Abstract
Irritable Bowel Syndrome (IBS) is the most prevalent functional gastrointestinal disorder. Psychosocial stress is one of the pathogenic factors involved in the pathogenesis of IBS. The Pressure Management Indicator (PMI) is a validated questionnaire to analyze all aspects of occupational stress—a model involving sources of pressure, the mechanisms of coping, the personality, and the resulting effects of the interaction between these 3 elements. The purpose of this study was to analyze the association between socio-professional stress effects in IBS, and the relationship of IL-6 levels and salivary cortisol with occupational stress.
We conducted a prospective cross-sectional study on 76 patients (39 patients with IBS, diagnosed according to the Rome III criteria and 37 healthy controls) who were investigated using a validated self-administered questionnaire: PMI. The biologic markers of chronic stress were analyzed using salivary cortisol and the immune response with serum interleukin 6 (IL-6).
The IBS patients corresponded to the following subtypes: diarrhea-predominant: 22, constipation-predominant: 14 and mixed: 3. All the socio-professional pressure effects variables and scales were statistically significant, in an inversely proportional relation with IBS. Lower scores (poor effects) were found in IBS subjects. The adjusted odds ratios of having IBS versus healthy subjects for the socio-professional pressure effects scales were: 0.81 (95% confidence interval (CI) 0.72–0.88), for satisfaction, 0.85 (95% CI 0.78–0.91) for organization, 0.85 (95% CI 0.79–0.91) for mental wellbeing and 0.8 (95% CI 0.71–0.87) for physical wellbeing (P <.001). Also, the serum IL-6 levels were significantly higher in IBS than in controls (p < 0.001). There was no statistical difference between the salivary levels of cortisol between IBS patients and controls (P = .898).
The level of occupational stress was higher in IBS patients compared to healthy subjects (socio-professional stress effects were lower in IBS patients) and correlated with IL-6 levels. Salivary cortisol was not associated with occupational pressure management.
Keywords: cortisol, interleukin 6, irritable bowel syndrome, occupational stress, pressure management
This paper was funded by a grant of the European Social Fund, Human Resources Development Operational Programme 2007 to 2013, project no. POSDRU/159/1.5/S/138776.
1. Introduction
Irritable Bowel Syndrome (IBS) is the most prevalent functional gastrointestinal disorder, presenting according to Rome IV criteria, recurrent abdominal pain, and bowel transit disorders.[1]
Various factors, including genetic background, food intolerance, intestinal infection, previous abdominal or pelvic surgery, intestinal immune disruption, gut microbiota alteration or bacterial overgrowth, sexual abuse, and psychological stress, are involved in the pathogenesis of IBS.[2–4] Studies showed that psychosocial stress is associated with the onset of IBS and different animal and human experiments have demonstrated the role of stress on visceral hypersensitivity and the influence of psychosocial stress on gut-brain axis pain pathways.[5–7] Occupational stress represents a significant precipitating factor in different diseases.[2,4,8,9] Its role in IBS needs clarification. The aim of our study was to evaluate occupational stress by validated questionnaires in IBS and to also appraise the relationship of interleukin 6 (IL-6) levels and salivary cortisol with occupational stress.
2. Materials and methods
2.1. Protocol
Patients with IBS and controls were included in this observational, prospective, cross-sectional study. These were investigated with a validated questionnaire for pressure measurement as a marker of professional stress. Salivary cortisol as a marker of stress and IL-6 as a marker of inflammation was also investigated.
2.2. Patients
A total of 76 participants (31 males, 45 females) were included in the study. IBS patients (n = 39), were recruited from a single tertiary center in consecutive order, between 2012 and 2016. Inclusion criteria were: age between 18 to 65 years (active before retirement age), employed, Caucasian, filling the IBS Rome III criteria.[10,11] Exclusion criteria were: being retired or unemployed; past or present medical conditions complicated by autonomic dysfunction (peripheral neuropathy, diabetes, asthma, heart failure, and renal insufficiency), diagnosed organic gastrointestinal diseases and previous abdominal surgery, chronic psychiatric disorders, inflammatory bowel diseases (ulcerative colitis and Crohn's disease), thyroid pathology (hypothyroidism and hyperthyroidism). One hundred twenty-one IBS patients were invited to participate in the present study, but only 39 accepted.
2.3. Controls
The study included 37 healthy controls (HCs) that were staff members and family members of patients, and were included in the study after proper information and given agreement. None of the controls were diagnosed with somatic or psychiatric diseases. The subjects were all employed, Caucasian and employed.
2.4. Questionnaire
The questionnaire used for the analysis of occupational stress was: PMI (Williams & Cooper, 1998, translated, adapted and validated for Romanian subjects by Adrian Brate, 2004), a 120 item self-report questionnaire developed from the Occupational Stress Indicator (OSI).[12] The PMI is designed to measure all aspects of occupational stress, has been extensively benchmarked, it is standardized, reliable, valid and has been translated in many languages. Its framework is based on the idea that there is a 4-way model of the stress, and it measures each of these dimensions.
This questionnaire provides an integrated diagnosis of the 4 major dimensions of occupational stress, which measure—the sources of stress—stressors levels (sources of social and professional stress)—then how the subject tries to deal with the sources of stress—the coping strategies (through emotional detachment, focusing on the problem, with social support)—then how personality can modulate the first 2—the individual differences (due to the individual personality: like patience or impatience, control, drive), and finally the stress effects (the final result of the interaction of the first 3 elements on satisfaction, security, commitment, state of mind, resilience, confidence level, physical symptoms, energy levels). The number of working hours per week and the number of holidays were also examined. The time limit for the self-completed questionnaires was 1 hour. Participants were asked to estimate the items that were potential sources of pressure at their work in relation to the degree of pressure over the past 3 months.[10–14]
Socio-professional sources of pressure were analyzed using the following variables: Workload, Relationships, Recognition, Organizational climate, Personal responsibility, Managerial role, Home/work balance, Daily hassles; and personality parameters (individual differences): Drive, Control, Impatience, Personal influence—as mediator variables. The estimate is made on a Likert scale with 6-steps (1 = definitely not a source; 6 = certainly a source). Higher scores indicate more pressure.
Effects of organizational stress were described as: job satisfaction (how satisfied someone feels about the type of work they are involved in), organizational satisfaction (how satisfied someone feels about the way an organization is structured and the way it works), organizational security (how secure someone feels about the stability of their organization and level of job security), organizational commitment (how committed a person is to their organization), state of mind (how satisfied an individual feels about their state of mind), resilience (the ability to “bounce back” from setbacks or problems), confidence level (the extent to which someone feels settled or worried), physical symptoms (how calm a person feels in terms of physical tension), energy level (the amount of energy and vitality someone has before they feel tired and worn out).[12,13] There are also 4 socio-professional pressure effects scales: the organization, mental wellbeing, physical wellbeing. Higher scores indicate better effects. In our study, only these resulting socio-professional effects as a variable to compare IBS subjects with HCs were used.
Coping strategies were analyzed using a Likert-type scale, 6 steps (1 = never used,6 = used very frequently. This scale includes the following subscales: focus on the problem (6 items), work-life balance (4 items), and social support (3 items). High scores indicate a greater use of these mechanisms in order to cope.[12]
2.5. Stress biomarkers
2.5.1. Salivary cortisol measurements
Patients and controls were instructed to collect saliva at 3 pm in their usual environment, during their work program. Samples were sent to our laboratory on the same day when they were collected. Before sampling, subjects were instructed not to eat, drink or smoke for 4 hours. For the sample analysis, a commercial enzyme immunoassay (Salimetrics, Eletrabox) was used.
2.5.2. Cytokines measurement
IL-6 as a marker of inflammation was also assessed to look for a putative association with stress. Peripheral venous blood samples were collected in plain vials, from all subjects. Blood samples were centrifuged after proper clotting to prevent hemolysis, stored at −80°C until further analysis and thawed only once. Serum IL-6 was measured by a commercially available enzyme-linked immunosorbent assay (Diaclone) and was performed according to the manufacturer's protocols. The minimal detectable concentration was <2 pg/mL for IL-6 and the normal value was <3,8pg/mL.
2.6. Statistical analysis
Statistical analysis was carried out using R software environment for statistical computing and graphics version 3.1.2 (R Foundation for Statistical Computing, Vienna, Austria). Qualitative data were presented as counts and percentages and compared between groups using the Pearson chi-square test (χ2), or Fisher exact test. Quantitative data were presented as means with standard deviations or medians with interquartile ranges. The t test for independent samples was used to compare quantitative data using a significance level of 0.05. The Kruskal–Wallis test was used to compare 4 groups of quantitative data, followed by nonparametric post hoc tests. To assess the relation between IBS presence (vs HCs) and the socio-professional effects pressure scales of the Pressure Management Indicator (PMI), we used a multivariate logistic regression, to control for confounding factors. Several models were built containing each item (1 item per model) of the occupational classification, and the socio-professional effects pressure variables and then the scales, each being adjusted for age and gender. Since the multicollinearity was present between the socio-professional effects pressure scales (checked with the variance inflation factor), we used a principal component analysis to extract 1 principal component that was used in the end instead of them as their synthesis. The models were assessed also for goodness of fit with the Hosmer and Lemeshow test, and misspecification (Osius-Rojek test and Stukel test). The results of regression are presented as odds ratios (OR) and 95% confidence interval (CI). For all statistical tests, a bilateral P value <.05 was considered to be statistically significant.
2.7. Ethics statement
The study was performed in agreement with the Declaration of Helsinki and was approved by the local Ethics Committee. Written informed consent was obtained from each participant.
3. Results
3.1. Demographic, occupational and lifestyle characteristics
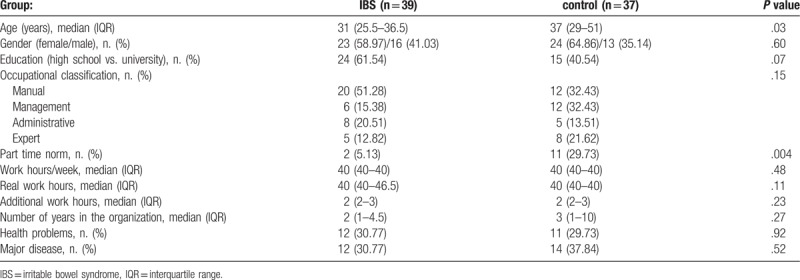
The demographic, occupational and lifestyle characteristics of IBS patients and HCs are presented in Table 1. The IBS subjects were younger and with less part-time work than the controls. Otherwise, no other statistically significant differences were found between the groups, occupationally and healthwise.
Table 1.
Demographic, occupational, and lifestyle characteristics.
3.2. Pressure management in IBS
We found statistically significant lower scores in the IBS group compared to HCs for all of the socio-professional pressure effects scales, including mental wellbeing, physical wellbeing, and occupational satisfaction and also for all the socio-professional pressure effects variables (Fig. 1).
Figure 1.
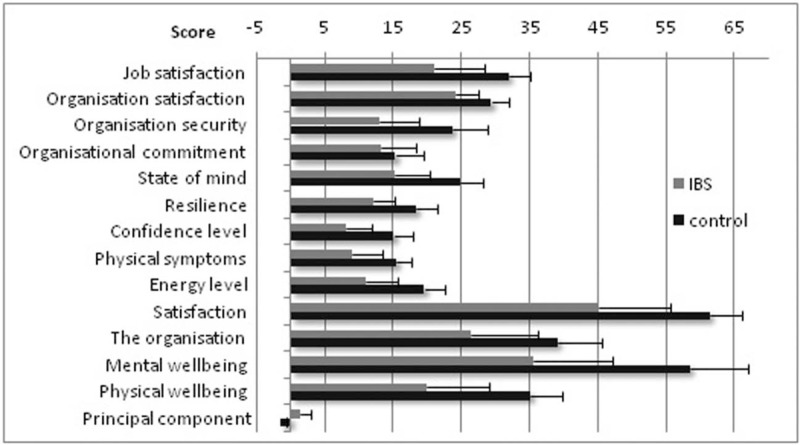
Comparison of the socio-professional pressure effects scales and the socio-professional pressure effects variables of mean scores (+ 1 standard deviation) between IBS and control subjects (higher scores indicate better effects). IBS = irritable bowel syndrome.
In order to look deeper into the relation between IBS and the socio-professional pressure effects variables and scales, we built separate logistic regression models for each score, controlling each for age and gender. Even after adjustment, the lower scores were statistically significant associated to higher odds of IBS compared to the control group, for all of the socio-professional pressure effects variables, and for all the 4 socio-professional pressure effects scales (Fig. 2). Due to multicollinearity we used in the final model the principal component extracted from the 4 socio-professional pressure effects scales as can be seen in Figure 2. The same association holds true for the principal component with the IBS
Figure 2.
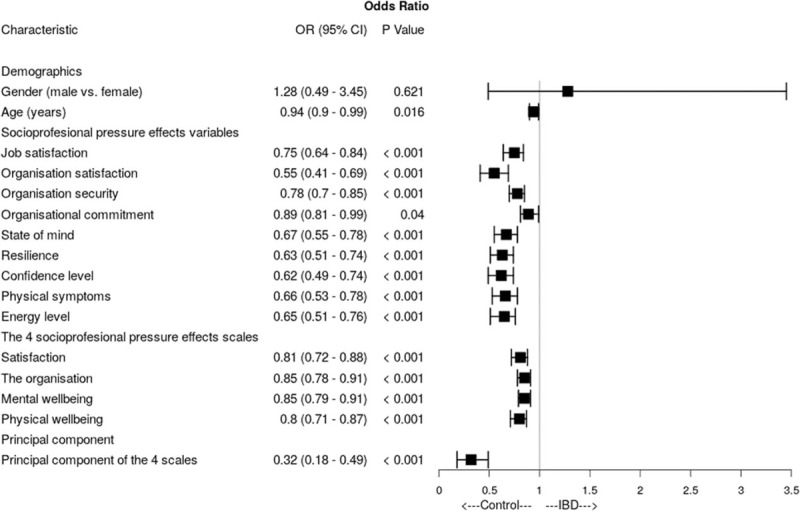
Forest plot of multivariate logistic regression predicting irritable bowel syndrome (IBS) adjusted for gender and age, for each of the effects of socio-professional pressure, the 4 scales of the Pressure Management Indicator—higher scores indicate better effects. CI = confidence interval, OR = odds ratio.
3.3. Biomarkers of inflammation
Associations of serum cytokine levels and symptoms in patients with IBS were analyzed (Table 2, Fig. 3), the result being that patients with IBS had significantly higher IL-6 levels compared with the HC group. The predominant diarrhea (IBS-D) type had the highest levels.
Table 2.
Interleukin 6 (IL-6) and salivary cortisol in irritable bowel syndrome (IBS) and healthy controls.
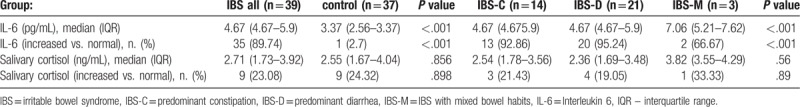
Figure 3.
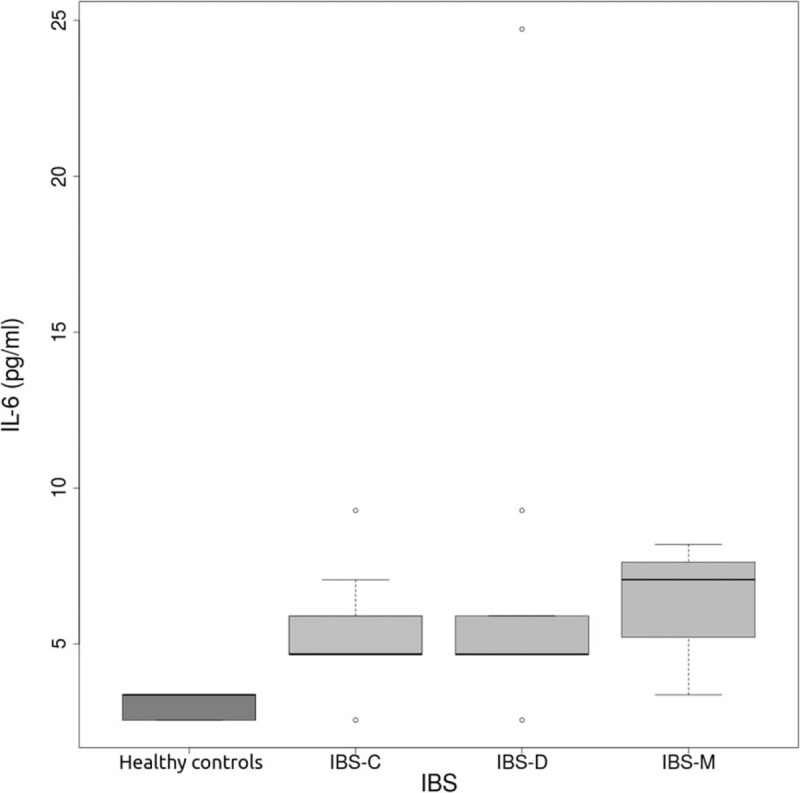
IL-6 in IBS subtypes (IBS-C = predominant constipation, IBS-D = predominant diarrhea, IBS-M = IBS with mixed bowel habits), and healthy control subjects. IBS = irritable bowel syndrome, IL-6 = interleukin 6.
3.4. Biomarkers of stress
Associations of salivary cortisol with IBS were analyzed (Table 2), resulting in that no significant difference was found between salivary cortisol levels of IBS patients and HC.
4. Discussion
The aim of this study was to investigate the level of occupational stress in a sample of adults diagnosed with IBS according to Rome III criteria compared with an HC group. Our results revealed that the occurrence of IBS symptoms is significantly related to the presence of occupational stress resulting from the psychosocial work environment. Additional analyses evaluated the influence of proinflammatory cytokines as immune mediators in the pathogenesis IBS and salivary cortisol as a marker of chronic stress. The results evidenced a significant correlation between IBS and IL-6. No statistically significant relation between salivary cortisol and IBS was found.
Occupational stress is defined as the stress that occurs when the needs of the job poorly align with the abilities of the employee and where available resources and expectations of the employer are causing harmful physical and emotional responses.[15] Several questionnaires have frequently investigated occupational stress: The Scale of Perceived Occupational Stress, Generic Job Stress Questionnaire, The Occupational Stress Inventory-Revised, The Occupational Stress Index.[12,13,15] Preliminary results of our study regarding the professional stress were published in a letter to the Editor.[5]
Previous research found that occupational stress including factors in the psychosocial work environment such as organizational climate, organizational satisfaction, job satisfaction, work demands, insufficient job control, a lack of any reward, home/work balance, organizational commitment, and low social support were significantly associated with worker anxiety, depression or functional gastrointestinal disorders.[16]
Recent data show that occupational stress is involved in the pathogenesis of numerous disorders. A systematic meta-analysis shows that job stress is associated with an increased risk of recurrent coronary heart disease events by 65%.[17] A cross-sectional study of differences among medical residents with various specialties working in German hospitals revealed that more than 17% of the physicians presented high levels of occupational stress and 9% reported high levels of depressive symptoms. Significant differences between medical specialties were also evidenced for occupational stress, depressive symptoms, work ability, job demands and job resources. Surgeons showed the highest levels of perceived stress but also the lowest scores for depression. Depressive symptoms were rated with the highest levels by anesthesiologists.[18] Until recent years, the research of the link between functional gastrointestinal disorders and psychological stress had concentrated more on childhood abuse, prenatal traumatic events, anxiety disorders, depression, major life events (divorce or death of a close relative), and major social events (war, revolution, social changes) and also daily hassles.[4,19–22] Nevertheless, evidence that supports the role of occupational stress in the occurrence of IBS is insufficient. This can be the result of the fact that investigating IBS is intricate with somatic disorders and a psychological status that promote each other, resulting in somatic symptoms which aggravate the patients’ psychological load, leading to the aggravation of anxiety and depression. Later, reliable attempts were made, notifying the relation between cytokines, hormones, genetic polymorphism, brain-gut axis dysfunction and the occurrence of functional gastro-intestinal disorders, first and foremost IBS.[23,24] We found a significant association between IBS and occupational stress evidenced by the following items: organizational satisfaction, mental wellbeing, physical wellbeing, sources of pressure, type A behavior, coping (P <.001), but no relation between occupational classification, workout program, norm, health status, major disease, negative pressure in the last 3 months, smoking, alcohol consumption, work hours, number of years in the organization and when IBS was diagnosed. These job-related factors are not standardized and might not have sufficient diagnostic accuracy to assess stress levels, compared to the questionnaire that we used. The differences found by the questionnaire between IBS and controls underlines once again the importance of using validated instruments in all studies that deal with latent variables. Psychosocial differences between Rome III IBS subtypes have not been well documented up to present.[14,16] We did not observe statistically significant differences between all 3 IBS subtypes with regard to occupational stress. The heterogeneity of association results with total IBS, predominant constipation (IBS-C), IBS-D, and IBS with mixed bowel habits (IBS-M) suggests that further studies are required to assess which biological marker is relevant for all specific IBS subtypes. In this study, we looked for PMI, as a component of occupational stress in IBS, as a stress-related condition. Previous studies, using PMI or OSI questionnaires, show that occupational stress is increased in depression, anxiety, burnout, sleep disorders, and cardiovascular disease.[12,14] PMI is higher in IBS patients compared to controls. We were not able to detect differences in PMI scores between subtypes of IBS. To our knowledge, this is the first assessment of PMI in IBS.
Since this is a cross-sectional study it cannot identify if occupational stress affects IBS or vice versa.
We also looked for a correlation between PMI and stress biomarkers. Salivary cortisol levels are not affected by salivary flow rate or salivary enzymes; as a result it is frequently used in clinical practice but also in research as an efficient marker of psychological stress. Furthermore, there is no study that has analyzed the link between professional stress, cortisol, and IBS. IL-6 is produced in response to infections and tissue injuries and has the main functions of stimulation of acute phase responses, hematopoiesis, and immune reactions. Because it plays an essential role in chronic inflammation and autoimmunity, we decided to investigate the link between IBS, IL-6 and professional stress. Our study demonstrates that patients with IBS have increased levels of pro-inflammatory cytokines IL-6, providing evidence that inflammation is involved in all IBS subgroups. Our findings are in accordance with a recent study by Scully et al[25] and also McKerman et al[26] demonstrating elevated IL-6 in patients with IBS. Similar findings of increased serum IL-6 and also TNF-α in IBS patients have been reported in other studies.[27–30] In our sample, no differences were observed in IL-6 levels between IBS subgroups. To our surprise, we did not find any statistically significant difference in the salivary cortisol levels between our patients and controls and PMI was not correlated to the level of salivary cortisol. However, our results are consistent with previous research where salivary cortisol was not found to be statistically significant in IBS patients[31,32] although other studies show opposite results.[33–35] This could be the result of an acute psychological stress and corticotropin-releasing hormone, which increases the intestinal permeability in humans by a mast cell-dependent mechanism.
There are potential limitations that need to be acknowledged. Because selection bias cannot be excluded, a larger sample of patients should be studied to certify the current findings. The fact that only some of the recruited subjects accepted to participate in our study might add a non-response bias. The observational nature of the study allows residual confounding to remain, even if we adjusted for several variables in the multivariate analysis. These possible situations could result in a diminished association between IBS presence and the studied variables. Furthermore, the observed relation of IL-6 levels and occupational stress does not indicate the causal direction of the association, and the underlying accurate mechanisms require to be further analyzed.
Despite the fact that the sample size was not that big, the results are highly statistically significant and the adjusted ORs are distant from the value of 1, thus suggesting an important force of association.
There are elements that help the generalization of the findings of this study to the target population, 1 of them being the consecutive recruitment of subjects that were studied, and the fact that part of the control group was at least from a similar environment to the patients (their relatives).
5. Conclusions
The level of occupational stress was higher in IBS patients compared to healthy subjects (the socio-professional stress effects were considerably lowers in IBS patients). Serum level of IL-6 was higher in IBS than in controls, suggesting the role of proinflammatory cytokines in the pathogenesis IBS. IL-6 levels and salivary cortisol were not associated with Pressure Management Indicator scores.
Author contributions
Stefan-Lucian Popa carried out the study, analyzed the data, and wrote the paper. Dan Lucian Dumitrascu supervised the study and made substantial contributions to conception and writing of the manuscripts; Daniel Leucuta made substantial contributions to the analysis of the data, interpretation, and revised the drafts. All authors read and approved the final manuscript.
Conceptualization: Stefan L. Popa, Dan Lucian Dumitrascu.
Formal analysis: Daniel Corneliu Leucuta.
Investigation: Stefan L. Popa.
Methodology: Stefan L. Popa, Dan Lucian Dumitrascu.
Project administration: Stefan L. Popa.
Resources: Stefan L. Popa.
Supervision: Dan Lucian Dumitrascu.
Visualization: Daniel Corneliu Leucuta.
Writing – original draft: Stefan L. Popa.
Writing – review & editing: Stefan L. Popa, Daniel Corneliu Leucuta, Dan Lucian Dumitrascu.
Daniel Corneliu Leucuta orcid: 0000-0003-4218-8622.
Footnotes
Abbreviations: CI = confidence interval, HC = healthy controls, IBS = Irritable Bowel Syndrome, IBS-D = predominant diarrhea, IL-6 = interleukin 6, OR = odds ratio, OSI = occupational stress indicator, PMI = the Pressure Management Indicator.
The authors have no conflicts of interest to disclose.
References
- [1].Drossman DA, Hasler WL. Rome IV-functional GI disorders: disorders of gut-brain interaction. Gastroenterology 2016;150:1257–61. [DOI] [PubMed] [Google Scholar]
- [2].Sperber AD, Dumitrascu D, Fukudo S, et al. The global prevalence of IBS in adults remains elusive due to the heterogeneity of studies: a Rome Foundation working team literature review. Gut 2016;27:1075–82. [DOI] [PubMed] [Google Scholar]
- [3].El-Salhy M, Gundersen D, Hatlebakk JG, et al. A cell density as a diagnostic marker for lymphocytic colitis. Dig Dis Sci 2012;57:3154–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Blaga T, Băban A, Dumitrascu D. Psychosocial determinants of irritable bowel syndrome. World J Gastroenterol 2012;18:616–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Popa SL, Brate AT, Leucuta DC, et al. Impaired pressure management in the irritable bowel syndrome. J Gastrointestin Liver Dis 2016;25:566–7. [PubMed] [Google Scholar]
- [6].Shi H, Liu C, Ding L, et al. Alterations in serotonin, transient receptor potential channels and protease-activated receptors in rats with irritable bowel syndrome attenuated by Shugan decoction. World J Gastroenterol 2015;21:4852–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Aguilera M, Vergara P, Martínez V. Stress and antibiotics alter luminal and wall-adhered microbiota and enhance the local expression of visceral sensory-related systems in mice. Neurogastroenterol Motil 2013;25:e515–29. [DOI] [PubMed] [Google Scholar]
- [8].Konturek PC, Brzozowski T, Konturek SJ. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol 2011;62:591–9. [PubMed] [Google Scholar]
- [9].Drossman DA, Camilleri M, Mayer EA, et al. AGA technical review on irritable bowel syndrome. Gastroenterology 2002;123:2108–31. [DOI] [PubMed] [Google Scholar]
- [10].Yao X, Yang YS, Cui LH, et al. Subtypes of irritable bowel syndrome on Rome III criteria: a multicenter study. Gastroenterol Hepatol 2012;27:760–5. [DOI] [PubMed] [Google Scholar]
- [11].Rusu F, Dumitrascu DL. Epidemiology of irritable bowel syndrome in the former communist countries from Eastern Europe: a systematic review. Clujul Med 2015;88:146–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Brate T. Sources of pressures, individual differences, coping strategies and organizational satisfaction: a model of mediation. Romanian J Exp Appl Psuchol 2004;5:34–6. [Google Scholar]
- [13].Brate AT. Avram E. Occupational organizational stress models. Organizational Health Psychology. Bucharest: Editura Universitara; 2011. 51–73. [Google Scholar]
- [14].Williams S, Cooper C. Measuring occupational stress: development of the pressure management indicator. J Occup Health Psychol 1998;3:306–21. [DOI] [PubMed] [Google Scholar]
- [15].Sauter S, Hurrell J, Murphy L. Stellman J, et al. Psychosocial and organizational factors. Encyclopaedia of Occupational Health and Safety. Vol. 1. Geneva, Switzerland: International Labour Office; 1997;34.1-34.77. [Google Scholar]
- [16].Caspi A, Milne BJ, Danese A, et al. Work stress precipitates depression and anxiety in young, working women and men. Melchior Psychol Med 2007;37:1119–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Li J, Zhang M, Loerbroks A, et al. Work stress and the risk of recurrent coronary heart disease events: a systematic review and meta-analysis. Int J Occup Med Environ Health 2015;28:8–19. [DOI] [PubMed] [Google Scholar]
- [18].Bernburg M, Vitzthum K, Groneberg D, et al. Physicians’ occupational stress, depressive symptoms and work ability in relation to their working environment: a cross-sectional study of differences among medical residents with various specialties working in German hospitals. BMJ Open 2016;6:e011369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Klooker TK, Braak B, Painter RC, et al. Exposure to severe wartime conditions in early life is associated with an increased risk of irritable bowel syndrome: a population-based cohort study. Am J Gastroenterol 2009;104:2250–6. [DOI] [PubMed] [Google Scholar]
- [20].Grad S, Grad C, Baban A, et al. Child abuse in the irritable bowel syndrome. Rom J Intern Med 2014;52:183–8. [PubMed] [Google Scholar]
- [21].Park SH, Videlock EJ, Shih W, et al. Adverse childhood experiences are associated with irritable bowel syndrome and gastrointestinal symptom severity. Neurogastroenterol Motil 2016;28:1252–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Bradford K, Shih W, Videlock E, et al. Association between early adverse life events and irritable bowel syndrome. Clin Gastroenterol Hepatol 2012;10:385-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Heikkilä K, Nyberg ST, Theorell T, et al. IPD-Work Consortium Work stress and risk of cancer: meta-analysis of 5700 incident cancer events in 116,000 European men and women. BMJ 2013;346:f165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Popa S, Dumitrascu D. Anxiety and IBS revisited: ten years later. Clujul Med 2015;88:253–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Scully P, McKernan DP, Keohane J, et al. Plasma cytokine profiles in females with irritable bowel syndrome and extra-intestinal co-morbidity. Am J Gastroenterol 2010;105:2235–43. [DOI] [PubMed] [Google Scholar]
- [26].McKernan DP, Gaszner G, Quigley EM, et al. Altered peripheral toll-like receptor responses in the irritable bowel syndrome. Aliment Pharmacol Ther 2011;33:1045–52. [DOI] [PubMed] [Google Scholar]
- [27].Dinan TG, Quigley EM, Ahmed SM, et al. Hypothalamic-pituitary-gut axis dysregulation in irritable bowel syndrome: plasma cytokines as a potential biomarker. Gastroenterology 2006;130:304–11. [DOI] [PubMed] [Google Scholar]
- [28].Liebregts T, Adam B, Bredack C, et al. Immune activation in patients with irritable bowel syndrome. Gastroenterology 2007;132:913–20. [DOI] [PubMed] [Google Scholar]
- [29].Barkhordari E, Rezaei N, Ansaripour B, et al. Proinflammatory cytokine gene polymorphisms in irritable bowel syndrome. J Clin Immunol 2010;30:74–9. [DOI] [PubMed] [Google Scholar]
- [30].Dinan TG, Clarke G, Quigley EM, et al. Enhanced cholinergic-mediated increase in the proinflammatory cytokine IL-6 in irritable bowel syndrome: role ofmuscarinic receptors. Am J Gastroenterol 2008;103:2570–6. [DOI] [PubMed] [Google Scholar]
- [31].Jarrett M, Cain KC, Barney P, et al. Balance of autonomic nervous system predicts who benefits from a self-management intervention program for irritable bowel syndrome. J Neurogastroenterol Motil 2016;22:102–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Walter S, Aardal-Eriksson E, Thorell LH, et al. Pre-experimental stress in patients with irritable bowel syndrome: high cortisol values already before symptom provocation with rectal distensions. Neurogastroenterol Motil 2006;18:1069–77. [DOI] [PubMed] [Google Scholar]
- [33].Kennedy PJ, Cryan J, Quigley E, et al. A sustained hypothalamic-pituitary-adrenal axis response to acute psychosocial stress in irritable bowel syndrome. Psychol Med 2014;44:3123–34. [DOI] [PubMed] [Google Scholar]
- [34].Elsenbruch S, Thompson J, Hamish MJ, et al. Behavioral and physiological sleep characteristics in women with irritable bowel syndrome. Am J Gastroenterol 2002;97:2306–14. [DOI] [PubMed] [Google Scholar]
- [35].Vanuytsel T, van Wanrooy S, Vanheel H, et al. Psychological stress and corticotropin-releasing hormone increase intestinal permeability in humans by a mast cell-dependent mechanism. Gut 2014;63:1293–9. [DOI] [PubMed] [Google Scholar]


