15.6) | (24.3) | (44.7) | (12.9) | (8.5) | (82.6) | (190.1) |
| Median (Q1, Q3) | 0 (0, 90) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0, (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 20 (0, 140) |
| 6 Months(n=184) | |||||||||||
| Mean | 93.2 | 8.8 | 11.6 | 4.3 | 3.5 | 7.0 | 4.6 | 2.4 | 4.5 | 21.2 | 160.9 |
| (sd) | (120.5) | (37.3) | (47.4) | (18.8) | (32.4) | (44.8) | (38.4) | (21.2) | (31.1) | (83.7) | (198.1) |
| Media(Q1,Q3) | 60(0,17.5) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 104(36.3,210) |
| 1 Year (n=264) | |||||||||||
| Mean | 98.4 | 12.1 | 12.7 | 5.3 | 3.1 | 4.0 | 6.7 | 3.2 | 4.4 | 29.7 | 179.7 |
| (sd) | (142.4) | (43.5) | (42.8) | (22.3) | (19.7) | (23.7) | (55.6) | (36.0) | (22.1) | (130.8) | (234.5) |
| Median(Q1,Q3) | 60(0,147.5) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 120(20, 247.5) |
| 2 Years (n=229) | |||||||||||
| Mean | 95.5 | 7.7 | 10.1 | 6.8 | 2.0 | 4.9 | 1.7 | 3.7 | 2.7 | 25.6 | 160.7 |
| (sd) | (138.9) | (23.2) | (35.6) | (27.8) | (15.1) | (39.9) | (14.0) | (30.2) | (18.7) | (122.0) | (207.7) |
| Median (Q1,Q3) | 60 (0, 140) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 110(30, 210) |
| 3 Years (n=132) | |||||||||||
| Mean | 84.0 | 6.1 | 8.6 | 4.6 | 2.1 | 5.9 | 12.8 | 1.8 | 4.7 | 68.6 | 199.3 |
| (sd) | (117.0) | (21.9) | (26.9) | (24.7) | (16.8) | (35.7) | (78.8) | (20.9) | (25.7) | (247.5) | (314.7) |
| Median (Q1, Q3) | 42.5(0,122. 5) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 97.5 (0, 240) |
SAMMPRIS (Stenting versus Aggressive Medical Management for Intracranial Arterial Stenosis)
When comparing the change in duration of walking for each individual at follow up compared to baseline, there was a significant increase in the mean duration of walking at all points (+40 minutes at 6 months, +36.8 minutes at 1 year, +32.4 minutes at 2 years, and +21.3 minutes at 3 years (p <0.05).
Discussion:
A post-hoc analysis from the SAMMPRIS trial showed that among patients with symptomatic severe intracranial atherosclerosis, physical activity was the most important risk factor associated with lower risk of recurrent stroke and vascular events6. SAMMPRIS also showed a positive linear relationship between intensity and duration of activity (as measured by the PACE score) and magnitude of prevention benefit (i.e. more exercise = lower risk) 6. By analyzing the physical activity data collected by INTERVENT in this report, we determined that the most common physical activity done by SAMMPRIS patients was walking, as measured by both the number of patients performing the exercise and the duration of exercise.
An AHA/ASA scientific statement recommends that stroke survivors beyond the acute phase of recovery should perform aerobic activity for 20–60 minutes per day, 3–5 times each week, as well as muscle strength and endurance sessions8. Yet, previous studies have shown that stroke survivors have low level of activity 9. A study by Ashe et al, showed that physical activity of community-living stroke survivors is lower than that of older adults with cardiovascular and musculoskeletal health conditions. This is believed to be related to various factors including post stroke disability, depression and fatigue10.
In SAMMPRIS, we found that increased physical activity among patients with prior stroke or TIA is feasible. The percentage of SAMMPRIS patients who met physical activity targets increased throughout the duration of the study from 30% at baseline to 68% at 3 years 11. In this report, we also found that for individual patients who exercised, their activity remained increased at each follow up visit compared to baseline. This increase in physical activity is likely due to the impact of frequent counseling by INTERVENT lifestyle coaches, given that improvement of many risk factors, including physical activity, was associated with good compliance with INTERVENT12. In addition, site coordinators and neurologists were also instructed to counsel patients on the importance of exercise.
This report has some limitations. While we demonstrate that increased physical activity is achievable in stroke patients, it should be noted that SAMMPRIS only included patients with non-disabling (modified Rankin score of <=3) stroke or TIA at baseline. Therefore, our findings do not include patients who are unable to walk without assistance at baseline. In addition, some argue that the intensive medical management provided in SAMMPRIS was not “real world” and therefore the findings related to risk factor control and physical activities are not generalizable. However, lifestyle modification counseling programs are commercially available and covered by many insurance companies. Furthermore, the AHA/ASA scientific statement on physical activity in stroke survivors recommends physicians encourage physical activity and specifically endorses the use of comprehensive lifestyle programs, such as cardiac rehabilitation, after mild stroke to improve risk factors10.
Conclusion:
Walking was the most common type of exercise performed by SAMMPRIS patients and the duration and percentage of subjects walking increased significantly during follow-up. Given that physical inactivity is associated with recurrent vascular events and that improvement in physical activity in stroke patients is feasible, clinicians should encourage stroke patients to increase their activity.
Acknowledgments
Sources of Funding
This work was supported by National Institutes of Health (NIH) U01NS058728.
Footnotes
Disclosures
Dr Fiorella received research/salary support from Siemens, Microvention, Penumbra, and Sequent. Medtronic, Sequent, Codman and Shurtleff, Penumbra, and Microvention provided consulting fees to Dr Fiorella. He received Codman & Shurtleff (REVIVE) royalties and fund from Vascular Simulations LLC. Dr Turan received personal fees from Gore and Boehringer Ingelheim for participating as a stroke adjudicator in clinical trials unrelated to this work. M.I. Chimowitz received other support from Astra Zeneca and Stryker Neurovascular (formerly Boston Scientific Neurovascular) related to the Stenting and Aggressive Medical Management for the Prevention of Recurrent Stroke in Intracranial Stenosis (SAMMPRIS) trial. Dr. Gordon is a member of INTERVENT international LLC. The other authors report no conflicts
References:
- 1.Gorelick PB, Wong KS, Bae HJ, et al. Large artery intracranial occlusive disease, a large worldwide burden but a relatively neglected frontier. Stroke 2008;39:2396–2399. [DOI] [PubMed] [Google Scholar]
- 2.Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med 2005;352:1305–1316. [DOI] [PubMed] [Google Scholar]
- 3.Mazighi M, Tanasescu R, Ducrocq X, et al. Prospective study of symptomatic atherothrombotic intracranial stenoses: the GESICA study. Neurology 2006;66:1187–1191 [DOI] [PubMed] [Google Scholar]
- 4.Turan TN, Lynn MJ, Nizam A, et al. Rationale, design, and implementation of aggressive risk factor management in the Stenting and Aggressive Medical Management for Prevention of Recurrent Stroke in Intracranial Stenosis (SAMMPRIS) trial. Circ Cardiovasc Qual Outcomes 2012;5:e51–e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med 2011;365:993–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turan TN, Nizam A, Lynn MJ, Egan BM, Le NA, Lopes-Virella MF,& Janis LS (2017). Relationship between risk factor control and vascular events in the SAMMPRIS trial. Neurology, 88(4), 379–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chimowitz MI, Lynn MJ, Turan TN, et al. Design of the stenting and aggressive medical management for preventing recurrent stroke in intracranial stenosis trial. J Stroke Cerebrovasc Dis 2011;20:357–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Billinger SA, Arena R, Bernhardt J, et al. ; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Lifestyle and Cardiometabolic Health; Council on Epidemiology and Prevention; Council on Clinical Cardiology. Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014; 45:2532–2553. [DOI] [PubMed] [Google Scholar]
- 9.Gebruers N, Vanroy C, Truijen S, et al. Monitoring of physical activity after stroke: a systematic review of accelerometrybased measures. Arch Phys Med Rehabil. 2010;91:288–297. [DOI] [PubMed] [Google Scholar]
- 10.Ashe MC, Miller WC, Eng JJ, et al. Older adults, chronic disease and leisure-time physical activity. Gerontology. 2009;55:64–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Derdeyn Colin P., Chimowitz Marc I., Lynn Michael J., Fiorella David, Turan Tanya N., Janis L. Scott, Montgomery Jean et al. “Aggressive medical treatment with or without stenting in high-risk patients with intracranial artery stenosis (SAMMPRIS): the final results of a randomised trial.” The Lancet 383, no. 9914 (2014): 333–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turan TN, Al Kasab S, Nizam, et al. (2018). Relationship between Risk Factor Control and Compliance with a Lifestyle Modification Program in the Stenting Aggressive Medical Management for Prevention of Recurrent Stroke in Intracranial Stenosis Trial. Journal of Stroke and Cerebrovascular Diseases, 27(3), 801–805. [DOI] [PubMed] [Google Scholar]


