Abstract
Background:
Preoperative neutrophil-lymphocyte ratio (NLR) and derived NLR (dNLR) have been suggested to be correlated with the prognosis of patients with breast cancer (BC). However, the results still remain controversial. Therefore, this study was to further evaluate the prognostic potential of preoperative NLR and dNLR for BC patients using a meta-analysis.
Methods:
Relevant articles were sought in PubMed and Cochrane Library databases up to September 2018. The associations between preoperative NLR/dNLR and overall survival (OS), disease-free survival (DFS) and recurrence-free survival (RFS) were assessed by the STATA software with the results presented as pooled hazard ratio (HR) with 95% confidence interval (CI).
Results:
Twenty-one studies were enrolled. Pooled results showed that elevated NLR was significantly associated with poorer OS (HR = 2.45, 95% CI: 1.69–3.54), DFS (HR = 1.54, 95% CI: 1.28–1.87) and RFS (HR = 4.05, 95% CI: 1.94–8.47) in BC patients undergoing surgery. High-preoperative dNLR was also significantly associated with worse OS (HR = 1.75, 95% CI: 1.39–2.19) and DFS (HR = 1.62, 95% CI: 1.09–2.41). Moreover, subgroup analysis showed significant associations between preoperative elevated NLR and poor prognosis were not changed by the stratification of ethnicity, cutoff of NLR, pathological stage, neoadjuvant, and adjuvant therapy.
Conclusion:
Preoperative NLR and dNLR may be effective predictive biomarkers for prognosis in patients with BC. Detection of NLR and dNLR may be helpful to identify the patients who may benefit from the surgery.
Keywords: breast cancer, derived neutrophil-lymphocyte ratio, meta-analysis, neutrophil-lymphocyte ratio, prognosis, surgery
1. Introduction
Breast cancer (BC) is one of the frequent malignancies and is the leading cause of cancer-related mortality in women, with an estimated 268,670 new cases and 41,400 deaths in the United States in 2018.[1] Surgery remains the gold standard for treatment of patients with BC. However, the prognosis remains unsatisfactory due to the recurrence and metastasis, with 5-year and 10-year survival rate of approximately 80% and 60%.[2] Also, there are several patients who are not reluctant to undergo surgical resection in clinic.[3] Therefore, it is essential to stratify the patients preoperatively and then the surgery is only strongly recommended for the patients with excellent prognostic outcomes.
Current studies have reported tumor size, pathologic tumor, node, metastasis (TNM) staging, Ki67 expression, receptor status (estrogen receptor, ER; progesterone receptor, PR; human epidermal growth factor receptor 2, HER2) and molecular subtypes (lumina-type, HER2-positive, and triple-negative) are significantly associated with the prognosis of patients with BC.[4–6] However, most of these factors are usually obtained under the requirement of core biopsies and with the aid of molecular technique, which is invasive and costly. Their prognostic accuracy is also reported to be unsatisfactory, with the example of the different TNM stage or molecular subtypes having the same prognoses.[7] Thus, more easily available and efficient preoperative prognostic parameters are desirable to guide individualized treatment.
Emerging evidence has demonstrated inflammation exerts important roles in the development and progression of cancer.[8,9] Moreover, blood-based tests for inflammatory factors are easy to perform, less expensive, and readily available. Thus, a serial of inflammatory immune cells (i.e., neutrophil, lymphocyte, white cells) and cytokines (i.e., C-reactive protein, interleukin 6 and tumor necrosis factor alpha) have been suggested as underlying prognostic biomarkers.[10] Of them, the ratio of absolute neutrophil count to absolute lymphocyte count (NLR) is the most commonly investigated indicator for assessment of the inflammatory status in patients with cancer.[11,12] A higher preoperative NLR is reported to be associated with poor survival in patients with BC.[13,14] However, some studies failed to find the correlation between the preoperative NLR and the overall survival (OS) of patients with BC.[15,16] Furthermore, in some clinical trials, only white cell and neutrophil counts are routinely detected and thus the derived NLR (dNLR) [defined as absolute neutrophil count divided by the derived lymphocyte count (absolute leukocyte count–neutrophil count)] was also used for NLR alternative. Also, it remains controversial on the prognostic role of dNLR for BC.[17,18] Hereby, the goal of this study was to further evaluate the prognostic potential of preoperative NLR and dNLR for BC patients using a meta-analysis.
2. Materials and methods
2.1. Search strategy
A systematic literature search was carried out independently by 2 investigators in PubMed and Cochrane Library databases for screening studies published to September 2018 that assessed the relationship between preoperative NLR and the prognosis of patients with BC. The search keywords included: “NLR” (or “neutrophil to lymphocyte ratio” or “neutrophil lymphocyte ratio” or “neutrophil-to-lymphocyte”) AND “breast cancer” AND “surgery” (or “resection”). In addition, the reference lists of all identified publications as well as pertinent reviews and meta-analyses were also manually screened to further obtain potentially eligible literatures. This analysis was performed in accordance to the Guidelines of the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA).[19] Ethics approval was not applicable as this is a meta-analytic study.
2.2. Selection criteria
Two investigators independently selected the relevant articles according to the inclusion criteria: BC was confirmed by pathological examination; NLR was measured by serum-based method preoperatively or at initial diagnosis (which was not influenced by neoadjuvant); prognostic outcomes [like OS, disease-free survival (DFS), recurrence-free survival (RFS) and disease specific survival (DSS)] were investigated; and hazard ratio (HR) with a 95% confidence interval (CI) could be directly obtained or indirectly estimated. Exclusion criteria were: duplicated literatures; abstracts, meta-analysis, reviews, letters, editorials, case reports, comments or non-clinical studies (animal experiments); HR and 95%CI were unavailable; NLR was measured after neoadjuvant or postoperatively; and literature written in language other than English.
2.3. Data extraction
Two reviewers independently extracted the following data: first author’ name, publication year, country of origin, sample size, study design, characteristics of patients (including age, stage, duration of follow-up), treatment strategies, treatment outcome, cut-off value of NLR and dNLR, HR with 95%CI for survival and related statistical methods. HR and 95%CI were extracted preferentially from multivariable analyses, otherwise from univariate analysis results.
Quality assessment was conducted using the Scottish Intercollegiate Guidelines Network (SIGN) checklists.[20] Good quality was presented as double plus (2++) which denoted cohort studies had very low risk of confounding, bias, or chance and a high probability that the relationship is causal; acceptable quality was presented as single plus (2+) which denoted cohort studies had a low risk of confounding, bias, or chance and a moderate probability that the relationship is causal; low quality was presented as a minus (2−) indicated cohort studies had high risk of confounding, bias, or chance and a significant risk that the relationship is not causal. Any disagreement in the data extraction and quality assessment was resolved by consensus.
2.4. Statistical analysis
Extracted data were pooled using the STATA software (version 13.0; STATA Corporation, College Station, TX). Statistical heterogeneity among the studies was assessed with Cochrane's Q (Chi-squared) and I2 statistic.[21] A random-effects model was used for heterogeneous studies (Q test P value < .10 and I2 > 50%); otherwise, the fixed-effects model was applied in the absence of heterogeneity. Publication bias was assessed with Egger's linear regression test and funnel plots.[22] The influence of publication bias on the overall effect was tested by the “trim and fill” method.[23] Sensitivity analysis was performed based on the leave-one-out approach. In addition, subgroup analyses were also performed for ethnicity, publication year, sample size, stage, follow-up time, cut-off, statistical methods, and adjuvant therapy. P < .05 was considered to be statistically significant.
3. Results
3.1. Study characteristics
Twenty-one studies[13,16–18,24–39] comprising a total of 10,599 patients were included according to the search strategy and the inclusion/exclusion criteria (Fig. 1). Of them, 20 studies[13,16,18,24–39] including 9837 participants were included for NLR and 3 studies,[4,17,31] including 2950 participants for dNLR. All studies collected data retrospectively. Twelve studies included only patients with early stage breast cancer (stage I–III), while 9 included both early and metastatic disease. Patients in most of the studies did not receive neoadjuvant (15/21, 71.4%), but a large proportion of them (90.5%) underwent adjuvant therapy (including chemotherapy, radiotherapy, and hormone therapy). The other characteristics of the included studies are shown in Table 1. Four studies were rated as SIGN level 2++, 11 were 2+ and 6 were 2−, suggesting most of our selected articles were of high quality.
Figure 1.
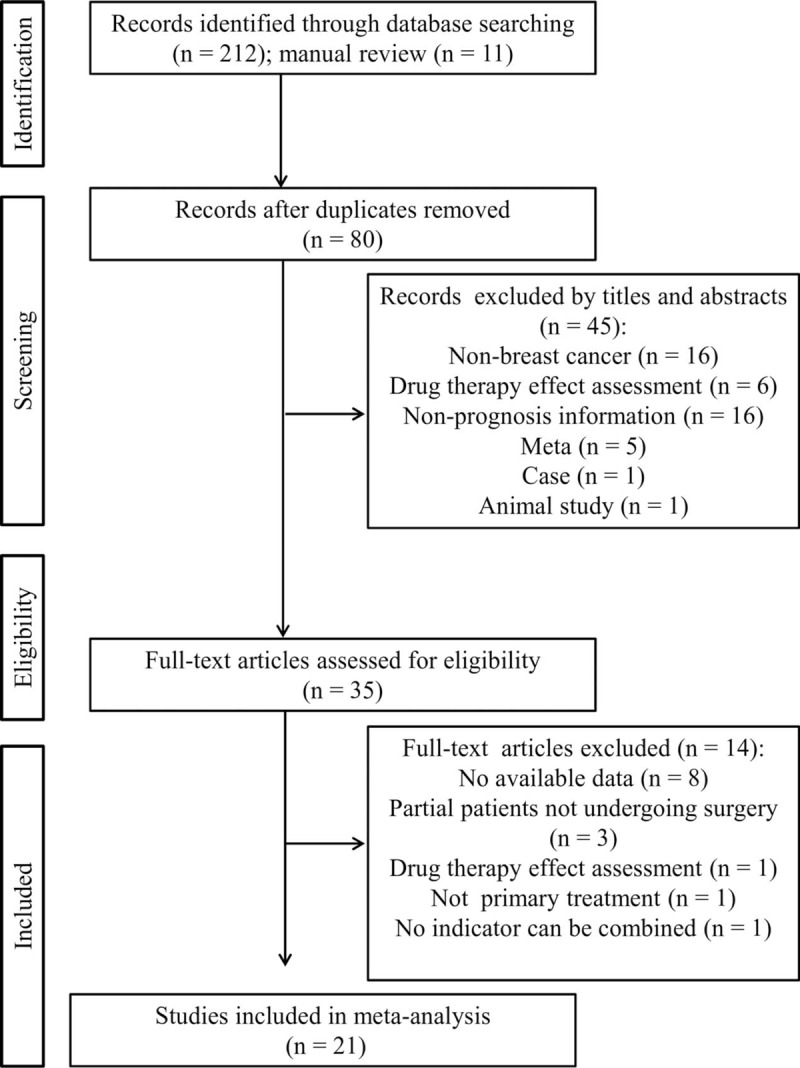
Flow diagram of study identification.
Table 1.
Characteristics of included studies.

3.2. Association between NLR and BC survival
There were 12 studies to investigate the prognostic significance of preoperative NLR for OS in BC patients. A significant heterogeneity was present between the studies (I2 = 60.6%, P = .003) and thus a random-effects model was chosen to pool the study results. Pooled results showed that elevated NLR was significantly associated with poorer OS (HR = 2.45, 95% CI: 1.69–3.54, P < .001) (Fig. 2A) in BC patients undergoing surgery.
Figure 2.

Forest plots of the correlation of neutrophil to lymphocyte ratio with survival. (A) Overall survival; (B) disease-free survival; (C) recurrence-free survival.
Fifteen studies assessed the prognostic significance of preoperative NLR for DFS in BC patients. There was evidence of a significant heterogeneity between the studies (I2 = 83.9%, P < .001) and thus a random-effects model was used. Pooled results showed that elevated NLR was significantly associated with poorer DFS (HR = 1.54, 95% CI: 1.28–1.87, P < .001) (Fig. 2B) in BC patients undergoing surgery.
Two studies analyzed the preoperative NLR for predicting the RFS of BC patients. A fixed effect was adopted to pool the study results because of I2 = 0% and P = .84. The pooled estimates analysis predicted that RFS was significantly lower in BC patients with an elevated NLR (HR = 4.05, 95% CI: 1.94–8.47, P < .001) (Fig. 2C).
There were 3 studies to investigate the prognostic significance of preoperative NLR for DSS in BC patients. A random-effects model were applied to pool the study results because a significant heterogeneity was detected between the studies (I2 = 76.3%, P = .015). The pooled results that no significant association between preoperative NLR and DSS for patients with BC (HR = 2.17, 95% CI: 0.97–4.82, P = .058).
3.3. Association between dNLR and BC survival
Two studies analyzed the association between preoperative dNLR and OS of BC patients. A fixed-effects was adopted to pool the study results because of I2 = 0% and P = .599. The pooled estimates analysis indicated that high-preoperative dNLR was also significantly associated with worse OS (HR = 1.75, 95% CI: 1.39–2.19, P < .001) (Fig. 3A).
Figure 3.

Forest plots of the correlation of derived neutrophil to lymphocyte ratio with survival. (A) overall survival; (B) disease-free survival.
There were 3 studies to investigate the prognostic value of preoperative dNLR for DFS in BC patients. A random-effects model were applied to pool the study results because an obvious heterogeneity was present between the studies (I2 = 81.43%, P = .004). The pooled results that high preoperative dNLR was significantly associated with DFS (HR = 1.62, 95% CI: 1.09–2.41, P = .017) (Fig. 3B).
3.4. Publication bias
The publication bias was present in NLR for DFS (P = .007), but not in NLR for OS (P = .436) and DSS (P = .144) as well as dNLR for DFS (P = .363). Subsequently, a trim-and-fill method was performed to explore the influence of publication bias on the effect estimate. The filled meta-analysis indicated no significant association was present between preoperative NLR and DFS (HR = 1.19; 95%CI: 0.98–1.44, P = .081), indicating the prognostic value of preoperative NLR for DFS needed further confirmation (Fig. 4).
Figure 4.

Funnel plot for the assessment of potential publication bias. (A) Egger's funnel plot for disease-free survival of neutrophil to lymphocyte ratio; (B) trim-and-fill funnel plot for disease-free survival of neutrophil to lymphocyte ratio.
3.5. Sensitivity analyses
Sensitivity analysis was conducted by assessing the potential impact of individual studies on the pooled HR. The results showed that pooled HR was not significantly altered when each study was successively deleted (Fig. 5).
Figure 5.

Sensitivity analysis.
3.6. Subgroup analysis
The subgroup analyses according to ethnicity, publication year, sample size, stage, follow-up time, cut-off, statistical methods, and adjuvant therapy were performed for NLR. The results showed that significant associations between preoperative elevated NLR and poor OS were not changed by the stratification of ethnicity (eastern or western), cutoff of NLR, pathological stage, neoadjuvant and adjuvant therapy, while the associations between preoperative elevated NLR and poor DFS were only significant in Eastern countries with follow-up duration longer than 50 months (Table 2). Few studies only performed the univariate analyses and heterogeneity may be present, leading to no significant associations between preoperative elevated NLR and poor OS/DFS with this analysis (Table 2).
Table 2.
Subgroup analysis.

4. Discussion
Although there were studies to use the meta-analysis approach to determine the prognostic role of NLR in BC, all of them focused on the pretreatment, but not paid attention on the surgery effects independently.[11,12,40,41] Also, all the included articles in these meta-analyses[11,12,40,41] were published before April 2016 and the evidence extensively accumulated therewith has not been enrolled. Our present study, for the first time, used the meta-analysis to specifically assess the prognostic value of preoperative NLR and prognosis in BC patients undergoing surgery with the literature updated to September 2018. The sample size was further expanded and more believable conclusion may be achieved. Our study identified 20 studies and the initial pooled meta-analysis results indicated that patients with higher preoperative NLR had shorter OS, DFS, and RFS outcomes in patients with BC. However, the significant association of NLR with DFS was vanished after correction of publication bias using the trim-and-fill method. Subgroup analyses predicted the nationality of patients, follow-up duration and statistical methods might be the major sources of heterogeneity to influence the prognostic importance of elevated NLR on DFS outcomes with only significant associations in Eastern populations, follow-up > 50 months and multivariate analyses. Our finding seemed to be different from the previous meta-analyses that found a high NLR appeared to be a negative prognostic marker in western populations,[11,12] further demonstrating the necessity of our study.
In addition, dNLR has been used for NLR alternative in several clinical trials. There was also evidence to show an independent significant association between high dNLR and poor OS as well as DFS outcomes in patients with BC[17] and other cancers[42,43]. However, the meta-analysis for integrative assessment of the prognostic value of dNLR with controversial literatures[17,18] had not been reported previously. In this study, we, for the first time, included 3 articles of BC and proved high-preoperative dNLR was also significantly associated with worse OS and DFS in patients with BC.
An elevated NLR/dNLR indicated the neutrophil-dependent inflammatory reaction was increased, but lymphocyte-mediated antitumor immune response was lower. There have evidence to demonstrate tumor associated neutrophils support metastatic initiation of BC.[44,45] Neutrophil-derived leukotrienes aided the colonization of distant tissues by selectively expanding the subpool of cancer cells that retain high tumorigenic potential. Inhibition of the leukotriene-generating enzyme arachidonate 5-lipoxygenase may abrogate pro-metastatic activity of neutrophils and reduce lung metastasis.[45] Anticancer drugs (i.e., 5-fluorouracil) mediated aggravation of BC metastasis to lung was also attributed to increased intrapulmonary neutrophil numbers and expression of neutrophilic chemokines (C-X-C motif chemokine ligand 1, Cxcl1 and Cxcl2) in tumor cells. The administration of a neutrophil-depleting antibody or a C-X-C motif chemokine receptor 2 (Cxcr2) antagonist, SB225002, significantly attenuated 5-fluorouracil-mediated enhanced lung metastasis.[46] Donati et al[47] also reported neutrophils may promote adhesiveness, invasiveness, and migration of BC cells by secreting cytokine interleukin-16, while instillation of an interleukin-16 neutralizing antibody reversed the effects of neutrophils. Even, Coffelt et al[48] found tumor-induced neutrophils may promote the establishment of pulmonary and lymph node metastases by suppressing cytotoxic T lymphocytes. BC patients with metastases are more prone to have shorter survival time. In line with these studies, we also found the HR of NLR for poor OS was higher in studies with mixed stage (having metastatic cases) than the early stage.
There are several limitations in this meta-analysis. Firstly, all of enrolled studies were retrospective, which may lead to some biases. Secondly, only 3 studies were included to evaluate the prognostic significance of dNLR for survival, which may lead to the overestimation or underestimation of its value. Thirdly, most of studies included neo-adjuvant and/or adjuvant treatment protocols and the survival outcomes may be influenced. Fourthly, the cut-off value for the NLR differed in each study although it was both significant according to our subgroup analysis. This may influence their clinical application.
In conclusion, this meta-analysis demonstrates preoperative NLR/dNLR may be effective predictive biomarkers for prognosis in patients with BC. Detection of NLR/dNLR may be helpful to identify the patients who benefit from the surgery.
Author contributions
JWD and MY participated in conception and design of this study. JWD and LLP performed acquisition of data; JWD and LLP performed the statistical analyses; MY was involved in interpretation of data. JWD drafted the manuscript. MY revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Conceptualization: Junwu Duan, Ming Yang.
Data curation: Junwu Duan, Linlin Pan.
Formal analysis: Junwu Duan, Linlin Pan.
Investigation: Linlin Pan.
Methodology: Junwu Duan.
Validation: Linlin Pan.
Writing – original draft: Junwu Duan.
Writing – review & editing: Ming Yang.
Footnotes
Abbreviations: BC = breast cancer, CI = confidence interval, Cxcl1 = C-X-C motif chemokine ligand 1, Cxcr2 = C-X-C motif chemokine receptor 2, DFS = disease-free survival, dNLR = derived NLR, DSS = disease specific survival, ER = estrogen receptor, HER2 = human epidermal growth factor receptor 2, HR = hazard ratio, NLR = neutrophil-to-lymphocyte ratio, OS = overall survival, PR = progesterone receptor, PRISMA = the Preferred Reporting Items for Systematic Review and Meta-analysis, RFS = recurrence-free survival, SIGN = Scottish Intercollegiate Guidelines Ne2rk, TNM = tumor node metastasis.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors have no conflicts of interest to disclose.
References
- [1].Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin 2018;68:7–30. [DOI] [PubMed] [Google Scholar]
- [2].Maishman T, Cutress RI, Hernandez A, et al. Local recurrence and breast oncological surgery in young women with breast cancer: the POSH Observational Cohort Study. Ann Surg 2017;266:165–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Menon M, Teh CH, Chua CL. Clinical and social problems in young women with breast carcinoma. Aust N Z J Surg 2010;62:364–7. [DOI] [PubMed] [Google Scholar]
- [4].Martincich L, Deantoni V, Bertotto I, et al. Correlations between diffusion-weighted imaging and breast cancer biomarkers. Eur Radiol 2012;22:1519–28. [DOI] [PubMed] [Google Scholar]
- [5].Lyman GH, Temin S, Edge SB, et al. Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 2014;32:1365–83. [DOI] [PubMed] [Google Scholar]
- [6].Hadad SM, Jordan LB, Roy PG, et al. A prospective comparison of ER, PR Ki67 and gene expression in paired sequential core biopsies of primary, untreated breast cancer. BMC Cancer 2016;16:745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Engstrøm MJ1, Opdahl S, Hagen AI, et al. Molecular subtypes, histopathological grade and survival in a historic cohort of breast cancer patients. Breast Cancer Res Treat 2013;140:463–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Jiang X, Shapiro DJ. The immune system and inflammation in breast cancer. Mol Cell Endocrinol 2014;382:673–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Huang A, Cao S, Tang L. The tumor microenvironment and inflammatory breast cancer. J Cancer 2017;8:1884–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Qian Y, Tao J, Li X, et al. Peripheral inflammation/immune indicators of chemosensitivity and prognosis in breast cancer patients treated with neoadjuvant chemotherapy. Onco Targets Ther 2018;11:1423–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Wei B, Yao M, Xing C, et al. The neutrophil lymphocyte ratio is associated with breast cancer prognosis: an updated systematic review and meta-analysis. Onco Targets Ther 2016;9:5567–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chen J, Deng Q, Pan Y, et al. Prognostic value of neutrophil-to-lymphocyte ratio in breast cancer. Febs Open Bio 2015;5:502–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Yao M, Liu Y, Jin H, et al. Prognostic value of preoperative inflammatory markers in Chinese patients with breast cancer. Onco Targets Ther 2014;7:1743–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Jia W, Wu J, Jia H, et al. The peripheral blood neutrophil-to-lymphocyte ratio is superior to the lymphocyte-to-monocyte ratio for predicting the long-term survival of triple-negative breast cancer patients. PLoS One 2015;10:e0143061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Chen Q, Yang LX, Li XD, et al. The elevated preoperative neutrophil-to-lymphocyte ratio predicts poor prognosis in intrahepatic cholangiocarcinoma patients undergoing hepatectomy. Tumour Biol 2015;36:5283–9. [DOI] [PubMed] [Google Scholar]
- [16].Cihan YB, Arslan A, Cetindag MF, et al. Lack of prognostic value of blood parameters in patients receiving adjuvant radiotherapy for breast cancer. Asian Pac J Cancer Prev 2014;15:4225–31. [DOI] [PubMed] [Google Scholar]
- [17].Krenn-Pilko S, Langsenlehner U, Stojakovic T, et al. The elevated preoperative derived neutrophil-to-lymphocyte ratio predicts poor clinical outcome in breast cancer patients. Tumour Biol 2016;37:361–8. [DOI] [PubMed] [Google Scholar]
- [18].Cho U, Hong SP, Im SY, et al. Prognostic value of systemic inflammatory markers and development of a nomogram in breast cancer. PLoS One 2018;13:e0200936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 elaboration and explanation. BMJ 2015;349:g7647. [DOI] [PubMed] [Google Scholar]
- [20].Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ 2001;323:334–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Egger M DSG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000;56:455–63. [DOI] [PubMed] [Google Scholar]
- [24].Forget P, Machiels JP, Coulie PG, et al. Neutrophil:lymphocyte ratio and intraoperative use of ketorolac or diclofenac are prognostic factors in different cohorts of patients undergoing breast, lung, and kidney cancer surgery. Ann Surg Oncol 2013;20:S650–60. [DOI] [PubMed] [Google Scholar]
- [25].Noh H EM, Han A. Usefulness of pretreatment neutrophil to lymphocyte ratio in predicting disease-specific survival in breast cancer patients. J Breast Cancer 2013;16:55–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Nakano K, Hosoda M, Yamamoto M, et al. Prognostic significance of pre-treatment neutrophil: lymphocyte ratio in Japanese patients with breast cancer. Anticancer Res 2014;34:3819–24. [PubMed] [Google Scholar]
- [27].Koh YW, Lee HJ, Ahn JH, et al. Prognostic significance of the ratio of absolute neutrophil to lymphocyte counts for breast cancer patients with ER/PR-positivity and HER2-negativity in neoadjuvant setting. Tumour Biol 2014;35:9823–30. [DOI] [PubMed] [Google Scholar]
- [28].Forget P, Bentin C, Machiels JP, et al. Intraoperative use of ketorolac or diclofenac is associated with improved disease-free survival and overall survival in conservative breast cancer surgery. Br J Anaesth 2014;113:i82–7. [DOI] [PubMed] [Google Scholar]
- [29].Bozkurt O, Karaca H, Berk V, et al. Predicting the role of the pretreatment neutrophil to lymphocyte ratio in the survival of early triple-negative breast cancer patients. J BUON 2015;20:1432–9. [PubMed] [Google Scholar]
- [30].Pistelli M, Lisa MD, Ballatore Z, et al. Pre-treatment neutrophil to lymphocyte ratio may be a useful tool in predicting survival in early triple negative breast cancer patients. BMC Cancer 2015;15:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Dirican A, Kucukzeybek BB, Alacacioglu A, et al. Do the derived neutrophil to lymphocyte ratio and the neutrophil to lymphocyte ratio predict prognosis in breast cancer? Int J Clin Oncol 2015;20:70–81. [DOI] [PubMed] [Google Scholar]
- [32].Suppan C, Bjelic-Radisic V, Garde ML, et al. Neutrophil/lymphocyte ratio has no predictive or prognostic value in breast cancer patients undergoing preoperative systemic therapy. BMC Cancer 2015;15:1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Hong J, Mao Y, Chen X, et al. Elevated preoperative neutrophil-to-lymphocyte ratio predicts poor disease-free survival in Chinese women with breast cancer. Tumour Biol 2015;37:4135–42. [DOI] [PubMed] [Google Scholar]
- [34].Yun YK, Park HK, Lee KH, et al. Prognostically distinctive subgroup in pathologic N3 breast cancer. J Breast Cancer 2016;19:163–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Takeuchi H, Kawanaka H, Fukuyama S, et al. Comparison of the prognostic values of preoperative inflammation-based parameters in patients with breast cancer. PLoS One 2017;12:e0177137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Hernández CM, Madrona AP, Vázquez PJG, et al. Usefulness of lymphocyte-to-monocyte, neutrophil-to-monocyte and neutrophil-to-lymphocyte ratios as prognostic markers in breast cancer patients treated with neoadjuvant chemotherapy. Clin Transl Oncol 2017;20:476–83. [DOI] [PubMed] [Google Scholar]
- [37].Qiu X, Song Y, Cui Y, et al. Increased neutrophil-lymphocyte ratio independently predicts poor survival in non-metastatic triple-negative breast cancer patients. IUBMB Life 2018;70:529–35. [DOI] [PubMed] [Google Scholar]
- [38].Geng SK FS, Fu YP, Zhang HW. Neutrophil to lymphocyte ratio is a prognostic factor for disease free survival in patients with breast cancer underwent curative resection. Medicine 2018;97:e11898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Lee J, Kim DM, Lee A. Prognostic role and clinical association of tumor-infiltrating lymphocyte, programmed death ligand-1 expression with neutrophil-lymphocyte ratio in locally advanced triple-negative breast cancer. Cancer Res Treat 2018;doi: 10.4143/crt.2018.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Liu X, Qu JK, Zhang J, et al. Prognostic role of pretreatment neutrophil to lymphocyte ratio in breast cancer patients: a meta-analysis. Medicine 2017;96:e8101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Ethier JL DD, Templeton A, Shah P, et al. Prognostic role of neutrophil-to-lymphocyte ratio in breast cancer: a systematic review and meta-analysis. Breast Cancer Res 2017;19:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Song S, Li C, Li S, et al. Derived neutrophil to lymphocyte ratio and monocyte to lymphocyte ratio may be better biomarkers for predicting overall survival of patients with advanced gastric cancer. Onco Targets Ther 2017;10:3145–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Capone M, Giannarelli D, Mallardo D, et al. Baseline neutrophil-to-lymphocyte ratio (NLR) and derived NLR could predict overall survival in patients with advanced melanoma treated with nivolumab. J Immunother Cancer 2018;6:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Ibrahim SA, Katara GK, Arpita K, et al. Breast cancer associated a2 isoform vacuolar ATPase immunomodulates neutrophils: potential role in tumor progression. Oncotarget 2015;6:33033–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Wculek SK, Malanchi I. Neutrophils support lung colonization of metastasis-initiating breast cancer cells. Nature 2015;528:413–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Sasaki S, Baba T, Muranaka H, et al. Involvement of prokineticin 2-expressing neutrophil infiltration in 5-fluorouracil-induced aggravation of breast cancer metastasis to lung. Mol Cancer Ther 2018;17:1515–25. [DOI] [PubMed] [Google Scholar]
- [47].Donati K, Sépult C, Rocks N, et al. Neutrophil-derived interleukin 16 in premetastatic lungs promotes breast tumor cell seeding. Cancer Growth Metastasis 2017;10:179064417738513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Coffelt SB, Kersten K, Doornebal CW, et al. IL17-producing γδ T cells and neutrophils conspire to promote breast cancer metastasis. Nature 2015;522:345–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


