Abstract
Rationale:
Lunate fractures are very rare, accounting for only 0.5% to 6.5% of all carpal fractures. They are mostly caused by high-energy trauma and commonly occur with fractures and dislocations of other carpal bones. It is rarely combined with Colles’ fracture and the underlying pathogenesis and prognostic significance still remain controversial.
Patient concerns:
Here we report a case of a fresh lunate fracture combined with Colles’ fracture, without dislocations of other carpal bones caused by a low-energy fall injury.
Diagnoses:
Lunate fracture, Colles’ fracture.
Interventions:
This patient received closed reduction and internal fixation (CRIF) with K-wire.
Outcomes:
The patient took follow up 1 year and the patient showed good function of the wrist joint
Lessons:
Lunate fractures have no high misdiagnosis rate. Patients suffering persistent wrist swelling after a trauma should be carefully examined and followed up to prevent severe secondary diseases and wrist joint dysfunction.
Keywords: CRIF, distal radius fracture, low-energy injure ;case report, lunate fractures
1. Introduction
Lunate fractures are very rare, accounting for only 0.5% to 6.5% of all carpal fractures and affecting men predominantly.[1,2] They are mostly caused by high-energy trauma[1,3] and commonly occur with fractures and dislocations of other carpal bones: “translunate, perilunate fracture-dislocations”.[3,4] To our best knowledge, only 1 case of lunate fracture with Colles’ fracture had been reported but without detailed data.[2]
Clinicians often face difficulty in the diagnosis of lunate fractures, resulting in a high rate of missed diagnosis. Previous studies on lunate fractures reported that lunate fractures were mostly defined as old fractures[5] and conventionally treated with open reduction and internal fixation (ORIF). Herein, we report for the first time a case of a fresh lunate fracture with Colles’ fracture caused by a low-energy fall injury, which was successfully treated by closed reduction and internal fixation (CRIF) with K-wire. This manuscript adheres to the CARE guidelines
2. Case report
A 66-year-old woman suffered a left wrist deformity due to a fall, accompanied by swelling and pain. She consequently complained of limited activity and presented to us on the second-day post-injury. After history taking, physical examinations, and radiography, she was diagnosed with “left distal radius fracture, ulnar styloid fracture.” In the past, she underwent screw internal fixation for right medial malleolus fractures.
On admission, physical examination revealed swelling, local bruise, marked deformity, local tenderness, percussion pain, bone friction signs, abnormal left wrist movement, limited dorsiflexion, and abduction of the left thumb, inability to make a fist, limited flexion, and extension of the left wrist, ulnar or radial deviation movement restriction, no obvious movement restriction of the left elbow joint, and slight numbness of left hand fingers.
Anteroposterior and lateral radiographs of the left wrist showed distal fracture of the left distal radius, with the fracture line involving the articular surface, and avulsion fracture of left ulnar styloid process (Fig. 1). Three-dimensional computed tomography (CT) of the left wrist showed multiple fracture lines of the left distal radius involving the articular surface, a transverse fracture line in the left ulnar styloid process, and disrupted left lunate continuity (Fig. 2). On the fifth day post-injury, she underwent ORIF of the left distal radius and CRIF of the lunate bone under regional anesthesia of the brachial plexus. ORIF with plate of the distal radius was performed, followed by a C-arm fluoroscopic CRIF with K-wire of the lunate bone (Fig. 3). She was given postoperative protection by a short-branch brace. Radiography at 6 postoperative weeks indicated that the fracture healed well (Fig. 4). After K-wire removal, she started functional exercise. Radiography at 24 postoperative weeks revealed healed bone fractures (Fig. 5) and improved wrist function (Fig. 6), with an excellent Mayo score. At 1 year post-treatment, she showed good function of the wrist joint (Fig. 7) with completely healed fracture. She was radiologically reexamined, and the fracture in the left wrist healed well. She presented with normal pronation and supination, flexion, and extension of the left wrist relative to the right wrist. The Mayo score (120 points) was excellent. Two-point discrimination measured on the middle and little fingers was 0. The disability of the arm, shoulder, and hand value was 1.67, and the patient-related wrist evaluation score (4 points) was excellent.
Figure 1.

Preoperative radiograph showing left distal radius fracture and ulnar styloid fracture.
Figure 2.
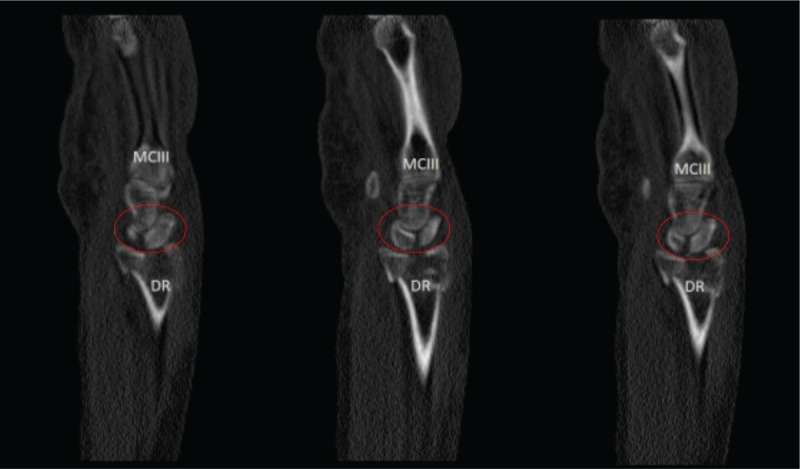
Preoperative 3-dimensional computed tomography image showing left distal radius fracture and lunate fracture (MCIII. third metacarpal bone DR. distal radius).
Figure 3.

Good reduction and internal fixation of the distal radius and lunate in the presented case.
Figure 4.

Distal radius fracture and lunate fracture healed well with good internal fixation in the presented case (6 postoperative weeks).
Figure 5.

Bony union of the distal radius fracture and lunate fracture in the presented case (24 postoperative weeks).
Figure 6.

Patient's wrist function returned to normal (24 postoperative weeks).
Figure 7.

Patient's wrist function returned to normal (1 postoperative year).
A written informed consent was obtained before the submission of the manuscript.
3. Discussion
In 1921, Roth reported the first case of lunate fracture.[6] Commonly, lunate fractures do not exist on their own, perilunate fracture-dislocations are most common, representing 70% to 90% of all related injuries.[5] To our best knowledge, this is the first report on lunate fracture with Colles’ fracture without obvious ligament injury, perilunate fracture-dislocations, and bone shift.
The lunate bone receives its blood supply from dorsal and palmar branches only in a small periosteum-covered area, as classified to Y, I, X, and simple palmar types.[7] Untreated lunate fractures are prone to ischemic necrosis.[8] Regardless of the blood supply type, in the present case, the fracture line passed through the lunate bone at the coronal plane, which may lead to ischemic necrosis if undiagnosed. The lunate bone forms a joint with the radius and carpals. If peripherization of the blood supply occurs, ischemic necrosis or surface cartilage destruction follows, and trabecular bone collapse ensues under continuous stress, leading to Kienbock's disease, and arthritis arises with persistent wrist pain and dysfunction.[2]
Based on the “greater and lesser arc injury” theory, Bain pointed out the theory of “translunar arc injury”,[9] which explained well the injury mechanism of translunate, perilunate fracture-dislocation. However, no consensus has been reached on the injury mechanism of lunate fractures without perilunate fracture-dislocation, which is mainly concerned with shear and axial stress[4,10] Carpal bone injuries are often determined by wrist position and injury strength.[11] The lunate has broad palmar surface, narrow dorsal surface, and palmar tilt on distal surface. The wrist joint, at the time of injury, is extremely outstretched and ulnarly deviated, causing pressure from the palmar side to concentrate on the lunate,[12] the proximal end of which also bears the impact from the dorsal lip.[13] The size and direction of forces are related to the shape of the fractures. Teisen–Hjarbaek classified lunate bone fractures into 5 groups according to their radiographic appearances.[2] The complex structure of the wrist ligament is an important intrinsic factor in lunate fracture occurrence. Our reported case is very rare and defined as Teisen–Hjarbaek type V, which accounts for only 5.8% of the total lunate fractures.[2] The mechanism of the injury may be as follows: when the wrist joint is landed on, lunate fractures are triggered by the simultaneous impact from the capitate bone and dorsal lip of the radius under axial stress. Under a high-intensity stress, the lunate bone is more vulnerable than the ligament;[14] hence, the ligament structure is still intact, and there is no marked dislocation and fracture displacement.
Accurate diagnosis of fresh lunate fractures has been considered a difficult clinical problem. Lunate fractures are often misdiagnosed in the emergency department as common sprains or masked by concurrent injuries.[3,5] This is mainly because
-
1)
almost 80% of the lunate bone surface is covered by articular cartilages, resulting in the absence of sensation after injury;[15]
-
2)
the main part of the lunate is surrounded by the dorsal lip of the distal radius, which cannot be palpated directly with unclear typical positioning signs;[16]
-
3)
finding lunate fractures by traditional radiography is difficult because of overlapping carpal bones;[5,17] and
-
4)
examiners only pay attention to other fractures but ignore the examination of the lunate.[3]
Definitive diagnosis of fresh lunate fractures should depend on CT, MRI, and bone scans.[17] In the present case, the fracture line passed along the coronal position through the lunate body and was not discovered by traditional radiography. Moreover, the physician ignored the examination of the carpal bone at the first visit. Eventually, we accidentally discovered a lunate fracture in this patient during the 3-dimensional CT of her left wrist joint.
No consensus has been made on the treatment of lunate fractures. Conservative treatment was most common in previous studies, and surgery was only considered to prevent ischemic necrosis due to palmar fractures.[2,7] Translunate, perilunate fracture-dislocations are characterized by severe cartilage injury, difficulty in anatomic reduction and fixation, and difficulty in ligament repair. Surgery is often performed, but long-term function is unsatisfactory.[4,9] In recent years, scholars increasingly advocate that surgical treatment is recommended even in cases without perilunate fracture-dislocations. More importantly, ORIF with K-wire or screw should be considered in cases of Teisen–Hjarbaek types IV and V.[14] Teisen–Hjarbaek type II cases can be treated with ligament repair after bone removal.[18] Dana successfully treated fresh lunate fractures with scapholunate ligament injury under wrist arthroscopy.[19] The present case did not involve a perilunate fracture-dislocation and had no apparent displacement of the bone mass. Considering that the wrist ligament plays an important role in the stability and function of the wrist joint, a CRIF with K-wire was therefore selected to prevent ligament injury and interruption of the blood supply due to excessive dissection. Ultimately, after active functional exercise, the patient achieved satisfactory outcomes in fracture healing and functional recovery.
In conclusion, lunate fractures have no characteristic clinical signs and have a low incidence but high misdiagnosis rate. Moreover, the consequences of missed diagnosis are serious. Patients suffering persistent wrist swelling after a trauma should be carefully examined and followed up. If necessary, CT and MRI should be performed to prevent severe secondary diseases and wrist joint dysfunction.
Author contributions
Conceptualization: Dankai Wu, Rui Li.
Data curation: Wenlai Guo, Baoming Yuan.
Investigation: Baoming Yuan, Zhe Zhu, Dankai Wu, Rui Li.
Methodology: Wenlai Guo, Baoming Yuan.
Resources: Chao Huang.
Software: Wenlai Guo, Baoming Yuan, Zhe Zhu.
Supervision: Rui Li.
Visualization: Wenlai Guo, Chao Huang.
Writing – original draft: Wenlai Guo.
Writing – review & editing: Dankai Wu, Rui Li.
Wenlai Guo orcid: 0000-0002-3494-9076.
Footnotes
Abbreviations: CRIF = closed reduction and internal fixation, CT = computed tomography, ORIF = open reduction and internal fixation.
The authors have no conflicts of interest to disclose.
References
- [1].Dennis H, Sze A, Murphy D. Prevalence of carpal fracture in Singapore. J Hand Surg Am 2011;36:278–83. [DOI] [PubMed] [Google Scholar]
- [2].Teisen H, Hjarbaek J. Classification of fresh fractures of the lunate. J Hand Surg Br 1988;13:458–62. [DOI] [PubMed] [Google Scholar]
- [3].Briseño MR, Yao J. Lunate fractures in the face of a perilunate injury: an uncommon and easily missed injury pattern. J Hand Surg Am 2012;37:63–7. [DOI] [PubMed] [Google Scholar]
- [4].Shin DH, Shin AY. Volarly displaced transscaphoid, translunate, transtriquetrum fracture of the carpus: case report. J Hand Surg Am 2014;39:1507–11. [DOI] [PubMed] [Google Scholar]
- [5].Amaravati RS, Saji MJ, Rajagopal HP. Greater arc injury of the wrist with fractured lunate bone: a case report. J Orthop Surg 2005;13:310–3. [DOI] [PubMed] [Google Scholar]
- [6].Roth PB. Fracture of right semilunar bone. Proc R Soc Med 1921;14:55–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Gelberman RH, Gross MS. The vascularity of the wrist: identification of arterial patterns at risk. Clin Orthop Relat Res 1986;202:40–9. [PubMed] [Google Scholar]
- [8].Vasireddy A, Lowdon I. Lunate fracture in an amateur soccer player. J Orthop Sports Phys Ther 2009;39:884. [DOI] [PubMed] [Google Scholar]
- [9].Bain GI, Mclean JM, Turner PC, et al. Translunate fracture with associated perilunate injury: 3 case reports with introduction of the translunate arc concept. J Hand Surg Am 2008;33:1770–6. [DOI] [PubMed] [Google Scholar]
- [10].Takase K, Yamamoto K. Unusual combined scaphoid and lunate fracture of the wrist: a case report. J Hand Surg Am 2006;31:414–7. [DOI] [PubMed] [Google Scholar]
- [11].Mayfield JK. Mechanism of carpal injuries. Clin Orthop 1980;149:45–54. [PubMed] [Google Scholar]
- [12].Lohan D, Cronin C, Meehan C, et al. Injuries to the Carpal Bones Revisited. Curr Probl in Diagn Radiol 2007;36:164–75. [DOI] [PubMed] [Google Scholar]
- [13].Ong JC, Devitt BM, O'Sullivan ME. Impaction-fracture of the capitate and lunate: a case report. J Orthop Surg 2012;20:243–5. [DOI] [PubMed] [Google Scholar]
- [14].Noble J, Lamb DW. Translunate scapho-radial fracture. A case report. Hand 1979;11:47–9. [DOI] [PubMed] [Google Scholar]
- [15].Brolin I. Post-traumatic lesions of the lunate bone. Acta Orthop Scand 1964;34:167–82. [DOI] [PubMed] [Google Scholar]
- [16].Graham B. The wrist. Diagnosis and operative treatment. J Hand Surg 1998;26:165–6. [Google Scholar]
- [17].Nierkens CM, Be VDH. Simultaneous fracture dislocation of the hamate, lunate fracture and scapholunate ligament lesion. J Hand Surg Eur Vol 2013;38:1005–6. [DOI] [PubMed] [Google Scholar]
- [18].Pan KL, Masbah O, Razak M. Rare combination of seven fractures in the same forearm and wrist. Med J Malaysia 2000;55:268–70. [PubMed] [Google Scholar]
- [19].Dana C, Doursounian L, Nourissat G. Arthroscopic treatment of a fresh lunate bone fracture detaching the scapholunate ligament. Chir Main 2010;29:114–7. [DOI] [PubMed] [Google Scholar]


