Abstract
Competency-Based Approaches to Community Health (COACH) is a randomized controlled trial of a family-centered, community-based, and individually-tailored behavioral intervention for childhood obesity among Latino pre-school children. COACH focuses on improving personal agency for health behavior change by tailoring content to overcome contextual barriers. The intervention focuses on diet, physical activity, sleep, media use, and engaged parenting. The content is individually adapted based on routine assessments of competency in specific health behaviors using a mobile health platform and novel measurement tools developed by our team. In response to these regular assessments, health coaches provide tailored health behavior change strategies to help families focus on the areas where they decide to improve the most. The intervention consists of a 15-week group-based intensive phase, with weekly sessions delivered by health coaches in community centers. Following weekly sessions, a 3-month maintenance phase of the intervention consists of twice monthly coaching calls for participants to focus on individual health goals for their families.
The primary outcome of the trial is child body mass index trajectory over 1 year. Secondary outcomes include parent body mass index change, child waist circumference, child diet, child physical activity, and other psychosocial mediators of child health behavior change. The control arm consists of a school readiness intervention, delivered by the Nashville Public Library.
By applying a personalized approach to child behavior change, in the setting of both family and community, COACH aims to develop sustainable solutions for childhood obesity by supporting healthy childhood growth in low-income, minority preschool children.
Keywords: Childhood Obesity, Behavioral Intervention, Personal Agency
1. Introduction
In the last 20 years there have been over 300 health-behavior interventions tested in randomized controlled trials to prevent or treat childhood obesity.1,2 These trials often result in heterogeneous, disappointing, and short-lived results.3-8 While it is widely accepted that there are multiple interacting determinants of childhood obesity, including macro-level influences (e.g., poverty, social norms, etc.) and micro-level influences (e.g., genetics, satiety set-point, etc.), the optimal approach for intervening across these multiple levels remains a topic ripe for further investigation.9
One challenge to the implementation of behavioral interventions for childhood obesity is the persistent reliance on an evaluation methodology that has its underpinnings in drug trials. Namely, behavioral interventions to reduce childhood obesity have often applied the same “dose” of the intervention to each participant, regardless of their pre-existing competency with health behaviors like healthy diet and physical activity. Furthermore, it is imperative that attempts to support healthy childhood growth consider the foundational contribution of a person’s context (i.e., culture, environment) to their health behaviors, especially as children from traditionally underserved minorities are often hardest hit by obesity.10 Thus, one potential contributor to the modest results of behavioral obesity trials is a one-sized-fits-all approach that hardly fits anyone.
The paradigm of personalized medicine considers how best to tailor treatment options to meet the unique needs of individuals. But, recognizing which treatments work best and for whom should not be limited to pharmacology or genetics. In order to operationalize a personalized childhood obesity intervention we developed an individually-adaptable curriculum using a trans-disciplinary approach that builds on theoretical and practical lessons from the learning sciences.
For decades, experts in learning theory have recognized that reducing variation in learning outcomes requires increasing variation in instruction (i.e., a personalized approach).11 In the context of childhood obesity, competency-based learning theory posits that an individual gains proficiency in health behaviors (e.g., diet and physical activity) by gaining mastery over specific skills and knowledge relevant to the health behavior in question. For example, in order to become proficient at eating healthy snacks, an individual must integrate several competencies (e.g., calorie-counting, successful navigation of grocery shopping, avoiding unplanned snacks) that are often learned in a non-linear manner and require contextualization.
The Competency-Based Approaches to Community Health (COACH) randomized controlled trial (RCT) tests a novel multi-level behavioral intervention for childhood obesity prevention and treatment, designed to be a personalized intervention that still leverages the power of community and individual contextual factors. This paper describes the design, methodology, and proposed evaluation of COACH. This intervention builds on best practices from childhood obesity interventions, including 1) focusing on group-based therapy to build social connections, 2) targeting both parents and children simultaneously, 3) leveraging the strengths of the built environment to facilitate physical activity, and 4) implementing behavior change strategies (i.e., goal setting, self-monitoring, and problem solving) in the context of health behaviors (i.e., diet, physical activity, sleep, media use, and engaged parenting).12-14 The main advancement of the COACH intervention is the way a personalized behavior change intervention is operationalized in this community and group-based context.
One of the primary goals of this intervention is to reduce health inequity through tailored content that addresses important sociocultural barriers in a historically underserved community with high rates of childhood obesity. Consequently, the participants included in the COACH intervention are from the Hispanic/Latino community, where childhood obesity prevalence approaches 22%.10,15 There are several ways that this intervention accounts for cultural differences: 1) the intervention was developed with community input using participatory approaches to research design; 2) the intervention is delivered by a native Spanish speaking health coach; 3) the intervention uses recipes that are consistent with typical food choices for the local Hispanic/Latino community; and 4) the intervention specifically addresses barriers to healthy behavior that are timely and relevant to immigrant and minority populations.
Making a sustainable improvement in childhood obesity will require the research community to push the envelope of existing paradigms and move beyond what has already been tried. By creating a personalized behavioral intervention for childhood obesity that engages families from underserved communities, the COACH RCT steps into new territory by considering which aspects of behavioral interventions work best for whom.
2. Materials and Methods
2.1. Study Aims
The primary aim of COACH is to evaluate the effectiveness of a novel personalized obesity intervention to prevent or treat childhood obesity at 1-year follow-up among children ages 3-5 at the time of study enrollment. The trial involves a 6-month intervention with 6 months of additional follow-up. We hypothesize that children in the intervention arm will demonstrate healthier body mass index (BMI) trajectories compared to the control arm over the 12-month trial period. We also hypothesize that both parents and children in the intervention arm will demonstrate improvements in health-related behavioral competencies (diet, physical activity, sleep, media use, and engaged parenting) compared to the control arm at 3 months, 9 months, and 12 months of follow-up. A secondary aim of COACH is to evaluate the effectiveness of the intervention using qualitative methodology, including focus groups and key informant interviews to investigate which components of the intervention supported sustainable health behavior change.
2.2. Theoretical Framework and Conceptual Model
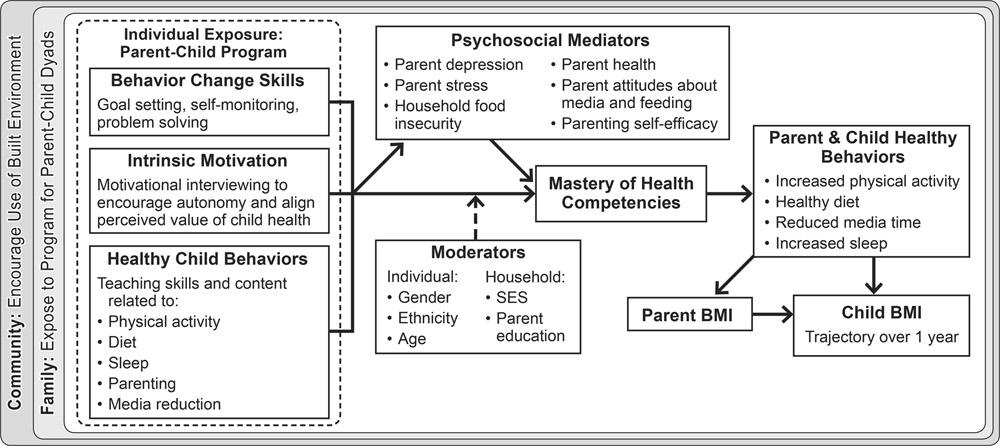
Personalized approaches to medicine consider how to best account for social, cultural, environmental, and individual variants. Our work aims to develop efficacious and dynamic methods to meet the unique needs of community members so as to prevent and treat pediatric obesity. This work draws on the synergies, as well as the unique contributions, between the theoretical positions of both health sciences and learning sciences.16 We employ theoretical frameworks from health sciences to develop a multi-level understanding of the determinants of childhood obesity (Figure 1), drawing on 1) self-determination theory, which articulates how competence, autonomy, and relatedness support motivation17 and 2) social cognitive theory, which frames learning as a reciprocal interaction between individual, environment, and behaviors.18,19 We also draw on theoretical frameworks from the learning sciences to understand how community members can sustainably change their practices, including 1) competency-based learning, which supports learners to develop competency in specific skills via personalized instruction20 and 2) scales of practice, which focuses on the need to make learning sustainable over time, socially relevant, and geographically situated.21
Figure 1:
A multi-level model for child obesity, recognizing the importance individual, family, and community influences on child health behaviors. This model shows the operationalized intervention constructs of the COACH intervention and the relationships between key mediators of child BMI.
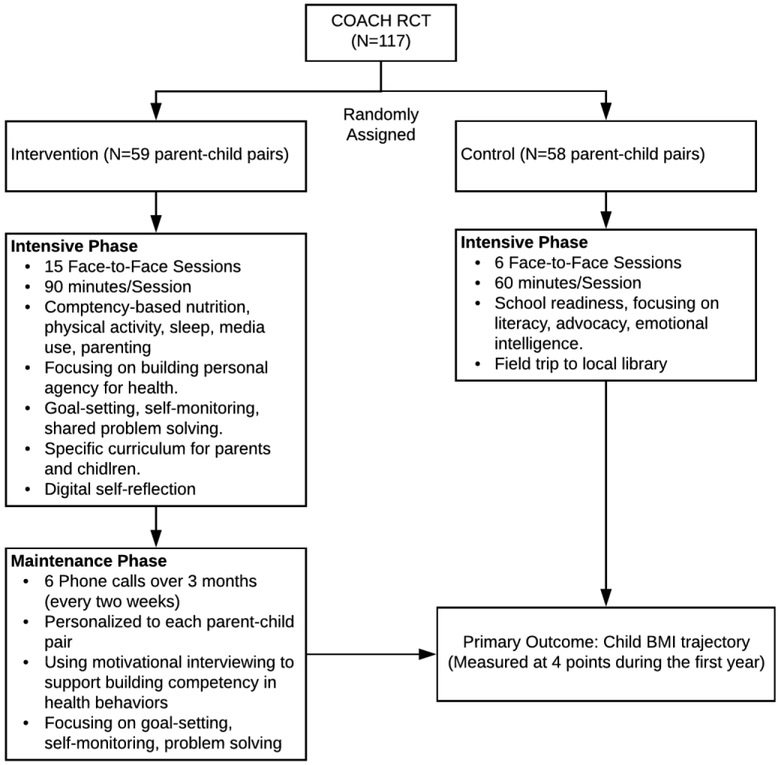
2.3. Trial Design Overview
COACH is a parallel-group, randomized controlled trial designed to prevent and treat childhood obesity by delivering a personalized healthy-lifestyle intervention to high-risk, parent-preschool child pairs. Parent-child pairs are randomized to either the intervention or control group. The COACH intervention is a tiered-intensity intervention lasting 6 months. The content focuses on developing competencies in health behaviors necessary to support healthy childhood growth (diet, physical activity, sleep, media use, and engaged parenting). The control group is a 3-month school-readiness intervention (readiness to read, multi-environment learning, and advocacy). See Figure 2 for participant flow through the trial.
Figure 2:
Flow diagram of intervention content for the COACH intervention.
The primary outcome of child BMI trajectory considers raw BMI collected at 4 points over the study period, which allows for characterization of the BMI growth curve during the important period of childhood growth. Other measures include anticipated mediators of the intervention (i.e., diet, physical activity for parents and children) as well as important sociodemographic characteristics that may modify treatment results.
As of the writing of this manuscript, the intervention has been delivered but not all follow-up data have been collected.
2.4. Study Setting and Population
Because childhood obesity is disproportionately prevalent among Latino families,10 COACH focused exclusively on parent-child pairs who self-identified as Hispanic or Latino. Parent-child pairs were recruited from Nashville, TN. The intervention was conducted in local community recreation centers. These centers were chosen based on their central location and accessibility for individuals from our target population. Participants were exclusively recruited from zip code regions in a 5-mile radius surrounding the community recreation centers to facilitate use of the built environment to promote physical activity and other health behaviors. To be eligible for the study, children had to already have obesity (i.e., BMI percentile ≥95th on standardized CDC growth curves) or be at risk for developing obesity (i.e., BMI percentile ≥ 50th on standardized CDC growth curves).
Inclusion criteria:
Child age 3-5 at time of randomization
Self-identified as Latino/Hispanic and speak Spanish
Child’s body mass index ≥50th percentile.
Parental commitment to participate in 1-year study
Consistent phone access
Parent age ≥18 years
Parents and children must be healthy, without medical conditions limiting physical activity
Residence in one of the following zip-code regions: 37013, 37115, 37189, 37203, 37204, 37206, 37207, 37208, 37210, 37211, 37214, 37216, 37217, 37219, 37220, 37228
We defined the index “parent” as the legal guardian of the child who spends the majority of time with the child at home.
2.5. Recruitment and Enrollment
We conducted rolling recruitment between April 2017 and September 2017. Recruitment was conducted by a native Spanish-speaking individual with extensive experience with community recruitment. Recruitment sites included doctors’ offices and local community sites serving families (e.g., pre-K programs, churches, community service programs). Referrals by participants or community members were accepted. Initial BMI eligibility was assessed at the time of recruitment.
Written informed consent was obtained by all study participants prior to baseline data collection. Since children were under age 7 when enrolled, the parent/legal guardian granted permission for participation. Verbal assent was obtained from children. Additionally, the study team paid close attention to dissenting behaviors that may have indicated a child’s unwillingness to participate. BMI eligibility was confirmed at the time of consent. We employed an enhanced approach to informed consent that uses visual aids and low-health-literacy communication techniques in addition to the traditional signed informed consent process.22,23 Informed consent was conducted by native Spanish speaking research assistants. This study was approved by the Vanderbilt University Medical Center Review Board and registered at ClinicalTrials.gov (NCT03141151).
2.6. Randomization
Within each of the two community-center regions, parent-child pairs were randomized to either the intervention or control group using a sequence with randomly permuted blocks of varying size. All baseline data was collected prior to randomization. Immediately prior to randomization, the research assistant confirmed both interest and confidence in participating in the study, regardless of randomization assignment.
All study staff who collect or interpret data are blinded to study group assignment. Because this is a behavioral intervention, neither the interventionist nor the participants could be blinded to study group assignment. Research staff who collect data after randomization will remain blinded until the end of the study, with the exception of those assessing key process measures necessary to insure appropriate intervention fidelity.
2.7. Retention
To increase the chances of successful retention, we use a multi-pronged strategy that consists of: 1) obtaining multiple methods of contact and updating those methods at each point of contact with the study team; 2) developing participant databases with protocols for loss to follow-up; 3) building effective relationships with study participants throughout the study; 4) providing frequent contact via text and phone call; 5) offering financial incentives for participation in data collection; and 6) providing scheduling flexibility around participant preference.
2.8. Intervention Group
COACH is a tiered intensity intervention with an intensive phase consisting of 15 weekly sessions, followed by 3 months of bi-monthly coaching calls.
2.8.1. Intensive Phase
The intensive phase curriculum focuses on developing agency for health behaviors for both parents and children by providing a personalized approach to health behavior change. The content is focused on healthy diet, physical activity, healthy sleep, engaged parenting, and media use. Each session lasted 90 minutes and was conducted in a local Parks and Recreation community center, with a cohort of 8-11 participants. The key curricular components that facilitate a personalized approach within a group setting include 1) individual assessment of competency in 7 health behaviors, 2) the development of individualized learning plans with the participant’s health coach, and 3) giving participants choice about which of the 5 key content areas to spend extra time during sessions. Each of the sessions is designed around key components of behavior change theory, with a focus on goal setting, self-monitoring, and problem solving. Each session consisted of several components: 1) welcome and icebreaker, 2) goal check-in from previous week, 3) group problem solving around previous week’s goal, 4) interactive didactic session, 5) small group discussion, 6) zoom-in on participant-chosen material, 7) setting a new goal, 8) shared interaction with children around material learned in the session, and 9) a shared meal. Each week goals were set using the SMART goal framework: Specific, Measureable, Achievable, Realistic, and Timely.12
One of the key objectives of the COACH intervention is to develop a meaningful and trusted relationship between the interventionist and the participants, as well as among the participants in each cohort. One strategy to achieve this was through shared problem solving, facilitated each week by the interventionist. Participants first assessed their progress on their goal from the previous week by gauging success on a Likert scale from 1-5. The interventionist then facilitated a conversation among participants using key concepts from motivational interviewing and low health-literacy communication techniques. During these conversations, the interventionists prioritized building relationships with and among families, understanding their needs, and providing support for their self-identified health goals.
The didactic component of each session has three key messages, built on successful implementation of previous child obesity interventions.12
Children were invited to participate in a children’s program designed to mirror the adult intervention content that occurred concurrently with the adult intervention content. Child sessions include 4 components: 1) interactive didactic session, 2) hands-on connected activity, 3) stretching and physical activity, and 4) review. Children then joined the parent session for shared interaction around material learned in the session and a shared meal.
As a part of each session, the parents received a booklet to reinforce key messages. These booklets have been previously developed and tested using best-practices for low-health literate communication and have been assessed using Suitability Assessment of Materials instrument.24
2.8.2. Maintenance Phase
After participants completed the intensive phase, they participated in twice-monthly coaching calls. The content of these calls focuses on setting individual goals, gauging progress on previous goals, and problem solving. These calls use motivational interviewing and are based on strategies identified in previous adult weight loss trials.25
2.8.3. Control Group
The control group was enrolled in a school readiness program, developed by the Nashville Public Library. These twice monthly sessions, over the course of 3 months, consisted of the following topics: 1) Getting Ready to Read, 2) Home is a Learning Zone, 3) Fun with Play, 4) Words and Letters in the World Around Us, 5) Work that Body, Feed that Mind, and 6) Advocacy. Participants were also invited to a field trip to their local library, to learn about services offered.
2.9. Incentives
Monetary compensation is provided for participation in data collection sessions and focus groups, but not for participation in intervention sessions. Meals or snacks (depending on time of day) were offered at each intervention and control session. We also conducted a raffle of a gift basket at one intervention session to encourage attendance at key intervention sessions.
2.10. Data Collection
All data collection occurs at a local community center or the participant’s home, based on participant preference. Data are collected at baseline, 15 weeks (after intensive phase), 6 months (after maintenance phase), 9 months after randomization, and 1 year after randomization. See Table 1 for the list of measures collected at each time point.
Table 1:
Frequency of Measurement for Primary and Secondary Outcomes
| Construct | Measure | Timing and Frequency |
|---|---|---|
| Parent and Child Body Mass Index | Research calibrated, digital scale and free-standing stadiometer. | T1, T2, T3, T4 |
| Competency of Health Behaviors | Newly developed scales: 7 constructs (5 items each) | T1, T2, T3, T4 |
| Child Diet | CDC Module (30 items)26 | T1, T2, T3, T4 |
| Parent Diet | 8 items measuring diet quality and problem eating behaviors.27 | T1, T2, T3, T4 |
| Parent and Child Physical Activity | CDC developed questions (12 items) | T1, T2, T3, T4 |
| Psychosocial mediators (stress, parent health, parent attitudes/practices around child health behaviors) | CFSQ (10 items),28 PAPP (38 items),29 PSS (7 items),30 Self-efficacy (16 items)31, CEBQ (4 items),32 CFQ (4 items).33 | T1, T2, T3, T4 |
| Demographics | Survey items: 15 items.34 | T1, T2, T3, T4 |
| Acculturation | Brief Acculturation Scale for Hispanics (4 items)35 | T1, T2, T3, T4 |
| Child Diet Recall Assessments | Nutrition Data System for Research (NDSR) | T4 |
T1: Baseline; T2: 3 month follow-up; T3: 9 month follow-up; T4: 1 year follow-up CFSQ: Child Feeding Styles Questionnaire. PAPP: Preschooler Physical Activity Parenting Practices PSS: Perceived Stress Scale. CEBQ: Children’s Eating Behavior Questionnaire. CFQ: Child Feeding Questionnaire
2.10.1. Primary Outcome Measure
The trajectory of child body mass index is the primary outcome measure, and child BMI is collected at all 4 time points. Weight and height are measured in light clothing without shoes. Weight is measured to the nearest 0.1kg using research-grade scales (Seca Model 876). Height is measured to the nearest 0.1cm using a freestanding stadiometer with movable headboard (Seca Model 217). BMI is calculated as weight in kilograms divided by the square of height in meters. The average of two height and two weight measures is taken, provided the measures fall within 0.5cm and 0.3kg of each other respectively. If there is a discrepancy, a third measure is taken to confirm accuracy. The average of the closest two measures are used for analysis.
2.10.2. Secondary Outcomes
The main secondary outcomes are parent BMI trajectory (measured and calculated as above), parent and child waist measurement, child diet, child physical activity, parent diet, and parent physical activity. Waist measurements for both parent and child are measured to the nearest 0.1cm using research-grade tape measures (Gulick II Tape Measure, Model). The average of two waist measures is taken, provided the measures fall within 1.0 cm of each other. If there is a discrepancy, a third measure is taken to confirm accuracy. The average of closest two measures are used for analysis. Child diet and child physical activity are measured using survey questions developed by CDC and implemented in the Infant Feeding Practices II study.36 Parent diet is measured using survey questions validated by the Southern Community Cohort Study and implemented by our study team in previous investigations of parent diet and weight-related behaviors.27 Parent physical activity is measured using the BRFSS module for physical activity. Additional up-stream determinants of childhood diet and physical activity are also measured (Table 1).
2.10.3. Survey Administration
Survey administration is conducted by guided-response, with a bi-lingual research assistant, in the participant’s native language. The survey takes 30-40 minutes to complete. Data are entered and stored in a secure REDCap database at the time of data collection.37
2.10.4. Process Measures
The COACH process measures included attendance, session fidelity, goals set in each of the intensive and maintenance phase sessions, and the extent to which participants self-identify their progress towards these goals. Certain members of the study team (but not follow-up data collectors) were unblinded to these process measures, as they were required for personalization of the intervention content.
A treatment fidelity plan included interventionist training and supervision, identification of essential treatment components, and use of fidelity measures with the goal of monitoring intervention delivery as intended. This process is consistent with the recommendations from the Treatment Fidelity Working Group of the NIH Behavior Change Consortium.38
2.10.5. Quality Assurance
For quality assurance, COACH uses a set of appropriate ranges for anthropometric measures, and branching logic for survey measures to ensure accuracy. Branching logic is embedded into the REDCap tool. During data entry, all survey and anthropometric variables are verified for completeness, and we attempt to collect any missing data within 48 hours of identifying its missingness. Before data collection, equipment is calibrated to ensure quality measurements. Also, the research coordinator conducts quality control checks on 10% of anthropometric measurements during data collection using predetermined thresholds for inaccuracy.
2.11. Qualitative Evaluation
To evaluate which aspects of the intervention are most effective, we will conduct focus groups with intervention participants who both respond (i.e., show healthy BMI trajectory) and do not respond to the intervention. Participants in the control group will be invited to participate, though in a separate session. These focus groups will be transcribed and coded by bilingual study staff. The standard qualitative analysis steps (data immersion, clustering of preliminary categories, editing, exploring new categories and subcategories, and identifying major themes) will be used.39,40 Qualitative analysis will occur in three interrelated phases: 1) individual quotes will be isolated in the transcripts; 2) a hierarchical coding system will be developed to organize the quotations in relationship to the study questions and to capture the full range and depth of participant response; and 3) the structure, frequency, and interrelationships of the coded quotes will be used to develop an integrative model of how to implement a healthy lifestyle program for families with young children. The process includes both inductive analysis (theory to fact) and deductive analysis (fact to theory). At least two independent reviewers will review each transcript line-by-line for patterns and themes.
2.12. Statistical Analysis
Our primary analysis will be an intent-to-treat analysis using a multilevel mixed-effects linear model, with time-varying child BMI (Level 1) following a quadratic growth trajectory and nested within children (Level 2). Time at Level 1 will be measured in months since baseline. The following child-level (Level 2) time-invariant variables will be predictors of the linear and quadratic components of the BMI growth rate and of the intercept at Level 1: age at baseline (centered at a value of interest) and random assignment to intervention or control. Child gender will be a child-level (Level 2), time-invariant predictor of the intercept at Level 1, but not of the growth rates.
The mixed-effects approach allows the estimation of growth rates using each child's age at baseline and individual measurement dates, while also allowing for different numbers of measurements per child in the case of missed data collections.23-25 To determine the statistical significance of the covariate-adjusted association between intervention assignment and child BMI trajectory, we will conduct a likelihood ratio test with two degrees of freedom to test whether the linear and quadratic intervention effects are jointly equal to zero. We will use a similar approach for the secondary outcomes.
One of the goals of this intervention is to determine which aspects of the intervention work best and for whom. As such, we will conduct a secondary analysis to evaluate the association between several metrics of intervention participation and changes in BMI at the 1-year follow-up. In particular, we will evaluate attendance at face-to-face sessions, completion of phone coaching calls, and progress made on weekly goals set in the intervention. We will also predict each of these metrics using sociodemographics collected at baseline.
2.12.1. Power Calculation
Our enrolled sample size of 117 participants, accounting for ~20% attrition, would result in 100 families in the final analysis. This would provide approximately 80% power to detect an effect size of 0.4 with a two-tailed Type I error rate of 5%. This is between “small” (d=0.2) and “medium” (d=0.5) by traditional criteria,41 and consistent with our previous findings regarding the effect size of a behavioral intervention on childhood weight trajectory.14 Recent work has identified that relatively small changes in weight are necessary to normalize weight trajectory over 1 year, indicating our follow-up time is sufficient to detect clinically relevant metrics.42
2.13. Participant safety
The participants are assessed for adverse events both actively (at each data collection time point) and passively (we encourage participants to tell their interventionists or callers at any time of an adverse event). The investigators follow a pre-specified protocol for evaluating whether an adverse event is related to, potentially related to, or not related to the study. Adverse events are monitored in real-time by the study coordinator and principal investigator.
3. Discussion
The COACH trial of a personalized behavioral intervention to prevent and treat childhood obesity among Latino parent-child pairs advances the field of study on childhood obesity prevention and treatment in several ways. A distinctive feature of COACH is the trans-disciplinary nature of the intervention—bringing together both theory and best-practices from the learning sciences and health behavior change. The intervention is adapted for each individual based on their pre-existing competency and stated goals. In addition, the goal of this study is to facilitate a person’s agency to navigate the complex systems necessary to engage in sustainable health behavior change for their family. The study moves past short-term intervention, with 1-year follow-up to gauge sustainability of health-behavior changes. In addition, the study is conducted in the participant’s built environment using public recreation centers, to facilitate ongoing and easy access to physical activity resources.
4. Conclusion
Applying a personalized approach to childhood obesity prevention has the potential to improve the sustainability of health behavior change. Developing strategies to prevent the long-term complications of obesity deserves continued investigation with well-developed randomized trials as described here. Forthcoming results from this trial will indicate whether a personalized behavioral intervention can have significant and sustainable effects on health behavior and BMI trajectories of Latino children at high risk of obesity.
Acknowledgements
This study is supported by Award Number K23 HL127104 from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung and Blood Institute or the National Institutes of Health. The REDCap database is supported by NCATS/NIH grant number: UL1TR000445.
Funding:
This study was funded by a K23 grant from the NHLBI (K23 HL127104).
Footnotes
Conflict of Interest Statement
None of the authors have any conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Heerman WJ, JaKa MM, Berge JM, et al. The dose of behavioral interventions to prevent and treat childhood obesity: a systematic review and meta-regression. The international journal of behavioral nutrition and physical activity 2017; 14(1): 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.JaKa MM, Haapala JL, Trapl ES, et al. Reporting of treatment fidelity in behavioural paediatric obesity intervention trials: a systematic review. Obesity reviews: an official journal of the International Association for the Study of Obesity 2016; 17(12): 1287–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011; (12): CD001871. [DOI] [PubMed] [Google Scholar]
- 4.Oude Luttikhuis H, Baur L, Jansen H, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev 2009; (1): CD001872. [DOI] [PubMed] [Google Scholar]
- 5.Boon CS, Clydesdale FM. A review of childhood and adolescent obesity interventions. Crit Rev Food Sci Nutr 2005; 45(7-8): 511–25. [DOI] [PubMed] [Google Scholar]
- 6.Young KM, Northern JJ, Lister KM, Drummond JA, O'Brien WH. A meta-analysis of family-behavioral weight-loss treatments for children. Clin Psychol Rev 2007; 27(2): 240–9. [DOI] [PubMed] [Google Scholar]
- 7.Seo DC, Sa J. A meta-analysis of obesity interventions among U.S. minority children. J Adolesc Health 2010; 46(4): 309–23. [DOI] [PubMed] [Google Scholar]
- 8.Stice E, Shaw H, Marti CN. A meta-analytic review of obesity prevention programs for children and adolescents: the skinny on interventions that work. Psychol Bull 2006; 132(5): 667–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang TT, Drewnosksi A, Kumanyika S, Glass TA. A systems-oriented multilevel framework for addressing obesity in the 21st century. Preventing chronic disease 2009; 6(3): A82. [PMC free article] [PubMed] [Google Scholar]
- 10.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity Among Adults and Youth: United States, 2015-2016. NCHS data brief 2017; (288): 1–8. [PubMed] [Google Scholar]
- 11.Bloom BS. Mastery learning In: Block JH, ed. Mastery learning: Theory and practice. New York: Hold, Rinehart & Winston; 1971: 47–63. [Google Scholar]
- 12.Po'e EK, Heerman WJ, Mistry RS, Barkin SL. Growing Right Onto Wellness (GROW): A family-centered, community-based obesity prevention randomized controlled trial for preschool child-parent pairs. Contemporary clinical trials 2013; 36(2): 436–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barkin S, Heerman WJ, Sommer EC, et al. Effect of a behavioral intervention for underserved preschool-age children on change in body mass index: a randomized clinical trial. JAMA : the journal of the American Medical Association 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barkin SL, Gesell SB, Po'e EK, Escarfuller J, Tempesti T. Culturally tailored, family-centered, behavioral obesity intervention for Latino-American preschool-aged children. Pediatrics 2012; 130(3): 445–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ogden CL, Carroll MD, Lawman HG, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988-1994 Through 2013-2014. JAMA : the journal of the American Medical Association 2016; 315(21): 2292–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teeters L, Singer-Gabella M, Jones S, Escarfuller J, Heerman WJ. Operationalizing Agency: A Personalized Approach to Public Health. International Journal of Community Research and Engagement 2018; 11(1). [Google Scholar]
- 17.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000; 55(1): 68–78. [DOI] [PubMed] [Google Scholar]
- 18.Bandura A Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 19.Bandura A Self-efficacy : the exercise of control New York: W.H. Freeman; 1997. [Google Scholar]
- 20.Guskey TR. Closing achievement gaps: revising Benjamin S. Bloom's "Learning for Mastery". Journal of Advanced Academics 2007; 19(1). [Google Scholar]
- 21.Jurow AS, Shea M. Learning in Equity-Oriented Scale-Making Projects. J Learn Sci 2015; 24(2): 286–307. [Google Scholar]
- 22.Heerman WJ, White RO, Barkin SL. Advancing Informed Consent for Vulnerable Populations. Pediatrics 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heerman WJ, White RO, Hotop A, et al. A Toolkit to Enhance the Informed Consent Process for Community-Engaged Pediatric Research. IRB: Ethics & Human Research 2016; 38(5). [PMC free article] [PubMed] [Google Scholar]
- 24.White RO, Thompson JR, Rothman RL, et al. A health literate approach to the prevention of childhood overweight and obesity. Patient Educ Couns 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Appel LJ, Clark JM, Yeh HC, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med 2011; 365(21): 1959–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ziegler P, Briefel R, Clusen N, Devaney B. Feeding Infants and Toddlers Study (FITS): development of the FITS survey in comparison to other dietary survey methods. Journal of the American Dietetic Association 2006; 106(1 Suppl 1): S12–27. [DOI] [PubMed] [Google Scholar]
- 27.Heerman WJ, Jackson N, Hargreaves M, et al. Clusters of Healthy and Unhealthy Eating Behaviors Are Associated With Body Mass Index Among Adults. Journal of nutrition education and behavior 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hughes SO, Anderson CB, Power TG, Micheli N, Jaramillo S, Nicklas TA. Measuring feeding in low-income African-American and Hispanic parents. Appetite 2006; 46(2): 215–23. [DOI] [PubMed] [Google Scholar]
- 29.O'Connor TM, Cerin E, Hughes SO, et al. Psychometrics of the preschooler physical activity parenting practices instrument among a Latino sample. The international journal of behavioral nutrition and physical activity 2014; 11: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ramírez MTG, Hernández RL. Factor Structure of the Perceived Stress Scale (PSS) in a Sample from Mexico. The Spanish Journal of Psychology 2007; 10(01): 199–206. [DOI] [PubMed] [Google Scholar]
- 31.Wright JA, Adams WG, Laforge RG, Berry D, Friedman RH. Assessing parental self-efficacy for obesity prevention related behaviors. The international journal of behavioral nutrition and physical activity 2014; 11: 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wardle J, Guthrie CA, Sanderson S, Rapoport L. Development of the Children's Eating Behaviour Questionnaire. J Child Psychol Psychiatry 2001; 42(7): 963–70. [DOI] [PubMed] [Google Scholar]
- 33.Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite 2001; 36(3): 201–10. [DOI] [PubMed] [Google Scholar]
- 34.Norris AE, Ford K, Bova CA. Psychometrics of a brief acculturation scale for Hispanics in a probability sample of urban Hispanic adolescents and young adults. Hispanic J Behav Sci 1996; 18(1): 29–38. [Google Scholar]
- 35.Mills SD, Malcarne VL, Fox RS, Sadler GR. Psychometric Evaluation of the Brief Acculturation Scale for Hispanics. Hisp J Behav Sci 2014; 36(2): 164–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fein SB, Labiner-Wolfe J, Shealy KR, Li R, Chen J, Grummer-Strawn LM. Infant Feeding Practices Study II: study methods. Pediatrics 2008; 122 Suppl 2: S28–35. [DOI] [PubMed] [Google Scholar]
- 37.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics 2009; 42(2): 377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bellg AJ, Borrelli B, Resnick B, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol 2004; 23(5): 443–51. [DOI] [PubMed] [Google Scholar]
- 39.Hickey G, Kipping C A multi-stage approach to the coding of data from open-ended questions Nurse Res 1996; 4: 81–91. [DOI] [PubMed] [Google Scholar]
- 40.LoBiondo-Wood G, Haber J. Nursing research: Methods and critical appraisal for evidence-based practice. 6th ed. St. Louis; 2006. [Google Scholar]
- 41.Cohen J Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, N.J.: L. Erlbaum Associates; 1988. [Google Scholar]
- 42.Goldschmidt AB, Wilfley DE, Paluch RA, Roemmich JN, Epstein LH. Indicated prevention of adult obesity: how much weight change is necessary for normalization of weight status in children? JAMA pediatrics 2013; 167(1): 21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]