Abstract
Objectives:
Catechol-O-methyltransferase (COMT), a key enzyme in degrading stress hormones, may influence susceptibility to delirium. Individuals with the COMT (rs4680) Val/Val genotype (designated “warriors”) withstand the onset of neuropsychiatric disorders and cognitive decline, while individuals with Met/Met and Val/Met genotypes (“non-warriors”) are more susceptible to these conditions. We evaluated whether COMT genotype modifies the established association between acute phase reactant (stress marker) C-reactive protein (CRP) and postoperative delirium.
Design:
Prospective cohort.
Setting:
Two academic medical centers.
Participants:
547 patients age ≥70 undergoing major non-cardiac surgery.
Measurements:
We collected blood, extracted DNA, and performed COMT genotyping using allele specific PCR assays, considering warriors vs. non-warriors. High plasma CRP, measured on postoperative day 2 (POD2) using ELISA, was defined by the highest sample-based quartile (≥234.12 mg/L). Delirium was determined using the Confusion Assessment Method, augmented by a validated chart review. We used generalized linear models adjusted for age, sex, and surgery type, stratified by COMT genotype, to determine whether the association between CRP and delirium differs by COMT.
Results:
Prevalence of COMT warriors was 26%, and postoperative delirium occurred in 23%. Among COMT warriors, high CRP was not associated with delirium (relative risk[RR] 1.0, 95% confidence interval[CI] 0.4–2.6). In contrast, among non-warriors, we found the expected relationship of high CRP and delirium (RR 1.5, 95% CI 1.1–2.2).
Conclusions:
COMT warriors may be protected against the increased risk of delirium associated with high POD2 CRP. With further confirmation, COMT genotype may help to target interventions for delirium prevention to the vulnerable non-warrior group.
Keywords: delirium, cathechol-O-methyltransferase, stress, reserve, C-reactive protein
INTRODUCTION
Delirium, an acute change in cognition, is a common, morbid, and costly condition that affects 25% of older adults undergoing major elective surgery, and up to 50% of older patients undergoing high-risk procedures (e.g., cardiac surgery and hip fracture repair).1 It has been associated with several adverse outcomes, including longer length of hospitalization,2 increased risk of cognitive and functional decline,3–5 and mortality.6,7
Although the basic epidemiology of postoperative delirium has been well-defined, its pathophysiology is less well understood. Recent work supports an inflammatory model of postoperative delirium, with mounting evidence of the involvement of C-reactive protein (CRP), a marker of inflammation and the stress response. Using an unbiased proteomics approach followed by enzyme-linked immunosorbent assay (ELISA) validation, we identified CRP as the most consistent and strongest protein associated with postoperative delirium both preoperatively (PREOP) and on postoperative day 2 (POD2).8 Since not all individuals with high inflammation develop delirium, other predisposing factors may be involved in delirium incidence. For instance, genetic factors may influence the permeability of the blood-brain barrier, or modify the effect of inflammation on the brain.
Catechol-O-methyltransferase (COMT), an enzyme that degrades catecholamines (stress hormones), is a key regulator of the stress response, with particularly strong influence on dopamine levels. The three COMT genotypes on the commonly examined single nucleotide polymorphism (SNP) rs4680 include: Val/Val, Val/Met, and Met/Met. Relative to persons with the Met/Met genotype, individuals with the Val/Val genotype have increased COMT activity, lower catecholamine levels (e.g., epinephrine, norepinephrine, and dopamine),9,10 and have been labeled ‘warriors’ given their ability to withstand the onset of adverse outcomes in the face of stress. In contrast, Met/Met genotypes have been termed ‘worriers’ (or non-warriors) due to their enhanced vulnerability to stress and general observed susceptibility to several adverse outcomes, including poor functioning on various domains of cognitive function, neuropsychiatric and motor system disorders (e.g., schizophrenia, depression, Parkinson’s disease). The Met/Met genotype has also been associated with increased susceptibility to the placebo effect.11
Since COMT has been associated with some brain disorders (e.g., schizophrenia) and moderates several relationships (described above), we considered whether COMT may also be important in delirium. Specifically, we hypothesized that COMT Val/Val genotype (warrior status) may be a marker of underlying brain reserve, and we used delirium as a model to examine this within the context of exposure to acute stress with increased capacity to withstand acute stress, in this case surgery. Within our theoretical model (see Figure 1), surgery is an acute stressor that may elicit a heightened stress response (high CRP) in some individuals, and postoperative delirium is an outcome of underlying brain reserve/vulnerability in the presence of heightened stress. Our study aims to examine the direct and indirect role of specific genetic factors and gene-protein interactions by studying (respectively): 1) the direct association between COMT status (warriors vs. non-warriors) and the incidence of postoperative delirium, and 2) whether COMT status modifies the previously reported association between CRP and delirium (Figure 1).
Figure 1.
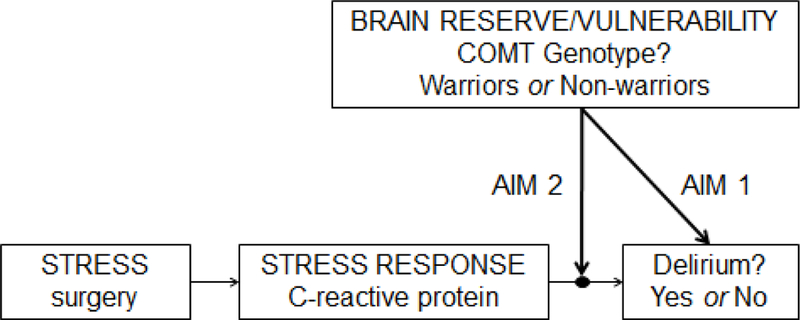
Theoretical Model for Study Aims
abbreviations: COMT=catechol-O-methyltransferase; COMT Warriors=Val/Val genotype; COMT Non-warriors=Met/Val or Met/Met genotypes
METHODS
Study Population
The Successful Aging after Elective Surgery (SAGES) study is an ongoing prospective cohort study focused on investigating risk factors and long-term outcomes of delirium. The SAGES study enrolled patients without dementia age ≥70 scheduled for major non-cardiac surgery (N=560), including orthopedic, vascular, or colectomy – under general or spinal anesthesia. Patients with dementia were excluded based on a detailed screening process, which culminated in a baseline neurocognitive battery (see12,13 for details). Informed consent for study participation was obtained from all subjects according to procedures approved by the institutional review boards of Beth Israel Deaconess Medical Center and Brigham and Woman’s Hospital, the two surgical sites, and Hebrew SeniorLife, the study coordinating center, all located in Boston, Massachusetts.
Specimen Collection
All patients underwent phlebotomy at 4 time points: PREOP, post-anesthesia care unit (PACU), POD2, and 1 month postop (PO1MO). Based on previous findings14 and our theoretical model (Figure 1), we focus on the POD2 time point for measurement of CRP (described below) to capture the stress response following surgery. For the POD2 time point, blood collection was incorporated into clinical blood draws taken on the surgical wards, and usually occurred in the morning between 6–8 AM. Mechanical disruption during phlebotomy was minimized to prevent hemolysis, and blood was stored on ice in heparinized tubes until processing. We used low-speed centrifugation (1500g for 15 minutes at 4°C) to separate plasma and cellular material, and plasma was stored at −80°C until analysis.
COMT.
Phlebotomy was performed on the entire cohort at baseline. To determine COMT genotype (rs4680), DNA was extracted from whole blood using a previously described technique (Ciulla et al., 1988), which yields high quantities of purified DNA of relatively high molecular weight that can be amplified using polymerase chain reaction (PCR) and restriction enzyme digestion. DNA was extracted, allele specific PCR assays were conducted in the Brigham Research Assay Core, and COMT genotyping was determined from the Partners Center for Personalized Medicine. The genotype frequencies were in Hardy-Weinberg equilibrium (χ2 = 2.45, df = 3, p ≈ 0.50). To consider the potential protective effects of the COMT Val/Val genotype (warriors) on postoperative delirium, our analysis compared COMT Val/Val (warriors) vs. COMT Val/Met or Met/Met (non-warriors), as examined in prior work15 and to maximize power.
CRP.
CRP on POD2 was measured in the entire SAGES sample using a high-sensitivity enzyme linked immunosorbent assay (ELISA) kit from R&D Systems, with all standards and samples run in duplicate (previously described8,14). Any specimens with a coefficient of variation (CV) >10% were repeated, and in the end all CVs were <5%. ELISA plates were read using a BioTek MX plate reader at Optical Density (OD) 450. A 4-parameter logistic curve was used with final calculations determined in an Excel template containing built-in macros for optimizing the best-fit model. Only community-based high-risk cutpoints for CRP have been identified to-date.16 Since these are not relevant for patients 2 days after major surgery, a cutpoint for ‘high’ CRP on POD2 (i.e., our definition of a heightened stress response) was defined as the highest quartile in our sample (i.e., 75th percentile: ≥234.12 mg/L). This was selected based on previous work indicating a nonlinear effect of CRP based on a categorical quartile scale; thus our use of a binary POD2 CRP variable remains consistent with previous publications.14
Delirium.
Postoperative delirium was determined from daily interviews during hospitalization, supplemented with a validated chart review method to pick up cases missed during the once-daily interview (e.g., delirious episodes that occurred only at night).17 All interviewers underwent training to conduct structured cognitive assessments of attention, orientation, and memory. Delirium was assessed using the Confusion Assessment Method (CAM) diagnostic algorithm, which required the patient to have an acute onset or fluctuating course of symptoms, inattention, and either disorganized thinking or altered level of consciousness.18 The presence of delirium by chart review was adjudicated by at least two delirium experts, and discordance was resolved through consensus conferences. Patients were considered delirious if delirium was present on either the CAM or the chart review method on any postoperative day; otherwise, patients were considered non-delirious.17,18
Covariates.
We examined covariates associated with COMT and postoperative delirium, including age, sex, surgery type, and race. Surgical procedures were classified into three types: 1) orthopedic (total knee replacement, total hip replacement, lumbar laminectomy, cervical laminectomy), 2) vascular (lower extremity bypass surgery; abdominal and thoracoabdominal aortic aneurysm repair [open procedure, not endovascular]), and 3) gastrointestinal (open or laparoscopic colectomy). Race was categorized as white or non-white.
Statistical Analysis.
We used generalized linear models with a log link and binomial error term to assess the association (unadjusted relative risks [RR]) between: 1) COMT warriors vs. non-warriors and postoperative delirium incidence, and 2) CRP and postoperative delirium, stratified by COMT warrior/non-warrior status. These associations were further examined by adjusting for age, sex, surgery type, and race (adjusted models). Notably, we did not adjust for baseline general cognitive performance (GCP), vascular comorbidity, or geriatric depression scale since these variables could potentially be on the causal pathway between COMT and postoperative delirium. All analyses were conducted using SAS Version 9.4, Cary N.C.
RESULTS
Table 1 reports the clinical characteristics of our study sample. On average, our sample consisted of older adults with mean age 76.7 years, who had a higher than US average preoperative GCP score. Slightly more than half of the sample was women (58%), and most underwent orthopedic surgery (81%), with fewer colectomies (6%) and vascular surgeries (13%). The clinical characteristics presented in Table 1 were generally similar in COMT warriors and non-warriors.
Table 1.
Clinical Characteristics of the Study Sample (N=547)
| Characteristic | Stratified by COMT status |
||
|---|---|---|---|
| Total | Val/Val (Warriors) | Val/Meta and Met/Met (Non-warriors) | |
| N=547 | N=145 | N=402 | |
| Age, M ± SD | 76.76 ± 5.2 | 75.8 ± 4.5 | 77.0 ± 5.3 |
| Female, N (%) | 317 (58) | 79 (55) | 238 (59) |
| Non-white, N (%) | 40 (7) | 15 (10) | 25 (6) |
| Surgery type, N (%) | |||
| Orthopedic | 444 (81) | 118 (81) | 326 (81) |
| Vascular | 33 (6) | 11 (8) | 22 (6) |
| Colectomy | 70 (13) | 16 (11) | 54 (13) |
| Preoperative GCP, M ± SD | 57.6 ± 7.3 | 58.0 ± 7.3 | 57.5 ± 7.3 |
| Vascular comorbidity, N (%) | 210 (38) | 55 (38) | 155 (39) |
| Geriatric Depression Scale, M ± SD | 2.5 ± 2.5 | 2.2 ± 2.6 | 2.5 ± 2.5 |
abbreviations: COMT=catechol-O-methyltransferase, GCP=general cognitive performance (externally scaled), M=mean, SD=standard deviation
Val/Met: N=289
Table 2 shows the incidence and relative risk (RR) of postoperative delirium among COMT warriors and non-warriors. Nineteen percent of COMT warriors developed delirium, and 25% of COMT non-warriors developed delirium (23% delirium rate in total sample). Thus, COMT warriors had a nonsignificant lower risk of postoperative delirium compared with COMT non-warriors.
Table 2.
Does COMT predict postoperative delirium? (N=547)
| Delirium | Unadjusted Model | Adjusted Modela | |
|---|---|---|---|
| COMT genotype | Incidence N(%) | RR(95% CI) | RR(95% CI) |
| Val/Val (warriors) (N=145) vs. | 27(19) | 0.7(0.5–1.1) | 0.8(0.5–1.1) |
| Met/Met or Met/Val (non-warriors) (N=402) | 100(25) |
abbreviations: CI=confidence interval, COMT=catechol-O-methyltransferase, RR=relative risk
Adjusted for age, sex, surgery type, and race
Table 3 shows the incidence and unadjusted RR of postoperative delirium among patients with POD2 CRP levels in Quartile [Q] 4 (≥234.12 mg/L) compared with those in Q1–3 (<234.12 mg/L) in the total sample and stratified by COMT warrior/non-warrior status. Consistent with previous findings, in the total sample, patients in the highest POD2 CRP quartile had higher delirium incidence relative to patients in Q1–3 for POD2 CRP (29% vs. 21%, respectively; relative risk [RR] 1.4, 95% confidence interval [CI] CI 1.0–1.9 [statistically significant]). In other words, patients in Q4 for POD2 CRP had a 40% increased risk of developing delirium.
Table 3.
Does CRP Predict Delirium: Effect Modification by COMT (Unadjusted Estimates)? (N=547)
| Entire Cohort (N=547) |
COMT Genotype |
|||||
|---|---|---|---|---|---|---|
| Val/Val (warriors, N=145) |
Met/Met or Met/Val (non-warriors, N=402) |
|||||
| CRP POD2 | Delirium N(%) | RR(95% CI) | Delirium N(%) | RR(95% CI) | Delirium N(%) | RR(95% CI) |
| Quartile 4 vs. | 40(29) | 1.4(1.0–1.9)a | 8(20) | 1.0(0.5–2.2) | 32(34) | 1.5(1.1–2.2) |
| Quartile 1–3 | 87(21) | 19(18) | 68(22) | |||
abbreviations: CI=confidence interval, COMT=catechol-O-methyltransferase, CRP=C-reactive protein, POD2=postoperative day 2, RR=relative risk
Sample-based quartiles of CRP: Quartiles 1–3 (<234.12 mg/L), Quartile 4 (≥234.12 mg/L)
All models are unadjusted (see Figure 2 for illustration of models adjusted for age, sex, and surgery type)
Statistically significant at p<.05
P for COMT genotype x CRP interaction = 0.40
After stratifying by COMT status, among the non-warriors, we observed a slightly greater (and significant) association between higher CRP and risk for postoperative delirium (RR [95% CI]: 1.5 [1.1–2.2]). However, there was no association between high CRP and delirium in COMT warriors (RR 1.0, 95% CI 0.5–2.2). The analytic models that adjusted for age, sex, surgery type, and race yielded very similar results (illustrated in Figure 2).
Figure 2.
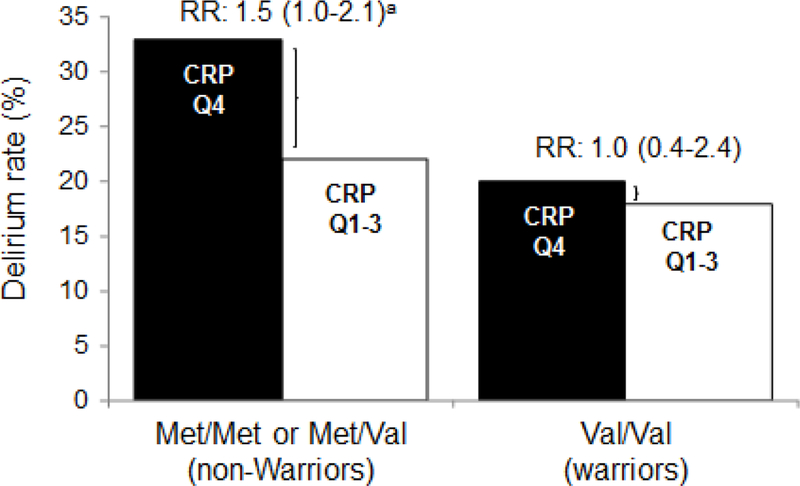
The Relationship between CRP and Delirium in COMT Warriors and Non-warriors (Adjusted Estimates) (N=547)
abbreviations: COMT=cathechol-O-methyltransferase, CRP=C-reactive protein, Q=Quartile, RR=relative risk (95% Confidence Interval)
All models adjusted for age, sex, surgery type, and race aStatistically significant at p<.05
P for COMT genotype x CRP interaction = 0.46
DISCUSSION
We examined the associations among COMT genotype, CRP, and postoperative delirium in older patients undergoing major elective surgery. We found a non-significant reduction in postoperative delirium in COMT warriors compared to non-warriors. In stratified analysis, however, we observed differences in the previously reported association between CRP and postoperative delirium by COMT genotype. COMT warriors appeared to be protected against the previously established increased risk of delirium associated with high POD2 CRP, while this lower susceptibility to delirium was not observed in non-warriors. This underscores the importance of examining gene-protein interactions in understanding the complex pathophysiology of postoperative delirium.
The absence of an association between COMT and postoperative delirium is consistent with one other study that examined this relationship.19 In the latter work, polymorphisms in three single nucleotide polymorphisms (SNPs) on the COMT gene (rs4680 [examined in the current study], rs4818, and rs6269) were not associated with the development of delirium in older adults admitted to a medical department or to a surgical department post hip fracture.19 We focused on only one SNP given its primary association with cognitive and neuropsychological vulnerability, and did find a modestly lower risk of delirium among COMT warriors, but this did not achieve statistical significance.
Importantly and distinct from previous work, our study examined the indirect effects of COMT by examining gene-protein interactions associated with postoperative delirium, an innovative approach to understanding delirium pathophysiology. More specifically, we explored the role of COMT genotype on delirium within the context of genetic predisposition as a brain reserve model under conditions of heightened stress. This model is particularly illuminating as it may provide a means to understand our current findings, as well as previous findings on COMT and delirium. Under conditions of acute stress (surgery) marked by a heightened stress response (high CRP on POD2), older patients with an enhanced reserve to stress (COMT warriors: Val/Val genotype) seem to be less susceptible to the increased risk of postoperative delirium. In comparison, older adults with a greater vulnerability to stress (COMT non-warriors: Met/Val and Met/Met genotypes) under these same conditions seem to be at increased risk of postoperative delirium. This indirect role of COMT has been previously observed in other settings, including clonidine treatment for chronic fatigue syndrome,20 the vitamin E and aspirin treatment effect on cardiovascular disease,11,21 and the effect of coffee intake on acute coronary events.22
Our study has a number of important strengths that underscore its innovation. SAGES represents one of the largest clinical studies of postoperative delirium to include information on blood-based proteins and genetic information, enabling consideration of both the direct effect of COMT on delirium and the indirect effect of COMT on the association between CRP and delirium. These strengths distinguish our study from previous work on COMT and delirium.19 Additional study strengths include our state-of-the-art measures of delirium and nearly complete capture of data on COMT genotype and CRP across the population (98%).
We acknowledge some study limitations. First, our use of a single measure of stress, CRP, may not fully capture the internal stress-related milieu after surgery. Nonetheless, we believe that the previous identification of CRP by our group and others8,14,23–25 as the protein most strongly and consistently associated with delirium supports our selection of CRP as a good, general marker of the stress response. Further planned work will consider the role of additional markers of the stress response once this data becomes available. Second, we acknowledge that we were likely underpowered to detect a significant COMT genotype x CRP interaction (see Table 3 and Figure 2 footnotes for p-for interaction values). However, the degree of effect modification by COMT on the relationship between CRP and delirium is of sufficient magnitude to be clinically significant, and suggests that our findings warrant further exploration in a larger sample. Third, we did not consider medication use in our analysis, as those data are not yet available for analysis in SAGES. Lastly, we acknowledge the limitations in generalizability of our results to the overall older patient population since this represents a surgical population free of dementia; however, the distribution of COMT genotypes in our population was similar to genotypes reported in general older patient populations.19 Ultimately, validation in a larger and more diverse patient sample is warranted.
In conclusion, although we observed only a small, non-significant direct association between COMT genotype and postoperative delirium, we found that the relationship between CRP and delirium differs by COMT genotype. Specifically, among COMT non-warriors, high CRP was associated with increased risk of delirium; however, no such relationship was observed in COMT warriors. In keeping with the brain reserve model, our findings support our hypothesis that COMT warriors seem to have a higher brain reserve relative to non-warriors and may be protected against the established increased risk of delirium associated with high POD2 CRP. Future studies should examine additional genetic modifiers of the stress response to determine whether other genes have a strong impact on the relationship between the stress response and postoperative delirium.
Acknowledgments
Source of Funding:
This research was supported by National Institute on Aging grants (P01AG031720 [SKI], R01AG051658 [ERM, TAL], R01AG041274 [ZX], R21AG048600 [ZX], R24AG054259 [SKI], K07AG041835 [SKI], K24AG035075 [ERM], K01AG057836 [SMV]), K01HL130625 [KTH]), the Charles A. King Trust Postdoctoral Research Fellowship Program, Bank of America, N.A., Co-Trustee [SMV], and the Alzheimer’s Association (AARF-18–560786 [SMV]). Dr. Inouye holds the Milton and Shirley F. Levy Family Chair. The authors gratefully acknowledge the contributions of the patients, family members, nurses, physicians, staff members, and members of the Executive Committee who participated in the Successful Aging after Elective Surgery (SAGES) Study.
Footnotes
Conflicts of Interest
The authors report no conflicts of interest.
Previous presentation: This work was presented during the American Delirium Society meeting in Nashville, TN (June 4–6, 2017).
REFERENCES
- 1.Marcantonio ER: Delirium in hospitalized older adults. N Engl J Med 2017; 377: 1456–1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rudolph JL, Jones RN, Rasmussen LS, Silverstein JH, Inouye SK, Marcantonio ER: Independent vascular and cognitive risk factors for postoperative delirium. Am J Med 2007; 120: 807–813. [DOI] [PubMed] [Google Scholar]
- 3.Koster S, Hensens AG, van der Palen J: The long-term cognitive and functional outcomes of postoperative delirium after cardiac surgery. Ann Thorac Surg 2009; 87: 1469–1474. [DOI] [PubMed] [Google Scholar]
- 4.Marcantonio ER, Flacker JM, Michaels M, Resnick NM: Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc 2000; 48: 618–624. [DOI] [PubMed] [Google Scholar]
- 5.Saczynski JS, Marcantonio ER, Quach L, et al. : Cognitive trajectories after postoperative delirium. N Engl J Med 2012; 367: 30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marcantonio ER, Goldman L, Mangione CM, et al. : A clinical prediction rule for delirium after elective noncardiac surgery. JAMA 1994; 271: 134–139. [PubMed] [Google Scholar]
- 7.Robinson TN, Raeburn CD, Tran ZV, Angles EM, Brenner LA, Moss M: Postoperative delirium in the elderly: risk factors and outcomes. Ann Surg 2009; 249: 173–178. [DOI] [PubMed] [Google Scholar]
- 8.Dillon ST, Vasunilashorn SM, Ngo L, et al. : Higher C-reactive protein levels predict postoperative delirium in older patients undergoing major elective surgery: A longitudinal nested case-control study. Biol Psychiatry 2017; 15: 145–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stein DJ, Newman TK, Savitz J, Ramesar R: Warrior versus worriers: The role of COMT gene variants. CNS Spectrums 2006; 11: 745–8. [DOI] [PubMed] [Google Scholar]
- 10.Ghimire LV, Kohli U, Li C, et al. : Catecholamine pathway gene variation is associated with norepinephrine and epinephrine concentrations at rest and after exercise. Pharmacogenet Genomics 2012; 22: 254–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall KT, Lembo AJ, Kirsch I, Ziogas DC, Douaiher J, Jensen KB: Catechol-O-methyltransferase val158met polymorphism predicts placebo effect in irritable bowel syndrome. PLoS One 2012; 7: e48135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmitt EM, Marcantonio ER, Alsop DC, et al. : Novel risk markers and long-term outcomes of delirium: The Successful Aging after Elective Surgery (SAGES) Study Design and Methods. J Am Med Dir Assoc 2012; 13: 818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmitt EM, Saczynski JS, Kosar CM, et al. : The Successful Aging after Elective Surgery Study: Cohort description and data quality procedures. J Am Geriatr Soc 2015;63:2463–2471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vasunilashorn SM, Dillon ST, Inouye SK, et al. : High C-reactive protein predicts delirium incidence, duration, and severity after major non-cardiac surgery. J Am Geriatr Soc 2017; 65: e109–e116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garcia-Fructuoso FJ, Lao-VIlladoniga JI, Beyer K, Santos C: Relationship between cathechol-O-methyltransferase genotypes and fibromyalgia’s severity. Reumatol Clin 2006; 2: 168–172. [DOI] [PubMed] [Google Scholar]
- 16.Ridker PM: High-sensitivity C-reactive protein and cardiovascular risk: Rationale for screening and primary prevention. Am J Cardiol 2003; 92: 17K–22K. [DOI] [PubMed] [Google Scholar]
- 17.Saczynski JS, Kosar CM, Xu G, et al. : A tale of two methods: Chart and interview methods for identifying delirium. J Am Geriatr Soc 2014; 62: 518–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI: Clarifying confusion: The Confusion Assessment Methods. A New method for detection of delirium. Ann Intern Med 1990; 113: 941–948. [DOI] [PubMed] [Google Scholar]
- 19.van Munster BC, Bass F, Tanck MW, de Rooij SEFJA: Polymorphisms in the catechol-O-methyltransferase gene and delirium in the elderly. Dement Geriatr Cogn Disord 2011; 31: 358–362. [DOI] [PubMed] [Google Scholar]
- 20.Hall KT, Kossowsky J, Oberlander TF, et al. : Genetic variation in catechol-O-methyltransferase modifies effects of clonidine treatment in chronic fatigue syndrome. Pharmacogenomics J 2016; 16: 454–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall KT, Nelson CP, Davis RB, et al. : Polymorphisms in catheol-O-methyltranferase modify treatment effects of aspirin on risk of cardiovascular disease. Arterioscler Thromb Vasc Biol 2014; 34: 2160–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Happonen P, Vaoutilainen S, Tuomainen T-P, Salonen J: Cathel-O-Methyltransferase Gene Polymorphism modifies the effect of coffee intake on incidence of acute coronary events. PLoS One 2006; 1: e117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pol RA, van Leeuwen BL, Izaks GJ, et al. : C-reactive protein predicts postoperative delirium following vascular surgery. Ann Vas Surg 2014; 28: 1923–1930. [DOI] [PubMed] [Google Scholar]
- 24.Ritchie CW, Newman TH, Leurent B, et al. : The association between C-reactive protein and delirium in 710 acute elderly hospital admissions. Int Psychogeriatr 2014; 26: 717–724. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Z, Pan L, Deng H, et al. : Prediction of delirium in critically ill patients with elevated C-reactive protein. J Crit Care 2014; 29: 88–92. [DOI] [PubMed] [Google Scholar]


