Abstract
Background:
This meta-analysis aimed to evaluate the efficiency and safety of the combined adductor canal block (ACB) with local infiltration anesthesia (LIA) versus LIA alone for pain control after total knee arthroplasty (TKA).
Methods:
We searched PubMed, Medline, Embase, Web of Science, the Cochrane Library and Google databases from inception to August 2017 to selected studies that comparing the combined ACB with LIA and LIA alone for pain control after TKA. Only randomized controlled trials (RCTs) were included. Outcomes included visual analogue scale (VAS) with rest or mobilization at 8 h, 24 h and 48 h, total morphine consumption at 6 h, 24 h and 48 h, distance walked at 24 h and 48 h and the length of hospital stay.
Results:
Seven randomized controlled trial (RCTs) were finally included in this meta-analysis. The present meta-analysis indicated that, compared with LIA alone, combined ACB with LIA was associated with a reduction of VAS with rest at 24 h and 48 h and VAS with mobilization at 24 h. Additionally, combined ACB with LIA was associated with an increase of the distance walked at 24 h and a reduction of the length of hospital stay.
Conclusion:
Combined ACB with LIA could significantly reduce pain scores and morphine consumption compared LIA alone after TKA. Further multimodal large sample RCTs are needed to identify the optimal drug of ACB and LIA.
Keywords: adductor canal block, local infiltration anesthesia, meta-analysis, total knee arthroplasty
1. Introduction
Total knee arthroplasty (TKA) has been shown as an efficacy operation in improving functional outcome and reliving pain for patients with knee osteoarthritis (OA) or rheumatoid arthritis (RA).[1,2] It has been estimated that TKA patients will reach 3.5 million by 2030.[3] However, appropriately 60% and 30% of patients experience severe pain and moderate pain respectively after TKA.[4] Various analgesia strategies have been implemented including patient-controlled anesthesia (PCA), local infiltration anesthesia (LIA), peripheral nerve block and epidural analgesia.[5,6]
Adductor canal block (ACB) is a new technique resulting in sensory blockade that can be easily visualized at the middle third of the thigh with use of ultrasonography.[7] It is a sufficient analgesic and gained popularity because of the small impact on the quadriceps muscle weakness. Thus, there was a low risk of postoperative falls. In addition, it could be implemented with a high success rate. LIA is considered an alternative choice for regional anesthesia.[8] The procedure can be performed without anaesthetists. Its simplicity and apparent safety gained popularity for pain control in orthopedic surgery. However, a short duration of action limits the clinical application. Therefore, combined ACB and peri-articular infiltration may improve and prolong analgesia. Whether the combined ACB and peri-articular infiltration provide superior analgesia compared peri-articular infiltration alone after TKA remains controversial.
Thus, we performed a meta-analysis from randomized controlled trial (RCTs) to evaluate the efficiency and safety of the combined ACB with LIA versus LIA alone for pain control after TKA.
2. Methods
This systematic review was reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines.[9]
3. Search strategy
We manually searched PubMed, Medline, Embase, Web of Science, the Cochrane Library and Google databases from inception to August 2017. The search strategies in Pubmed database was as follows: (((((((intra-articular infiltration) OR local infiltration) OR peri-articular infiltration) OR local infiltration analgesia)) AND ACB)) AND (((((“Arthroplasty, Replacement, Knee” [Mesh]) OR TKR) OR TKA) OR total knee replacement) OR total knee arthroplasty). This meta-analysis collected data from published articles and thus no ethic approval was necessary for this article.
4. Inclusion criteria and exclusion criteria
-
1.
Participants: Patients prepared for TKA.
-
2.
Interventions: The intervention group received the combined ACB and LIA for pain control after TKA.
-
3.
Comparisons: The control group received LIA alone for pain control after TKA.
-
4.
Outcomes: visual analogue scale (VAS) with rest or mobilization at 8 h, 24 h and 48 h, total morphine consumption at 6 h, 24 h and 48 h, distance walked at 24 h and 48 h and the length of hospital stay.
-
5.
Study design: RCTs were regarded as eligible in the study.
Non-RCTs, letters, editorial comments and combined ACB with LIA with other comparison were excluded in this meta-analysis.
5. Study selection
Articles would be excluded from the present meta-analysis for case reports, conference abstract or review articles. Two reviewers independently scanned the abstracts of the potential articles identified by the above searches. Subsequently, the full text of the studies that met the inclusion criteria was screened, and a final decision was made. A senior author had the final decision in any case of disagreement regarding which studies to include.
6. Date extraction
The included studies were examined by 2 investigators and key data were extracted including first author name, samples size, published year, baseline characteristics, intervention of each groups and other outcome parameters. The primary outcomes were VAS with rest or mobilization at 8 h, 24 h and 48 h, total morphine consumption at 6 h, 24 h and 48 h, distance walked at 24 h and 48 h and the length of hospital stay.
7. Outcome measures and statistical analysis
Continuous outcomes (VAS with rest or mobilization at 8 h, 24 h, and 48 h, total morphine consumption at 6 h, 24 h and 48 h, distance walked at 24 h and 48 h and the length of hospital stay) were expressed as the weighted mean differences (WMD) with 95% CI. Statistical significance was set at P < .05 to summarize the findings across the trials. Variables in the meta-analysis were calculated using Stata software, version 12.0 (Stata Corp., College Station, TX). Statistical heterogeneity was evaluated using the chi-square test and the I2 statistic. When there was no statistical evidence of heterogeneity (I2 < 50%, P > .1), a fixed-effects model was adopted; otherwise, a random-effects model was chosen. Publication bias was tested using funnel plots. Publication bias was visually assessed using funnel plots and was quantitatively assessed using the Begg test.
8. Results
8.1. Search results
In the initial search, a total of 386 studies were identified from the electronic databases (PubMed = 112, EMBASE = 108, Web of Science = 60, Cochrane Library = 50, Google database = 56). Then, all papers were input into Endnote X7 (Thomson Reuters Corp., USA) software for the removal of duplicate papers. A total of 308 papers were reviewed and 209 papers were removed according to the inclusion criteria at abstract and title levels. Additionally, 1 study was a duplicate publication so we only included the most recently published paper. Ultimately, 7 clinical studies with 596 patients (combined ACB with LIA group = 285, LIA group = 311) were included in the meta-analysis.[10–16] The flow diagram for the included studies can be seen in Figure 1.
Figure 1.
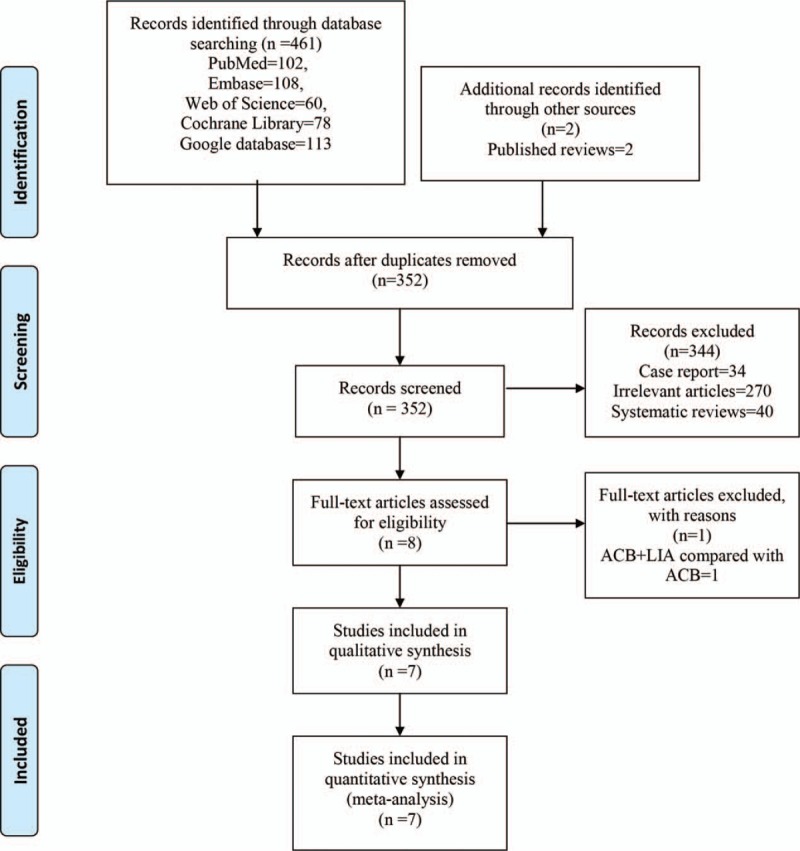
PRISMA flowchart for the included studies. PRISMA = preferred reporting items for systematic reviews and meta-analyses.
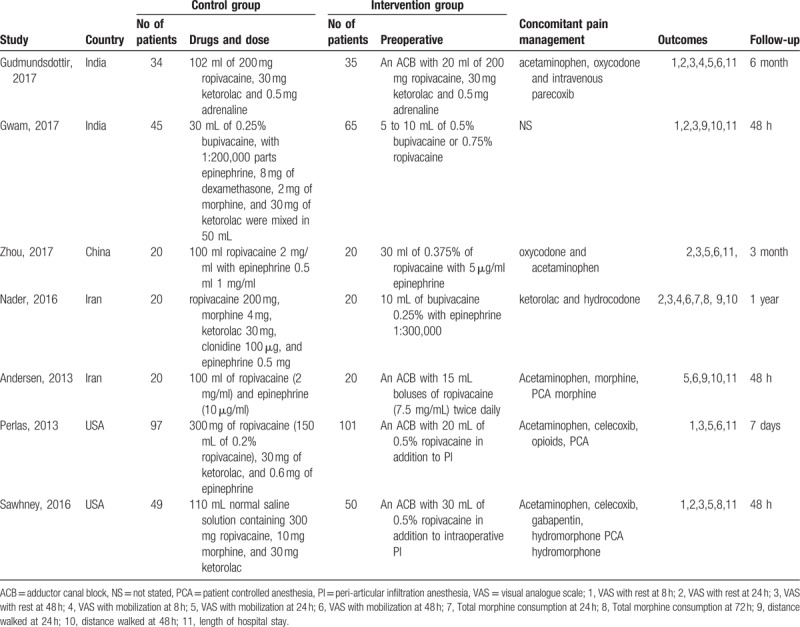
The sample of the included studies ranged from 20 to 101. The dose of ACB ranged from 10 ml to 30 ml. The drug for LIA included ropivacaine and bupivacaine. The follow-up ranged from 48 h to 6 months. The general characteristics of the included studies can be seen in Table 1.
Table 1.
The general characteristic of the included studies.
8.2. Quality assessment
The quality assessment of the included studies is summarized in Figures 2 and 3. All of the included studies describe the random sequence generation procedure; 2 studies did not describe the allocation concealment. Blinding of the participants and personnel were all with high risk of bias. Three studies did not describe the sample calculation and thus identified as unclear risk of bias. The overall kappa value regarding the evaluation of the risk of bias of included RCTs was 0.763, indicating that the agreement between the 2 reviewers was acceptable.
Figure 2.
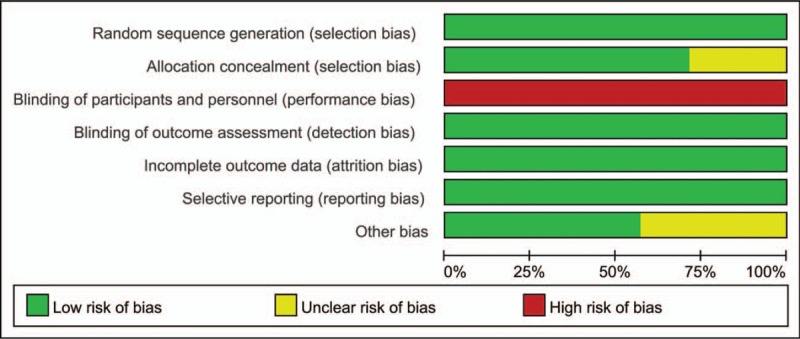
The risk of bias graph for the included studies.
Figure 3.
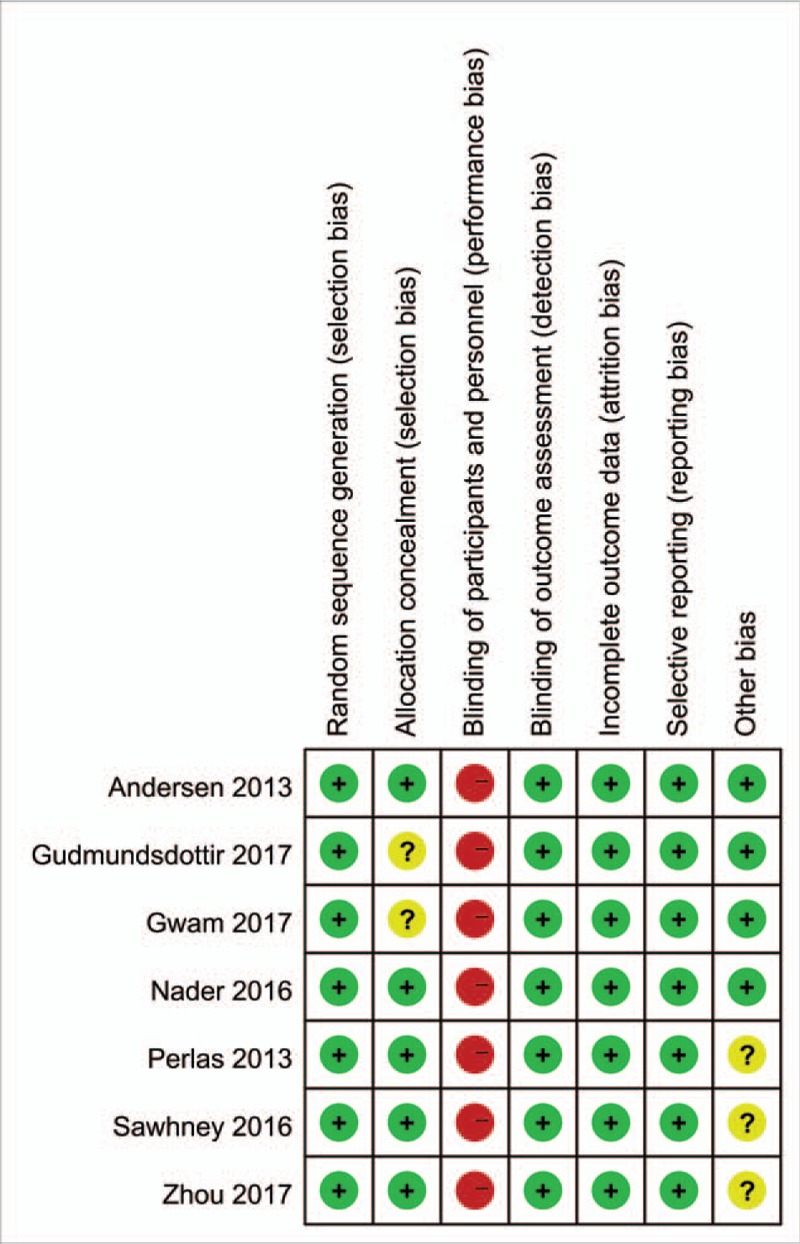
The risk of bias summary for the included studies.
9. Results of the meta-analysis
9.1. VAS with rest at 8 h, 24 h and 48 h
Postoperative VAS scores with rest at 8 h were reported in 5 studies,[10–12,14,15] and the pooled results indicated that combined ACB with LIA has no beneficial for reducing VAS scores with rest at 8 h (WMD = −4.63, 95% CI −16.07, 6.82, P = .428, Fig. 4).
Figure 4.
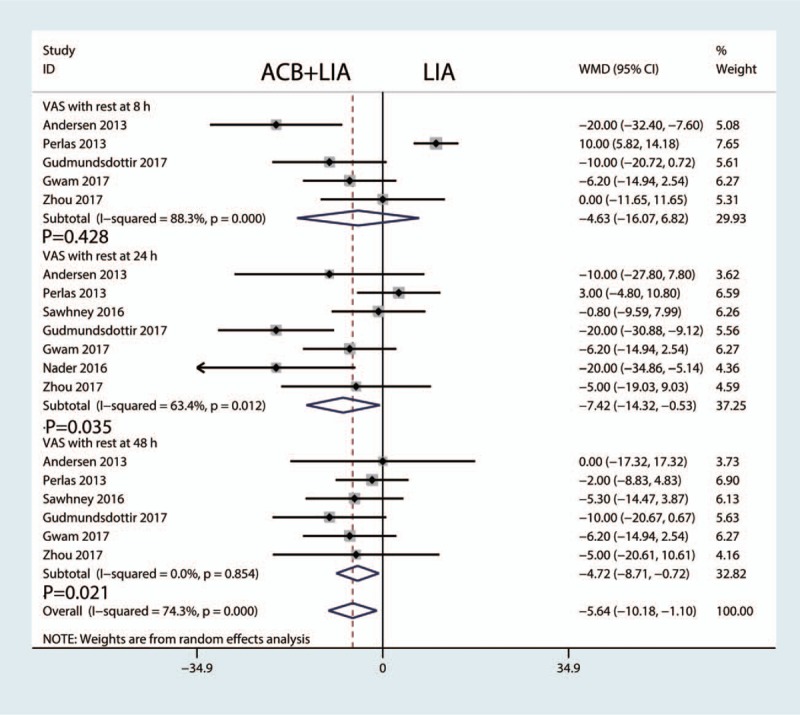
Forest plot comparing VAS scores with rest at 8 h, 24 h and 48 h. VAS = visual analogue scale.
Postoperative VAS scores with rest at 24 h were available in 7 studies.[10–16] The meta-analysis results indicated, compared with LIA alone, ACB combined with LIA was associated with a reduction of the VAS scores with rest at 24 h (WMD = −7.42, 95% CI −14.32, −0.53, P = .035, Fig. 4).
Postoperative VAS scores with rest at 24 h were available in 6 studies.[10–12,14–16] Pooled results indicated that, compared with LIA alone, combined ACB with LIA was associated with a reduction of VAS scores with rest at 48 h (WMD = −4.72, 95% CI −8.71, −0.72, P = .021, Fig. 4).
9.2. VAS with mobilization at 8 h, 24 h and 48 h
Pooled results indicated that there was no significant difference between the ACB combined LIA versus LIA alone in terms of the VAS scores with mobilization at 8 h, 24 h and 48 h (P = .769, P = .825 and P = .224 respectively, Fig. 5).
Figure 5.
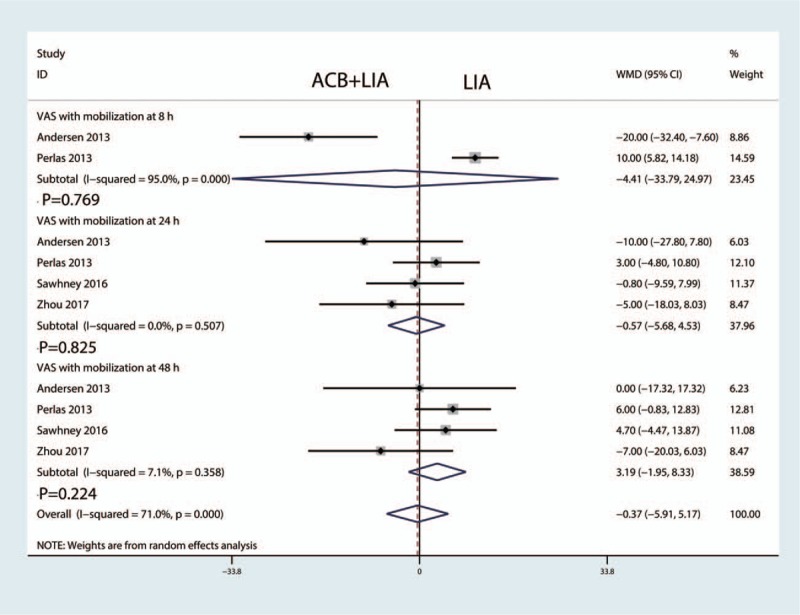
Forest plot comparing VAS scores with mobilization at 8 h, 24 h and 48 h. VAS = visual analogue scale.
9.3. Total morphine consumption at 6 h, 24 h and 48 h
Total morphine consumption at 6 h were reported in 3 studies,[10,14,15] and the pooled results indicated that combined ACB with LIA was associated with a reduction of total morphine consumption at 6 h than LIA alone group (WMD = −9.36, 95% CI −16.57, −2.15, P = .011, Fig. 6).
Figure 6.
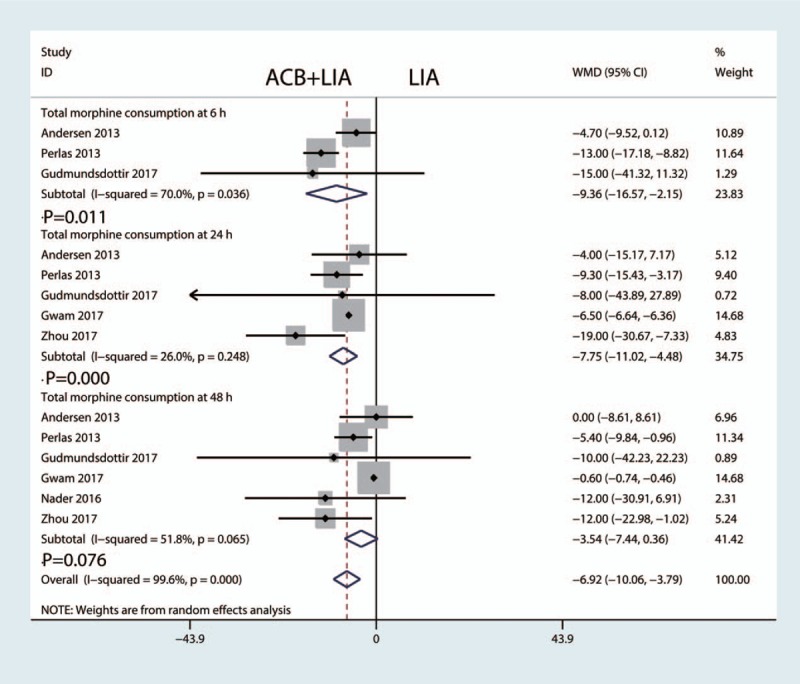
Forest plot comparing the total morphine consumption at 6 h, 24 h and 48 h.
Total morphine consumption at 24 h were available in 5 studies.[10–12,14,15] The meta-analysis results indicated, compared with LIA alone, ACB combined with LIA was associated with a reduction of the total morphine consumption at 24 h (WMD = −7.75, 95% CI −11.02, −4.48, P = .000, Fig. 6).
Total morphine consumption at 48 h were available in 6 studies.[10–12,14–16] Pooled results indicated that there was no significant difference between the total morphine consumption at 48 h between ACB combined LIA group and LIA alone group (WMD = −3.54, 95% CI −7.44, 0.36, P = 0.076, Fig. 6).
9.4. Distance walked at 24 h and 48 h
Distance walked at 24 h were reported in 3 studies,[13,15,16] and the pooled results indicated that combined ACB with LIA was associated with an increase of distance walked at 24 h than LIA alone group (WMD = 7.23, 95% CI 0.91, 13.56, P = .025, Fig. 7).
Figure 7.
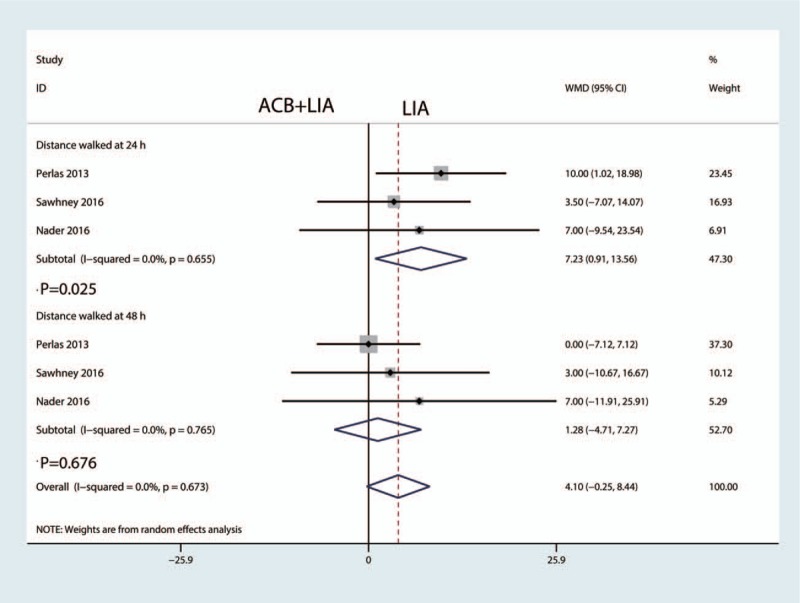
Forest plot of distance walked at 24 h and 48 h between the two groups.
Distance walked at 48 h were available in 3 studies.[13,15,16] The meta-analysis results indicated that there was no significant difference between the distance walked at 48 h between combined ACB with LIA group with LIA alone group (WMD = 1.28, 95% CI −4.71, 7.27, P = .676, Fig. 7) Figure 8.
Figure 8.
Forest plots comparing the length of hospital stay between the two groups.
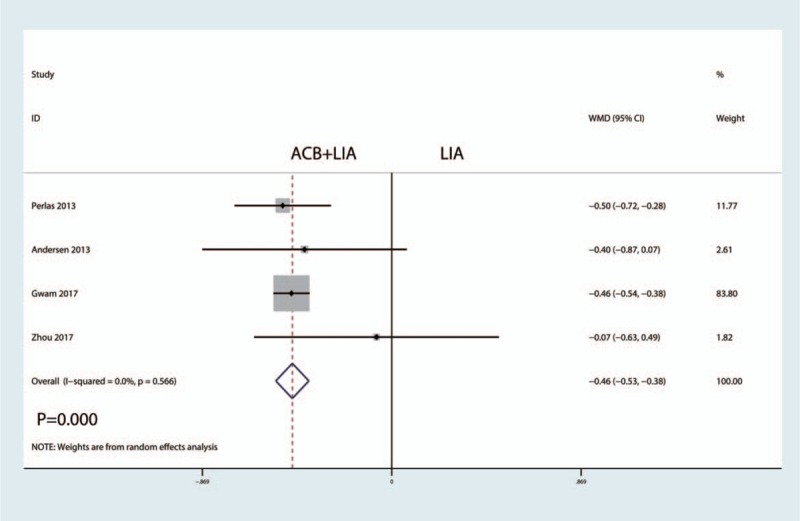
9.5. Length of hospital stay
Length of hospital were reported in 4 studies,[11,12,14,15] and the pooled results indicated that, compared with LIA alone, ACB combined with LIA was associated with a reduction of the length of hospital stay by 0.46 days (WMD = −0.46, 95% CI −0.53, −0.38, P = .000, Fig. 7).
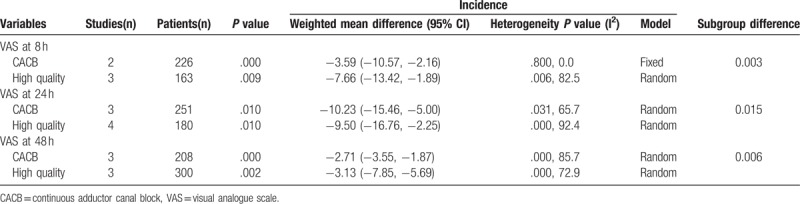
9.6. Subgroup analysis
We performed a subgroup analysis according to the quality of the studies and the continuous ACB. Results can be seen in Table 2. Final results indicated that combined ACB with LIA was associated with a reduction of VAS with rest at 8 h, 24 h and 48 h at any subgroup.
Table 2.
Subgroup analysis for the VAS with rest at 8 h, 24 h and 48 h.
10. Discussion
This systematic review and meta-analysis aimed to assess the effects of combined ACB with LIA versus LIA alone for pain control in patients following primary TKA. The final results indicated that treatment with combined ACB with LIA was associated with lower pain scores with rest at 24 h and 48 h postoperatively. In addition, combined ACB with LIA decreased the total morphine consumption at 6 h and 24 h and the length of hospital stay. After a comprehensive search of multiple electronic databases, a total of 7 studies were included in this meta-analysis. A major strength of the current meta-analysis was the statistical rigor with which the outcomes were calculated.
The pooled results indicated that ACB combined LIA was associated with a less pain scores at 24 h and 48 h after TKA, which was equivalent on a 110-point VAS to 7.42 points at 24 h and 4.72 points at 48 h. Ma et al[17] conducted a meta-analysis about the combined ACB with periarticular infiltration versus periarticular infiltration for analgesia after TKA. The results of their meta-analysis revealed that combined ACB with periarticular infiltration may not associate with a reduction in analgesia when compared to periarticular infiltration alone in the early postoperative period after TKA. With respect to VAS scores with mobilization at 8 h, 24 h and, 48 h, there was no significant difference between combined ACB with LIA and LIA alone group. However, Zhou et al [12] revealed that combined ACB with LIA was associated with a reduction of VAS with mobilization at 24 h and 48 h than LIA alone group.
Furthermore, combined ACB with LIA associated with a reduction of total morphine consumption at 6 h (WMD = −9.36, 95% CI −16.57, −2.15, P = .011) and 24 h (WMD = −7.75, 95% CI −11.02, −4.48, P = .000). Sawhney et al[16] found that the combination of ACB with LIA provided better pain relief and reduce total morphine consumption compared with LIA alone. Gudmundsdottir et al[10] indicated that no benefit of ACB added to a single-dose LIA compared with LIA alone on pain and total morphine consumption.
Additionally, combined ACB with LIA was associated with an increase of the distance walked at 24 h. Sawhney et al[16] suggested that when ACB is combined with LIA, analgesia is improved because of the ability to provide local anesthetic to the anterior, medial, lateral, and posterior aspects of the knee, potentially providing more complete analgesia compared with using LIA individually. Perlas et al[15] reported that combined ACB with LIA provided early ambulation and a higher incidence of home discharge.
There were a total of 5 limitations in the current meta-analysis: Only seven RCTs were included in the study, all of them were recently published, however, the sample size was relatively small; Postoperative knee functional is an important parameter, due to the insufficiency of relevant data, we cannot perform a meta-analysis; Methodological weakness in RCTs should be considered when analyzing the results; Duration of follow up is relatively short which leads to underestimate complications; Publication bias may existed due to the limited number of the included studies.
In conclusion, immediate analgesic efficacy and opioid-sparing effects were obtained with the administration of combined ACB with local infiltration analgesia in TKA patients. Additionally, ACB combined with local infiltration analgesia was associated with a reduction of the length of hospital stay. The number of the included studies and the quality of the studies were limited and thus need for more studies to identify.
Author contributions
Data curation: Aixiang Li.
Formal analysis: Aixiang Li.
Investigation: Yanan Li.
Software: Yanan Li.
Visualization: Yixuan Zhang.
Writing – original draft: Yixuan Zhang.
Footnotes
Abbreviations: CI = confidence interval, NNH = number needed to harm. NRS = numerical rating scale, PRISMA = preferred reporting items for systematic reviews and meta-analyses, RCTs = randomized controlled trials, RR = risk ratio, SD = standard deviation, VAS = visual analogue scale, WMD = weighted mean differences.
The authors report no conflicts of interest
References
- [1].Grant AE, Schwenk ES, Torjman MC, et al. Postoperative analgesia in patients undergoing primary or revision knee arthroplasty with adductor canal block. Anesth Pain Med 2017;7:e46695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Tang Y, Tang X, Wei Q, et al. Intrathecal morphine versus femoral nerve block for pain control after total knee arthroplasty: a meta-analysis. J Orthop Surg Res 2017;12:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780–5. [DOI] [PubMed] [Google Scholar]
- [4].Wang X, Sun Y, Wang L, et al. Femoral nerve block versus fascia iliaca block for pain control in total knee and hip arthroplasty: a meta-analysis from randomized controlled trials. Medicine 2017;96:e7382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Yue C, Wei R, Liu Y. Perioperative systemic steroid for rapid recovery in total knee and hip arthroplasty: a systematic review and meta-analysis of randomized trials. J Orthop Surg Res 2017;12:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Xing LZ, Li L, Zhang LJ. Can intravenous steroid administration reduce postoperative pain scores following total knee arthroplasty?: A meta-analysis. Medicine 2017;96:e7134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Dong CC, Dong SL, He FC. Comparison of adductor canal block and femoral nerve block for postoperative pain in total knee arthroplasty: A systematic review and meta-analysis. Medicine 2016;95:e2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Yan H, Cang J, Xue Z, et al. Comparison of local infiltration and epidural analgesia for postoperative pain control in total knee arthroplasty and total hip arthroplasty: a systematic review and meta-analysis. Bosn J Basic Med Sci 2016;16:239–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical research ed) 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Gudmundsdottir S, Franklin JL. Continuous adductor canal block added to local infiltration analgesia (LIA) after total knee arthroplasty has no additional benefits on pain and ambulation on postoperative day 1 and 2 compared with LIA alone. Acta Orthop 2017;88:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Gwam CU, Mistry JB, Richards IV, et al. Does addition of adductor canal blockade to multimodal periarticular analgesia improve discharge status, pain levels, opioid use, and length of stay after total knee arthroplasty? J Knee Surg 2017;31:184–8. [DOI] [PubMed] [Google Scholar]
- [12].Zhou M, Ding H, Ke J. Adductor canal block in combination with posterior capsular infiltration on the pain control after TKA. Ir J Med Sci 2017;187:465–71. [DOI] [PubMed] [Google Scholar]
- [13].Nader A, Kendall MC, Manning DW, et al. Single-dose adductor canal block with local infiltrative analgesia compared with local infiltrate analgesia after total knee arthroplasty: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med 2016;41:678–84. [DOI] [PubMed] [Google Scholar]
- [14].Andersen HL, Gyrn J, Moller L, et al. Continuous saphenous nerve block as supplement to single-dose local infiltration analgesia for postoperative pain management after total knee arthroplasty. Reg Anesth Pain Med 2013;38:106–11. [DOI] [PubMed] [Google Scholar]
- [15].Perlas A, Kirkham KR, Billing R, et al. The impact of analgesic modality on early ambulation following total knee arthroplasty. Reg Anesth Pain Med 2013;38:334–9. [DOI] [PubMed] [Google Scholar]
- [16].Sawhney M, Mehdian H, Kashin B, et al. Pain after unilateral total knee arthroplasty: a prospective randomized controlled trial examining the analgesic effectiveness of a combined adductor canal peripheral nerve block with periarticular infiltration versus adductor canal nerve block alone versus periarticular infiltration alone. Anesth Analg 2016;122:2040–6. [DOI] [PubMed] [Google Scholar]
- [17].Ma J, Gao F, Sun W, et al. Combined adductor canal block with periarticular infiltration versus periarticular infiltration for analgesia after total knee arthroplasty. Medicine 2016;95:e5701. [DOI] [PMC free article] [PubMed] [Google Scholar]


