Abstract
Rationale:
Currently, interventional injection of albumin glue and nerve sleeve plasty by cyst excision is the main treatment for sacral cysts. However, albumin glue can only be used in patients with partial cystic neck stenosis, and surgical treatment may result in postoperative complications such as numbness and cyst recurrence. Here, a modified radiculoplasty is presented, in which the lamina is restored with the nerve root wrapped with 3-dimensional (3D)-printed artificial dura mater.
Patient concerns:
The first patient, a 28-year-old man, had been complaining of aggravated perineal pain for 8 months a visual analog scale (VAS) score of 7. Sacrococcygeal magnetic resonance imaging (MRI) revealed multiple sacral canal cysts. The second case, a 48-year-old woman, has been complaining of lumbosacral and left leg pain for 1 month (VAS score of 7). Physical examination showed hyperalgesia below the right sacrum 2 level. Sacrococcygeal MRI and computed tomography (CT) revealed multiple sacral canal cysts and a calcified lesion in the cyst.
Diagnoses and Intervention:
The first patient underwent radiculoplasty with reconstruction using 3D-printed artificial dura mater, with 3 cysts treated and the lamina restored. Four cysts of the second patients were treated, including 1 bone-occupying lesion. Radiculoplasty with reconstruction using 3D-printed artificial dura mater was used for the cysts and the lamina was restored
Outcomes:
The postoperative VAS score was 0 to 2 points in the 2 patients. No postoperative infection or new neurological dysfunction was observed. Postoperative MRI showed no cysts, with lamina restoration. After 6 months, the VAS score was 0, and MRI showed no recurrence.
Lessons:
Radiculoplasty with reconstruction using 3D-printed artificial dura mater and lamina restoration could be beneficial for the treatment of symptomatic sacral canal cysts.
Keywords: surgery, Tarlov cysts
1. Introduction
Sacral canal cysts, that is, dural cysts in the sacral canal, often occur at multiple sites and contain nerve roots. They were first reported by Tarlov in 1938 and have been gradually recognized since then. Some patients with sacral canal cysts may show no clinical symptoms and may seek medical help due to pain and numbness in the sacrococcygeal joint and the perineum, bladder/bowel dysfunction, sex function disorders, and other sacral canal-related manifestations. Large cysts may lead to local pressure and remodel bones, but symptoms are not associated with cyst size[1].
With the increasing popularity of magnetic resonance imaging (MRI), sacral cysts are more and more commonly found and treated in neurosurgery. Kuhn et al[2] reported that the detection rate was 13.2% in 1100 consecutive sacral MRI studies. Due to suboptimal understanding of the pathogenesis of symptomatic sacral cysts, many treatment methods have been developed, including puncture-aspiration and albumin glue injection, excision, and shunt. Currently, interventional injection of albumin glue and nerve sleeve plasty by cyst excision is the main method. Nevertheless, interventional injection of albumin glue is only suitable for patients with partial cystic neck stenosis, while the current surgical treatments may lead to postoperative complications such as numbness and cyst recurrence. Weigel et al[3] reported that despite the use of the nerve sheath folding suture technique, 15% of the patients still have short-term cyst recurrences, suggesting that the methods still have to be refined.
In August 2017, 2 patients with symptomatic sacral canal cyst underwent modified radiculoplasty by 3-dimensional (3D)-printed artificial dura mater to strengthen the nerve root sleeves and satisfactory results were obtained. This could be a novel approach to protect nerve roots and prevent symptom recurrence after surgery.
2. Case report
2.1. Case 1
The patient was a 28-year-old man who had been complaining of aggravated perineal pain for 8 months, with inguinal region discomfort for 2 months and a visual analog scale (VAS) score of 7 points. Pain was alleviated after rest. Physical examination showed normal sensation, deep and shallow reflection, and sphincter function. Extensor longus strength was grade 4. Sacrococcygeal MRI revealed multiple sacral canal cysts (Fig. 1). Under general anesthesia, the patient was placed in the prone waist-bridge position with head-down. Somatosensory evoked potential (SEP) and motor evoked potential (MEP) were monitored in real-time. An incision was made within 7 cm of the spinous process of L5 to S3 in the posteromedian line and the paraspinal muscles were cut open along the midline to expose the sacral spinous process and bilateral fused lamina. The bilateral laminae and caudal spinous processes were incised using an ultrasonic bone knife, removing the entire spinous process-lamina complex. Under a microscope, 3 cysts were visible in the sacral canal. Two cysts were 1.5 cm in diameter and the third was 0.8 cm. The cysts were connected to the subarachnoid space via the end of the dural sac and extended to the anterior sacral foramina. The tissue surrounding the cysts was dissected, with the sacral nerve removed from the cyst wall. For the largest cysts, the nerve roots were tortuously attached to the cyst wall, and the cyst wall was partly removed after loosening the nerve root.[4] The cyst wall was retracted by bipolar coagulation at a location without nerve root and sutured around the nerve root. For the smallest cyst, the nerve root was shaped by bipolar-coagulation of the cyst wall at a location without nerve root, and the whole shaped nerve root was wrapped tightly with 3D-printed dura mater patches (ReDura, Medprin Regenerative Medical Technologies Co. Ltd.) cut into 2∗3 cm pieces and closed using an anastomat. The patient's head was lifted to confirm there was no leakage. The sacral canal cavity was filled with gelatin sponge and the lamina was restored and fixed with titanium nails and plates, followed by wound closure. The operation lasted 180 minutes, with intraoperative bleeding of 50 ml. The patient was required to remain in the prone position for 1-week post-surgery. No postoperative infection or new neurological dysfunction was observed. Review MRI at postoperative 1 week revealed cyst disappearance and a good position for the restored lamina. The patient was discharged at postoperative 12 days. Follow-up at postoperative 6 months showed that symptoms were relieved, and a VAS score of 0 point was recorded. In addition, postoperative pathology revealed that the cyst wall tissue derived from a simple cyst.
Figure 1.
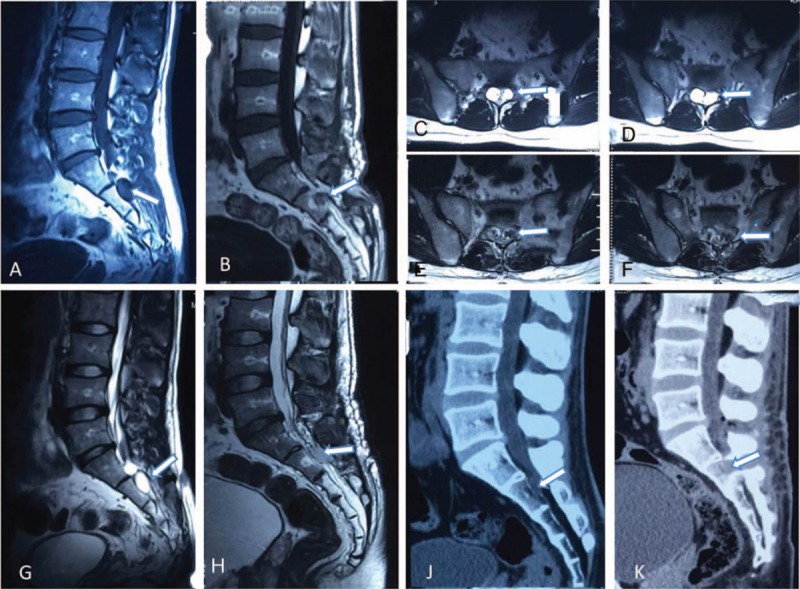
A, Sagittal MRI T1-weighted image of a sacral canal cyst (arrow). B, Postoperative T1-weighted image showing sacral canal cyst disappearance (arrow). C and D, Axial MRI T2-weighted images showing 2 sacral canal cysts (arrows). E and F, Postoperative axial MRI T2-weighted images showing sacral canal cyst disappearance (arrows). G, Sagittal MRI T2-weighted image showing multiple sacral canal cysts (arrow). H, Postoperative T2-weighted image showing the disappearance of the sacral canal cysts (arrow). J, Sagittal CT reconstruction image of the sacral canal cyst (arrow). K, Postoperative sagittal CT reconstruction image showing sacral canal cyst disappearance (arrow) and lamina restoration. CT = computed tomography, MRI = magnetic resonance imaging.
2.2. Case 2
The patient was a 48-year-old woman who had been complaining of lumbosacral pain and left leg pain for 1 month, which was aggravated for 10 days. VAS score was 7 and pain was alleviated after rest. Physical examination showed hyperalgesia below the right thigh, normal muscle strength of lower extremities, normal anal sphincter function, normal tendon reflex, and no pathological sign. Bladder sacrococcygeal MRI and computed tomography (CT) revealed multiple sacral canal cysts, with calcified lesions in cysts at the right sacrum 2 level (Fig. 2). The patient underwent general anesthesia and surgery as mentioned above, that is, cyst excision and radiculoplasty with reconstruction using 3D-printed artificial dura mater, with lamina restoration. Four cysts were treated. One bone-occupying lesion was removed from the cyst. Two cyst walls were partially removed and sutured. Two small cysts were submitted to bipolar-coagulation. During the operation, 2 large cysts were opened under the microscope, with the nerve root fixed to the cyst wall by the arachnoid band (Fig. 3). The cyst was connected to the dural sac. The bone lesion was located at the intervertebral foramen, which constituted the outlet of the nerve root in the cyst, adhering to the nerve. Under a microscope, the adhesion was separated, with the lesion completely removed. All 4 cysts were submitted to the modified radiculoplasty mentioned above. The residual sacral cavity was filled with gelatin sponge and the lamina was restored and fixed with titanium plates and nails, followed by wound closure. The operation lasted 190 minutes, with intraoperative bleeding of 50 mL. The patient was required to remain in the prone position for 1 week post-surgery. She underwent MRI and CT review at postoperative 1 week, which showed cyst disappearance and that the lesions were completely removed, with complete lamina restoration (Fig. 4). The patient showed no postoperative infection or new neurological dysfunction and was discharged at postoperative 7 days. Postoperative pathology revealed that the cyst wall tissue derived from a simple cyst and the calcified lesions were bone tissues. At 6-month follow-up, the symptoms were relieved and a VAS score of 0 point was obtained. The MRI examination showed no recurrence of the cyst (Fig. 4).
Figure 2.
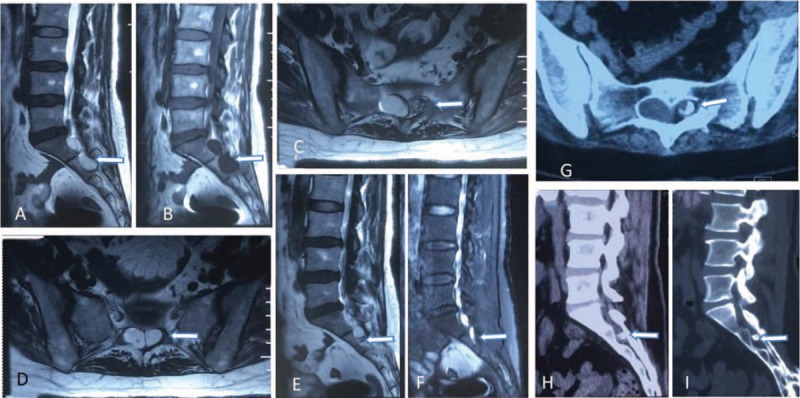
A, Sagittal MRI T2-weighted image showing multiple sacral canal cysts (arrow). B, Sagittal T1-weighted image of sacral canal cysts (arrow). C, Axial MRI T2-weighted image showing low signal lesions in the sacral canal cyst (arrow). D, Axial MRI T2-weighted image of sacral canal cysts (arrow). E and F, Sagittal MRI T2-weighted images showing low signal lesions in the sacral canal cyst (arrow). G, Axial CT image showing high-density lesions in the sacral canal cyst (arrow). H and I, Sagittal CT reconstruction image showing high-density lesions in the sacral canal cyst (arrow). CT = computed tomography, MRI = magnetic resonance imaging.
Figure 3.
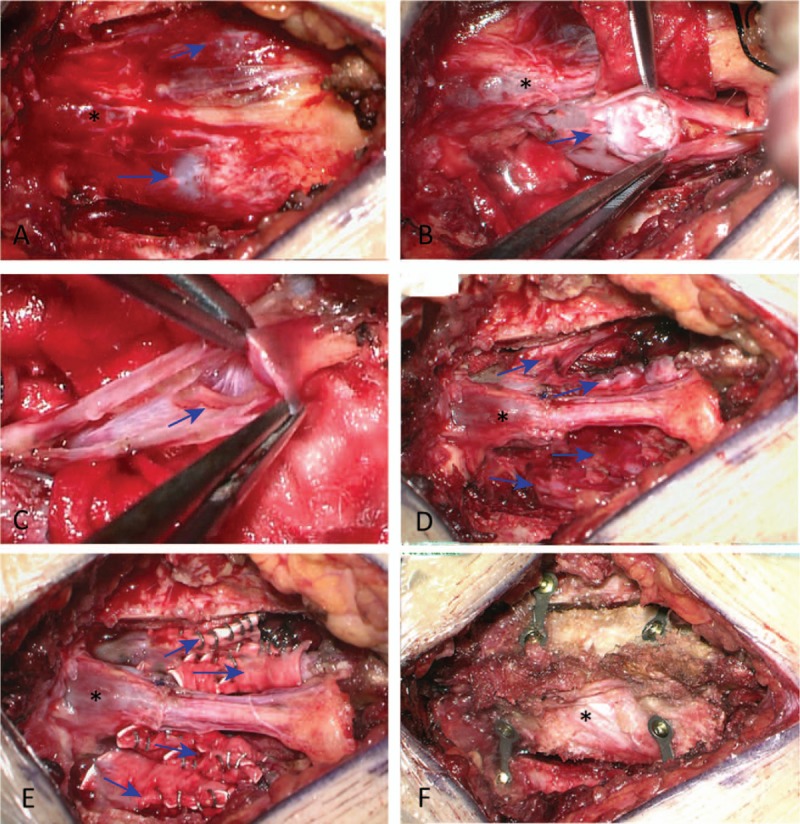
A, End of the dural sac in the sacral canal after lamina removal (∗), with multiple sacral canal cysts in the tail end (arrow). B, Bone occupying lesions in the cyst (arrow). C, Nerve root which tortuously travels and adheres to the cyst wall (arrow). D, Nerve root sleeve plasty after partial removal of the cyst wall (arrow) (∗, end of the dural sac). E, Post-radiculoplasty by artificial dura mater wrapping (arrow) (∗, end of the dural sac). F, ∗Restored lamina fixed with titanium nails and plates.
Figure 4.
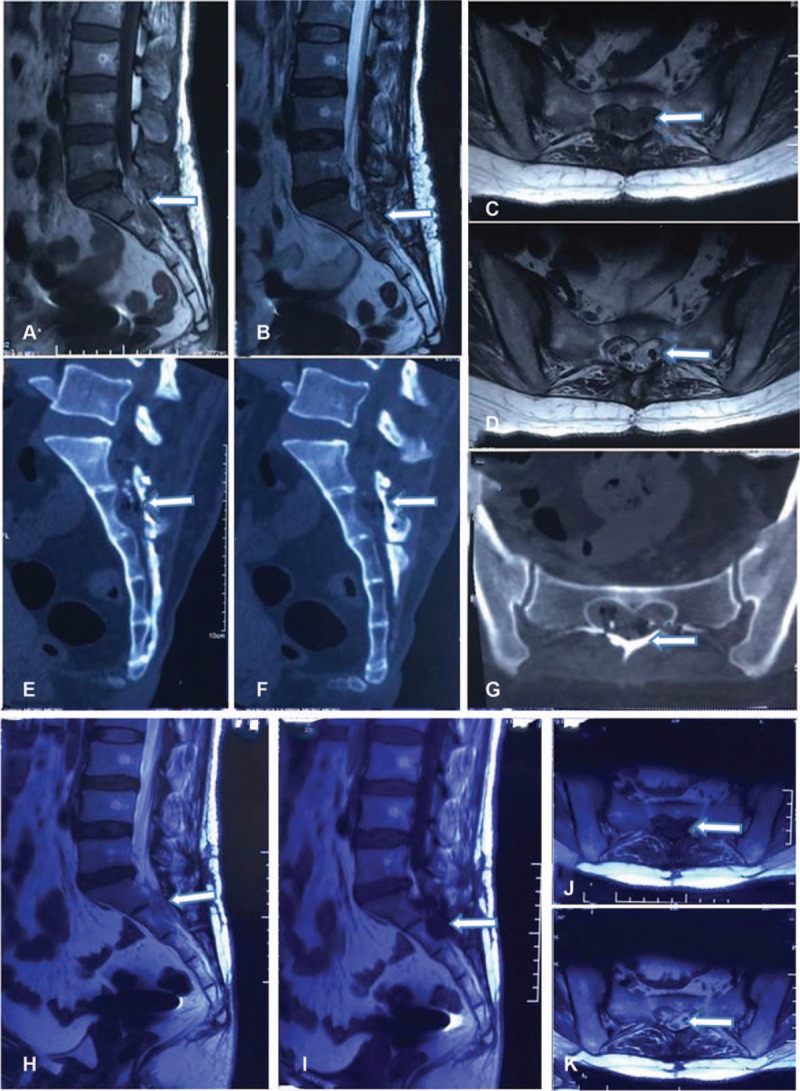
A, Postoperative sagittal MRI T1-weighted image showing the disappearance of multiple sacral canal cysts (arrow). B, Postoperative sagittal MRI T2-weighted image showing the disappearance of the sacral canal cysts (arrow). C, Postoperative axial MRI T1-weighted image showing the disappearance of the sacral canal cysts, with low signal lesions in the removed cysts (arrow). D, Axial MRI T2-weighted image showing the disappearance of the sacral canal cysts, with low signal indicating the reconstructed nerve root (arrow). E, Sagittal CT reconstruction image showing removal of high-density lesions, with dotted-line titanium nail shadows visible along the nerve root track (arrow). F, Sagittal CT reconstruction image showing lamina restoration (arrow). G, Axial CT image showing lamina restoration, with the fixed titanium plates showing high-density (arrow) and titanium nail shadows visible in the sacral canal. H, Postoperative 6 months sagital MRI T2-weighted image showing the disappearance of the sacral canal cysts, with low signal lesions in the cysts removed (arrow). I, Postoperative 6 months sagital MRI T1-weighted image showing the disappearance of the sacral canal cysts, with low signal lesions in the cysts removed (arrow). J, Postoperative 6 months axial MRI T1-weighted image showing the disappearance of the sacral canal cysts, with low signal lesions in the cysts removed (arrow). K. Postoperative 6 months axial MRI T2-weighted image showing the disappearance of the sacral canal cysts, with the low signal indicating the reconstructed nerve root (arrow). CT = computed tomography, MRI = magnetic resonance imaging.
3. Discussion
The detection rate of sacral cysts is 13.2% and nearly 1 patient in 4 has symptoms.[2] The most common sacral canal cyst symptom is lumbosacral pain, which explains why it is associated with nerve root degeneration, twist, and compression in the cyst, and causes the cyst to invade the sacrum, involving periosteal receptors.[5] In this study, the nerve root was found to tortuously travel and adhere to the cyst wall. Intraoperative exploration revealed traction of the arachnoid band, which was released, resulting in significantly alleviated pain postoperatively. These findings suggested that nerve root adhesion and traction are likely the most important reasons for pain. In addition, the cysts adhered to the peripheral nerve to different degrees. Thus, the occupying effect of cysts on the peripheral nerve may also cause pain.
In order to relieve the symptoms, a variety of treatment methods have been developed, including puncture-aspiration and albumin glue injection, excision, and shunt.[6–8] So far, radiculoplasty under microscope and interventional injection of albumin glue are the main methods.[9] Murphy et al[9] injected albumin glue into cysts in 213 patients using the double-needle puncture method and 81.1% of them achieved remission; therefore, they proposed that this method could be considered a preferred treatment for patients with a small cyst opening communicating with the subarachnoid space.[9] Nevertheless, albumin glue injection cannot effectively remediate the space-occupying effect of the cysts. Compared with interventional puncture, microsurgery enables direct release of the nerve root and effectively removes the occupying effect of the cysts, but this surgery may induce new neurological symptoms such as numbness. The absence of lamina and filling of the sacral canal post-surgery are important factors causing cyst recurrence and pain. Potts et al[10] applied laminotomy and paravertebral muscle filling for the treatment of 35 patients, and obtained a postoperative relapse rate of pain reaching 50%, indicating that even though laminotomy decompression is effective over the short term, the filling tissue is not sufficient to prevent cyst recurrence. Therefore, how to restore the normal anatomy and physiology of the sacral canal remains challenging. Weigel et al[3] replaced cyst wall resection by reverse cyst wall suturing, while performing lamina restoration and sacral plastic surgery. Pain and neurological deficits were relieved in 11 patients after an average follow-up of 5.3 years,[3] suggesting that a good curative effect can be achieved for cysts properly treated and that the anatomical morphology of the sacral canal can be recovered after lamina restoration. Nevertheless, about 20% recurrence of the symptoms was found within 3 month due to recurrent cysts. For the 2 patients described here, after cyst and nerve root shaping, 3D-printed artificial dura mater was used to wrap the nerve root, strengthening the nerve root to reduce the possibility of postoperative cyst recurrence and compensating for heterogeneous nerve capsule strength after nerve root sleeve plasty. The 3D-printed artificial dura mater (ReDura) does not only strengthen nerve root sleeves but also induces dural regeneration. Meanwhile, a good absorbability to the dural tissue is obtained, with subsequently reduced occurrence of cerebrospinal fluid leakage; this reduces the surgical difficulty compared with cyst wall infolding suture.[3] Wrapping the nerve root with artificial dura mater can shorten the operation time, undoubtedly reducing the possibility of exposure and damage of the nerve root. After cyst treatment, the nerve surrounding the cyst in the sacral canal was decompressed naturally and the residual cavity was filled with gelatin sponge to reduce the occupying effect. Meanwhile, lamina restoration could yield morphological and physiological protection of the sacral canal, while eliminating the residual cavity generated by postoperative bone defects.
In this study, surgery was carried out under electro-neurophysiological monitoring. Real-time SEP and MEP monitoring can reduce iatrogenic nerve injury. The lamina should be incised with a width that fully exposes the cyst during the whole process, with the head end revealing the terminus of the dural sac to facilitate the identification and treatment of the opening; the tail end should reach the lower boundary of the cyst, while the lateral side should extend to the lateral crypt of the sacral canal to reveal the cyst at the intervertebral foramen. One should avoid damaging the thinned sacral nerve outside the cyst when separating the cyst and the lamina. It is particularly important to avoid nerve root injury when incising and coagulating the cyst wall. Low power should be applied during electrocoagulation. In this study, bipolar coagulation was performed in the cyst wall without nerve root deviation using an ERBE high-frequency electric knife (15-W bipolar electrocoagulation). The nerve root should be wrapped with 3D-printed artificial dura mater properly; 2 cm long artificial dura mater can be used to wrap a 5 mm diameter nerve root, to avoid nerve root compression.[3]
The literature reports that 1 of the pathophysiological changes of sacral cysts is cystic hemorrhage. The second patient in this paper showed postoperative pathological findings of bone tissue in the cyst, which was considered to be caused by calcification of the hematoma after hemorrhage. Compression caused by the lesions and secondary inflammatory reactions are also causes of pain. Sacral cysts can present calcifications occupying the cyst, and surgical treatment should be preferred in this case. Reconstruction of nerve root sleeves by 3D-printed artificial dura mater wrapping is a viable surgical procedure. Meanwhile, lamina restoration can recover the normal morphology of the sacral canal, thereby providing conditions for physiological function recovery of the sacral canal. This study suggests that microsurgery should be the first choice for sacral cyst. Although the modified surgical method achieved good short-term effects in the treatment of 2 cases with sacral canal cysts, the sample size was small in this study. Therefore, long-term curative effects of this method should be verified by trials with large sample size and long-term follow-up.
In conclusion, radiculoplasty with reconstruction using 3D-printed artificial dura mater and lamina restoration could be beneficial for symptomatic sacral canal cysts.
Acknowledgments
We are grateful to the patients for allowing the publication of this report.
Author contributions
Investigation: Bin Liu, Zhenyu Wang, Guozhong Lin, Jia Zhang.
Methodology: Bin Liu, Zhenyu Wang, Guozhong Lin, Jia Zhang.
Supervision: Bin Liu.
Validation: Bin Liu.
Writing – original draft: Bin Liu, Zhenyu Wang, Guozhong Lin, Jia Zhang.
Writing – review & editing: Bin Liu, Zhenyu Wang, Guozhong Lin, Jia Zhang.
Footnotes
Abbreviations: 3D = 3-dimensional, CT = computed tomography, MEP= motor evoked potential, MRI = magnetic resonance imaging, SEP = somatosensory evoked potential, VAS = visual analog scale.
The study was approved by ethics committee of Peking University Third Hospital, and informed consent for publication of the case details and the accompanying images was given by the patients involved in this study.
The study was supported by Beijing Municipal Science & Technology Commission (No. Z181100001718171).
The authors have no conflicts of interest to disclose.
References
- [1].Davis SW, Levy LM, LeBihan DJ, et al. Sacral meningeal cysts: evaluation with MR imaging. Radiology 1993;187:445–8. [DOI] [PubMed] [Google Scholar]
- [2].Kuhn FP, Hammoud S, Lefevre-Colau MM, et al. Prevalence of simple and complex sacral perineural Tarlov cysts in a French cohort of adults and children. J Neuroradiol 2017;44:38–43. [DOI] [PubMed] [Google Scholar]
- [3].Weigel R, Polemikos M, Uksul N, et al. Tarlov cysts: long-term follow-up after microsurgical inverted plication and sacroplasty. Eur Spine J 2016;25:3403–10. [DOI] [PubMed] [Google Scholar]
- [4].Guo D, Shu K, Chen R, et al. Microsurgical treatment of symptomatic sacral perineurial cysts. Neurosurgery 2007;60:1059–65. [DOI] [PubMed] [Google Scholar]
- [5].Tarlov IM. Spinal perineurial and meningeal cysts. J Neurol Neurosurg Psychiatry 1970;33:833–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Jiang W, Qiu Q, Hao J, et al. Percutaneous fibrin gel injection under C-arm fluoroscopy guidance: a new minimally invasive choice for symptomatic sacral perineural cysts. PLoS One 2015;10:e0118254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Mezzadri J, Abbati SG, Jalon P. Tarlov cysts: endoscope-assisted obliteration of the communication with the spinal subarachnoid space. J Neurol Surg A Cent Eur Neurosurg 2014;75:462–6. [DOI] [PubMed] [Google Scholar]
- [8].Takemori T, Kakutani K, Maeno K, et al. Symptomatic perineural cyst: report of two cases treated with cyst-subarachnoid shunts. Eur Spine J 2014;23suppl 2:267–70. [DOI] [PubMed] [Google Scholar]
- [9].Murphy K, Oaklander AL, Elias G, et al. Treatment of 213 patients with symptomatic Tarlov Cysts by CT-guided percutaneous injection of Fibrin Sealant. AJNR Am J Neuroradiol 2016;37:373–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Potts MB, McGrath MH, Chin CT, et al. Microsurgical fenestration and paraspinal muscle pedicle flaps for the treatment of symptomatic sacral Tarlov cysts. World Neurosurg 2016;86:233–42. [DOI] [PubMed] [Google Scholar]


