Abstract
Institutional review boards (IRBs) that refuse to grant waivers of guardian permission may hinder research to inform needed online sexual health interventions for adolescent males interested in sex with males (AMSM). Information on the challenges of obtaining (or waiving) guardian permission is imperative. In June-July 2017, AMSM (N = 206; ages 14–17) in the United States completed an online survey on sexual behaviors, sexually explicit media use, and sexual education exposure/needs. A mixed-methods approach assessed attitudes towards guardian permission for the current survey and future online sexual health intervention research. Logistic regression models assessed differences by “outness” to a guardian. A framework matrix analysis was conducted to summarize, then aggregate, qualitative responses. Findings indicate that most AMSM would not participate if guardian permission was required (current: 83%; future: 87%). Youth who were not “out” were more likely to say they would not participate (current: AOR=2.8, 95%CI: 1.2–6.8); future: AOR=4.7, 95%CI: 1.6–13.5). Participants reported that guardian permission would be an invasion of their privacy, lead to involuntary “outing,” and endanger participants. Overall, guardian permission appears to be a barrier to AMSM participation in online sexual health research. Investigators and IRBs should consider alternative practices and policies to facilitate such research.
Keywords: Adolescent, MSM, sexual health, guardian permission, HIV
INTRODUCTION
Adolescent males interested in sex with males (AMSM) are at elevated risk for HIV in the United States, accounting for 93% of new infections among males in their age cohort (Centers for Disease Control and Prevention, 2016). Racial/ethnic minority AMSM are particularly vulnerable (Centers for Disease Control and Prevention, 2016). HIV infection among AMSM often results from early sexual experiences (Kann et al., 2016), or occurs later as a result of behavior patterns established during adolescence (Glick & Golden, 2014; Kann et al., 2016). Sexual education interventions that serve AMSM, preferably before sexual behavior patterns are formed, are essential to addressing HIV disparities among these youth.
Despite the need, there is a dearth of educational resources to prepare AMSM for healthy sexual activity. AMSM are less likely than their heterosexual peers to receive relevant sexual health information in school (Raifman, Beyrer, & Arrington-Sanders, 2018; Rasberry et al., 2018) or from their parents (Mustanski, Greene, Ryan, & Whitton, 2015). As a result, AMSM turn to the Internet where they obtain sexual health information and make connections with other AMSM (Mustanski, Lyons, & Garcia, 2011). AMSM use sexually explicit online media (SEOM) to learn the mechanics of sex, confirm their sexual attractions, and learn about gay culture (Arrington-Sanders et al., 2015; Kubicek, Beyer, Weiss, Iverson, & Kipke, 2010). Because the Internet is particularly influential on the sexual development of AMSM and because it can be an effective way to reach “hidden” populations in research (Lane, Armin, & Gordon, 2015), the Internet is an ideal location to provide sexual health interventions to AMSM.
Limited research has investigated the Internet’s potential to provide sexual health interventions to AMSM (Hergenrather, Emmanuel, Durant, & Rhodes, 2016; Ybarra et al., 2017). One barrier to such research is institutional review boards (IRBs) reluctance to approve waivers of guardian permission. This issue and a call for research in this area was first raised by Mustanski (2011). Subsequent research has documented guardian permission as a potential barrier to sexual and gender minority youth participation in online sexuality survey research (Macapagal, Coventry, Arbeit, Fisher, & Mustanski, 2017), HIV testing studies (Mustanski, Coventry, Macapagal, Arbeit, & Fisher, 2017), and pre-exposure prophylaxis (PrEP) prevention trials (Fisher, Arbeit, Dumont, Macapagal, & Mustanski, 2016). This research indicates that for these types of studies requiring guardian consent is likely to decrease participation rates, create a biased sample, and could lead to harm for the participants (Fisher et al., 2016; Macapagal et al., 2017; Mustanski, Coventry, et al., 2017). This is particularly true for sexual and gender minority youth who are not yet “out” to their guardians (Fisher et al., 2016; Macapagal et al., 2017; Mustanski, Coventry, et al., 2017). For these reasons, guardian consent waivers have been recommended by research ethics experts (Fisher & Mustanski, 2014; Mustanski & Fisher, 2016).
Regardless of expert recommendations, IRBs often fail to consider AMSM-unique risks related to requiring guardian permission (Fisher & Mustanski, 2014; Mustanski & Fisher, 2016). When IRBs decline to approve waivers of guardian permission they inadvertently hinder research that could form the evidential base for sexual health interventions for AMSM. The current study sought to provide IRBs and investigators with the information needed to make informed decisions around guardian permission for AMSM participation in online sexual health research; specifically with regard to AMSM’s willingness to participate in online sexual health interventions designed to increase youth’s ability to engage in health sexual relationships with male partners and decrease their HIV risk. We used mixed-methods to determine the extent to which guardian permission is a barrier to engagement in online sexual intervention research among AMSM, particularly for AMSM who are not “out” to their guardians.
This study builds on and extends previous research in this area (Fisher et al., 2016; Macapagal et al., 2017; Mustanski, Coventry, et al., 2017) in multiple ways. Previous studies included sexual and gender minority youth more broadly and had relatively small samples of AMSM (range of AMSM in previous studies n = 22 to 29). Our study represents the largest study to date (N = 206) of AMSM-specific attitudes towards guardian permission for sexual health research. Further, previous studies focused on sexual and gender minority youth attitudes towards guardian permission for an online survey about sexual health and sexual/gender minority identity (Macapagal et al., 2017), an HIV testing study (Mustanski, Coventry, et al., 2017), and a PrEP adherence trial (Fisher et al., 2016). Our study is the first to assess AMSM-specific attitudes towards guardian permission for online sexual health intervention research. Although guardian permission may serve as a barrier to sexual and gender minority youth participation in sexual health research generally, AMSM represent a unique population that experiences substantial sexual health disparities in the U.S. and is in need of tailored online sexual health interventions. Given this need, information on the challenges of obtaining (or waiving) guardian permission for this specific research is imperative.
METHOD
Study Design
Closed and open-ended questions were imbedded in a cross-sectional survey designed to inform the development of an online-administered sexual health intervention for AMSM (ages 14–17). Participants were recruited June-July 2017 via online advertisements and posts on social media sites (e.g., Instagram). Social media advertisements/posts included GIFs and static images that featured young men and emoji. Text focused on participating in an online survey to help researchers develop a more inclusive online sexual health program. To optimize racial/ethnic diversity and increase the potential that advertisements/posts would be seen by males who are interested in male sexual partners, but not necessarily identify as gay/bisexual, advertisements/posts were broadly targeted to 14–17 year old males in the U.S. who were identified by the Facebook/Instagram algorithms as interested in topics our youth advisory board and our own research generated as popular among racial/ethnic minority AMSM (e.g., King Bach, Kim Kardashian, RuPaul’s Drag Race, Todrick Hall, Shakira, Rihanna). Eligibility criteria were: (1) age 14 to 17, (2) cisgender male, (3) self-identify as gay/bisexual, report being sexually attracted to males, or report having voluntary sexual contact with a male partner (past year), (4) reside in the US, (5) have a personal email address, and (6) be new to the study.
Upon clicking on an advertisement or social media post, potential participants were directed to the survey website, hosted using REDCap (Harris et al., 2009), which described the study and asked respondents to continue for eligibility questions. To protect against fraudulent entries or multiple enrollments, screening and survey responses were cross-referenced against: date of birth, location, sexual activity, and email address (Bowen, Daniel, Williams, & Baird, 2008; Sullivan, Grey, & Simon Rosser, 2013).
After screening, respondents progressed to consent material. We adapted procedures used by Newcomb et al. (2014); thus, capacity to consent was confirmed via four questions that evaluated respondents’ ability (1) to name things they would be expected to do during the study, (2) to explain what they would do if they no longer wished to participate in the study, (3) to explain what they would do if they experienced distress during the study, and (4) to identify potential risks for participating in the study (Dunn & Jeste, 2001; Newcomb & Mustanski, 2014; The University of California at San Diego Task Force on Decisional Capacity, 2003). Specifically, participants were asked: (1) “If you agree to be in this study, what are we asking you to do?” (2) “What should you do if you no longer want to be in this study?” (3) “What can you do if you experience distress while taking part in this study?” and (4) “What are the potential risks of being in this study?” Respondents unable to answer all four questions after three tries were ineligible. Those who consented received an email containing a unique survey link. The survey took 30 minutes (SD=12) on average. Participants who completed the survey received a $15 Amazon.com gift code by email. All procedures, including a waiver of guardian consent, were reviewed and approved by our hospital IRB.
Measures
The survey covered multiple potentially sensitive topics (e.g., sexual behaviors, SEOM use, and sexual education exposure/needs) in addition to questions about guardians and ethical issues. For this manuscript, we report on socio-demographics, “outness” to guardians, and attitudes towards guardian permission.
Socio-demographics.
Characteristics included recruitment source (Instagram, Facebook/other), census region of the U.S. (northeast, midwest, south, west), age (continuous), race/ethnicity (White, Black/African American, Latino, Mixed Race/Other), enrollment in school (yes, no), highest education level (< 9th grade, 9th, 10th, 11th grade or more), living situation (in guardians’ home, other), urbanicity (metropolitan residence, other; University of North Dakota Center for Rural Health, 2014), employment (unemployed, employed ≥ part-time), sexual orientation (gay-identified, other), and age realized sexually attracted to men (continuous). “Other” in recruitment source includes from a friend (n = 11) or participants who reported “other” as their source (n = 3). Census region was designated using self-reported state of residence (U.S. Department of Commerce Economics and Statistics Administration, 2015).
Guardians.
Participants indicated whether they had told their guardian(s) that they are sexually attracted to other boys/males (yes, no; Glick & Golden, 2014). Separate questions assessing primary and secondary guardian (if they had one) were combined to form a variable indicating whether they were “out” with at least one guardian (0,1).
Attitudes towards guardian permission.
Guardian permission questions were adapted from previous work (Fisher et al., 2016). At the end of the survey, participants rated if (a) they would have participated in the current survey if a guardian’s permission had been required (yes, no), (b) researchers should require a guardian’s permission for this type of survey (yes, no), and (c) they agreed (4-point likert scale) with reasons why researchers should (e.g., “they could help explain the risks and benefits to me”) and should not (e.g., “they might punish me”) require guardian permission. Other reasons researchers should and should not get written guardian permission for this type of survey were assessed in an open-ended format.
Participants then read the following description of a future study involving an online sexual health intervention:
“The next set of questions asks about how you might feel about getting written parental/guardian permission for the study of the online sexual health program we are designing. Participants will be asked to fill out a survey, complete the developed sexual health program or use an alternative source of online sexual health information, and then fill out two additional surveys (one right after they complete the intervention and one 3 months later). The surveys will contain information similar to what you just filled out. The sexual health program will take about 90 minutes to complete and will include a discussion of online pornography.”
Participants were then asked questions that mirrored the questions and response options they answered about the current survey (described in the previous section; i.e., would they participate, should guardian permission be required, reasons to require guardian permission, reasons against requiring guardian permission, and open-ended options for and against guardian permission).
Analyses
Quantitative analysis.
Socio-demographic differences by outness with a guardian were assessed using t- and χ2 tests. Logistic regression models assessed differences in attitudes towards guardian permission by outness with a guardian. Race/ethnicity, age, and sexual orientation were controlled for in adjusted multivariable logistic regression models. Of the 206 AMSM, 34 (17%) had missing data on ≥ 1 guardian permission attitude variables. To assess socio-demographic differences between participants with missing data versus those with complete data, we conducted t- and χ2 tests. Participants with missing data were more likely to live outside a metropolitan area (31% vs. 14%, p = 0.03). There were no other socio-demographic differences.
Qualitative analysis.
Two coders from the study team independently reviewed answers to the four open-ended questions ([1] other reasons to require guardian permission for the current survey; [2] other reasons against requiring guardian permission for the current survey; [3] other reasons to require guardian permission for the future intervention study; [4] other reasons against requiring guardian permission for the future intervention study) and identified emergent concepts. The coders agreed upon a set of initial codes, which included deductive codes drawn from research questions (e.g., guardians could provide help with the logistics of participation) and inductive codes representing concepts raised in participant answers (e.g., participants feel capable of consenting themselves). The codebook was revised throughout. Data from the open-ended questions were double-coded and disagreements were resolved through discussions between the coders.
Finalized codes, and the answers assigned to them, were entered into NVivo 11 (NVivo qualitative data analysis software, 2012). Cohen’s kappa for the final codes ranged from 0.83 to 1.00, indicating excellent interrater reliability (McHugh, 2012). A framework matrix analysis was conducted to summarize, aggregate, and establish frequencies of code endorsement (Green & Thorogood, 2013). A mixed-methods analysis was conducted to explore whether endorsement of codes differed according to whether participants had disclosed their sexual attraction to male partners (“out”) to their guardians. In accordance with prior studies (Magee, Bigelow, Dehaan, & Mustanski, 2012; Mustanski, Coventry, et al., 2017), we performed these analyses only on codes endorsed by at least five participants, and considered differences by outness in code application rates of at least 20% to be meaningful.
To assess socio-demographic differences between participants who responded to open-ended questions versus those who did not, we conducted t- and χ2 tests. Most participants (n = 122, 59%) answered at least one of the open-ended questions. Participants recruited through Facebook/Other were more likely to have answered at least one of the open-ended questions compared to those recruited through Instagram (76% vs. 56%, χ2 = 4.4, p = 0.04). There were no other socio-demographic differences.
RESULTS
Participants
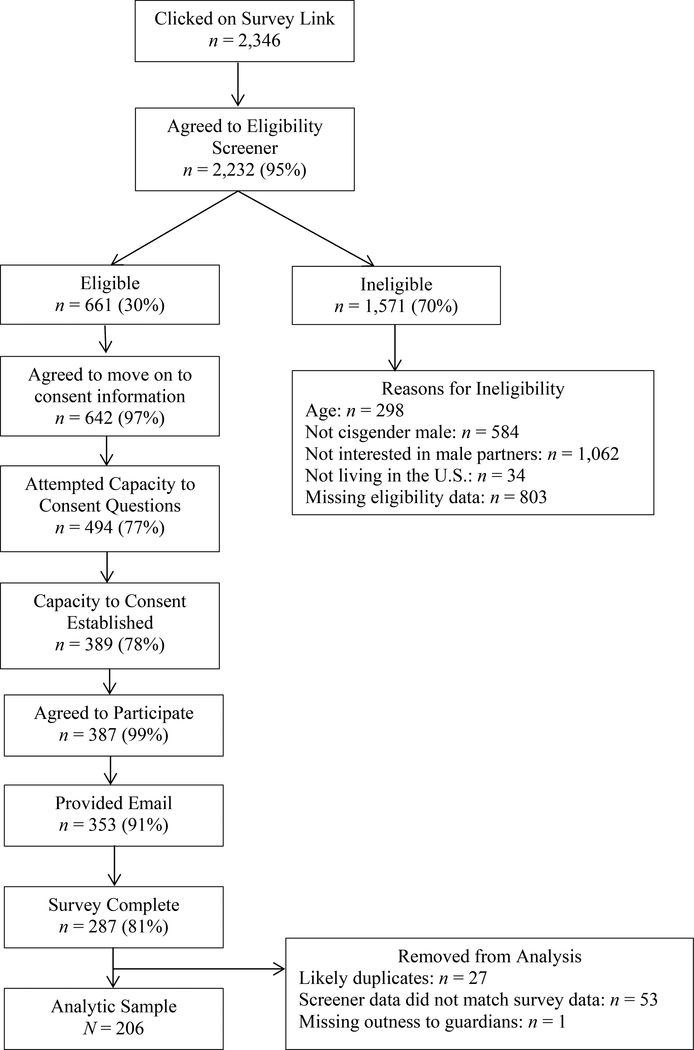
A total of 2,346 potential participants clicked on the survey link, 2,232 (95%) agreed to the screener, and 661 (30%) were eligible (see Figure 1). About half of the eligible respondents (n = 353; 53%) completed the consent process, agreed to participate, and were emailed the survey. Of these, 287 (81%) completed the survey. Eighty (28%) participants were excluded due to internal discrepancies suggesting ineligibility or a potential duplicate. One (0.3%) participant had missing data about outness with a guardian. This left a final analytic sample of 206 AMSM.
Figure 1:
Study Flow Diagram
There were two steps in the process where there were differences in attrition by socio-demographics collected in the screener (age, race/ethnicity, sexual orientation). First, those who identified as gay were more likely to attempt the capacity to consent questions compared to those who did not (80% vs. 73%, χ2 = 4.6, p = 0.02). Second, Mixed Race/Other individuals were more likely to establish capacity to consent compared to White, Black/African American, and Latino individuals (White: 78% vs. Black/African American: 82% vs. Latino: 72% vs. Mixed Race/Other: 90%, χ2 = 8.3, p = 0.04). There were no other socio-demographic differences in attrition.
The average age of participants was 16 years (SD = 1.0) and half (53%) were “out” to ≥1 guardian(s) (see Table 1). The majority (84%) were recruited via Instagram. Participants reported living in 40 states (17% Northeast, 20% Midwest, 29% South, and 34% West). Approximately half (48%) identified as racial/ethnic minorities, almost all (95%) were enrolled in school, most (93%) lived at home with their parents/guardians, and the majority (87%) lived in a metropolitan area. Two-thirds (66%) self-identified as gay. Participants who were “out” with at least one guardian were more likely to be enrolled in school (98% vs. 92%, p = 0.03) and gay-identified (74% vs. 56%, p < 0.01). There were no other socio-demographic differences by “outness.”
Table 1.
Socio-demographics by outness with at least one guardian among 14 to 17 year old males who are interested in male sexual partners in the United States.
| Total | Not out | Out | ||
|---|---|---|---|---|
| N = 206 | n = 97 | n = 109 | ||
| Socio-demographics | n (%) | n (%) | n (%) | X2 |
| Recruitment source | 0.9 | |||
| 173 (84) | 79 (81) | 94 (86) | ||
| Facebook/Other | 33 (16) | 18 (18) | 15 (14) | |
| Region | 1.2 | |||
| Northeast | 34 (17) | 16 (17) | 18 (17) | |
| Midwest | 41 (20) | 17 (18) | 24 (23) | |
| South | 58 (29) | 28 (29) | 30 (29) | |
| West | 69 (34) | 36 (37) | 33 (31) | |
| Age (in years) | 4.6 | |||
| 14 | 32 (16) | 18 (19) | 14 (13) | |
| 15 | 51 (25) | 23 (24) | 28 (26) | |
| 16 | 68 (33) | 36 (37) | 32 (29) | |
| 17 | 55 (27) | 20 (21) | 35 (32) | |
| Race/Ethnicity | 4.6 | |||
| White | 107 (52) | 52 (54) | 55 (51) | |
| Black/African American | 30 (15) | 17 (18) | 13 (12) | |
| Latino | 42 (20) | 14 (14) | 28 (26) | |
| Mixed Race/Other | 25 (12) | 13 (14) | 12 (11) | |
| Currently enrolled in school | 196 (95) | 89 (92) | 106 (98) | 4.5* |
| Highest level of education achieved | 2.1 | |||
| Less than 9th grade | 26 (13) | 13 (14) | 13 (12) | |
| 9th grade | 49 (24) | 27 (28) | 22 (21) | |
| 10th grade | 51 (26) | 24 (25) | 27 (26) | |
| 11th grade or more | 74 (37) | 31 (33) | 43 (41) | |
| Live in guardian(s) home | 191 (93) | 87 (90) | 104 (95) | 2.5 |
| Metropolitan residence | 169 (87) | 79 (87) | 90 (87) | 0.0 |
| Ever been homeless | 12 (6) | 8 (8) | 4 (4) | 2.0 |
| Employed at least part-time | 71 (34) | 30 (31) | 41 (38) | 1.0 |
| Gay identified | 136 (66) | 54 (56) | 82 (75) | 8.8** |
| m (SD) | m (SD) | m (SD) | t | |
| Age realized sexually attracted to males | 12 (2) | 12 (2) | 12 (2) | −1.5 |
p<0.05
p<0.01.
Participation if Guardian Permission is Required
Most AMSM would not participate in either the current survey or the future study if guardian permission was required (current: 83%; future: 87%; see Table 2). Compared to youth who were “out” to ≥ 1 guardian(s), youth who were not “out” had almost 3 times greater odds of reporting that they would not participate in the current survey (Adjusted Odds Ratio [AOR]=2.9, 95% Confident Interval [CI]: 1.2–6.8), and approximately 5 times greater odds of reporting that they would not participate in the future intervention study (AOR=4.8, 95%CI: 1.7–13.9), if guardian permission was required. Regardless of “outness,” almost all participants felt that guardian permission should not be required (current: 94%; future: 98%).
Table 2.
Associations between guardian permission questions and not being out with at least one guardian among 14 to 17 year old males who are interested in male sexual partners in the United States.
| Total | Not Out | Out | |||
|---|---|---|---|---|---|
| N = 206 | n = 97 | n = 109 | |||
| n (%) | n (%) | n (%) | OR (95% CI) | AOR (95% CI) | |
| Current Survey | |||||
| would not participate if guardian permission was required | 171 (83) | 87 (90) | 84 (77) | 2.6 (1.2, 5.7) | 2.9 (1.2, 6.8) |
| guardian permission should not be required | 193 (94) | 92 (96) | 101 (93) | 1.8 (0.5, 6.3) | 2.2 (0.6, 8.0) |
| Future Study | |||||
| would not participate if guardian permission was required | 179 (87) | 91 (95) | 88 (81) | 4.3 (1.5, 12.0) | 4.8 (1.7, 13.9) |
| guardian permission should not be required | 202 (98) | 96 (99) | 106 (97) | 2.7 (0.3, 26.5) | 2.3 (0.2, 24.6) |
Note: OR = Odds Ratio, AOR = Adjusted Odds Ratio; AOR adjusted for race/ethnicity, age, and sexual orientation.
Reasons to Require Guardian Permission
Quantitative Data.
Half of the AMSM agreed with the investigator-nominated reasons that guardian permission should be required for the current survey (range: 43–54%) or future study (range: 44–54%; see Table 3). The only differences by “outness” in agreement with these reasons was that guardian permission provided opportunities for parents to explain research risks and benefits for the current survey: AMSM who were not “out” were less likely to agree with this reason (AOR=0.5, 95%CI: 0.3–0.9).
Table 3.
Associations between agreeing with reasons to require guardian permission and not being out with at least one guardian among 14 to 17 year old males who are interested in male sexual partners in the United States.
| Total | Not out | Out | |||
|---|---|---|---|---|---|
| N = 206 | n = 97 | n = 109 | |||
| n (%) | n (%) | n (%) | OR (95% CI) | AOR (95% CI) | |
| Current Survey | |||||
| they could explain the risks and benefits to me | 88 (43) | 36 (37) | 52 (48) | 0.6 (0.4, 1.1) | 0.5 (0.3, 0.9) |
| they could help me say no to the researchers if I didn’t feel comfortable enough to do it myself | 111 (54) | 48 (50) | 62 (57) | 0.7 (0.4, 1.3) | 0.7 (0.4, 1.2) |
| they could answer questions I had after taking the survey | 91 (44) | 38 (39) | 53 (49) | 0.7 (0.4, 1.2) | 0.6 (0.3, 1.1) |
| Future Study | |||||
| they could explain the risks and benefits to me | 90 (44) | 38 (40) | 51 (47) | 0.7 (0.4, 1.3) | 0.6 (0.3, 1.1) |
| they could help me say no to the researchers if I didn’t feel comfortable enough to do it myself | 111 (54) | 47 (49) | 64 (59) | 0.7 (0.4, 1.2) | 0.6 (0.3, 1.0) |
| they could answer any follow-up questions I had about the information provided in the sexual health program | 95 (47) | 38 (40) | 56 (52) | 0.6 (0.3, 1.0) | 0.5 (0.3, 1.0) |
| they could help remind me to complete the follow-up assessments | 101 (50) | 44 (47) | 57 (54) | 0.8 (0.4, 1.3) | 0.7 (0.4, 1.2) |
Note: OR = Odds Ratio, AOR = Adjusted Odds Ratio; AOR adjusted for race/ethnicity, age, and sexual orientation.
Qualitative Data.
Of those who responded to the open-ended question regarding the current survey (n = 91) or the future study (n = 56), one of the most frequently endorsed reasons for why guardian permission should be required was that guardians could support youth as they participated (current: 24%; future: 32%). For example, one participant noted, “My Papa could help me understand questions after survey” (15 years old, Latino, “out” with a guardian). Another participant wrote, “They could help me if I was unsure what I was thinking” (17 years old, Black/African American, “out” with a guardian), and another stated “They could go through it with me” (14 years old, Black/African American, not “out” with a guardian). There was not a meaningful difference in the frequency of endorsement of this potential benefit between those who were “out” compared to those who were not “out” with a guardian (current: 33% vs. 15%; future: 41% vs. 22%).
Interestingly, in response to this question, many participants took this opportunity to voice their opposition to the assertion that parental permission should be required (current: 36%; future: 27%). The majority of these responses simply stated, as one participant did, “they shouldn’t” (15 years old, Mixed Race/Other, “out” with a guardian). Some participants were specific about reasons why guardian permission should not be required. For example, one stated, “Its uncomfortable and I would lie on the survey if parental consent was required” (15 years old, White, “out” with a guardian). Participants who were “out” gave this type of response less often than those who were not “out” for the future intervention study (current: 27% vs. 46%; future: 10% vs. 44%).
Reasons Against Requiring Guardian Permission
Quantitative Data.
Most AMSM agreed guardian permission might lead to questions about their sexual behaviors (current: 92%; future: 91%) and SEOM use (current: 89%; future: 90%) or to being “outed” (current: 80%; future: 78%) (Table 4). Compared to participants who were “out,” those who were not “out” were more likely to feel that they would be punished (current: AOR=2.3, 95%CI: 1.3–4.1; future: AOR=3.2, 95%CI: 1.7–6.0), “outed” (current: AOR=8.9, 95%CI: 3.4–23.7; future: AOR=14.8, 95%CI: 4.9–45.0), kicked out of the house (current: AOR=3.3, 95%CI: 1.6–6.7; future: AOR=2.6, 95%CI: 1.3–5.2), or forced to speak with a counselor/religious person (current: AOR=2.1, 95%CI: 1.2–3.9; future: AOR=1.9, 95%CI: 1.1–3.5) if guardian permission was required. Regardless of “outness,” the majority (87%) reported that it would be very easy or easy for them to say no to a researcher if they did not want to participate.
Table 4.
Associations between agreeing with reasons against requiring guardian permission and not being out with at least one guardian among 14 to 17 year old males who are interested in male sexual partners in the United States.
| Total | Not out | Out | |||
|---|---|---|---|---|---|
| N = 206 | n = 97 | n = 109 | |||
| n (%) | n (%) | n (%) | OR (95% CI) | AOR (95% CI) | |
| Current Survey | |||||
| they might punish me | 99 (48) | 58 (60) | 41 (38) | 2.5 (1.4, 4.4) | 2.3 (1.3, 4.1) |
| they might start asking about my sexual behavior | 189 (92) | 91 (94) | 97 (90) | 1.7 (0.6, 4.8) | 1.7 (0.6, 5.0) |
| they might start asking about my pornography use | 183 (89) | 85 (88) | 97 (90) | 0.8 (0.3, 1.9) | 0.7 (0.3, 1.8) |
| they might find out that I am gay, bisexual, or interested in sex with male partners | 164 (80) | 91 (94) | 73 (68) | 7.1 (2.8, 17.7) | 8.9 (3.4, 23.7) |
| they might kick me out of the house | 49 (24) | 34 (35) | 15 (14) | 3.4 (1.8, 6.8) | 3.3 (1.6, 6.7) |
| they might make me talk to a counselor or religious person | 95 (46) | 54 (56) | 41 (38) | 2.1 (1.2, 3.6) | 2.1 (1.2, 3.9) |
| Future Study | |||||
| they might punish me | 102 (50) | 62 (66) | 40 (37) | 3.3 (1.8, 5.9) | 3.2 (1.7, 6.0) |
| they might start asking me about my sexual behavior | 186 (91) | 93 (98) | 93 (86) | 7.5 (1.7, 33.7) | 7.4 (1.5, 35.5) |
| they might start asking me about pornography use | 182 (90) | 88 (93) | 94 (87) | 1.9 (0.7, 4.9) | 1.7 (0.6, 4.9) |
| they might find out that I am gay, bisexual, or interested in sex with male partners | 157 (78) | 91 (96) | 66 (62) | 13.8 (4.7, 40.4) | 14.8 (4.9, 45.0) |
| they might kick me out of the house | 48 (24) | 32 (34) | 16 (15) | 3.0 (1.5, 5.9) | 2.6 (1.3, 5.2) |
| they might make me talk to a counselor or religious person | 94 (47) | 53 (56) | 41 (38) | 2.0 (1.2, 3.6) | 1.9 (1.1, 3.5) |
Note: OR = Odds Ratio, AOR = Adjusted Odds Ratio; AOR adjusted for race/ethnicity, age, and sexual orientation.
Qualitative Data.
Of those who responded to the open-ended question asking them to elaborate on other reasons why guardian permission should not be required for the current survey (n = 112) or the future study (n = 70), the most common reasons given were that (a) requiring guardian permission would be an invasion of privacy (current: 31%; future: 19%), (b) it would be uncomfortable (current: 16%; future: 19%), and (c) it could be dangerous (current: 22%; future: 23%). There were no meaningful differences in the frequency of endorsement of these reasons by “outness” with a guardian.
For responses that highlighted privacy, most participants stated something like the sentiments of two participants: “It’s an invasion of privacy” (16 years old, Latino, “out” with a guardian) and “Sometimes kids like to keep this information to themselves” (17 years old, Black/African American, “out” with a guardian). Some participants were more nuanced in their language. For example, one participant stated, “It’s not their business. It’s not their choice. The law should be more considerate to recognize teens as people with rights of privacy too” (15 years old, Black/African American, not “out” with a guardian). Another stated, “I should have some amount of personal freedom to share my own personal experiences with a researcher without my parents being involved.” (14 years old, White, not “out” with a guardian).
When talking about guardian permission for sexual health research being uncomfortable, participants often noted that they did not want to talk with their guardians about these topics. As one participant said, “I don’t talk to my parents about stuff like this because I don’t feel comfortable doing it and I feel like I don’t have to.” (15 years old, White, not “out” with a guardian). Another stated, “[it] is awkward to discuss with a person who upholds you to a standard of ‘innocence,’ like being abstinent and heterosexual.” (16 years old, Latino, not “out with a guardian). Stated another way, “since these questions are pretty personal, a lot of teens would not feel comfortable with their parents knowing” (15 years old, White, not “out” with a guardian). Many participants stated sentiments similar to this participant: “It could make people uncomfortable” (14 years old, Mixed Race/Other, not “out” with a guardian).
Youth felt that requiring guardian permission could be dangerous. One participant stated, “for some people it could be really dangerous for their guardian(s) to find out if they are unsupportive and the participant is dependent on them” (16 years old, White, not “out” to a guardian) whereas another wrote, “It’s not always safe to have parents’ permission on a topic like this” (17 years old, Mixed Race/Other, “out” to a guardian). Some feared consequences to requiring guardian permission such as “They could kick me out or punish me” (14 years old, Black/African American, not “out” to a guardian) or “Because we could be disowned or something” (17 years old, Latino, “out” to a guardian).
DISCUSSION
AMSM experience increased risk for HIV acquisition (Centers for Disease Control and Prevention, 2016) and decreased access to relevant sexual education (Raifman et al., 2018; Rasberry et al., 2018). In lieu of relevant sexual education, AMSM turn to the Internet to obtain sexual health information and to locate sexual health-related services (DeHaan, Kuper, Magee, Bigelow, & Mustanski, 2013; Magee et al., 2012). Although AMSM frequently use the Internet to find sexual health information and locate services, they also recognize that the Internet can be an unreliable source (DeHaan et al., 2013; Magee et al., 2012). Online sexual health interventions for these youth have the potential not only to meet them where they are already seeking sexual health information, but also to help them develop the necessary skills to critically examine the information available online and dispel myths that may be presented (Nelson & Carey, 2016).
Despite the importance of tailored sexual health interventions for AMSM that address the misinformation they may be receiving online, there has been limited research among AMSM < 18 years old to guide the development of interventions for these youth. A barrier to the inclusion of AMSM in sexual health research is the stance that many IRBs take in requiring guardian permission for research involving under age AMSM. Federal regulations permit IRBs to waive guardian permission when research is minimal risk or when such permission is not a reasonable protection for the child (U.S. Department of Health and Human Services, 2009). The few online sexual health studies that have been conducted with AMSM have received waivers of guardian permission, indicating that waivers of guardian permission can be successfully obtained for this work from some IRBs (Bauermeister et al., 2015; Mustanski, Garofalo, Monahan, Gratzer, & Andrews, 2013; Mustanski et al., 2015; Ybarra et al., 2017). Empirical evidence on the barriers and potential harms guardian permission poses to online sexual health research among AMSM is essential to making informed judgments regarding the risks and benefits of this requirement (Fisher & Mustanski, 2014; Mustanski & Fisher, 2016). To provide IRBs and investigators with the information they need to make ethical decisions around guardian permission for online sexual health research with AMSM, we examined AMSM attitudes towards guardian permission for an online sexual health survey and for a future online sexual health intervention trial.
In this sample, AMSM overwhelmingly reported that they would not have participated in the current survey or a future online sexual health intervention study if guardian permission was required. This was particularly true for individuals who were not “out” to their guardian(s); these AMSM were three times more likely to say they would not have participated in the survey and five times more likely to say they would not participate in the intervention study. Further, regardless of “outness” with a guardian, almost all participants felt that guardian permission should not be required for this type of research. These findings are in line with similar findings that requiring guardian permission would decrease participation in sexuality-focused online survey research, HIV testing studies, and PrEP prevention trials among sexual and gender minority youth (Fisher et al., 2016; Macapagal et al., 2017; Mustanski, Coventry, et al., 2017).
Only about half of the participants agreed with proposed reasons why guardian permission should be required. Previous research regarding HIV testing among sexual and gender minority adolescents found that <10% of participants endorsed similar reasons for requiring guardian permission (Mustanski, Coventry, et al., 2017). Measurement difference may explain these two findings. In the HIV testing study participants were provided a list of potential reasons and asked to “check all that apply” (Mustanski, Coventry, et al., 2017). In the current study, participants indicated how much they agreed or disagreed with each potential reason. Asking participants to indicate agreement may capture more nuanced data about participant’s attitudes. Research should examine the best methods of measuring the risks and benefits of guardian permission among AMSM.
Most participants endorsed multiple reasons why guardian permission could be detrimental, including concerns that it would be an invasion of their privacy, lead to unwanted “outing,” and endanger participants. Participants also felt that requiring guardian permission would lead to uncomfortable conversations with their guardian(s), which could serve as a barrier to participation. These findings supplement the results of previous smaller studies with sexual and gender minority youth that found that requiring guardian permission would bias samples and may lead to harm for participants (Fisher et al., 2016; Macapagal et al., 2017; Mustanski, Coventry, et al., 2017).
Guardian permission requirements are predicated on assumptions that guardian decisions reflect the best interest of the child and protect the child from harms, and that youth are incapable of making informed decisions on their own or will have difficulty saying no to researchers. Our results as well as related research indicate that these assumptions may not hold true (Fisher et al., 2016; Macapagal et al., 2017; Mustanski, Coventry, et al., 2017). Specifically, guardians may make decisions based on their own beliefs about sexuality rather than focusing on the risks and benefits of youth participation (Macapagal et al., 2017). Further, requiring guardian permission has the potential to increase risks for some participants, especially for those with guardians who do not support their child’s sexual preferences. Research also indicates that ≥ 14 year old adolescents understand the nature of research and participant rights at the same level as adults (Fisher et al., 2016; Koelch et al., 2009). Finally, our results, in line with previous HIV-specific research (Fisher et al., 2016; Mustanski, Coventry, et al., 2017), found that the majority of adolescents feel capable of declining participation in online sexual health research on their own.
As guardian permission appears to serve as a barrier to participation and may not be necessary to protect AMSM participating in online sexual health research, it is important for researchers and IRBs to consider alternative ways to protect AMSM participating in this critical work. One means to protect these youth is to create a consent process that matches the developmental and educational status of participants (Fisher et al., 2016; Fisher & Mustanski, 2014; Mustanski & Fisher, 2016). Research on optimizing consent among youth recommends a process that includes multimedia presentations, quizzes to assess understanding, and an emphasis on the potential benefits of the research for youth (Mustanski, Coventry, et al., 2017; Sineath et al., 2014). Additional research assessing the best way to present online consent materials that are understandable, engaging, and optimizes adolescents’ ability to make informed and voluntary participation is warranted.
The limitations of this study should be considered. Although this study presents data from a relatively large and diverse sample, the findings may not generalize to other youth, such as transgender or youth interested exclusively in opposite-sex partners. Further, participants were recruited through advertisements on social media platforms. It is possible that youth who click on an advertisement for a sexual health study differ from youth who do not. As social media websites are commonly used for recruiting sexual minority youth (e.g., Mustanski et al., 2015; Ybarra et al., 2017), it is important to assess potential bias that results from these methods. Notably, only 206 (31%) of the 661 eligible individuals completed the study and were included in the analyses. Differential attrition in this study occurred primarily during the consent process, lending further support regarding the need for effective and efficient online consent processes for sexual health research. Although attrition is not unusual in online research, additional investigation assessing ways to decrease attrition generally and statistical means to address potential biases introduced by attrition in online research is needed (Hochheimer et al., 2016). Lastly, our participants reported on their perceptions of how their guardians would react to their participation in online sexual health research. These assumptions may not accurately reflect how guardians may react. Two U.S. studies found that guardians understand the importance of guardian permission waivers for HIV research and believe that waivers of guardian permission increase study validity and reduce obstacles to participation (Mustanski, Macapagal, et al., 2017; Newcomb, Clifford, Greene, & Mustanski, 2016). Additional research assessing guardian attitudes towards AMSM participation in online sexual health research and guardian permission requirements, especially among guardians who are less likely to be accepting of their adolescent’s sexual preferences, is needed.
In conclusion, AMSM are getting most of their sexual health information from the Internet, likely without guardian permission or awareness. Research on online sexual health interventions for AMSM is critical to ensure the creation of efficacious sexual health programs that provide essential information and increase AMSM ability to engage in healthy sexual relationships. Requiring guardian permission for this research would likely exclude youth who are not “out” to their guardians or do not feel comfortable asking for guardian permission. AMSM who are not “out” or have unsupportive families are at increased risk for adverse health outcomes (Glick & Golden, 2014; Ryan, Huebner, Diaz, & Sanchez, 2009). Eliminating these youth from online sexual health research will bias our understanding of their needs which, in turn, will undermine the development of efficacious online sexual health interventions. Among the advantages of conducting online sexual health intervention research with AMSM is the removal of interpersonal, geographic, logistical, and stigma-based barriers to participation (Lane et al., 2015; Mustanski, 2015). Given our results, guardian permission appears to potentially create a significant barrier to the online sexual health research needed to promote sexual well-being and decrease HIV risk among AMSM. Therefore, we recommend that investigators and IRBs reevaluate this practice and consider alternative procedures and policies to facilitate this research with AMSM.
Acknowledgements:
We would like to thank our research assistant Jaime Ramirez. Funding for the study came from R25 DA031608 and K23 MH109346. The content of this publication is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
REFERENCES
- Arrington-Sanders R, Harper GW, Morgan A, Ogunbajo A, Trent M, & Fortenberry JD (2015). The role of sexually explicit material in the sexual development of same-sex-attracted Black adolescent males. Archives of Sexual Behavior. 44, 597–608. 10.1007/s10508-014-0416-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Pingel ES, Jadwin-Cakmak L, Harper GW, Horvath K, Weiss G, & Dittus P (2015). Acceptability and preliminary efficacy of a tailored online HIV/STI testing intervention for young men who have sex with men: the Get Connected! program. AIDS and Behavior, 19, 1860–1874. 10.1007/s10461-015-1009-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen AM, Daniel CM, Williams ML, & Baird GL (2008). Identifying multiple submissions in Internet research: preserving data integrity. AIDS and Behavior, 12, 964–973. 10.1007/s10461-007-9352-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2016). HIV Surveillance Report, 2015; vol 27 Atlanta, GA: Centers for Disease Control and Prevention; Retrieved from http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. [Google Scholar]
- DeHaan S, Kuper LE, Magee JC, Bigelow L, & Mustanski BS (2013). The interplay between online and offline explorations of identity, relationships, and sex: A mixed-methods study with LGBT youth. Journal of Sex Research, 50, 421–434. 10.1080/00224499.2012.661489 [DOI] [PubMed] [Google Scholar]
- Dunn LB, & Jeste DV (2001). Enhancing informed consent for research and treatment. Neuropsychopharmacology, 24, 595–607. 10.1016/S0893-133X(00)00218-9 [DOI] [PubMed] [Google Scholar]
- Fisher CB, Arbeit MR, Dumont MS, Macapagal K, & Mustanski B (2016). Self-consent for HIV prevention research involving sexual and gender minority youth: Reducing barriers through evidence-based ethics. Journal of Empirical Research on Human Research Ethics, 11, 3–14. 10.1177/1556264616633963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher CB, & Mustanski B (2014). Reducing health disparities and enhancing the responsible conduct of research involving LGBT youth. Hastings Center Report, 44, S28–S31. 10.1002/hast.367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glick SN, & Golden MR (2014). Early male partnership patterns, social support, and sexual risk behavior among young men who have sex with men. AIDS and Behavior, 18, 1466–1475. 10.1007/s10461-013-0678-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green J, & Thorogood N (2013). Qualitative Methods for Health Research (Third Edition edition). SAGE Publications Ltd. [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42, 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hergenrather KC, Emmanuel D, Durant S, & Rhodes SD (2016). Enhancing HIV prevention among young men who have sex with men: A systematic review of HIV behavioral interventions for young gay and bisexual men. AIDS Education And Prevention, 28, 252–271. 10.1521/aeap.2016.28.3.252 [DOI] [PubMed] [Google Scholar]
- Hochheimer CJ, Sabo RT, Krist AH, Day T, Cyrus J, & Woolf SH (2016). Methods for evaluating respondent attrition in web-based surveys. Journal of Medical Internet Research, 18, e301 10.2196/jmir.6342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kann L, Olsen EO, McManus T, Harris WA, Shanklin SL, Flint KH, … Zaza S (2016). Sexual identity, sex of sexual contacts, and health-related behaviors among students in grades 9–12 - United States and selected sites, 2015. Morbidity and Mortality Weekly Report. Surveillance Summaries, 65, 1–202. 10.15585/mmwr.ss6509a1 [DOI] [PubMed] [Google Scholar]
- Koelch M, Singer H, Prestel A, Burkert J, Schulze U, & Fegert JM (2009). “...because I am something special” or “I think I will be something like a guinea pig”: Information and assent of legal minors in clinical trials – assessment of understanding, appreciation and reasoning. Child and Adolescent Psychiatry and Mental Health, 3, 2 10.1186/1753-2000-3-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubicek K, Beyer WJ, Weiss G, Iverson E, & Kipke MD (2010). In the dark: young men’s stories of sexual initiation in the absence of relevant sexual health information. Health Educ Behav, 37, 243–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane TS, Armin J, & Gordon JS (2015). Online recruitment methods for web-based and mobile health studies: A review of the literature. Journal of Medical Internet Research, 17(7), e183 10.2196/jmir.4359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macapagal K, Coventry R, Arbeit MR, Fisher CB, & Mustanski B (2017). “I won’t out myself just to do a survey”: Sexual and gender minority adolescents’ perspectives on the risks and benefits of sex research. Archives of Sexual Behavior, 46, 1393–1409. 10.1007/s10508-016-0784-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magee JC, Bigelow L, Dehaan S, & Mustanski BS (2012). Sexual health information seeking online: A mixed-methods study among lesbian, gay, bisexual, and transgender young people. Health Education & Behavior, 39, 276–289. 10.1177/1090198111401384 [DOI] [PubMed] [Google Scholar]
- McHugh ML (2012). Interrater reliability: the kappa statistic. Biochemia Medica, 22, 276–282. [PMC free article] [PubMed] [Google Scholar]
- Mustanski B (2011). Ethical and regulatory issues with conducting sexuality research with LGBT adolescents: A call to action for a scientifically informed approach. Archives of Sexual Behavior, 40, 673–686. 10.1007/s10508-011-9745-1 [DOI] [PubMed] [Google Scholar]
- Mustanski B (2015). Future directions in research on sexual minority adolescent mental, behavioral, and sexual health. Journal of Clinical Child & Adolescent Psychology, 44, 204–219. 10.1080/15374416.2014.982756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Coventry R, Macapagal K, Arbeit MR, & Fisher CB (2017). Sexual and gender minority adolescents’ views on HIV research participation and parental permission: A mixed-methods study. Perspectives on Sexual and Reproductive Health, 49, 111–121. 10.1363/psrh.12027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, & Fisher CB (2016). HIV rates are increasing in gay/bisexual teens: IRB barriers to research must be resolved to bend the curve. American Journal of Preventive Medicine. 51, 249–252. 10.1016/j.amepre.2016.02.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Garofalo R, Monahan C, Gratzer B, & Andrews R (2013). Feasibility, acceptability, and preliminary efficacy of an online HIV prevention program for diverse young men who have sex with men: The Keep It Up! Intervention. AIDS and Behavior, 17, 2999–3012. 10.1007/s10461-013-0507-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Greene GJ, Ryan D, & Whitton SW (2015). Feasibility, acceptability, and initial efficacy of an online sexual health promotion program for LGBT youth: the Queer Sex Ed intervention. Journal of Sex Research, 52, 220–230. 10.1080/00224499.2013.867924 [DOI] [PubMed] [Google Scholar]
- Mustanski B, Lyons T, & Garcia SC (2011). Internet use and sexual health of young men who have sex with men: a mixed-methods study. Archives of Sexual Behavior, 40, 289–300. 10.1007/s10508-009-9596-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Macapagal K, Thomann M, Feinstein BA, Newcomb ME, Motley D, & Fisher CB (2017). Parents’ perspectives about adolescent boys’ involvement in biomedical HIV prevention research. Archives of Sexual Behavior. 10.1007/s10508-017-1035-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson KM, & Carey MP (2016). Media literacy is an essential component of HIV prevention for young men who have sex with men. Archives of Sexual Behavior, 45, 787–788. 10.1007/s10508-016-0712-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Clifford A, Greene GJ, & Mustanski B (2016). Parent perspectives about sexual minority adolescent participation in research and requirements of parental permission. The Journal of Adolescent Health, 59, 443–449. 10.1016/j.jadohealth.2016.05.014 [DOI] [PubMed] [Google Scholar]
- Newcomb ME, & Mustanski B (2014). Diaries for observation or intervention of health behaviors: factors that predict reactivity in a sexual diary study of men who have sex with men. Annals of Behavioral Medicine, 47, 325–334. 10.1007/s12160-013-9549-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NVivo qualitative data analysis software. (2012). (Version 10). QSR International Pty Ltd.
- Raifman J, Beyrer C, & Arrington-Sanders R (2018). HIV education and sexual risk behaviors among young men who have sex with men. LGBT Health, 5, 131–138. 10.1089/lgbt.2017.0076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasberry CN, Condron DS, Lesesne CA, Hocevar Adkins S, Sheremenko G, & Kroupa E (2018). Associations between sexual risk-related behaviors and school-based education on HIV and condom use for adolescent sexual minority males and their non-sexual-minority peers. LGBT Health, 5, 69–77. 10.1089/lgbt.2017.0111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan C, Huebner D, Diaz RM, & Sanchez J (2009). Family rejection as a predictor of negative health outcomes in White and Latino lesbian, gay, and bisexual young adults. Pediatrics, 123, 346–352. 10.1542/peds.2007-3524 [DOI] [PubMed] [Google Scholar]
- Sineath RC, Ross A, Sullivan PS, Stephenson R, Sanchez T, & Stein AD (2014). Methods for improving consent and survey completion in online HIV prevention research with young men who have sex with men. Presented at the Medicine 2.0 Conference. Retrieved from http://www.medicine20congress.com/ocs/index.php/med/med2014/article/view/2671
- Sullivan PS, Grey JA, & Simon Rosser BR (2013). Emerging technologies for HIV prevention for MSM: What we have learned, and ways forward. Journal of Acquired Immune Deficiency Syndromes, 63, S102–107. 10.1097/QAI.0b013e3182949e85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The University of California at San Diego Task Force on Decisional Capacity. (2003). Procedures for determination of decisional capacity in persons participating in research protocols. San Diego, CA: The University of California. [Google Scholar]
- University of North Dakota Center for Rural Health. (2014, August 4). RUCA 3.10. Retrieved July 7, 2017, from https://ruralhealth.und.edu/ruca
- U.S. Department of Commerce Economics and Statistics Administration. (2015). Census regions and divisions of the United States. Washington, DC: U.S. Census Bureau; Retrieved from https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf [Google Scholar]
- U.S. Department of Health and Human Services. (2009, January 15). 45 CFR 46 [Text]. Retrieved February 7, 2018, from https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/index.html
- Ybarra ML, Prescott TL, Phillips GL, Bull SS, Parsons JT, & Mustanski B (2017). Pilot RCT results of an mHealth HIV prevention program for sexual minority male adolescents. Pediatrics, 140 10.1542/peds.2016-2999 [DOI] [PMC free article] [PubMed] [Google Scholar]