Abstract
Background.
Network analysis is an emerging approach in the study of psychopathology, yet few applications have been seen in eating disorders (EDs). Furthermore, little research exists regarding changes in network strength after interventions. Therefore the present study examined the network structures of ED and co-occurring depression and anxiety symptoms before and after treatment for EDs.
Method.
Participants from residential or partial hospital ED treatment programs (N=446) completed assessments upon admission and discharge. Networks were estimated using regularized Graphical Gaussian Models using 38 items from the Eating Disorders Examination-Questionnaire, Quick Inventory of Depressive Symptomatology, and State-Trait Anxiety Inventory.
Results.
ED symptoms with high centrality indices included desire to lose weight, guilt about eating, shape overvaluation, and wanting an empty stomach, while restlessness, self-esteem, lack of energy, and decision-making bridged ED to depression and anxiety symptoms. Comparisons between admission and discharge networks indicated the global network strength and importance of symptoms did not change significantly, though symptom severity decreased. Participants with denser networks at admission evidenced less change in ED symptomatology during treatment.
Conclusions.
Findings suggest that symptoms related to shape and weight concerns and guilt are central ED symptoms, while physical symptoms, self-esteem, and decision-making are links that may underlie comorbidities in EDs. Results provided some support for the validity of network approaches, in that admission networks conveyed prognostic information. However the lack of correspondence between symptom reduction and change in network strength indicates future research is needed to examine network dynamics in the context of intervention and relapse prevention.
Keywords: eating disorders, depression, anxiety, network analysis, treatment, classification
Network theory is an emerging approach that posits causal systems of interrelated symptoms are the “active ingredients” of disorders rather than effects of a latent entity (Borsboom, 2017; Borsboom & Cramer, 2013). Within this framework, edges refer to connections between symptoms (i.e., nodes), and disorders are conceptualized as patterns of dynamic relationships between symptoms, with greater connectivity conveying increased vulnerability for psychopathology (Scheffer et al., 2012). This approach differs fundamentally from latent variable models, and as such, offers unique advantages. That is, latent variable frameworks model shared variance among symptoms, with the assumption that an underlying common cause activates multiple symptoms and accounts for symptom covariation. In contrast, the focus of network models centers around estimating unique variance between symptoms. Despite the growing number of network analyses in other fields of psychopathology (for an overview see Fried et al., 2017), thus far few studies have examined the network structure of eating disorder (ED) symptoms, nor assessed the extent to which network structures change over the course of treatment.
Like other psychiatric disorders, EDs are serious illnesses that are associated with a range of negative correlates and sequelae, including significant co-occurring psychopathology (Klump et al., 2009). Mood and anxiety disorders represent the most common comorbid diagnoses in EDs (Hudson et al., 2007), which is consistent with a preponderance of research implicating negative affectivity in the onset and maintenance of EDs (e.g., Stice, 2001; Haedt-Matt & Keel, 2011; Wonderlich et al., 2015). Such evidence suggests ED and affective symptoms may have reciprocal and/or causal underlying relationships. Hence, identifying and understanding the complexities of relationships between ED and affective symptoms may allow prevention and intervention efforts to more precisely target key risk and maintenance mechanisms.
Network Analyses of EDs
Network analysis is a developing methodology in the study of EDs. Among adults with EDs, body-checking emerged as a central symptom, and feeling the need to exercise daily and items related to dietary restraint were identified as “key players”(Forbush et al., 2016). That is, key players refer to nodes that, when removed, fractures a network into smaller, more disconnected components; thus, this allows for the assessment of a node’s influence on network cohesion (Borgatti, 2006; Ortiz-Arroyo, 2010). In another network analysis of adults with bulimia nervosa (BN), fear of weight gain and overvaluation of shape and weight emerged as centrally important, while physical sensations bridged ED to depression and anxiety symptoms (Levinson et al., 2017). Most recently, DuBois and colleagues (2017) examined the network of a diagnostically heterogeneous sample of individuals with EDs and found that shape and weight overvaluation were central symptoms; furthermore, network connectivity was stronger among those with higher levels of overvaluation.
It is also worth noting that analytic techniques varied across these studies. Forbush et al. (2016) examined an association network in which the strength of connections between symptoms (i.e., edge weights) reflect zero-order correlations. In contrast, edge weights in the other networks (DuBois et al., 2017; Levinson et al., 2017) were partial correlation coefficients that control for all other symptoms, and were regularized using the graphical least absolute shrinkage and selection operator (glasso; Tibshirani, 1996; Friedman et al., 2008), which shrinks small edges to zero in order to estimate more parsimonious networks.
Treatment Outcome and Network Analysis
Network analysis can also be used to examine changes in symptom associations over time, and is thus well-suited to evaluate treatment targets and mechanisms of change. In theory, altering network structures may lead to reductions in symptom severity (Borsboom, 2017). Moreover, negative affect, specifically depression and anxiety, is related to severity and treatment outcomes across ED diagnoses and treatment types (e.g., Spindler & Milos, 2007; Vall & Wade, 2015). Therefore, it is possible that connectivity between ED, depression, and anxiety symptoms contributes to severity and maintenance of ED and co-occurring psychopathology; thus, identifying and targeting links between these symptoms may lead to reductions in connectivity, and allow for the development of more effective and efficient interventions.
Although a growing number of network studies have utilized ecological momentary assessment (EMA) to examine intra-individual temporal relationships (e.g., Bringmann et al., 2016; Fisher et al., 2017; Pe et al., 2015; Wichers et al., 2014), it is unclear the extent to which structural elements of networks convey prognostic information about individuals’ treatment outcome or course of illness over longer time periods, such as whether denser networks are more resistant to interventions given that highly connected symptoms are more prone to reciprocally activate and maintain each other. A study by Van Borkuko et al. (2015) compared network density of individuals with remitted and persistent depression, with results indicating that those with persistent depression evidenced a more densely connected network at baseline. Another study found increased connectivity in the network over the course of treatment, although symptom severity decreased (Beard et al., 2016). In sum, it is yet unclear if and how treatment is associated with changes in network density.
The Present Study
The present research sought to examine the network of ED, depression, and anxiety symptoms before and after treatment in a clinical sample of individuals with EDs. This builds upon prior cross-sectional network studies of ED symptoms (DuBois et al., 2017; Forbush et al., 2016) and the relationships between ED and affective symptoms (i.e., Levinson et al., 2017) by assessing changes in the global strength of networks over the course of treatment. There were three primary objectives of this study. First, we aimed to characterize the network structure of ED, depression, and anxiety symptoms at admission. These constructs were chosen given the preponderance of theoretical and empirical work implicating negative affect as a salient etiological and maintaining factor in EDs. Second, we assessed changes in global network strength at admission and discharge, and examined whether such changes corresponded to decreases in symptom severity. Given the tenets of network theory, we expected that network strength would decrease over the course of treatment. Third, we also assessed the validity of network theory by examining whether individuals with denser networks (i.e., higher global network strength) upon admission evidenced poorer outcomes. Evaluation of these aims may (1) lend further evidence regarding central ED and affective symptoms, and (2) provide novel information regarding the validity of network theory.
Method
Participants and Procedure
Participants were consecutively admitted patients in residential and partial hospitalization programs. All participants were diagnosed with an ED according to Diagnostic and Statistical Manual-IV-Text Revised (DSM-IV-TR) criteria (American Psychiatric Association, 2000) based on clinical interviews. Upon admission and discharge, participants completed self-report questionnaires. All participants provided informed consent for research. The initial sample consisted of 2,739 patients; the present study was limited to those who were at least 16 years oldand completed both admission and discharge assessments, resulting in a final sample of 446 participants from residential (n=204) or partial hospital programs (n=242).1 The sample was predominantly female (84.0%) and Caucasian (96.0%). Participants ranged in age from 16 to 64 (M=26.12, SD=10.12). The mean BMI of the sample was 22.27 (SD=7.71, Range: 13.25–76.02); the mean lengths of stay for residential and partial hospitalization patients were 56.68 days (SD=28.95) and 35.78 days (SD=22.99), respectively.2 Regarding ED diagnoses, 29.4% were diagnosed with anorexia nervosa restricting subtype (AN-r); 15.9% were diagnosed with anorexia nervosa binge-purge subtype (AN-bp); 28.0% were diagnosed with bulimia nervosa (BN); and 26.7% were diagnosed with eating disorder not otherwise specified (EDNOS). Of the individuals with EDNOS, 13.7% reported objective binge-eating episodes (OBEs) without purging behavior, 36.8% reported purging behavior in the absence of OBEs, and 23.1% reported both OBEs and purging. The remaining 26.5% denied both OBEs and purging. Additionally, a large proportion of the sample met criteria for mood (70.6%) and anxiety disorders (73.8%).
Measures
Each network included selected items from the Eating Disorder Examination Questionnaire version 4 (EDE-Q; Fairburn & Beglin, 1994), Quick Inventory of Depressive Symptomatology – Self-Report (QIDS-SR; Rush et al., 2003), and State-Trait Anxiety Inventory-Trait Subscale (STAI-T; Spielberger et al., 1983). Item abbreviations (Table 1) were used in figures.
Table 1.
Item abbreviations
| Abbreviation | EDE-Q item(s) |
|---|---|
| Restraint1 |
|
| Fast | Have you gone for long periods of time (8 hours or more) without eating anything in order to influence your shape weight? |
| Empty | Have you wanted your stomach to be empty? |
| FoodConc | Has thinking about food or its calorie content made it much more difficult to concentrate on thing you are interested in; for example, read, watch TV, or follow a conversation? |
| FearControl | Have you been afraid of losing control over eating? |
| Secret | Have you eaten in secret? (Do not count binges.) |
| Flat | Have you definitely wanted your stomach to be flat? |
| SpWtConc | Has thinking about shape or weight made it more difficult to concentrate on things you are interested in; for example read, watch TV, or follow a conversation? |
| FearGain | Have you had a definite fear that you might gain weight or become fat? |
| Fat | Have you felt fat? |
| Desire | Have you had a strong desire to lose weight? |
| Guilt | On what proportion of times that you have eaten have you felt guilty because the effect on your shape or weight? (Do not count binges.) |
| OBE | During how many of these episodes of overeating did you have a sense of having lost control over your eating? (Objective binge episode frequency) |
| SBE | Have you had other episodes of eating in which you have had a sense of having lost control and eaten too much, but have not eaten an unusually large amount of food given the circumstances? How many such episodes have you had over the past four weeks? (Subjective binge episode frequency) |
| Vomit | Over the past four weeks have you made yourself sick (vomit) as a means of controlling your shape or weight? How many such episodes have you had over the past four weeks? |
| Lax | Have you taken laxatives as a means of controlling your shape or weight? How many times have you done this over the past four weeks? |
| Exer | Have you exercised hard as a means of controlling your shape or weight? How many times have you done this over the past four weeks? |
| Overval1 |
|
| Dissatis1 |
|
| SelfWeigh | How much would it upset you if you had to weigh yourself once a week for the next four weeks? |
| OthersEat | How concerned have you been about other people seeing you eat? |
| DiscOwn | How uncomfortable have you felt seeing your body; for example, in the mirror, in shop window reflections, while undressing or taking a bath or shower? |
| DiscOthers | How uncomfortable have you felt about others seeing your body; for example, in communal changing rooms, when swimming or wearing tight clothes? |
| QIDS-SR item(s) | |
| Sleep1 |
|
| Sad | Feeling sad |
| Conc | (Difficulties with) concentration/decision-making |
| SelfEst | (Negative) view of myself |
| Suic | Thoughts of death or suicide |
| Anhed | (Lack of) general interest |
| Energy | (Low) energy level |
| Slowed | Feeling slowed down |
| Restless | Feeling restless |
| STAI-T item | |
| Nervous | I feel nervous and restless |
| Overwhelm | I feel that difficulties are piling up so that I cannot overcome them (overwhelmed) |
| Worry | I worry too much over something that really doesn’t matter |
| Decision | I make decisions easily |
| Intrusive | Some unimportant thought runs through my mind and bothers me (intrusive thoughts) |
| Ruminat | I get in a state of tension or turmoil as I think over my recent concerns and interests (rumination) |
Note. EDE-Q=Eating Disorder Examination-Questionnaire; QIDS-SR=Quick Inventory of Depressive Symptomatology Self-Report; STAI-T=State Trait Anxiety Inventory trait subscale.
Calculated as the mean of the specified items.
EDE-Q.
The EDE-Q is a 36-item measure of ED cognitions and behaviors over the previous 28 days. Most items range from 0 to 6, with higher scores signifying greater severity. The EDE-Q also assesses frequencies of ED behaviors (i.e., OBEs, self-induced vomiting, and laxative use). The EDE-Q Global score was used as an index of overall ED psychopathology.
QIDS-SR.
The QIDS-SR is a self-report measure of depressive symptoms over the previous week. Items are based on DSM criteria for depression and are rated from 0 to 3. Higher QIDS-SR total scores indicate greater depressive symptoms.
STAI-T.
The 20-item STAI Trait subscale assesses individuals’ general anxiety level. Items are rated on a 4-point scale ranging from 1 (almost never) to 4 (almost always); higher STAI-T total scores indicate higher levels of trait anxiety.
Statistical Analyses
Missing data were imputed with using multiple imputation based upon fully conditional Markov Chain Monte Carlo (MCMC) modeling (Schafer, 1987). A total of 10 separate imputation data sets were created.3 The final data set for network analysis was based on the average values of the 10 imputed data sets. The amount of missing data ranged from 0% to 4.7% at admission and 0% to 4.3% at discharge. Each network included 38 items from the EDE-Q, QIDS-SR, and STAI-T. Potential topological overlap was addressed by combining highly correlated variables that measured the same construct (Fried & Cramer, 2017). Based on prior research assessing the factor structure of the EDE-Q (Grilo, 2015), items related to dietary restraint (i.e., restraint over eating, food avoidance, and dietary rules), shape/weight overvaluation (i.e., importance of weight and shape), and body dissatisfaction (i.e., dissatisfaction with shape and weight) were combined into nodes labeled as “Restraint,” “Importance,” and “Dissatisfaction,” respectively. Four items on the QIDS that assess sleep disturbances were combined into one “Sleep” node.
Network estimation.
Gaussian graphical models (GGMs) were used to estimate network structures, in which edge weights reflect partial polychoric correlations (i.e., conditionally independent relationships) between nodes. GMMs were regularized using the glasso (Tibshirani, 1996; Friedman et al., 2008). Edges were displayed in the resulting figures for weights ≥ .05. To create the graphs, the Fruchterman-Reingold algorithm (Fruchterman & Reingold, 1991) was applied. Each network included 38 nodes and 703 edge weights.
Aim 1.
First we characterized the admission network structure by examining the relative importance of nodes using the following centrality measures: strength, closeness, and betweenness. Strength is the sum of all absolute connections to other nodes, thereby representing the overall involvement of a node in the network. Closeness is the inverse of the mean shortest connection to all other nodes in the network; high closeness indicates a short distance between a node and other nodes, and reflects more direct flow of information to a given node. Therefore, closeness accounts for both direct connections to other nodes as well as the importance within the global network structure. Betweenness is the number of times the node lies within the shortest path between two other nodes; consequently, betweenness measures the extent to which a node acts as a bridge within the network. All centrality measures were standardized in figures. We also examined bridge symptoms linking ED symptoms to depression and anxiety symptoms in the network structure at admission.
Aim 2.
We then assessed changes in global network strength between admission and discharge using an extension of the Network Comparison Test (NCT) that is appropriate for repeated measurements (Van Borkulo et al., 2017). The NCT is a two-tailed permutation test that can evaluate the difference in global network strength between two networks; a resulting p-value less than .05 indicates a significant difference in global strength (Van Borkulo, 2015).
Independent from the network analyses, we also evaluated the degree to which symptom severity decreased during treatment. A repeated measures multivariate analysis of variance (RM MANOVA) assessed the degree to which total scores for all three scales (i.e., EDE-Q, QIDS-SR, and STAI-T) decreased from admission to discharge. RM MANOVA analyses included length of stay (days) as a covariate.
Aim 3.
Lastly, we assessed the degree to which global network strength at admission is a prognostic indicator of treatment outcome. We examined whether participants who evidenced relatively worse outcomes had a more densely connected network structure at admission compared to those who evidenced relatively better outcomes. To do so we calculated the change in EDE-Q global score from admission to discharge for each participant; the sample was then divided into two groups based on the median value of EDE-Q global change scores. A between-groups NCT test was then conducted to compare the global network strength between these groups at admission and discharge assessments (van Borkulo et al., 2015). In addition, dependent NCTs were repeated to compare changes in network density between admission and discharge separately within each group.
Stability analyses.
Stability analyses were conducted with the bootnet R package (Epskamp et al., 2017). The accuracy of edge weights was examined using bootstrapped 95% confidence intervals (CI), with larger edge weight CIs being indicative of lower accuracy. The stability of centrality indices was assessed by correlations between centrality indices for the full sample and indices for networks sampled with progressively fewer cases. Lower correlations between original indices and those from subsamples suggest results are more prone to error. We also calculated the correlation stability coefficient (CS-coefficient), which indicates the maximum proportion of cases that can be dropped such that the correlation between original centrality indices and those from subsamples is .70 or higher (Epskamp et al., 2017). Epskamp and colleagues (2017) have suggested that the CS-coefficient should be at least .25, and preferably above .50. We also computed the edge weight and centrality difference tests for the admission network, which assess whether two edge weights or centrality indices significantly differ (Epskamp et al., 2017). Analyses were conducted using SPSS versions 22 and 25, R 3.3.2 (package qgraph 1.4.4; Epskamp et al., 2017).
Results
Stability analyses
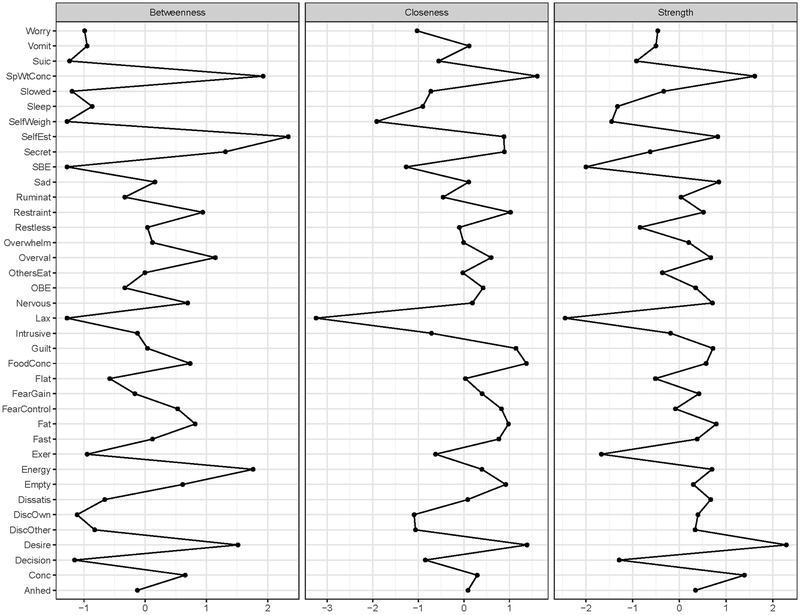
Stability analyses for the admission network are available as supplementary material. There were small to medium edge weight CIs. The CS-coefficients for strength, closeness, and betweenness were .67, .44, and .13, respectively; thus node strength was most stable.
Aim 1: Characterizing the admission network structure
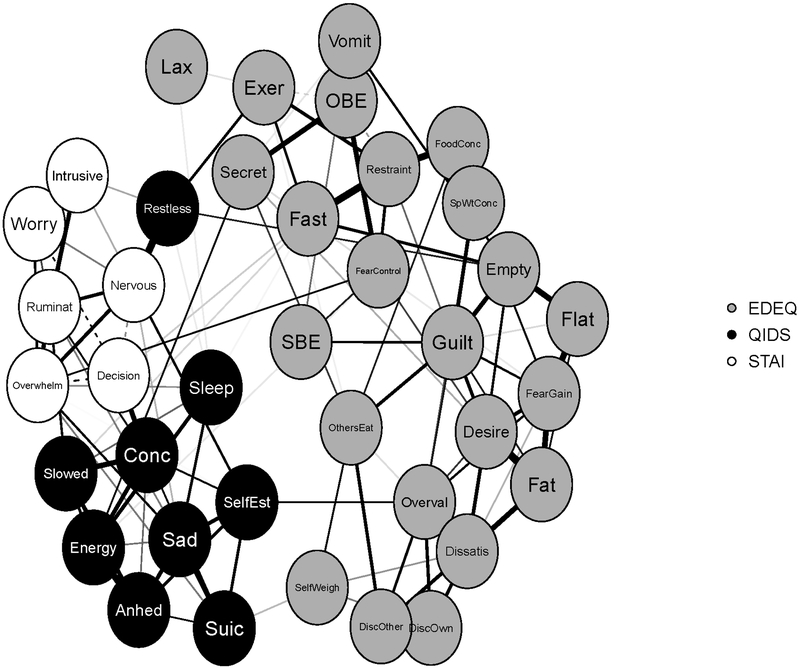
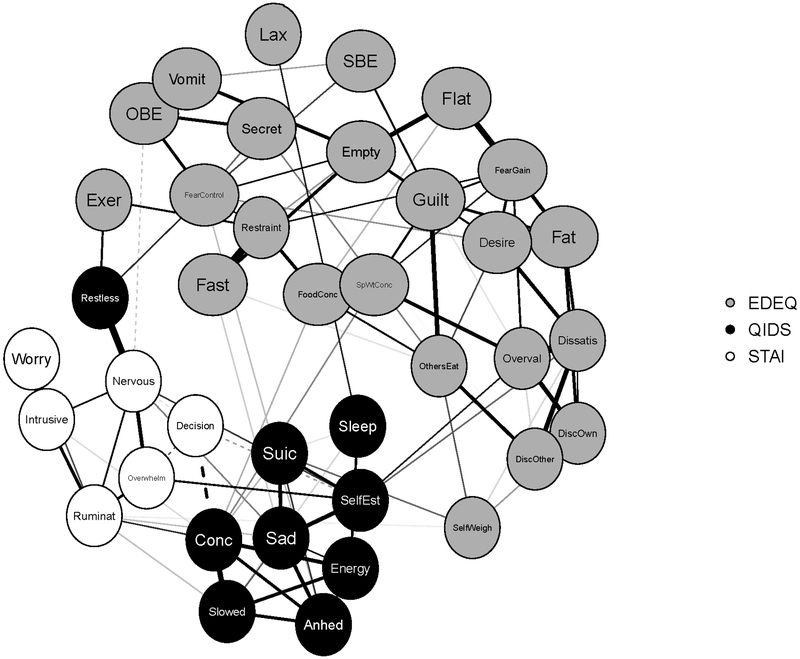
The network structure and standardized centrality indices at admission are displayed in Figures 1 and 2, respectively.4 Nodes with highest strength were shape and weight-related concentration difficulties (1.36), general concentration difficulties (1.22), guilt about eating (1.19), desire to lose weight (1.17), and nervousness (1.12). Nodes high in closeness included the desire for an empty stomach (1.48), fear of losing control over eating (1.44), dietary restraint (1.27), guilt about eating (1.17), and nervousness (.94). Nodes with highest betweenness were self-esteem (2.91), overvaluation of shape/weight (2.27), nervousness (1.68), desire for an empty stomach (1.30), and fear of losing control over eating (1.30). Restlessness served as a bridge from anxiety and depression symptoms to ED symptoms (i.e., exercise and wanting an empty stomach), and there were notable links between feeling overwhelmed and fear of losing control over eating, between lack of energy and eating in secret, and between self-esteem and overvaluation of shape/weight.
Figure 1.
Network structure of eating disorder, depression, and anxiety symptoms at admission (full sample). Solid edge=positive association; dashed edge=negative association.
Figure 2.
Centrality indices for the admission network of eating disorder, depression, and anxiety symptoms.
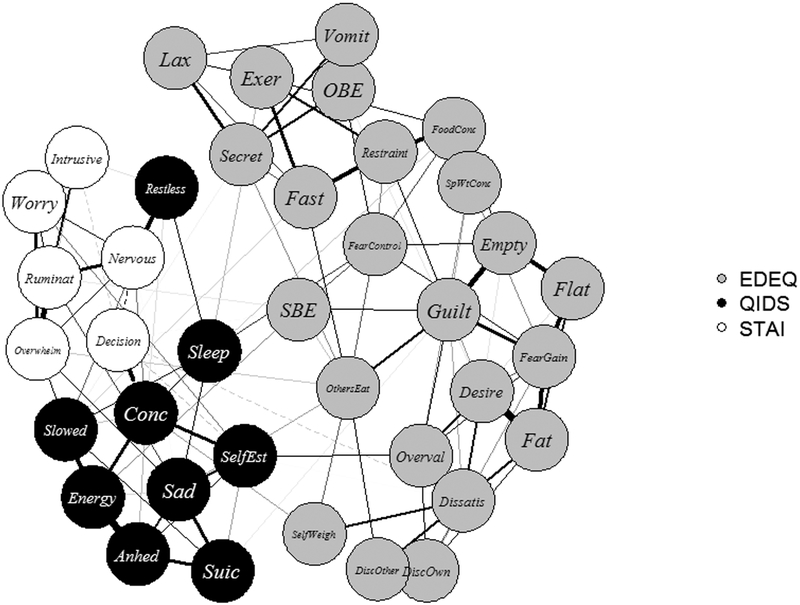
Aim 2: Comparison of global network strength between admission and discharge and correspondence with changes in symptom severity
The discharge network is shown in Figure 3. Results of the dependent NCT indicated that the global network strength did not change significantly between admission and discharge, p=.900. Conversely, RM MANOVA results indicated a significant effect of time across all measures, reflecting decreases in ED, depression, and anxiety symptoms, with medium to large effect sizes.5
Figure 3.
Network structure of eating disorder, depression, and anxiety symptoms at discharge (full sample). Solid edge=positive association; dashed edge=negative association.
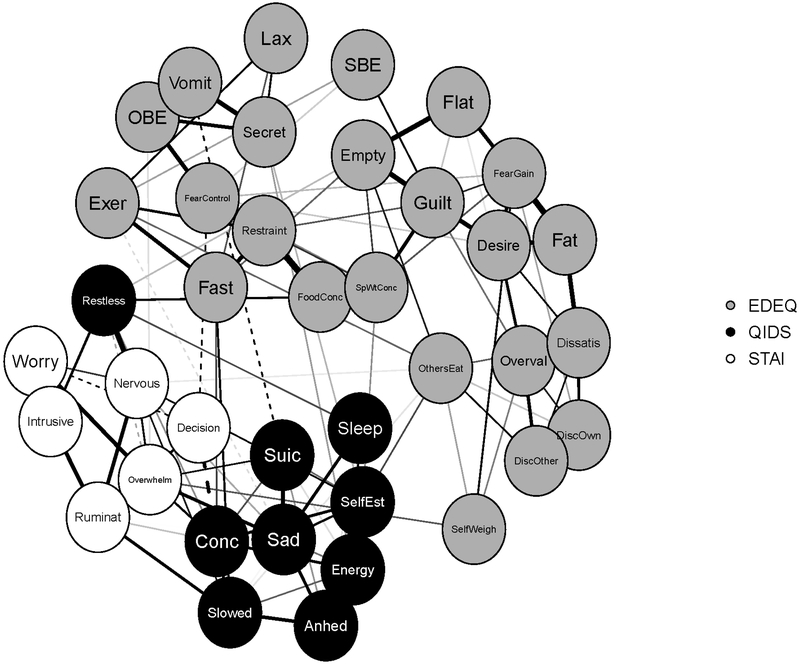
Aim 3: Assessment of the validity of admission networks
The admission networks for participants who evidenced less decrease in EDE-Q global scores during treatment (i.e., less improved group) and those who evidenced greater decreases in EDE-Q global scores (i.e., more improved group) based on the median split of changes in EDE-Q global scores are displayed in Figures 4 and 5, respectively. The between-group NCT comparing admission global network strength between groups was significant, p=.030, which indicated that the density of the admission network was greater among the less improved group compared to the more improved group. The same group differences were present in discharge networks, p<.001. Similar to the results for the entire sample, dependent NCTs within each group revealed no significant changes in global network strength over the course of treatment (more improved group: p=.500; less improved group: p=.860).
Figure 4.
Network structure of the less improved group admission. “Less improved” versus “more improved” groups were defined by the median split of decreases on the Eating Disorder Examination Questionnaire global scale. Solid edge=positive association; dashed edge=negative association.
Figure 5.
Network structure of the more improved group at admission. “Less improved” versus “more improved” groups were defined by the median split of decreases on the Eating Disorder Examination Questionnaire global scale. Solid edge=positive association; dashed edge=negative association.
Discussion
This the first network study to include prospective data in an ED sample. Findings identified centrally important ED and affective symptoms in the admission network structure, and despite decreases in the severity of these symptoms, the global network strength did not significantly change during treatment.
Aim 1: Central ED, depression, and anxiety symptoms
Guilt about eating, fear of losing control over eating, and shape- and weight-related concerns (i.e., desire to lose weight, desire to have an empty stomach, shape/weight overvaluation, and concentration difficulties due to shape/weight concerns) emerged as important ED symptoms. The findings regarding shape and weight-related concerns add to converging evidence for shape and weight concerns being core ED symptoms, which is consistent with a large body of theoretical and empirical work. In particular, the transdiagnostic cognitive behavioral model of EDs suggests overvaluation of eating, shape, and weight are core features of EDs and serve as dysfunctional schemes for evaluating one’s self-worth (Fairburn et al., 2003).
Several affective symptoms were identified as important nodes in the network. Emotion-related ED symptoms (i.e., guilt about eating and fear of losing control over eating) evidenced high centrality, which is notable in light of affect regulation theories and empirical studies indicating negative affect, particularly guilt, is an salient factor contributing to ED behaviors (e.g., Berg et al., 2013, 2015). In addition, several other negative affect symptoms demonstrated high centrality (i.e., nervousness, feeling overwhelmed, concentration difficulties, and low self-esteem), which suggests that targeting these symptoms may be particularly effective.
A number of bridges to ED symptoms were also identified, which may lend insight into symptom relationships underlying comorbid mood and anxiety psychopathology in EDs. The bridge between feeling overwhelmed and fear of losing control over eating, which in turn was related to OBE frequency, is also consistent with affect regulation models; it could be that individuals who feel overwhelmed have greater tendencies to regulate or escape from negative affect via binge eating. Thus, emotion-focused interventions that aim to help individuals cope adaptively with distress may be useful to weaken these network connections.
The bridge between self-esteem and shape/weight overvaluation provides further support that self-appraisals may contribute to both ED psychopathology and affective disturbances. For instance, the transdiagnostic cognitive behavioral model suggests low self-esteem is one possible maintaining mechanism of EDs (Fairburn et al., 2003). From another perspective, the theory underlying integrative cognitive affective therapy (ICAT) suggests that self-discrepancies (i.e., inconsistencies between one’s self view compared to one’s evaluative standards) may give rise to self-regulatory behaviors (e.g., self-criticism), which in turn promote negative affect and consequent ED psychopathology (Wonderlich et al., 2015). Regardless of the theoretical standpoint, these findings suggest that targeting the link between self-esteem and shape and weight concerns (e.g., modifying schemes of self-evaluation) may be effective in reducing ED and co-occurring depressive symptoms.
In addition, exercise frequency and desiring an empty stomach were related to restlessness, which in turn was associated with nervousness. These results are noteworthy in light of Levinson et al.’s (2017) finding that symptoms related to physical sensations bridged ED to anxiety and depression symptoms. Previous research has also indicated that drive for activity and restlessness are salient characteristics of AN (Casper, 2006; Scheurink et al., 2010) and that excessive exercise is related to anxiety and obsessive-compulsive symptoms in EDs (Holtkamp et al., 2004; Shroff et al., 2006). One possibility is that exercise serves to reduce anxiety among those with EDs (Holtkamp et al., 2004), and/or individuals with anxious temperament may experience restlessness and a stronger drive to exercise, especially in AN. This is also consistent with the close proximity of exercise frequency and restricting symptoms in the admission network.
Regarding the bridge between lack of energy and eating in secret, it may be that fatigue is related to decreased activity and social contact, which in turn may be related to a propensity to eat alone. Alternatively, some have suggested that fatigue is a marker of resource-depletion that limits capacity for self-regulation (Baumeister, 1998; Hagger et al., 2010) and could be a risk for binge-eating behavior (Loth et al., 2016); it is notable that eating in secret is a common feature of binge-eating episodes and was closely related to OBE frequency in the network. It may be that individuals who are fatigued are more prone to experiences lapses in self-control over eating, though further research is needed to test the directionality of this relationship.
Aims 2 and 3: Treatment outcome
Decreases in symptom severity during treatment did not correspond to changes in network connectivity. While the cause is not clear, and may be in part related to a lack of statistical power to detect meaningful change, these results are not inconsistent with those of Beard et al. (2016), and other research showing correlations between symptoms increase during treatment (Fried et al., 2016). A greater reduction in symptom severity and/or longer period of time could be necessary to change global network strength. Alternatively, it is possible that the treatment administered in these programs, while successful in dampening overall symptom severity, was not effective in targeting key symptom relationships maintaining ED psychopathology (i.e., network edges). If this was the case, participants may be vulnerable to relapse, though the lack of follow-up data in the present study precludes examination of this question. Therefore, additional research is needed to test whether changes in network structure are associated with better outcomes and lower rates of relapse. However, results indicated that those who evidenced less improvement had more densely connected networks upon admission, which converges with findings of Van Borkuko et al. (2015) and provides some evidence in support of the validity of network approaches.
Limitations
There are several limitations to acknowledge. Participants were from partial hospitalization and residential treatment programs, so ED behaviors may have been less likely to occur in these controlled environments, which may prevent generalizability to other treatment settings. The sample was also predominantly female and Caucasian and was limited to individuals ages 16 and older; thus it is not clear to what extent results apply to other demographic groups. The lack of change in density could be due to the heterogeneous nature of the treatment offered in these programs. The treatments implemented were not standardized, and therefore we cannot make conclusions regarding the influence of treatment components. Although there were relatively little missing data in the present study, and missing values were handled via multiple imputation, it is also worth noting that it is currently unclear how to best deal with missing data in network analysis. While stability analyses were consistent with previous network analyses finding the highest stability for node strength (Beard et al., 2016; Epskamp et al., 2017), closeness and betweenness were less stable and should be interpreted with more caution. In addition, the nonsignificant NCT comparing admission and discharge network density should be interpreted cautiously as the ratio of parameters to participants in the present study (703:450) was likely underpowered to detect differences. Thus, it is imperative that future studies that aim to assess similar research questions utilize larger sample sizes. With respect to measures, the QIDS has not yet been examined in ED networks, which limits comparisons to existing ED networks including depressive symptoms. Additionally, the STAI has been criticized as a measure of primarily somatic symptoms and may not adequately discriminate between anxiety and depression symptoms (e.g., Bieling et al., 1998); thus, this measure may fail to capture all facets of anxiety, and may overlap with depressive symptomatology. Future research could also assess the networks of ED symptoms and other specific anxiety features (e.g., social anxiety) that are not captured by the STAI. It is also important to note that networks were based on single items from self-report questionnaires, and individuals were assessed at only two times. Future research may benefit from multimodal assessments, the inclusion of latent variables within networks, and the use of intensive longitudinal designs. Lastly, it is clearly not possible to characterize individuals at the outset of treatment based on future treatment outcomes, which limits the utility of the present results. However, these findings nevertheless suggest that an individual who has a denser network at admission may evidence a poorer prognosis, and highlight the need for future prospective, intra-individual network analyses in the context of treatment.
Conclusions and future directions
Despite these limitations, results have relevant clinical implications and highlight important avenues for future research. Increasing evidence suggests shape and weight concerns and facets of negative affect are core components of ED networks, which is consistent with a wealth of theoretical and empirical work. Throughout the network literature, many have discussed highly central symptoms as being particularly relevant and potent targets of interventions, such that targeting these domains could maximize reductions in psychopathology. Certainly, future research is needed to test the extent to which focused interventions targeting these domains are effective in disrupting network structures. However, it is imperative to note that central symptoms may be the most difficult to treat due to their high connectivity within the network, as activation of any number of other connected symptom could serve to re-activate and maintain the central symptom. Therefore, in the context of interventions, it is likely that clinicians need to not only target central symptoms but also identify and address key symptom chains and clusters in which central symptoms are embedded. Furthermore, it has yet to be determined whether highly central symptoms are the most impairing aspects of psychopathology networks. In the case of EDs, it may be that while cognitive symptoms such as shape and weight concerns are highly connected within the network structure, the related negative affectivity and maladaptive behavioral responses (e.g., binge eating) may be more disruptive to individuals’ functioning and quality of life. We also note that due to the cross-sectional nature of the present network structures, it is yet unclear the degree to which nodes with high centrality temporally influence other symptoms, or alternatively, whether such symptoms are the end result of other causal symptom chains.
Along this line, research is needed to examine the nature of changes driving the evolution of network structures and compare network dynamics across different ED diagnoses. Furthermore, adapting network approaches at the individual level may provide clinicians with more precise understanding of idiographic symptom relationships and allow for more tailored interventions. In conclusion, results build upon previous ED networks and demonstrate a clear need for continued research to explore how this approach can best inform ED research and clinical practice.
Supplementary Material
Acknowledgments
Financial support
This research was supported by the National Institute of Mental Health grant number T32 MH082761 (K.S. and T.M.).
Conflict of interest
None
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Those who completed admission assessments did not differ from those who did not complete discharge assessments in BMI, age, or severity of ED symptoms.
Length of stay was calculated as calendar days.
The complete syntax for these analyses are available as supplementary material.
Partial correlation matrices are available in supplementary material
See supplementary material for table with full RM MANOVA results.
References
- American Psychiatric Association (2000). DSM-IV-TR: Diagnostic and statistical manual of mental disorders, text revision. Washington, DC: American Psychiatric Association. [Google Scholar]
- Baumeister RF, Bratslavsky E, Muraven M, Tice DM (1998). Ego depletion: Is the active self a limited resource? Journal of Personality and Social Psychology 74, 1252–1265. [DOI] [PubMed] [Google Scholar]
- Beard C, Millner A. Forgeard M, Fried E, Hsu K, Treadway M, Leonard C, Kertz S, Bjorgvinsson T (2016). Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychological Medicine 46, 3359–3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bieling PJ, Antony MM, Swinson P (1998). The State--Trait Anxiety Inventory, Trait version: structure and content re-examined. Behaviour Research and Therapy, 36, 777–788. [DOI] [PubMed] [Google Scholar]
- Berg KC, Crosby RD, Cao L, Crow SJ, Engel SG, Wonderlich SA, Peterson CB (2015). Negative affect prior to and following overeating-only, loss of control eating-only, and binge eating episodes in obese adults. International Journal of Eating Disorders 48, 641–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KC, Crosby RD, Cao L, Peterson CB, Engel SG, Mitchell JE, Wonderlich SA (2013). Facets of negative affect prior to and following binge-only, purge-only, and binge/purge events in women with bulimia nervosa. Journal of Abnormal Psychology 122, 111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgatti SP (2006). Identifying sets of key players in a social network. Computational & Mathematical Organization Theory 12, 21–34. [Google Scholar]
- Borsboom D (2017). A network theory of mental disorders. World Psychiatry 16, 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Cramer AO (2013). Network analysis: an integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology 9, 91–121. [DOI] [PubMed] [Google Scholar]
- Bringmann LF, Pe ML, Vissers N, Ceulemans E, Borsboom D, Vanpaemel W, Tuerlinckx F, Kuppens P (2016). Assessing temporal emotion dynamics using networks. Assessment 23, 425–435. [DOI] [PubMed] [Google Scholar]
- Casper RC (2006). The drive for activity and restlessness in anorexia nervosa: potential pathways. Journal of Affective Disorders 92, 99–107. [DOI] [PubMed] [Google Scholar]
- DuBois RH, Rodgers RF, Franko DL, Eddy KT, Thomas JJ (2017). A network analysis investigation of the cognitive-behavioral theory of eating disorders. Behaviour Research and Therapy 97, 213–221. [DOI] [PubMed] [Google Scholar]
- Epskamp S, Borsboom D, Fried EI (2017). Estimating psychological networks and their accuracy: A tutorial paper Behavior Research Methods. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Costantini G, Haslbeck J, Cramer AO, Waldorp LJ, Schmittmann VD, Borsboom D (2017). Package qgraph (https://cran.r-project.org/web/packages/qgraph/qgraph.pdf).
- Fairburn CG, Beglin SJ (1994). Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders 16, 363–370. [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R (2003). Cognitive behaviour therapy for eating disorders: A transdiagnostic theory and treatment. Behaviour Research and Therapy 41, 509–528. [DOI] [PubMed] [Google Scholar]
- Fisher AJ, Reeves JW, Lawyer G, Medaglia JD, Rubel JA (2017). Exploring the idiographic dynamics of mood and anxiety via network analysis. Journal of Abnormal Psychology 126, 1044. [DOI] [PubMed] [Google Scholar]
- Forbes MK, Wright AG, Markon K, Krueger R (2017). Evidence that psychopathology symptom networks have limited replicability. Journal of Abnormal Psychology 126, 969–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbush KT, Siew C, Vitevitch M (2016). Application of network analysis to identify interactive systems of eating disorder psychopathology. Psychological Medicine 46, 2667–2677. [DOI] [PubMed] [Google Scholar]
- Fried EI, Cramer AO (2017). Moving forward: challenges and directions for psychopathological network theory and methodology. Perspectives on Psychological Science 12, 999–1020. [DOI] [PubMed] [Google Scholar]
- Fried EI, van Borkulo CD, Cramer AO, Boschloo L, Schoevers RA, Borsboom D (2017). Mental disorders as networks of problems: A review of recent insights. Social Psychiatry and Psychiatric Epidemiology 52, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI, van Borkulo CD, Epskamp S, Schoevers RA, Tuerlinckx F, Borsboom D (2016). Measuring depression over time… Or not? Lack of unidimensionality and longitudinal measurement invariance in four common rating scales of depression. Psychological Assessment 28, 1354–1367. [DOI] [PubMed] [Google Scholar]
- Friedman J, Hastie T, Tibshirani R (2008). Sparse inverse covariance estimation with the graphical lasso. Biostatistics 9, 432–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fruchterman TM, Reingold EM (1991). Graph drawing by force-directed placement. Software: Practice and Experience 21, 1129–1164. [Google Scholar]
- Grilo CM, Reas DL, Hopwood CJ, Crosby RD (2015). Factor structure and construct validity of the eating disorder examination-questionnaire in college students: Further support for a modified brief version. International Journal of Eating Disorders 48, 284–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haedt-Matt AA, Keel PK (2011). Revisiting the affect regulation model of binge eating: a meta-analysis of studies using ecological momentary assessment. Psychological Bulletin 137, 660–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagger MS, Wood C, Stiff C, Chatzisarantis NL (2010). Ego depletion and the strength model of self-control: A meta-analysis. Psychological Bulletin 136, 495–525. [DOI] [PubMed] [Google Scholar]
- Holtkamp K, Hebebrand J, Herpertz-Dahlmann B (2004). The contribution of anxiety and food restriction on physical activity levels in acute anorexia nervosa. International Journal of Eating Disorders 36, 163–171. [DOI] [PubMed] [Google Scholar]
- Klump KL, Bulik CM, Kaye WH, Treasure J, Tyson E (2009). Academy for eating disorders position paper: eating disorders are serious mental illnesses. International Journal of Eating Disorders 42, 97–103. [DOI] [PubMed] [Google Scholar]
- Levinson CA, Zerwas S, Calebs B, Forbush KT, Kordy H, Watson H, Hofmeier S, Levine M, Crosby RD, Peat C, Runfola CD (2017). The core symptoms of bulimia nervosa, anxiety, and depression: A network analysis. Journal of Abnormal Psychology 126, 340–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loth K, Goldschmidt AB, Wonderlich SA, Lavender JM, Neumark-Sztainer D, Vohs KD (2016). Could the resource depletion model of self-control help the field to better understand momentary processes that lead to binge eating? International Journal of Eating Disorders 49, 998–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz-Arroyo D (2010). Discovering sets of key players in social networks In Computational Social Network Analysis (pp. 27–47). Springer London. [Google Scholar]
- Pe ML, Kircanski K, Thompson RJ, Bringmann LF, Tuerlinckx F, Mestdagh M, Gotlib IH (2015) Emotion-network density in major depressive disorder. Clinical Psychological Science 3, 292–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Markowitz JC, Ninan PT, Kornstein S, Manber R, Thase ME (2003). The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry 54, 573–583. [DOI] [PubMed] [Google Scholar]
- Schafer JL (1987). Analysis of Incomplete Multivariate Data. Chapman & Hall: London. [Google Scholar]
- Scheffer M, Carpenter SR, Lenton TM, Bascompte J, Brock W, Dakos V, Van de Koppel J, Van de Leemput IA, Levin SA, Van Nes EH, Pascual M. (2012). Anticipating critical transitions. Science 338, 344–348. [DOI] [PubMed] [Google Scholar]
- Scheurink AJ, Boersma GJ, Nergardh R, Sodersten P (2010). Neurobiology of hyperactivity and reward: Agreeable restlessness in anorexia nervosa. Physiology & Behavior 100, 490–495. [DOI] [PubMed] [Google Scholar]
- Shroff H, Reba L, Thornton LM, Tozzi F, Klump KL, Berrettini WH, Brandt H, Crawford S, Crow S, Fichter MM, Goldman D (2006). Features associated with excessive exercise in women with eating disorders. International Journal of Eating disorders 39, 454–461. [DOI] [PubMed] [Google Scholar]
- Spielberger C, Gorsuch R, Lushene R, Vagg P, Jacobs G (1983), Manual for the state-trait anxiety inventory. Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Spindler A, Milos G (2007). Links between eating disorder symptom severity and psychiatric comorbidity. Eating Behaviors 8, 364–373. [DOI] [PubMed] [Google Scholar]
- Stice E (2001). A prospective test of the dual-pathway model of bulimic pathology: Mediating effects of dieting and negative affect. Journal of Abnormal Psychology 110, 124–135. [DOI] [PubMed] [Google Scholar]
- Tibshirani R (1996). Regression shrinkage and selection via the lasso. Journal of the Royal Statistical Society. Series B 58, 267–288. [Google Scholar]
- Wichers M (2014). The dynamic nature of depression: a new micro-level perspective of mental disorder that meets current challenges. Psychological Medicine 44, 1349–1360 [DOI] [PubMed] [Google Scholar]
- Vall E, Wade TD (2015). Predictors of treatment outcome in individuals with eating disorders: A systematic review and meta-analysis. International Journal of Eating Disorders 48, 946–971. [DOI] [PubMed] [Google Scholar]
- Van Borkulo C (2015). Network Comparison Test: Permutation-Based Test of Differences in Strength of Networks. Available from https://cran.r-project.org/web/packages/NetworkComparisonTest/NetworkComparisonTest.pdf
- Van Borkulo C, Boschloo L, Borsboom D, Penninx BW, Waldorp LJ, Schoevers RA (2015). Association of symptom network structure with the course of depression. JAMA Psychiatry 72, 1219–1226. [DOI] [PubMed] [Google Scholar]
- Van Borkulo C, Boschloo L, Kossakowski J, Tio P, Schoevers R, Borsboom D, Waldorp L (2017). Comparing network structures on three aspects: A permutation test. Manuscript submitted for publication, doi: 10.13140/RG.2.2.29455.38569 [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Peterson CB, Smith TL (2015). Integrative cognitive-affective therapy for bulimia nervosa: A treatment manual. Guilford Publications. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.