Abstract
In clinical practice, we found a unilateral instability in patients with right thoracic scoliosis during asymmetric spinal stabilization exercise (ASSE), which can be an important clue to identify the pathophysiology of idiopathic scoliosis (IS).
We investigated the relationship between unilateral postural instability and weakness of paraspinal muscles according to curve pattern. And finally, we propose the new exercise method based on the curve pattern.
Combined use of prospective and retrospective clinical trials.
Fifteen participants without IS and 10 patients with IS in 1 tertiary referral hospital.
In 15 participants without IS, surface electromyography (sEMG) was used to evaluate the muscular activation patterns in the bilateral erector spinae (ES), rectus abdominis (RA), and external oblique (EO) muscles during ASSE. In addition, to assess the clinical effect of ASSE, Cobb angle and rotation grade were measured from 10 patients with IS.
The most significant findings from the sEMG data were the increased activities of ipsilateral 7th thoracic ES during hand-up motion, ipsilateral 3rd lumbar ES during leg-up motion, and 12th thoracic and 3rd lumbar ES during side-bridging. In a radiographic analysis, specific components of ASSE that activates the concave side muscles were found to be effective for IS.
The paraspinal muscle strengthening of the concave side using ASSE can improve the severity of scoliosis. Based on this research, we could propose a new exercise protocol that can be personalized according to the curve pattern.
Keywords: exercise therapy, idiopathic scoliosis, rehabilitation, spinal curvatures, spinal disease
1. Introduction
Scoliosis is classified by whether it has a specific cause. Disorders of the central or peripheral nervous system, neuromuscular disease, and myopathy are well-known causes.[1] Aside from these causes, most scoliosis are idiopathic, despite some recent studies suggesting genetic predisposition, connective tissue problem, and asymmetric spinal growth related with abnormal muscle action as potential causes.[2]
There has been much effort in recent years to understand the causes of idiopathic scoliosis (IS). Some studies suggested muscle imbalance as a cause of scoliosis based on asymmetric muscular activation.[3,4] Although these findings are not observed in several other studies,[5] muscle imbalance is still thought to be a possible cause of scoliosis.
Treatment of IS can be addressed in several ways, such as exercise, brace, and surgery.[1] Many studies have shown controversial results with respect to non-surgical interventions, like the use of braces and exercise therapy.[6] Reports analyzing the previously published review articles about treatments of IS have concluded that the effectiveness of exercise therapy for correcting scoliosis cannot be determined.[6–8] Exercise therapy has only been proven to be effective for managing chronic low back pain.
We noticed some important findings during our clinical practice. While teaching asymmetric spinal stabilization exercises (ASSE) to patients with IS for the prevention and reduction of back pain,[9,10] we noticed that they were unable to maintain a specific posture on one side, but they were able to do so on the contralateral side. For example, patients showing right thoracic scoliosis were unable to maintain a bird-dog posture with holding the left hand and right leg up (Fig. 1, Type II (C)). Patients with scoliosis at the lumbar level that convex to left side also showed instability while maintaining at bird-dog posture with right leg up (Fig. 1, Type II (B)). These patients also showed upper extremity weakness at the thoracic concave side (Fig. 1, Type I (A), (D), II (A)) and leg weakness at the lumbar concave side while maintaining a posture with both hands and legs raised (Fig. 1, Type I (B), (D), II (B)).
Figure 1.
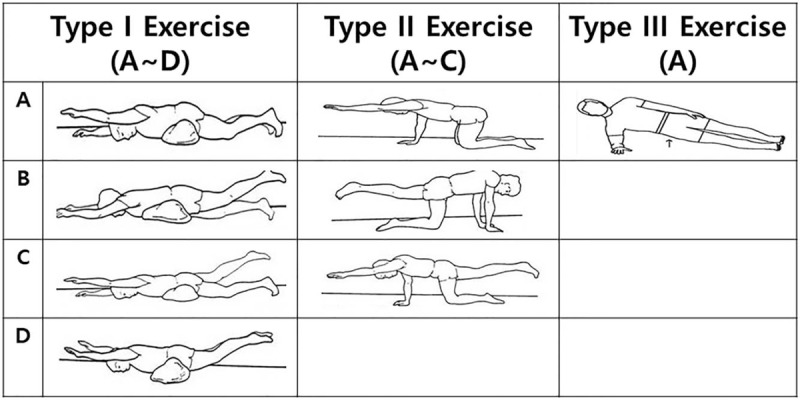
This figure shows the asymmetric spinal stabilizing exercise (ASSE) from the in dividualized graded lumbar stabilization exercise. Type I exercise consists of 4 movements in prone position. Type II exercise is composed of 3 movements in quadruped position. Type III exercise is known as the so-called side bridging exercise.
Previous studies supported our findings. These studies revealed a decrease in the number of slow-twitch muscle fibers[11] and a reduction in the bioelectric activity measured by surface electromyography (EMG) on the concave side of the spinal curvature.[4,12] In other words, asymmetric muscular weaknesses might be correlated with the development and aggravation of IS.
Therefore, our first hypothesis is that postural instability was due to concave side muscle weakness and strengthening of concave side muscles could be helpful to prevent and improve scoliosis. The second hypothesis is that ASSE may have a corrective effect on scoliosis in plane radiography if ASSE can strengthen the weak paraspinal muscles.
The first purpose of this study is to find out which paraspinal muscles were activated during a specific posture that could not be sustained in a typical right-sided thoracic scoliosis patient. This process can be useful for understanding the relationship between postural instability and weakness of paraspinal muscles of concave side. The second, in order to evaluate the clinical efficacy of ASSE, counter-directional motion of ASSE was performed and the change of Cobb angle with direction was measured in patients with IS. Finally, based on the results of the 2 steps mentioned above, we try to develop an exercise protocol for IS using ASSE (prone, quadruped, and side lying exercises), depending on the type of spinal curvature including the location of apex and the direction of convexity. This is a small-scale preliminary pilot study to design curvature specific exercise before a full-scale research project.
2. Materials and methods
2.1. Characteristics of subjects
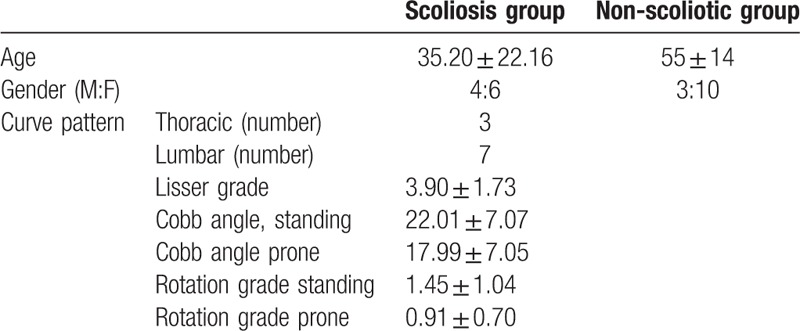
Fifteen subjects without scoliosis, defined as the non-scoliotic group, were included to analyze the muscle activation patterns during ASSE, prospectively. Another group of 10 patients with IS (Cobb angle: 22.0° ± 7.1°, rotation: grade 1.5 ± 1.0), classified as the scoliotic group, were recruited to determine the immediate effect of ASSE. Patients with the following were excluded: history of spinal cord surgery, cerebral palsy, muscular dystrophy, poliomyelitis, congenital spondylosis, mental retardation, and acute back pain. Patient demographic data and baseline status are described in Table 1. The prospective component was part of a clinical trial (NCT02938169) and all procedures were approved by the Institutional Review Board (B-1604–344–004). And the retrospective component was approved by the Institutional Review Board (B-1701–378–103).
Table 1.
Baseline data of scoliotic group and normal control (non-scoliotic) group.
2.2. Assessment
For the consistency of experiment, 1 experienced therapist conducted the tests. At first, we recorded prospectively surface-electromyography (S-EMG) data in the non-scoliotic group during ASSE for quantitative analysis of muscle activation patterns.
The 7th, 12th thoracic, and 3rd lumbar erector spinae were selected, as these levels were the most common curves patterns.[13,14] Before ASSE, in order to reduce the skin resistance, we wiped the skin with alcohol on the electrode attaching area. The electrodes of S-EMG were attached at bilateral 7th, 12th thoracic, 3rd lumbar erector spinae (EST7, EST12, ESL3), rectus abdominis (RA), and external oblique (EO) muscles.
For detecting activity of bilateral 7th, 12th thoracic, 3rd lumbar erector spinae (EST7, EST12, ESL3), active electrodes were attached at 2 cm lateral to the spinous process at T7, T12, and L3 levels. In the sidelying exercise, the activity of the 2 muscles was additionally measured. To analyze rectus abdominis (RA) muscle activity, the active electrodes were placed 3 cm apart and parallel to the muscle fibers of rectus so that they are located approximately 2 cm lateral and across from the umbilicus over the muscle belly. The active electrodes for external oblique (EO) were placed 2 cm apart, lateral to the rectus abdominis and directly above the anterior superior iliac spine.[9]
Patients were asked to maintain a specific posture of the ASSE and the S-EMG data were recorded. Then, the root mean square (RMS) values were calculated for 10 seconds. To evaluate the degree of muscle contraction during exercise, a wireless S-EMG analysis system (BTS FREEEMG 1000 with EMG-BTS EMG-Analyzer, BTS Bioengineering Co., Quincy, MA) was used for electrophysiological quantitative analysis. The S-EMG signals were received from 8 channels, converted into a digital signal, and transmitted to the personal computer wirelessly. The acquisition frequency of the EMG signal was 1024 Hz and we used a bandpass filter between 20 and 500 Hz. And we analyzed the signals by RMS.
Second, in the scoliotic group, a whole spine radiography at anteroposterior and lateral directions were examined at standing position, followed by spine x-rays again at prone position and unilateral hand- or leg-up position. Hand- or leg-up position was determined by the pattern of scoliotic curvature. Hand-up position was used in patients with thoracic curve, while a leg-up position was used in patients with lumbar curve. For the consistency of experiment, the medical staff who had experienced about scoliosis always accompanied the patient to check the posture and the process. Cobb angle and rotation grade (Cobb method) were measured, retrospectively.
2.3. Description of exercise tasks
Before the surface EMG analysis, all subjects were warmed up. The warm-up exercise consisted of a 5-minute walk and full body stretching. After warm-up exercise, we repeatedly performed a specific posture (type I, II, III) of ASSE for 10 to 20 minutes until participants became accustomed. Because ASSE is an easy, simple, and familiar exercise, every participant can be considered an advanced experience through repeated training. Subjects were required to maintain a specific posture according to each type of exercise while performing ASSE.[9,10] The individualized graded lumbar stabilization exercise (IGLSE) is composed of spinal stabilizing exercises at different posture for chronic back pain. This exercise is proven to be effective in strengthening the core muscle around the spine and can easily be carried out without any apparatus.[9,10] This program was based on the condition of each patient, and the degree of difficulty ranged from easy to difficult. Patients gradually increased the degree of instability until the most unstable posture was achieved; this method is advantageous as it is safe and can be personalized.[9,10] ASSE includes the following actions:
2.3.1. Type I exercise
Type I exercise consisted of 4 movements, each of which has a common beginning in the prone position (Fig. 1). Type I (A) motion involved the lifting of the unilateral hand from prone position and maintaining that position. Type I (B) motion involved the lifting of the unilateral leg from prone position and maintaining that position. Type I (C) exercise involved lifting of the unilateral hand and contralateral leg. Finally, Type I (D) motion involved keeping both hands and legs raised. Type I (D) exercise is the only motion with a symmetric component.
2.3.2. Type II exercise
Type II exercise was composed of 3 movements at quadruped position (Fig. 1). Except for the initial preparation position as being quadruped, the 3 types of type II actions (A–C) were performed in the same manner as Type I (A–C) exercises.
2.3.3. Type III exercise
Type III exercise is known as the “side bridging exercise” (Fig. 1). It starts out with the patient lying on the side, while keeping the upper arm perpendicular to the ground and the lower back and the chest on the same line.
2.3.4. Development of exercise protocol for specific curve pattern
As the first step, the scoliosis curve pattern was divided by the number of curves (single or double curve) and locations (mid thoracic, low thoracic, and mid lumbar). Then, we chose and made cluster of exercises that can reinforce the concave side muscle relative to the convex side on the scoliotic curvature. For objective and quantitative analysis, the relative strength of muscles during isometric contraction was calculated using the asymmetric index (AI) based on the RMS value of S-EMG. The formula was: AI = [(RMS ipsilateral – RMS contralateral)/(RMS ipsilateral + RMS contralateral) × 100].[15]
2.3.5. Statistics
For all statistical analyses, SPSS for Windows version 22 was used (SPSS Inc.; Chicago, IL). Kolmogorov–Smirnov and the Shapiro-Wilk tests were done using SPSS for sample normality test. And every variable did not follow the normal distribution (P < .05). Because surface EMG and radiologic outcomes were not normally distributed, the Mann–Whitney U test was used to assess the difference in muscle activity (peak amplitude value and mean RMS value) in both paraspinal muscles according to the ASSE posture. To compare the changes of the scoliotic curvature according to the direction of the ASSE, Wilcoxon method was used to analyze the Cobb angle and grade of rotation in radiographs. P values of <.05 were considered statistically significant. In addition, since we were studying the difference of bilateral muscles in each person, case-control matching was not necessary.
3. Results
3.1. Mean RMS and peak amplitude value of S-EMG data
3.1.1. Type I exercise
During type I (A) exercise, the mean RMS and peak amplitude values measured on the EST7 muscle were significantly increased on the ipsilateral side compared with the contralateral side. In type I (B) exercise, significantly increased mean RMS and peak amplitude in the ipsilateral side of ESL3. In type I (C) exercise, which is a kind of crossed activation exercise (hand-up and opposite side leg-up exercise), the activation at EST7 was significantly increased compared with the contralateral side. Although the ipsilateral side of ESL3 muscle was more activated than the contralateral side, the differences were not significant. In type I (D) exercise, showing symmetric activation pattern, the absolute values of mean RMS and peak amplitude were significantly higher than the other types of exercise (Tables 2 and 3).
Table 2.
Mean RMS values of paraspinal muscles during asymmetric spinal stabilizing exercise (ASSE).
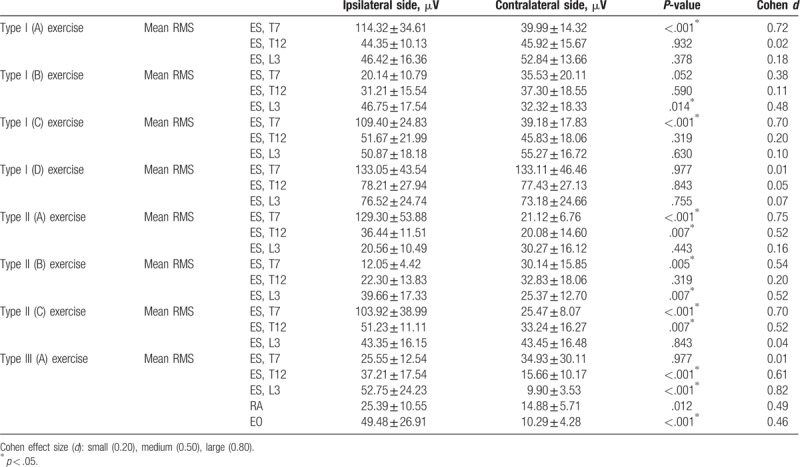
Table 3.
Peak torque values of paraspinal muscles during asymmetric spinal stabilizing exercise (ASSE).
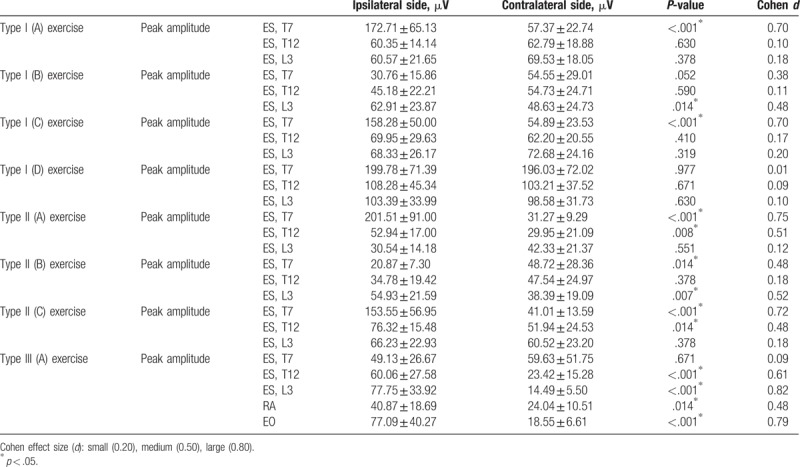
3.1.2. S-EMG data of Type II
Type II exercise was found to induce more selective activation of the T12 level erector muscle than type I exercise. In Type II (A) exercise, the RMS value and peak amplitude of the ipsilateral side of EST12 as well as EST7 muscles were also significantly increased compared with the contralateral side. In type II (B), significantly increased mean RMS and peak amplitude in ipsilateral side of ESL3 and contralateral side of EST7 muscles were observed. In type II (C), significantly increased muscle activities in the ipsilateral side of EST7 and EST12 muscles were observed (Tables 2 and 3).
3.1.3. S-EMG data of Type III
Type III (A) exercise (side bridging exercise) showed a significant increase in the mean RMS and peak amplitude values at the ipsilateral side (dependent portion of side lying position) muscles of EST12, ESL3, RA, and EO. However, the mean RMS and peak amplitude values at EST7 were not statistically significant (Tables 2 and 3).
3.2. Cobb angle and grade of rotation
In the scoliotic group, the Cobb angle and grade of rotation were significantly (P < .05) improved when measured in prone position (Cobb angle: 17.99 ± 7.05°, rotation grade: 0.91 ± 0.70°) than in standing position (Cobb angle: 22.01 ± 7.07°, rotation grade: 1.45 ± 1.04°).
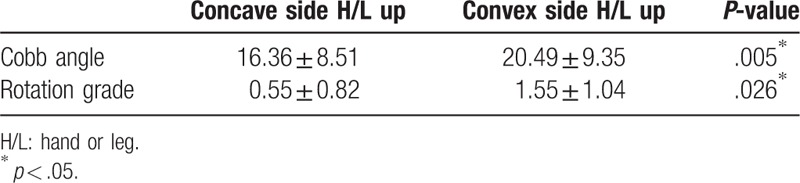
The tendency for worsening or improving scoliotic curvature depended on the laterality of the muscles used during ASSE. Asymmetric components of ASSE which activates the concave side muscles of scoliotic spine were effective for the correction of scoliotic curvature (Fig. 2). Cobb angle and rotation grade showed a statistically significant difference when comparing the concave side hand-up or leg-up exercise (Cobb angle: 16.36 ± 8.51°, rotation grade: 0.55 ± 0.82°) with the convex side hand-up or leg-up exercise (Cobb angle: 20.49 ± 9.35°, rotation grade: 1.55 ± 1.04°) (Table 4).
Figure 2.
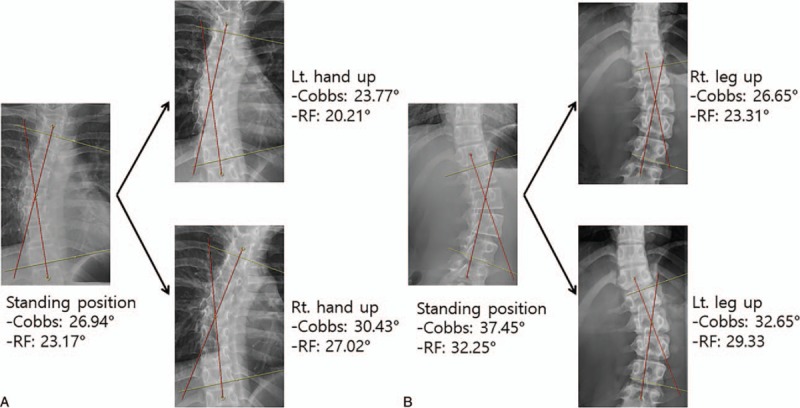
Asymmetric components of asymmetric spinal stabilizing exercise (ASSE) that activate the concave side muscles of scoliotic spine were effective for correcting idiopathic scoliosis.
Table 4.
Difference of Cobb's angle and rotation grade comparing the concave side hand-up or leg-up exercise with the convex side hand-up or leg-up exercise.
3.3. A new exercise protocol for idiopathic scoliosis
Asymmetry index (AI) showed a selective activation in the specific paraspinal muscles (Fig. 3). Using the AI, exercise protocol for specific curve pattern was developed (Ryu scoliosis exercise protocol, Fig. 4).
Figure 3.
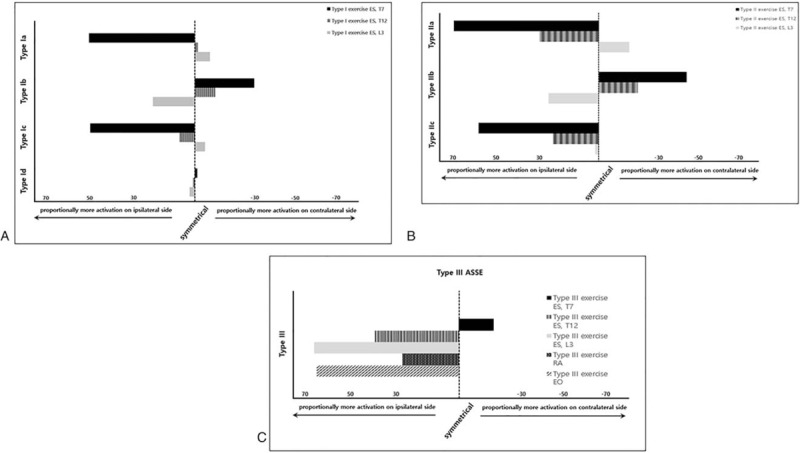
Strength of muscles during ASSE using asymmetric index (AI). (A) Type I (A–D), (B) Type II (A–C), (C) Type III (A). ASSE = asymmetric spinal stabilization exercise.
Figure 4.
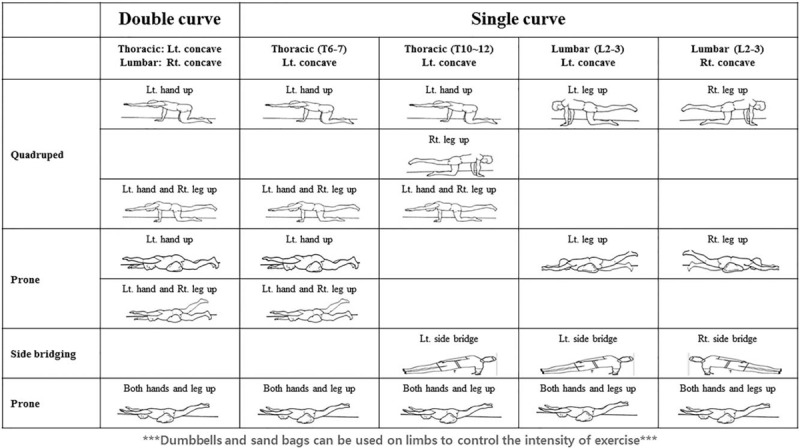
Ryu scoliosis exercise protocol for idiopathic scoliosis using asymmetric spinal stabilizing exercises (ASSE, prone, quadruped, and side lying exercises) depending on the type of spinal curvature. Dumbbells and sand bags can be used on limbs to control the intensity of exercise. ASSE = asymmetric spinal stabilization exercise.
4. Discussion
We hypothesized that postural instability in patients showing Rt. thoracic curve was due to concave side muscle weakness. In the present study, we addressed which muscles worked for postural stability during ASSE using the S-EMG study. These results proven this posture (Fig. 1, Type II (C)) activated significantly left thoracic paraspinal muscles, and suggest the weakness of left thoracic paraspinal muscles resulted postural instability in these patients. In other postures, we found out that ASSE could activate the unilateral side paraspinal and abdominal muscles, selectively.
When we compared the changes of Cobb angle using radiography during ASSE, we observed an improvement in the Cobb angle and rotation grade of the spine during an asymmetric activation of the concave side muscles. These findings imply that asymmetric components of ASSE can activate the specific paraspinal muscles of the desired region and reverse scoliotic curvature. Based on the S-EMG and radiographic findings, we think that strengthening of the concave side paraspinal muscles might improve scoliosis. Follow up studies are required.
Previous studies supported our findings. These studies revealed a decrease in the number of slow-twitch muscle fibers[11] and a reduction in the bioelectric activity on the concave side of the spinal curvature.[3,12] Furthermore, decreased muscle fibers were substituted by connective tissues.[11] In other words, asymmetric muscular weaknesses might be correlated with the development and aggravation of IS, and an activation of the weak side could reverse scoliosis.
However, caution about asymmetric strengthening of the concave side muscles is advised. This was due to the notion that muscle strengthening on the concave side could potentially exacerbate tension on the concave side of the curved spine, which is known as the “bowstring effect.”[16,17] Scoliosis, however, develops at resting standing position, suggesting that the weak paraspinal muscles may not support the spine in a straight position due to loss of muscle fiber. Figure 5 shows how asymmetric weakness provokes scoliosis. The functions of muscles include not only movement, but also maintenance (shaping) of the structure. Therefore, exercise therapy should be focused on the concave side to strengthen and recover the atrophied muscles to keep the spine straight.
Figure 5.
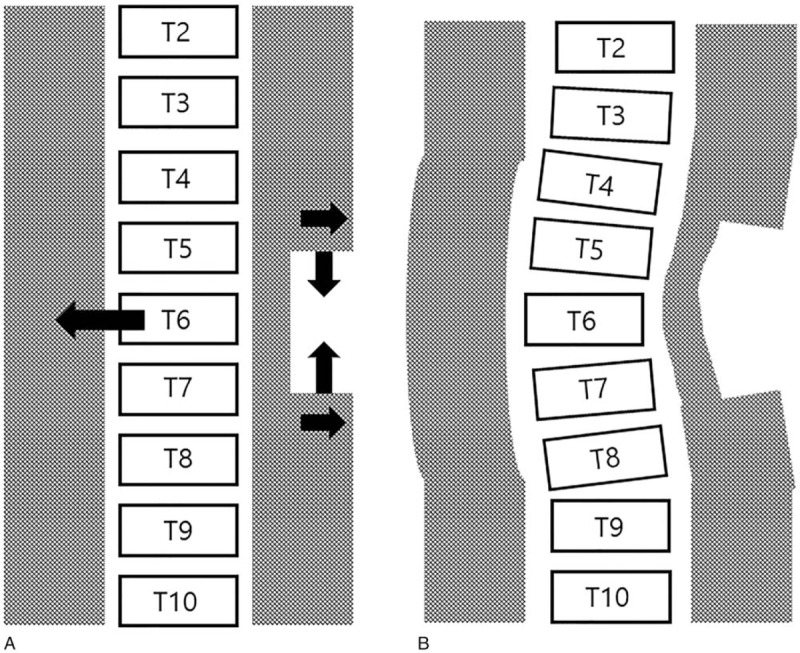
This figure shows how asymmetric weakness provokes scoliosis. Though we often think of muscles acting dynamically around the joints, paravertebral muscles act to keep the spine straight. As you see from this picture, the spine is inclined to the weaker side.
In this study, we observed significant differences of the Cobb angle and rotation grade between the prone and standing positions. These findings suggest that there is a flexible component of IS. This is supported by previous studies; it was shown that there may be flexible causes, such as muscle imbalance, as well as non-flexible causes, such as bony deformity.[3,12] This obviously means that reversible causes, including muscle imbalance, may be a large part of IS.
Until now, diverse physiotherapy scoliosis specific exercises have been used as an exercise therapy for scoliosis. These methods include Lyon approach, the Schroth approach, scientific exercise approach to scoliosis (SEAS), the side-shift approach, and functional individual therapy of scoliosis approach, etc.[18] Several studies have shown that the Schroth approach alleviated back asymmetry in the frontal and transverse plane through improvements in muscle imbalance.[19–21] SEAS, side-shift approach, and Lyon approach also showed a clinically significant outcome.[22–24] However, recent literature review concluded that there is insufficient evidence to determine the effectiveness of exercise therapy for the correction of scoliosis. Moreover, better quality researches are required before physiotherapy scoliosis specific exercises can be recommended in clinical practice.[6–8]
In addition, there were also problems with previous exercise therapies. First, although the effects of exercise were equivocal to individuals, they did not verify the mechanism of action. Second, these methods are inconvenient and difficult to follow. For example, the Schroth approach was more effective when supervised by physiotherapists, and less effective when performed at home.[25] Therefore, such approach may increase medical costs and become a social issue.
Since scoliosis is a rare disease, it is difficult to perform double blinded, randomized, controlled studies on topics pertaining to scoliosis. Exercise therapy is needed to be based on scientific evidence, with the understanding of normal anatomy and movement of the spine and musculature. Based on literature review, we believe that exercise containing asymmetric components may be more effective in managing scoliosis than other exercise methods. It is interesting that the Schroth approach, SEAS, and side-shift approach all include components of ASSE introduced in this study. The Schroth approach included types I and III exercises of ASSE; and the side-shift approach included a component similar to types II and III exercises. As previous physiotherapy scoliosis specific exercises include a diverse component of exercises, direct comparison to our exercise protocol is difficult. Follow-up studies are required.
Ryu scoliosis exercise protocol was established based on the results of S-EMG values in this study. This exercise protocol can be implemented easily (Fig. 4). The process of developing this protocol was as follows. First, the scoliosis curve pattern was divided by the number of curves (single or double curve) and locations (mid thoracic, low thoracic, and mid lumbar). Second, we choose and make cluster of exercises that can reinforce the concave side muscle relative to the convex side on the scoliotic curvature. For objective and quantitative analysis, relative strength of the muscles during isometric contraction was calculated using the asymmetric index (AI) based on the RMS value of S-EMG (Fig. 3).[15] We also used the subtype of ASSE showing statistical significance. As an exception, type I (D) symmetric exercise was added to the protocol, which showed the greatest increase in the RMS value considering the overall strengthening of the muscles. ASSE was intended to correct the scoliotic curve, and the last symmetric exercise (type I (D)) was intended to maintain a symmetric spine. Therefore, type I (D) was performed as the final step.
5. Study Limitations
This study has several limitations, including a relatively small sample size and lack of outcome. A future randomized, prospective study with a larger sample size to better evaluate Ryu scoliosis exercise protocol is required.
6. Conclusion
In this study, we were able to find a component of a specific ASSE that improved the Cobb angle on radiography. Moreover, the S-EMG data showed that the component of each ASSE can selectively activate the paraspinal and abdominal muscles of the unilateral side. By combining these 2 experimental findings, we conclude that the paraspinal muscle strengthening of the concave side using ASSE can improve the severity of scoliosis. Finally, based on our findings, we propose a new exercise protocol that can be personalized based on the curve pattern.
6.1. Suppliers
-
a.
BTS FREEEMG 1000 with EMG-BTS EMG-Analyzer, BTS Bioengineering Co.
-
b.
SPSS for Windows version 22.0, SPSS Inc., Chicago, Illinois, USA.
Acknowledgment
The authors thank the Medical Research Collaborating Center at Seoul National University Bundang Hospital for statistical analyses.
Author contributions
Conceptualization: Ju Seok Ryu.
Data curation: Jin Young Ko, Hayoung Kim
Formal analysis: Jin Young Ko, Ju Seok Ryu.
Funding acquisition: Ju Seok Ryu.
Investigation: Jin Young Ko, Hayoung Kim, Ju Seok Ryu.
Methodology: Jee Hyun Suh, Ju Seok Ryu.
Project administration: Ju Seok Ryu.
Resources: Jin Young Ko, Ju Seok Ryu.
Software: Ju Seok Ryu.
Supervision: Ju Seok Ryu.
Writing – original draft: Jin Young Ko
Writing – review & editing: Ju Seok Ryu.
Footnotes
Abbreviations: ASSE = asymmetric spinal stabilization exercise, EO = external oblique, ES = erector spinae, IS = idiopathic scoliosis, RA = rectus abdominis, SEAS = scientific exercise approach to scoliosis, sEMG = surface electromyography.
This study received an approval from the institutional review board.
This work was Supported by grant no 09-2017-001 from the SNUBH Research Fund.
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer any benefit upon the authors or upon any organization with which the authors are associated.
References
- [1].Hresko MT. Clinical practice. Idiopathic scoliosis in adolescents. N Engl J Med 2013;368:834–41. [DOI] [PubMed] [Google Scholar]
- [2].Dickson RA, Lawton JO, Archer IA, et al. The pathogenesis of idiopathic scoliosis. Biplanar spinal asymmetry. J Bone Joint Surg Br 1984;66:8–15. [DOI] [PubMed] [Google Scholar]
- [3].Cheung J, Halbertsma JP, Veldhuizen AG, et al. A preliminary study on electromyographic analysis of the paraspinal musculature in idiopathic scoliosis. Eur Spine J 2005;14:130–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Cheung J, Veldhuizen AG, Halbertsma JP, et al. The relation between electromyography and growth velocity of the spine in the evaluation of curve progression in idiopathic scoliosis. Spine (Phila Pa 1976) 2004;29:1011–6. [DOI] [PubMed] [Google Scholar]
- [5].Gaudreault N, Arsenault AB, Lariviere C, et al. Assessment of the paraspinal muscles of subjects presenting an idiopathic scoliosis: an EMG pilot study. BMC Musculoskelet Disord 2005;6:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Plaszewski M, Bettany-Saltikov J. Non-surgical interventions for adolescents with idiopathic scoliosis: an overview of systematic reviews. PLoS One 2014;9:e110254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Mordecai SC, Dabke HV. Efficacy of exercise therapy for the treatment of adolescent idiopathic scoliosis: a review of the literature. Eur Spine J 2012;21:382–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Romano M, Minozzi S, Zaina F, et al. Exercises for adolescent idiopathic scoliosis: a Cochrane systematic review. Spine (Phila Pa 1976) 2013;38:E883–93. [DOI] [PubMed] [Google Scholar]
- [9].Kim CR, Park DK, Lee ST, et al. Electromyographic changes in trunk muscles during graded lumbar stabilization exercises. PM R 2016;8:979–89. [DOI] [PubMed] [Google Scholar]
- [10].Lee HS, Kim DJ, Oh Y, et al. The effect of individualized gradable stabilization exercises in patients with chronic low back pain: case-control study. J Back Musculoskelet Rehabil 2016;29:603–10. [DOI] [PubMed] [Google Scholar]
- [11].Mannion AF, Meier M, Grob D, et al. Paraspinal muscle fibre type alterations associated with scoliosis: an old problem revisited with new evidence. Eur Spine J 1998;7:289–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Avikainen VJ, Rezasoltani A, Kauhanen HA. Asymmetry of paraspinal EMG-time characteristics in idiopathic scoliosis. J Spinal Disord 1999;12:61–7. [PubMed] [Google Scholar]
- [13].Negrini S, Donzelli S, Lusini M, et al. The effectiveness of combined bracing and exercise in adolescent idiopathic scoliosis based on SRS and SOSORT criteria: a prospective study. BMC Musculoskelet Disord 2014;15:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Suh SW, Modi HN, Yang JH, et al. Idiopathic scoliosis in Korean schoolchildren: a prospective screening study of over 1 million children. Eur Spine J 2011;20:1087–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Naeije M, McCarroll RS, Weijs WA. Electromyographic activity of the human masticatory muscles during submaximal clenching in the inter-cuspal position. J Oral Rehabil 1989;16:63–70. [DOI] [PubMed] [Google Scholar]
- [16].Schmid AB, Dyer L, Boni T, et al. Paraspinal muscle activity during symmetrical and asymmetrical weight training in idiopathic scoliosis. J Sport Rehabil 2010;19:315–27. [DOI] [PubMed] [Google Scholar]
- [17].Chwala W, Plaszewski M, Kowalski P. Variations in bioelectric activity during symmetric loading and asymmetric stretching of paraspinal extensors in young adult women with mild single curve scoliosis. Stud Health Technol Inform 2012;176:129–32. [PubMed] [Google Scholar]
- [18].Berdishevsky H, Lebel VA, Bettany-Saltikov J, et al. Physiotherapy scoliosis-specific exercises - a comprehensive review of seven major schools. Scoliosis Spinal Disord 2016;11:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Rigo M, Quera-Salva G, Villagrasa M, et al. Scoliosis intensive out-patient rehabilitation based on Schroth method. Stud Health Technol Inform 2008;135:208–27. [PubMed] [Google Scholar]
- [20].Weiss HR, Negrini S, Hawes MC, et al. Physical exercises in the treatment of idiopathic scoliosis at risk of brace treatment -- SOSORT consensus paper 2005. Scoliosis 2006;1:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Schreiber S, Parent EC, Khodayari Moez E, et al. Schroth physiotherapeutic scoliosis-specific exercises added to the standard of care lead to better Cobb angle outcomes in adolescents with idiopathic scoliosis - an assessor and statistician blinded randomized controlled trial. PLoS One 2016;11:e0168746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Romano M, Negrini A, Parzini S, et al. SEAS (Scientific Exercises Approach to Scoliosis): a modern and effective evidence based approach to physiotherapic specific scoliosis exercises. Scoliosis 2015;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Maruyama T, Kitagawa T, Takeshita K, et al. Conservative treatment for adolescent idiopathic scoliosis: can it reduce the incidence of surgical treatment? Pediatr Rehabil 2003;6:215–9. [DOI] [PubMed] [Google Scholar]
- [24].Mamyama T, Kitagawal T, Takeshita K, et al. Side shift exercise for idiopathic scoliosis after skeletal maturity. Stud Health Technol Inform 2002;91:361–4. [PubMed] [Google Scholar]
- [25].Kuru T, Yeldan I, Dereli EE, et al. The efficacy of three-dimensional Schroth exercises in adolescent idiopathic scoliosis: a randomised controlled clinical trial. Clin Rehabil 2016;30:181–90. [DOI] [PubMed] [Google Scholar]


