Abstract
This study is to investigate the role of cervical morphology evaluated by magnetic resonance imaging (MRI) in predicting invasive placenta previa (IPP).
Totally 105 cases of pregnant women underwent prenatal placental MRI at 32 to 36 weeks of gestation for suspected IPP were included in this study. Cervical morphology (cervical length and placental protrusion) was evaluated independently by 2 radiologists. The association between the cervical morphology and surgery findings was analyzed.
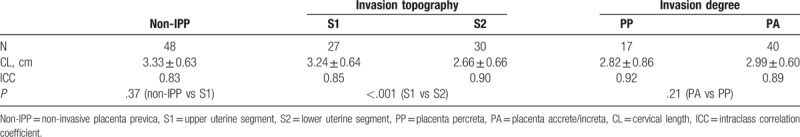
Totally, 57 pregnant women were confirmed as IPP. For invasion degree, there were 17 cases with placenta percreta and 40 with accreta. For invasion topography, there were 27 cases with S1 invasion and 30 with S2 invasion. The sensitivity and specificity for the MRI sign of placental protrusion in evaluating cervical invasion of IPP were 100% and 100%, respectively. All the 7 IPP patents with cervical invasion received total hysterectomy and had severe blood loss (3500–6000 mL). The IPP patients with S2 invasion had shorter cervical length than those with S1 invasion (2.66 ± 0.66 cm vs 3.24 ± 0.64 cm, P <.001). However, cervical lengths did not correlate with the degree of invasion (placenta percreta vs placenta accreta: 2.82 ± 0.86 vs 2.99 ± 0.60, P = .21).
Placental protrusion is a reliable MRI sign for cervical invasion of IPP, and cervical lengths correlate with the invasion topography.
Keywords: cervical invasion, cervical lengths, invasive placenta previa (IPP), magnetic resonance imaging (MRI)
1. Introduction
Invasive placenta refers to a spectrum of disease characterized by abnormal adherent placenta in the uterus, which is also known as placenta accreta, increta, or percreta.[1] The specific pathogenic mechanisms for invasive placenta have not yet been fully established, however, previous cesarean section and placenta previa have been recognized as 2 of the most vital risk factors for invasive placenta.[2–4] Over the past decades, the incidence of invasive placenta has dramatically increased, along with the increasing rate of cesarean delivery.[4] Invasive placenta can prevent placenta from completely separating from the uterus during delivery, which would potentially result in life-threatening intra- or post-partum uterine hemorrhage. A multidisciplinary team (a combination of gynaecology, obstetrics, urology, radiology, obstetric anesthesia, and blood banking) is always recommended to reduce the risk of maternal morbidity and mortality.
Magnetic resonance imaging (MRI) is featured by large field view, satisfactory soft-tissue contrast, and multi-planar imaging. It has been increasingly applied in the evaluation of invasive placenta in recent years. Numerous previous studies have focused on the performance of MRI in diagnosing invasive placenta and the role of MRI signs in the disease prediction.[5–10] Besides, the placental MRI can also characterize the topography of invasive placenta.[11]
It has been shown that the cervical length has a vital impact on the clinical outcomes of patients undergoing peripartum hysterectomy due to placenta previa/percreta.[12] However, the cervical morphology of invasive placenta previa (IPP) is less studied. Therefore, the purpose of our study is to investigate the role of cervical morphology evaluated by MRI in predicting IPP.
2. Materials and methods
2.1. Study patients
Totally 105 cases of pregnant women at 32 to 36 weeks of gestation undergoing prenatal placental MRI examination for suspected IPP in our hospital, from April 2010 to May 2014, were included in this study. Inclusion criteria: patients with gestational age between 32 and 36 weeks, placenta previa, and complete placental MRI images were included. Patients with multiple pregnancies, poor image quality, and incomplete surgical records were excluded. No fetal or maternal sedation was used for the examination. Informed consents were obtained from patients and the study was approved by the ethics review board of our hospital.
2.2. MRI examination
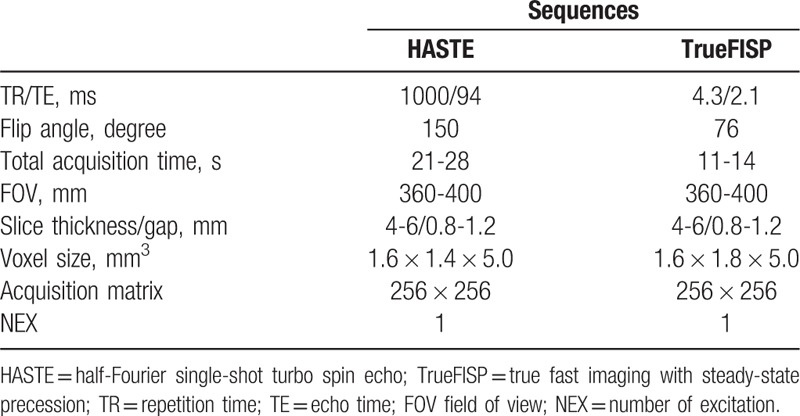
MRI examination was performed on a 1.5-T MR system (Magnetom Sonata, Siemens Healthcare, Erlangen, Germany) with body and spine array coils. Patient was in a supine or left-lateral position, with moderately full bladder. Axial, coronal, and sagittal half-Fourier single-shot turbo spin echo imaging (HASTE), and true fast imaging with steady-state precession sequence (True FISP) were conducted. Intravenous gadolinium injection was avoided for all the patients. The acquisition parameters for all the sequences were shown in Table 1.
Table 1.
MRI parameters in this study.
2.3. MR imaging analysis
Two experienced radiologists, blinded to the surgical findings, evaluated the cervical morphology (the cervical length and the sign of placental protrusion). The MRI sign of placental protrusion was defined as placental protrusion into the internal os.[13] The measurement of cervical length was showed in Figure 1.
Figure 1.
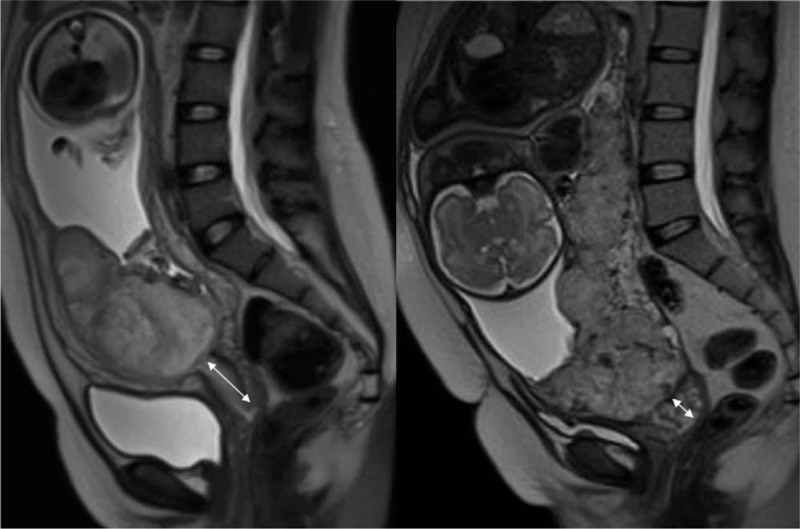
The measurement of cervical lengths. The image of non-invasive placenta previa (from a 30-year-old woman at 34-week gestation) was shown on the left panel and that of IPP with S2 invasion (from a 32-year-old woman at 34-week gestation) was shown on the right panel. Arrows indicate the measurement of cervical lengths.
2.4. Standard of reference
The degree of IPP was defined based on the previously published surgical and/or pathologic criteria.[5,14,15] Confirmation of placenta percreta was based on surgical and/or pathological evidence of gross placenta/villi fully penetrating through the myometrium and invading the uterine serosa or even extrauterine structures. Confirmation of placenta accreta/increta was based on surgical and/or pathological evidence of placental adhesion to or invasion into the myometrium with intact uterine serosa. If the placenta is easily removed during cesarean delivery without massive bleeding, it should be considered as non-invasive.[15] For clinical relevance and statistical analysis, we used “placenta accreta” as an umbrella term for placenta accreta and increta. The topography of IPP, which included upper uterine segment (S1) and lower uterine segment (S2), was confirmed according to clinical and anatomical criteria in the surgical records.[11,16] For the cases of combined S1 and S2 invasions, the group was assigned according to the higher percentage of invasion.
2.5. Statistical analysis
SPSS software (version 21.0) was used for statistical analysis. Inter-rater reliability of the cervical lengths between the 2 radiologists was assessed by the intra-class correlation coefficient. Sensitivity and specificity for MRI in evaluating cervical invasion were calculated. The association between the cervical lengths and surgery findings (invasion topography and invasion degree) was analyzed by independent-samples t test. P <.05 was considered statistically significant.
3. Results
3.1. Basic information and obstetrical data of study patients
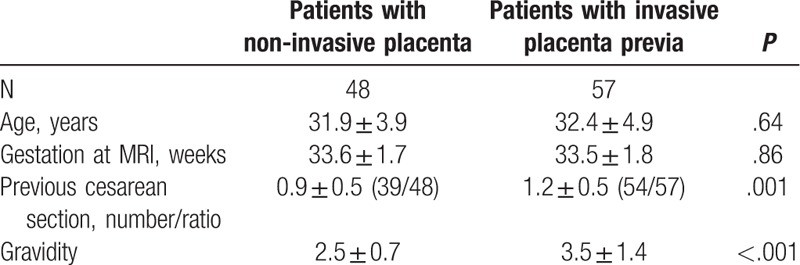
Out of the totally 105 subjects, there were 57 patients who were confirmed as IPP. For invasion degree, there were 17 cases with placenta percreta and 40 with accreta. For invasion topography, there were 27 cases with S1 invasion and 30 with S2 invasion. There were 7 cases of IPP with placenta involved in the cervix. There was no significant difference in the age and gestation week at MRI between patients with IPP and those with non-IPP. The difference of the gestation week at MRI between IPP patients with S1 and S2 invasions was not significant (P = .64). The average times of previous cesarean section and pregnancy of IPP patients were significantly higher than those of non-IPP patients (P < .05). All the obstetrical data were listed in Table 2.
Table 2.
Obstetrical data of the study subjects.
3.2. Relationship between cervical morphology and surgical findings
To investigate the relationship between cervical lengths and invasion topography, the cervical lengths between the S1 and S2 involvement were compared (Fig. 2). Compared with patients with S1 involvement, the cervical lengths of patients with S2 involvement were significantly shorter (2.66 ± 0.66 cm vs 3.24 ± 0.64 cm; P <.001). However, there were no significant differences in the cervical length between the patients with S1 invasion and patients with non-IPP (P = .37). Moreover, no significant differences in the cervical lengths were observed between the patients with placenta percreta and with placenta accreta (i.e., accreta and increta) (P = .21) (Table 3), suggesting that cervical lengths are not related with the degree of invasion. Inter-rater reliability of the cervical lengths between the 2 radiologists was good (P >.75).
Figure 2.
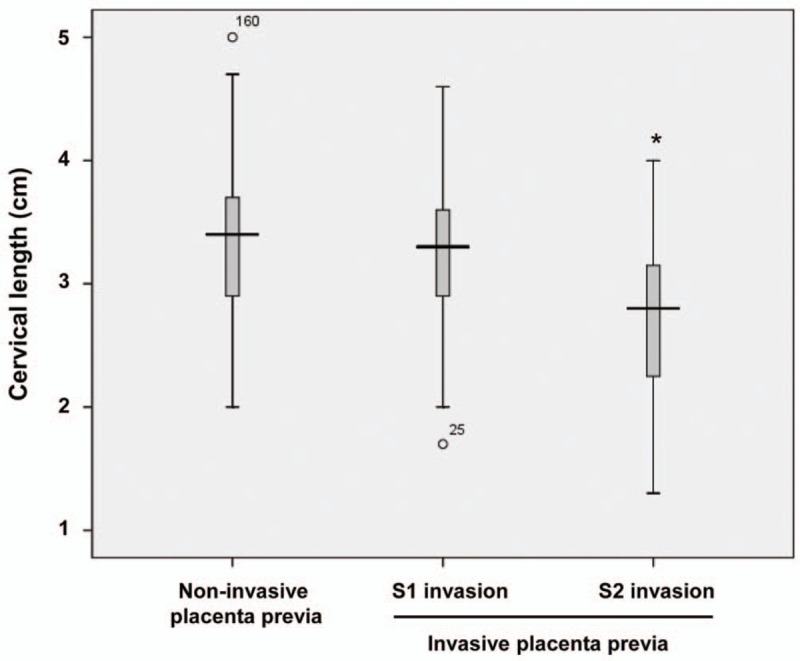
Cervical length in non-invasive placenta previa, S1 and S2 invasive placenta previa between 32 and 36 weeks of gestation. Compared S1 involvement, ∗P <.05.
Table 3.
The cervical lengths evaluated by 2 radiologists.
Importantly, our results showed that the 7 cases of IPP with cervical invasion exhibited the MRI sign of placental protrusion (Fig. 3). The sensitivity and specificity for placental protrusion in evaluating cervical invasion were 100% and 100%, respectively. All the 7 IPP patients with cervical invasion received total hysterectomy with severe blood loss (3500–6000 mL).
Figure 3.
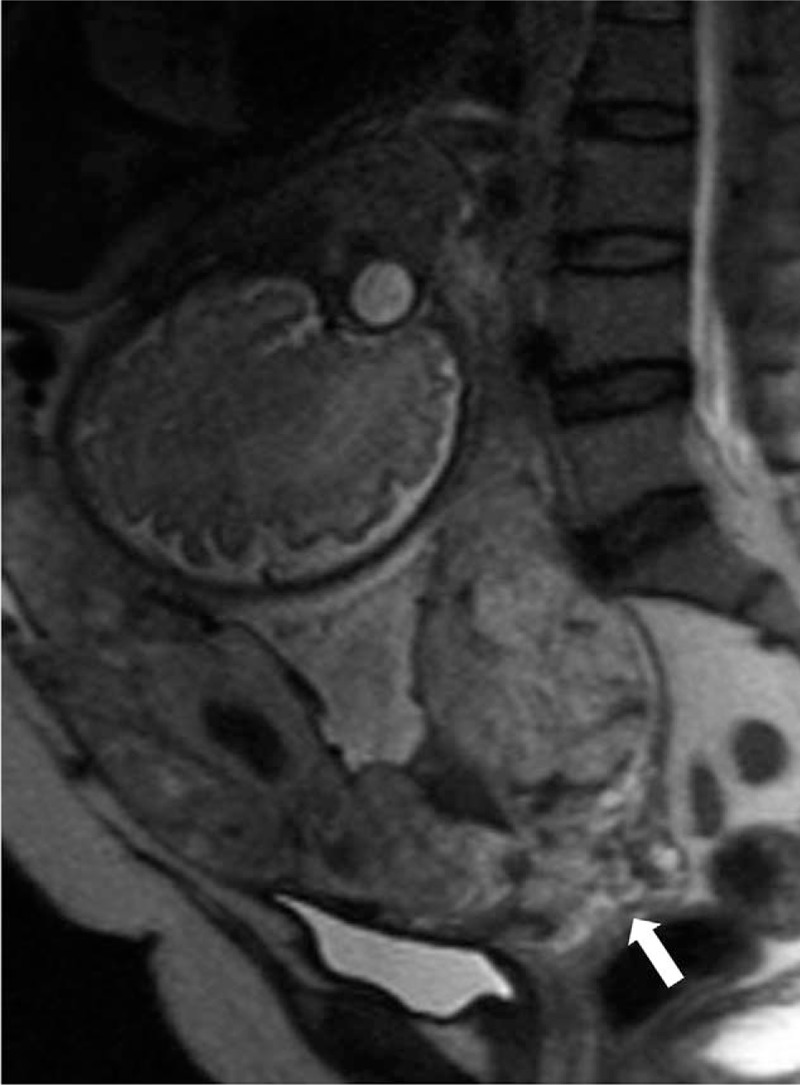
Placenta accreta with cervical invasion in a 35-year-old woman at 35-week gestation. Sagittal HASTE MR image showed placental protrusion (white arrow).
4. Discussion
The results of this study demonstrate that placental protrusion is a reliable MRI sign for cervical invasion of IPP. Moreover, the patients with S2 invasion had shorter cervical length than those with S1 invasion, indicating that cervical lengths of IPP are related with invasion topography.
Although rarely seen, placenta previa could significantly increase the maternal and fetal morbidity and mortality.[17] Up to now, the capability of MRI in diagnosing the cervix invasion of placenta is less studied. A previous study reported a case of cervical invasion with MRI, which suggests abnormal zonal anatomy of cervix.[18,19] In our study, all the 7 patients with cervical invasion exhibited placental protrusion, and the placental protrusion was found to be a reliable MRI sign for cervical invasion. A previous study found that placental protrusion was an MRI finding for diagnosis of IPP.[13] However, this study did not explore the role of placental protrusion in diagnosing cervical invasion. These 7 patients received total hysterectomy and had severe blood loss, which indicates that cervical invasion can deteriorate the maternal outcomes.
The topography of IPP has been shown to be significantly different depending on the possibility of uterine conservation, hysterectomy, and blood transfusion volume.[11] The S1 is irrigated by the uterine and upper vesical vessels, which are generally of easy access and adequate hemostasis. However, S2 has anastomotic irrigation, and these irrigating vessels are deeply located, which significantly increase the surgical complexity and the possibility of massive hemorrhage. Therefore, the topographic findings of IPP are essential for the disease management and surgical treatment. Palacios et al[11] have analyzed the diagnostic images and surgical findings of placenta accreta, and have suggested that MRI is essential to delineate the topography of placental invasion.[20] What is more, short cervix appears to be one of the warning signs for elevated difficulty in the operations for placenta previa/percreta.[12] A previous ultrasound study showed that women with IPP had shorter cervical lengths at 32 to 34 weeks than women with a non-adherent low-lying placenta or placenta previa.[21] Our results showed that patients with the S2 involvement had shorter cervical lengths than the patients with the S1 invasion. Measurement of cervical lengths could help to depict the S2 invasion and increase the accuracy of topographic evaluation. However, no significant differences were observed in the cervical lengths between the patients with the S1 invasion and non-invasive placenta, nor between the patients with placenta percreta and non-placenta percreta. These results indicate that the cervical length is related to the topography of IPP, rather than the degree of IPP. It is of great importance to pay attention to the cervical lengths in the clinical treatment of IPP. In general, the treatment plan did not differ between placenta accreta and increta. Therefore, our study did not distinguish placenta accreta from increta.[22] In addition, the placental or placental-myometrial specimen was not always intact, and superficial placenta increta may be partly misdiagnosed as placenta accreta during surgery or pathological examination. In our study, placenta accreta and increta were grouped and analyzed together, which would reduce the effects of misdiagnoses.
There are also some limitations for our study. First, only 7 patients with cervical invasion were enrolled in this study, and the MRI features of cervical invasion are still needed to be further investigated. Second, the MRI findings were not compared with the results from the ultrasound detection. Third, all the patients herein were suspected for IPP, resulting in the high IPP rate.
In conclusion, placental protrusion was a reliable MRI sign for cervical invasion of IPP, and cervical lengths were related with the invasion topography. Our findings might facilitate the adequate preoperative preparation and multidisciplinary management of IPP in clinic.
Author contributions
GW designed the research. WL, XC, CS, and XW collected the cases. RS assessed the data. WL, XC, and GW performed statistical analysis. WL prepared the manuscript. XC, GW, and RS revised the manuscript. All authors have read and approved the final version of the manuscript to be submitted.
Conceptualization: Wen Liu, Guangbin Wang.
Data curation: Ruiqin Shan.
Investigation: Wen Liu, Xin Chen, Cong Sun, Xinhong Wei.
Software: Wen Liu, Xin Chen, Guangbin Wang.
Writing – original draft: Wen Liu.
Writing – review & editing: Xin Chen, Guangbin Wang, Ruiqin Shan.
Footnotes
Abbreviations: IPP = invasive placenta previa, MRI = magnetic resonance imaging.
This work was supported by the National Natural Science Foundation of China (No. 81371534 and No. 81171380).
Authors have no conflicts of interest to disclose.
References
- [1].FG C. Obstetrical hemorrhage. New York: McGraw-Hill; 2010. [Google Scholar]
- [2].Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol 1997;177:210–4. [DOI] [PubMed] [Google Scholar]
- [3].Silver RM, Landon MB, Rouse DJ, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol 2006;107:1226–32. [DOI] [PubMed] [Google Scholar]
- [4].Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol 2005;192:1458–61. [DOI] [PubMed] [Google Scholar]
- [5].Bour L, Place V, Bendavid S, et al. Suspected invasive placenta: evaluation with magnetic resonance imaging. Eur Radiol 2014;24:3150–60. [DOI] [PubMed] [Google Scholar]
- [6].Derman AY, Nikac V, Haberman S, et al. MRI of placenta accreta: a new imaging perspective. AJR Am J Roentgenol 2011;197:1514–21. [DOI] [PubMed] [Google Scholar]
- [7].Kim JA, Narra VR. Magnetic resonance imaging with true fast imaging with steady-state precession and half-Fourier acquisition single-shot turbo spin-echo sequences in cases of suspected placenta accreta. Acta Radiol 2004;45:692–8. [DOI] [PubMed] [Google Scholar]
- [8].Lax A, Prince MR, Mennitt KW, et al. The value of specific MRI features in the evaluation of suspected placental invasion. Magn Reson Imaging 2007;25:87–93. [DOI] [PubMed] [Google Scholar]
- [9].Maldjian C, Adam R, Pelosi M, et al. MRI appearance of placenta percreta and placenta accreta. Magn Reson Imaging 1999;17:965–71. [DOI] [PubMed] [Google Scholar]
- [10].Teo TH, Law YM, Tay KH, et al. Use of magnetic resonance imaging in evaluation of placental invasion. Clin Radiol 2009;64:511–6. [DOI] [PubMed] [Google Scholar]
- [11].Martinez M. Magnetic resonance imaging in 300 cases of placenta accreta: surgical correlation of new findings. Acta Obstet Gynecol Scand 2006;85:377. [PubMed] [Google Scholar]
- [12].Polat M, Kahramanoglu I, Senol T, et al. Shorter the cervix, more difficult the placenta percreta operations. J Matern Fetal Neonatal Med 2016;29:2327. [DOI] [PubMed] [Google Scholar]
- [13].Ueno Y, Kitajima K, Kawakami F, et al. Novel MRI finding for diagnosis of invasive placenta praevia: evaluation of findings for 65 patients using clinical and histopathological correlations. Eur Radiol 2014;24:881–8. [DOI] [PubMed] [Google Scholar]
- [14].Oyelese Y, Smulian JC. Placenta previa, placenta accreta, and vasa previa. Obstet Gynecol 2006;107:927–41. [DOI] [PubMed] [Google Scholar]
- [15].Sentilhes L, Gromez A, Clavier E, et al. Long-term psychological impact of severe postpartum hemorrhage. Acta Obstet Gynecol Scand 2011;90:615–20. [DOI] [PubMed] [Google Scholar]
- [16].Palacios Jaraquemada JM, Pesaresi M, Nassif JC, et al. Anterior placenta percreta: surgical approach, hemostasis and uterine repair. Acta Obstet Gynecol Scand 2004;83:738–44. [DOI] [PubMed] [Google Scholar]
- [17].Lin CC, Adamczyk CJ, Montag AG, et al. Placenta previa percreta involving the left broad ligament and cervix: a case report. J Reprod Med 1998;43:839–43. [PubMed] [Google Scholar]
- [18].Leyendecker JR, DuBose M, Hosseinzadeh K, et al. MRI of pregnancy-related issues: abnormal placentation. AJR Am J Roentgenol 2012;198:311–20. [DOI] [PubMed] [Google Scholar]
- [19].Mar WA, Berggruen S, Atueyi U, et al. Ultrasound imaging of placenta accreta with MR correlation. Ultrasound Q 2015;31:23–33. [DOI] [PubMed] [Google Scholar]
- [20].Masselli G, Brunelli R, Casciani E, et al. Magnetic resonance imaging in the evaluation of placental adhesive disorders: correlation with color Doppler ultrasound. Eur Radiol 2008;18:1292–9. [DOI] [PubMed] [Google Scholar]
- [21].Rac MW, Mcintire DD, Wells CE, et al. Cervical length in patients at risk for placenta accreta. J Ultrasound Med Off J Am Inst Ultrasound Med 2017;36:1431–6. [DOI] [PubMed] [Google Scholar]
- [22].Kilcoyne A, Shenoy-Bhangle AS, Roberts DJ, et al. MRI of placenta accreta, placenta increta, and placenta percreta: pearls and pitfalls. AJR Am J Roentgenol 2017;208:214–21. [DOI] [PubMed] [Google Scholar]


