Abstract
Objective.
To explore associations of joint hypermobility (a condition where range of motion is greater than normal) with ankle and foot radiographic osteoarthritis and symptoms in a large community-based cohort of African American and Caucasian adults 55–94 years old.
Methods.
Ankle and foot radiographs and joint hypermobility data (Beighton Criteria) were available for 848 participants (2003–2010) in this cross-sectional study. General joint hypermobility was defined as a Beighton score ≥4 (range 0–9); knee hypermobility was defined as hyperextension of at least one knee. Standing anteroposterior and lateral foot radiographs were read with standard atlases for Kellgren-Lawrence grade, osteophytes and joint space narrowing at the tibiotalar joint and for osteophytes and joint space narrowing to define osteoarthritis at five foot joints. Ankle or foot symptoms were self-reported. Separate person-based logistic regression models were used to estimate associations of ankle and foot osteoarthritis and symptom outcomes with hypermobility measures, adjusting for age, sex, race, body mass index, and history of ankle/foot injury.
Results.
This sample was: 68% women and 33% African American; mean age=71 years; mean body mass index=31 kg/m2; general joint hypermobility=7%, knee hypermobility=4%; ankle injury=11.5%, foot injury=3.8%. Although general joint hypermobility was not associated with ankle and foot outcomes, knee hypermobility was associated with ankle symptoms, foot symptoms, and talonavicular osteoarthritis (adjusted odds ratios of 4.4, 2.4, and 3.0, respectively).
Conclusions.
Knee joint hypermobility may be related to talonavicular osteoarthritis and to ankle and foot symptoms.
Keywords: joint hypermobility, joint pain, osteoarthritis, foot, ankle, epidemiologic study
Joint hypermobility is a condition in which the range of motion is greater than normal at most joints. The Beighton scoring system is the most commonly used measure for assessing joint hypermobility in clinical and research settings. This 9 point test assesses hypermobility of the trunk (forward bending with straight knees) and bilaterally of the first and fifth fingers, elbows, and knees (1). Typically, a cutoff point of 4 is used to define general joint hypermobility. Joint hypermobility is common in youth and is a lifelong condition, but its frequency in the population declines with older age due to the common joint stiffening that occurs with aging (2, 3). Prevalence of joint hypermobility is estimated between 2 and 57%, depending on the criteria used and the population studied (4–8). Joint hypermobility is more frequent among women than men (8), may differ by race (8, 9), and is linked to obesity (10) and joint injury (11, 12).
Key risk factors for osteoarthritis (OA), the most common form of arthritis and a leading cause of disability (13), include older age, female sex, obesity, and joint injury, which are similar risk factors to those seen in joint hypermobility. Of the lower body joints, most community-based OA studies have examined the knee and hip, and less is known about OA of the ankle and foot and their risk factors. In the first community-based cohort study of older African American and white men and women (14), we demonstrated associations of older age, obesity, prior injury, and ankle symptoms (i.e., pain, aching, and stiffness) with radiographic ankle OA, but the relationship of joint hypermobility with ankle OA or symptoms was not investigated. No prior published cohort study has examined the association of joint hypermobility with foot OA or foot or ankle symptoms.
In clinical settings, joint hypermobility appears to be associated with OA, but evidence from larger cohort studies does not readily support this observation (15–19). Among these few published cross-sectional cohort studies, associations of joint hypermobility and OA vary. For the hand, positive associations between metacarpophalangeal joint hypermobility and first carpometacarpal joint OA were reported in a population-based study of older adults in Reykjavik, Iceland (N=384) (17), while inverse associations were noted of general joint hypermobility and hand OA in a cohort of sibling pairs from the United States and United Kingdom (UK; N=1043)) and in an extended family of African American and American Indian descent (from a single founder born in the 1700s; N=280) (18). In the same extended family, general joint hypermobility was inversely associated with knee OA (15), yet a positive association was observed among 100 women 50+ years old in a clinical population in the UK (19). No apparent associations were seen between general joint hypermobility and lumbar or thoracic spine OA in a study of 716 older Caucasian women in a community study in the UK (16). This lack of agreement may be due in part to differences in joint hypermobility definitions used in these studies, but also may suggest differences in the association of hypermobility and OA outcomes by joint site, as well as differences in the samples. Potentially, joint sites that are vulnerable to the biomechanical impact of joint hypermobility, such as weight-bearing joints of the foot or ankle, might contribute to poorer joint health. A study of 112 female soccer players demonstrated that joint hypermobility was associated with greater midfoot loading attributed to medial foot collapse, a condition that is linked to joint injuries (20). Furthermore, hypermobility of the knee is associated with altered neuromuscular strategies during walking, which may affect multiple joints along the kinetic chain including the ankle and foot (21).
The purpose of this study was to explore the associations of joint hypermobility with ankle and foot OA and symptoms in a large community-based cohort. Our primary hypermobility measure was general joint hypermobility, based on the commonly used Beighton score of at least 4. We also chose to examine knee hypermobility (the ability to complete the knee maneuver on the Beighton criteria in at least one knee) for two reasons: 1) the biomechanical connection of the knee with the ankle-foot complex, as supported by the altered lower body joint moments observed with knee hypermobility (21) and the poorer ankle joint health among knees with poor joint health (22, 23); and 2) the possibility that older adults with general joint hypermobility may be less likely to achieve at least four Beighton maneuvers due to joint stiffness with aging. We hypothesized that joint hypermobility (general and knee) would be associated with foot and ankle OA and symptoms.
MATERIALS AND METHODS
Study Participants.
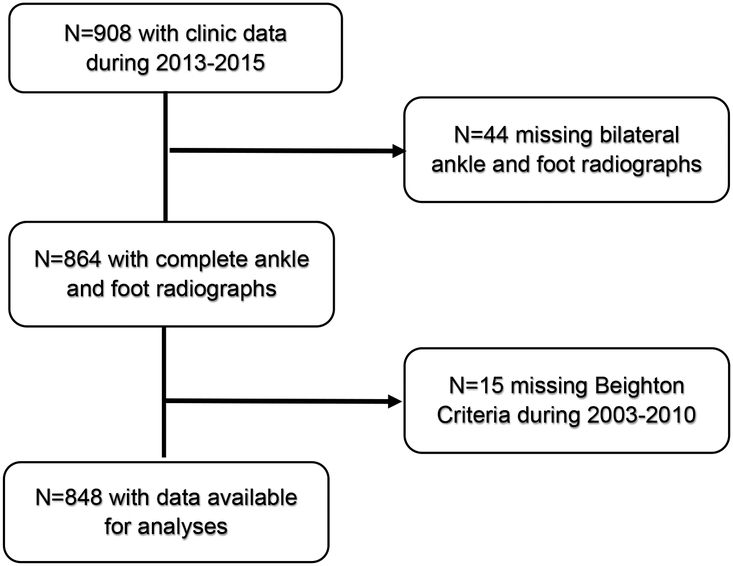
The Johnston County Osteoarthritis Project is a prospective, ongoing, community-based study of OA and OA risk factors that began in 1991 (24). Participants included in this cohort are African American and Caucasian men and women 45+ years old residing in one of six townships in Johnston County, North Carolina for at least one year. Baseline data were collected from 1991–1997 for the original cohort (N=3187) and from 1999–2003 for the enrichment cohort (N=1015), and follow-up visits of these cohorts were completed approximately every 5 years. Measurement of joint hypermobility (Beighton Criteria) was conducted during the 2003–2004 and 2006–2010 clinical exams, but not during the 2013–2015 exam. Radiographs of the feet and ankles were first collected in Johnston County Osteoarthritis Project during 2013–215. Radiographic, joint symptoms, and participant characteristics data collected during the 2013–2015 study visit for 907 individuals were used in the present analyses (Figure 1), at which time participants had aged to be at least 55 years old. For the duration of the project, the Johnston County Osteoarthritis Project has been continuously approved by the Institutional Review Boards of the University of North Carolina at Chapel Hill and the Centers for Disease Control and Prevention.
Figure 1.
Johnston County Osteoarthritis Project participants available for analyses.
Joint Hypermobility.
The Beighton scoring system for hypermobility was used during the 2003–2004 and 2006–2010 clinical exams in the Johnston County Osteoarthritis Project. The Beighton criteria have demonstrated high intra-rater and inter-rater reliability (Spearman r = 0.81–0.86 and 0.75–0.87, respectively) among women 15–45 years old (25) and a high intra-class correlation of 0.91 among 20 patients with benign joint hypermobility syndrome or Ehlers-Danlos compared to 20 controls (26). The Beighton criteria determine the ability to complete nine maneuvers: passive dorsiflexion right/left fifth finger ≥ 90 degrees, passive apposition right/left thumbs to forearm, right/left elbow hyperextension ≥10 degrees, passive right and left knee hyperextension ≥10 degrees, and palms on floor during forward trunk flexion with knees extended (1). As described by Beighton et al, one point is assigned for each completed maneuver (total score: 0 [unable to perform any maneuver] to 9 [performed all maneuvers]). Two examiners were trained by an expert in musculoskeletal assessment to conduct each of the Beighton maneuvers; inter-rater reliability was high (κ>0.80) (27).
General joint hypermobility was defined as a Beighton score ≥4. Additionally, knee hypermobility, based on the ability to complete the knee maneuver in at least one knee, was examined specifically because of the biomechanical association of the knee with the ankle and foot.
Ankle OA.
Ankle images in the Johnston County Osteoarthritis Project included standardized mortise and lateral views in standing during 2013–2015. Using an atlas (28), radiographs were read by an expert musculoskeletal radiologist (JBR, intra-rater reliability kappa 0.91) for Kellgren-Lawrence grade (KLG), osteophyte (OST, grade 0–3), and joint space narrowing (JSN, grade 0–3) grades of the tibiotalar joints. In this atlas, the KLGs were slightly modified: 0 was selected for no radiographic findings of OA, 1 indicated “minute osteophytes of doubtful clinical significance”; 2 was selected when definite osteophytes and mild joint space narrowing were present; 3 was designated for definite osteophytes and moderate joint space narrowing; and 4 indicated both definite osteophytes and severe joint space narrowing. For the present analyses, ankle (tibiotalar joint) radiographic OA (rOA) was defined as a KLG ≥ 2 (28). Radiographic features of OA were examined separately for OST (grade ≥1 versus 0) and JSN (grade ≥1 versus 0) (29).
Foot OA.
During 2013–2015, standing anteroposterior and lateral foot x-rays were read with the LaTrobe atlas for foot rOA (30) to measure OST (0–3) and JSN (0–3) at five joint sites: first metatarsophalangeal, first cuneo-metatarsal, second cuneo-metatarsal, navicular-first cuneiform, and talonavicular. A joint with a score ≥2 OST or ≥2 JSN was considered rOA (30). According to the LaTrobe atlas, foot rOA was defined as ≥1 joint with rOA within the same foot.
Ankle and Foot Symptoms.
Presence of symptoms consistent with OA was asked separately for each ankle and foot during the 2013–2015 follow-up visit with the question: “On most days of any one month in the last 12 months did you have pain, aching or stiffness in your left/right ankle/foot?” [yes / no]. This question is supported for OA pain at other joint sites (knee and hip) (31) and considers the chronic pain experience and the fluctuations in symptom intensity over the course of a year. Symptoms were categorized as present separately for each foot and ankle based on an affirmative response to the above question. Additionally, the presence of ipsilateral symptoms and rOA were examined for both the ankle (ankle symptoms + ankle KLG≥2, along with an alternative definition of ankle symptoms + ankle OST) and foot (foot symptoms + foot rOA).
Demographic and Clinical Characteristics.
Potential confounders included self-reported sex (men/women), self-reported race (African American/Caucasian), age (in years, continuous), BMI (kg/m2, continuous, calculated from clinic measures of weight and height), and self-reported history of ankle/foot injury, which were collected during the 2013–2015 follow-up visit. History of injury was asked separately for each ankle and foot and was considered present based on an affirmative response to the question, “Have you ever injured your (right/left) (ankle/foot) badly enough that it limited your ability to walk for at least 2 days?”
Analysis.
Participants with complete radiographic and Beighton data were included in analyses (Figure 1). Chi-square statistics for categorical variables and t-tests for continuous variables were used to compare demographic and clinical characteristics (sex, race, age, BMI, injury) by hypermobility status. Separate logistic regression person-based models were used to estimate associations of hypermobility (general and knee) with each ankle (KLG, OST, JSN, symptoms, symptoms + KLG) and foot outcome (rOA, symptoms, symptoms + rOA), adjusting for covariates of sex, race, age, body mass index (BMI), and history of injury at the joint site. Pairwise interactions between hypermobility and each covariate were examined at the 0.10 significance level.
RESULTS
Study Participants.
Of the 908 participants who attended a clinic visit during 2012–2105, 864 participants had complete ankle and foot radiographs. Of those, 848 had Beighton (joint hypermobility) data collected during 2003–2010. Those able to participate in the 2012–2015 clinic visit with available Beighton data were generally similar to non-participants in this analytic sample in regard to sex, race, and BMI, but were typically younger at their baseline visit (56 versus 62 years old) and were more likely to have completed high school (85% versus 58%). Primary reasons for not participating included death, moving outside of the study area, or being physically or mentally unable to participate.
Of the 848 participants available for these analyses, 68% were women and 33% were African American with a mean age of 71.2 years (standard deviation [SD] 7.6) and mean BMI 30.9 kg/m2 (SD 6.4; Table 1). Over 11% reported a history of an ankle injury, and 3.8% reported a history of a foot injury. General joint hypermobility was present in 59 participants (7%) and was most common among those <55 years (12.1%); 4.0% of participants had knee hypermobility in at least one knee. Ankle OST was defined in 74.7% of participants while 6.6% had an ankle KLG≥2, and 7.5% had ankle JSN. Foot rOA was present among 22.3% of participants; the first metatarsophalangeal joint was the most common site for rOA (10.4%) of the five foot joint sites. Ankle and foot symptoms were present in 17.2% and 20.8% of participants, respectively. The combination of ankle symptoms + KLG≥2 was rare (2.1%); 14.2% had ankle symptoms + OST and 5.4% had foot symptoms + rOA.
Table 1.
Participants Characteristics.
| Mean (SD), range or n/N (%) | ||||
|---|---|---|---|---|
| Characteristic | Category | Total Sample N=848 |
Beighton Score ≥4 n=59 (7.0%) |
Beighton Score <4 n=789 (93.0%) |
| Age group (years) | -- | 71.2 (7.6), 55–94 | 70.2 (8.2), 56–88 | 71.3 (7.6), 55–94 |
| Body mass index (kg/m2) | -- | 30.9 (6.4), 16.1–60.2 | 29.1 (6.1), 17.8–51.1 | 31.0 (6.4), 16.1–60.2 |
| Gender | Women | 577/848 (68.0) | 48/59 (81.4) | 529/789 (67.1) |
| Race | African American | 280/848 (33.0) | 12/59 (20.3) | 268/789 (34.0) |
| History of Ankle injury | Yes | 96/838 (11.5) | 10/29 (17.0) | 87/787 (11.1) |
| History of Foot injury | Yes | 32/838 (3.8) | 17/59 (28.8) | 33/787 (4.2) |
| Joint Hypermobility | Knee Maneuver | 34/845 (4.0) | 12/29 (20.3) | 22/786 (2.8) |
| Ankle Outcomes | KLG ≥2 | 56/848 (6.6) | 2/59 (3.4) | 54/789 (74.3) |
| OST ≥1 | 632/848 (74.5) | 48/59 (81.4) | 584/789 (74.0) | |
| JSN ≥1 | 65/848 (7.7) | 2/59 (3.4) | 63/789 (8.0) | |
| Ankle Symptoms | 146/848 (17.2) | 14/59 (23.7) | 132/789 (16.7) | |
| Ankle Symptoms + KLG ≥2 | 18/848 (2.1) | 1/59 (1.7) | 17/789 (2.2) | |
| Ankle Symptoms + OST | 119/848 (14.2) | 12/59 (20.3) | 107/789 (13.6) | |
| Foot Outcomes | Foot rOA | 189/848 (22.3) | 12/59 (20.3) | 177/789 (22.4) |
| 1st metatarsophalangeal rOA | 88/848 (10.4) | 7/59 (11.9) | 81/789 (10.3) | |
| 1st cuneo-metatarsal rOA | 21/848 (2.5) | 0/59 (0.0) | 21/789 (2.7) | |
| 2nd cuneo-metatarsal rOA | 59/848 (7.0) | 5/59 (8.5) | 54/789 (6.8) | |
| Navicular-1st cuneiform rOA | 41/848 (4.8) | 4/59 (6.8) | 37/789 (4.7) | |
| Talonavicular rOA | 49/848 (5.8) | 4/59 (6.8) | 45/789 (5.7) | |
| Foot symptoms | 176/848 (20.8) | 17/59 (28.8) | 159/789 (20.2) | |
| Foot symptoms + Foot rOA | 46/848 (5.4) | 4/59 (6.8) | 42/789 (5.3) | |
KLG = Kellgren Lawrence grade; OST=osteophytes; JSN=joint space narrowing; rOA = radiographic osteoarthritis; SD=standard deviation
General Joint Hypermobility.
Overall, associations of general joint hypermobility and ankle and foot outcomes were not statistically significant (Table 2). No association was observed for foot rOA with general joint hypermobility (adjusted odds ratio [aOR] 1.08, 95% confidence interval [CI] 0.55, 2.12), There were no statistically significant interactions for general joint hypermobility with any covariate.
Table 2.
Adjusted* odds ratios (OR) and 95% confidence intervals (CI) for ankle and foot outcomes with hypermobility measures.
| Outcome | Beighton Score ≥4 n=59 |
Beighton Score <4 n=789 |
Adjusted OR (95% CI) |
Knee Maneuver n=34 |
No Knee Maneuver n=811 |
Adjusted OR (95% CI) |
|---|---|---|---|---|---|---|
| Ankle KLG§ ≥2, n (%) | 2 (3.4) | 554 (6.8) | 0.55 (0.13, 2.39) | 3 (8.8) | 53 (6.5) | 1.45 (0.42, 5.13) |
| Ankle OST§ ≥1, n (%) | 48 (81.4) | 584 (74.0) | 1.87 (0.92, 3.80) | 27 (79.4) | 602 (74.2) | 1.50 (0.62 3.66) |
| Ankle JSN§ ≥1, n (%) | 2 (3.4) | 63 (8.0) | 0.47 (0.11, 2.03) | 3 (8.8) | 61 (7.5) | 1.32 (0.38, 4.56) |
| Ankle symptoms, n (%) | 14 (23.7) | 132 (16.7) | 1.55 (0.80, 3.01) | 15 (44.1) | 131 (16.2) | 4.41 (2.06, 9.44) |
| Ankle symptoms + KLG ≥2, n (%) | 1 (1.70) | 17 (2.15) | 0.87 (0.11, 6.97) | 3 (8.8) | 15 (1.9) | 5.34 (1.37, 20.79) |
| Ankle symptoms + OST, n (%) | 12 (20.3) | 107 (13.6) | 1.67 (0.81, 3.42) | 13 (38.2) | 106 (13.1) | 4.65 (2.07, 10.45) |
| Foot rOA§, n (%) | 12 (20.3) | 177 (22.4) | 1.08 (0.55, 2.12) | 7 (20.6) | 181 (22.3) | 0.91 (0.38, 2.15) |
| 1st metatarsophalangeal rOA, n (%) | 7 (11.9) | 81(10.3) | 1.36 (0.59, 3.14) | 3 (8.8) | 85 (10.5) | 0.82 (0.25, 2.77) |
| 1st cuneo-metatarsal rOA, n (%) | 0 (0) | 21 (2.7) | † | 0 (0) | 21 (2.6) | † |
| 2nd cuneo-metatarsal rOA, n (%) | 5 (8.5) | 54 (6.8) | 1.55 (0.57, 4.22) | 3 (8.8) | 56 (6.9) | 1.32 (0.38, 4.65) |
| Navicular-1st cuneiform rOA, n (%) | 4 (6.8) | 37 (4.7) | 2.16 (0.70, 6.67) | 2 (5.9) | 39 (4.8) | 1.23 (0.27, 5.59) |
| Talonavicular rOA, n (%) | 4 (6.8) | 45 (5.7) | 1.65 (0.55, 4.95) | 5 (14.7) | 43 (5.3) | 3.05 (1.10, 8.51) |
| Foot symptoms, n (%) | 17 (28.8) | 159 (20.2) | 1.54 (0.84, 2.83) | 12 (35.3) | 163 (20.1) | 2.40 (1.15, 5.04) |
| Foot symptoms + Foot rOA, n (%) | 4 (6.8) | 42 (5.3) | 1.43 (0.48, 4.28) | 3 (8.8) | 42 (5.2) | 2.04 (0.56, 7.21) |
Adjusted for age, gender, race, ankle injury and body mass index
KLG = Kellgren Lawrence grade; OST=osteophytes; JSN=joint space narrowing; rOA = radiographic osteoarthritis
No participants with hypermobility (Beighton ≥4 or able to complete knee maneuver) had 1st cuneo-metatarsal rOA.
Knee Hypermobility.
The adjusted odds of ankle symptoms, ankle symptoms + KLG≥2, and ankle symptoms + OST were statistically significantly increased (aORs 4.41–5.34) in association with knee hypermobility (Table 2). Compared to those without knee hypermobility, the adjusted odds of talonavicular rOA and of foot symptoms indicated statistically significantly increased (aORs 3.0 and 2.4, respectively) associations with knee hypermobility. No associations were noted for foot rOA nor first metatarsophalangeal rOA with knee hypermobility. No statistically significant interactions for knee hypermobility with sex, race, age, BMI, or injury were observed.
DISCUSSION
The results of this cross-sectional study demonstrated that the relationships of joint hypermobility with OA and symptoms outcomes at the ankle and foot vary by joint site. Notably, ankle symptoms, ankle symptoms + ankle rOA, foot symptoms, and talonavicular rOA were strongly associated with knee hypermobility. The foot rOA definition that considered rOA at five joint sites of the foot was not associated with general joint hypermobility nor knee hypermobility based on the Beighton criteria. Associations of general joint hypermobility and ankle outcomes were not statistically significant.
Although general joint hypermobility has been considered a risk factor for increased musculoskeletal pain (2), we did not find any objective evidence for an association between general joint hypermobility and ankle or foot symptoms. This differs from findings for a large cohort of 2,901 adolescents, which reported an 82% higher odds of ankle/foot pain among individuals with general joint hypermobility vs. those without hypermobility (10), but was consistent with our results of an association of knee hypermobility and ankle and foot symptoms. This is interesting considering that a hypermobile joint may have altered biomechanics, and this joint, along with other joints in the kinetic chain, may become overloaded during repetitive motions occurring with daily or occupational activities (5). The joints may thus experience microtrauma resulting in increased joint pain (5). With knee hypermobility specifically, the reduced stability of the knee may contribute to malalignment of the knee, along with other lower body joints, altering knee joint loads and contributing to joint pain. In fact, both radiographic knee OA and knee malalignment have been associated with bone scintigraphic abnormalities of the contralateral ankle (associated with ankle joint symptoms) and forefoot (22). These data, taken together with our findings, suggest that therapeutic interventions targeting mechanical factors, particularly for knee hypermobility, may be needed to prevent ankle and forefoot symptoms.
For rOA, the only significant result was an association of knee hypermobility with the talonavicular joint. Our results suggested a possible link of joint hypermobility with a radiographic ankle outcome that relied on the presence of osteophytes (i.e., ankle OST). Similar results were not seen for radiographic outcomes related to cartilage degeneration (e.g., JSN), but these analyses were limited considerably by small sample sizes. Additional investigations are needed to clarify whether joint hypermobility has a varying relationship with different joint tissue processes at the ankle. Local foot or ankle hypermobility is not assessed as part of the Beighton Criteria, and associations of joint hypermobility and rOA in our analyses may differ if validated measures for hypermobility of the foot and ankle were a part of the assessment of general joint hypermobility. Joint hypermobility of the first ray, which includes the first metatarsophalangeal, cuneo-metatarsal, and interphalangeal joints, has been considered by clinicians to be associated with hallux valgus, although there is debate as to whether hypermobility is the cause or the result of the deformity (32). The first ray has been clinically considered as hypermobile when it translates 1 cm or more superiorly and inferiorly with respect to the 2nd ray, and this type of hypermobility has been qualitatively described and suggested to be related to hallux valgus and hallux rigidus, two conditions seen with first metatarsophalangeal joint OA (33, 34).
Strengths of the present study include the use of a large community-based sample, inclusion of African American and Caucasian men and women participants 45 years of age and older, and use of detailed data for these analyses (e.g., Beighton criteria, foot and ankle radiography, foot and ankle symptoms). To our knowledge, this is the first large cohort study to explore associations of joint hypermobility with ankle and foot osteoarthritis and symptoms.
An important limitation of this study is that there were small numbers for some analyses due to low frequency of hypermobility and certain outcomes; thus, results should be considered preliminary rather than definitive. Additionally, the analyses were not conducted over time, and thus, we were unable to determine how joint hypermobility may contribute to progression of ankle and foot symptoms and radiographic features of OA. Individuals in this cohort who were hypermobile in their youth may have experienced stiffening in the joints that typically is seen with aging. At the time of this study, our participants were over the age of 45 years when we assessed their joint hypermobility status with the Beighton criteria; therefore, participants who at one time had general joint hypermobility (Beighton Criteria ≥4) now may be classified as not having this condition. The occurrence of joint hypermobility was 7% in this study, which is within the range of frequencies reported in other large cohorts of adults in this age group (15–18) but less than what is observed in younger populations (up to 57%) (5, 35–37). It is important to note that the hypermobility measures (2002–2010) were collected several years before the ankle and foot radiographs were acquired (2013–2015), and the presence of joint hypermobility may have been less frequent at the time of outcome assessment. Also, participants included in these analyses likely were not fully representative of the overall Johnston County Osteoarthritis Project cohort because they were more likely to be younger and to have completed more years of school than those who did not participate, although sex, race, and BMI were comparable for participants and non-participants.
In summary, joint hypermobility may be linked to ankle and foot symptoms and talonavicular rOA. These findings should be further examined in other populations and in longitudinal analyses, particularly studies that may include data on joint hypermobility during younger ages, to determine the contribution of joint hypermobility over time to the incidence and progression of ankle and foot OA outcomes.
SIGNIFICANCE AND INNOVATIONS.
Reports of associations of joint hypermobility and osteoarthritis (OA) vary widely, potentially because hypermobility may affect each joint site differently.
This is the first large cohort study to examine the relationship of joint hypermobility with OA and symptoms at the foot or ankle.
In a large cohort of adults 45+ years old, the associations of joint hypermobility and radiographic OA and symptom outcomes appear to differ by specific ankle and foot joints, even when considering age, race, sex, obesity, and injury.
Acknowledgments
We would like to thank the participants and staff of Johnston County Osteoarthritis Project for their commitment to this research project.
Funding: National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) R01AR067743 (Golightly, Hannan, Cleveland, Nelson, Schwartz, Renner, Jordan), NIH/NIAMS P60AR064166 (Jordan, Golightly, Nelson, Cleveland, Schwartz), Centers for Disease and Prevention Control (CDC) / Association of Schools of Public Health S043, S3486 (Jordan, Renner), CDC U01DP003206 ((Jordan, Golightly, Nelson, Cleveland, Schwartz), NIH/NIAMS R01AR047853 Framingham Foot Study (Hannan, Hillstrom, Jordan); NIH K23 AR061406 (Nelson), P30-AG-028716 (Kraus)
Abbreviations.
- OA
osteoarthritis
- KLG
Kellgren Lawrence Grade
- OST
osteophytes
- JSN
joint space narrowing
- rOA
radiographic OA
- BMI
body mass index
- SD
standard deviation
- aOR
adjusted odds ratio
- CI
confidence interval
Footnotes
Competing Interests: The authors report no conflicts of interest in relation to this work.
REFERENCES
- 1.Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis 1973;32(5):413–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wolf JM, Cameron KL, Owens BD. Impact of joint laxity and hypermobility on the musculoskeletal system. J Am Acad Orthop Surg 2011;19(8):463–71. [DOI] [PubMed] [Google Scholar]
- 3.van der Giessen LJ, Liekens D, Rutgers KJ, Hartman A, Mulder PG, Oranje AP. Validation of beighton score and prevalence of connective tissue signs in 773 Dutch children. J Rheumatol. 2001;28(12):2726–30. [PubMed] [Google Scholar]
- 4.Grahame R Joint hypermobility and genetic collagen disorders: are they related? Arch Dis Child. 1999;80(2):188–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hakim A, Grahame R. Joint hypermobility. Best Pract Res Clin Rheumatol. 2003;17(6):989–1004. [DOI] [PubMed] [Google Scholar]
- 6.Jessee EF, Owen DS Jr, Sagar KB. The benign hypermobile joint syndrome. Arthritis Rheum. 1980;23(9):1053–6. [DOI] [PubMed] [Google Scholar]
- 7.Klemp P, Williams SM, Stansfield SA. Articular mobility in Maori and European New Zealanders. Rheumatology (Oxford). 2002;41(5):554–7. [DOI] [PubMed] [Google Scholar]
- 8.Remvig L, Jensen DV, Ward RC. Epidemiology of general joint hypermobility and basis for the proposed criteria for benign joint hypermobility syndrome: review of the literature. J Rheumatol. 2007;34(4):804–9. [PubMed] [Google Scholar]
- 9.Wordsworth P, Ogilvie D, Smith R, Sykes B. Joint mobility with particular reference to racial variation and inherited connective tissue disorders. Br J Rheumatol. 1987;26(1):9–12. [DOI] [PubMed] [Google Scholar]
- 10.Tobias JH, Deere K, Palmer S, Clark EM, Clinch J. Joint hypermobility is a risk factor for musculoskeletal pain during adolescence: findings of a prospective cohort study. Arthritis Rheum. 2013;65(4):1107–15. [DOI] [PubMed] [Google Scholar]
- 11.Ramesh R, Von Arx O, Azzopardi T, Schranz PJ. The risk of anterior cruciate ligament rupture with generalised joint laxity. J Bone Joint Surg Br 2005;87(6):800–3. [DOI] [PubMed] [Google Scholar]
- 12.Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med 2003;31(6):831–42. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC). Prevalence and most common causes of disability among adults - United States, 2005. Morb Mortal Wkly Rep 2009;58:421–6. [PubMed] [Google Scholar]
- 14.Lateef S, Golightly YM, Renner JB, Jordan JM, Nelson AE. A cross-sectional analysis of radiographic ankle osteoarthritis frequency and associated factors: The Johnston County Osteoarthritis Project. J Rheumatol. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen HC, Shah SH, Li YJ, Stabler TV, Jordan JM, Kraus VB. Inverse association of general joint hypermobility with hand and knee osteoarthritis and serum oligomeric matrix protein levels. Arthritis Rheum. 2008;58(12):3854–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dolan AL, Hart DJ, Doyle DV, Grahame R, Spector TD. The relationship of joint hypermobility, bone mineral density, and osteoarthritis in the general population: the Chingford Study. J Rheumatol. 2003;30(4):799–803. [PubMed] [Google Scholar]
- 17.Jónsson H, Elíasson GJ, Jónsson A, Eiríksdóttir G, Sigurdsson S, Aspelund T, et al. High hand joint mobility is associated with radiological CMC1 osteoarthritis: the AGES-Reykjavik study. Osteoarthritis Cartilage. 2009;17(5):592–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kraus VB, Li YJ, Martin ER, Jordan JM, Renner JB, Doherty M, et al. Articular hypermobility is a protective factor for hand osteoarthritis. Arthritis Rheum. 2004;50(7):2178–83. [DOI] [PubMed] [Google Scholar]
- 19.Scott D, Bird H, Wright V. Joint laxity leading to osteoarthrosis. Rheumatol Rehabil. 1979;18(3):167–9. [DOI] [PubMed] [Google Scholar]
- 20.Foss KD, Ford KR, Myer GD, Hewett TE. Generalized joint laxity associated with increased medial foot loading in female athletes. J Athl Train. 2009;44(4):356–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Simonsen EB, Tegner H, Alkjaer T, Larsen PK, Kristensen JH, Jensen BR, et al. Gait analysis of adults with generalised joint hypermobility. Clin Biomech (Bristol, Avon). 2012;27(6):573–7. [DOI] [PubMed] [Google Scholar]
- 22.Kraus VB, Worrell TW, Renner JB, Coleman RE, Pieper CF. High prevalence of contralateral ankle abnormalities in association with knee osteoarthritis and malalignment. Osteoarthritis Cartilage. 2013;21(11):1693–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muehleman C, Margulis A, Bae WC, Masuda K. Relationship between knee and ankle degeneration in a population of organ donors. BMC Med 2010;8:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;34(1):172–80. [PubMed] [Google Scholar]
- 25.Boyle KL, Witt P, Riegger-Krugh C. Intrarater and interrater reliability of the Beighton and Horan Joint Mobility Index. J Athl Train. 2003;38(4):281–5. [PMC free article] [PubMed] [Google Scholar]
- 26.Juul-Kristensen B, Røgind H, Jensen DV, Remvig L. Inter-examiner reproducibility of tests and criteria for generalized joint hypermobility and benign joint hypermobility syndrome. Rheumatology (Oxford) 2007;46(12):1835–41. [DOI] [PubMed] [Google Scholar]
- 27.Flowers PPE, Cleveland RJ, Schwartz TA, Nelson AE, Kraus VB, Hillstrom HJ, et al. Association between general joint hypermobility and knee, hip, and lumbar spine osteoarthritis by race: a cross-sectional study. Arthritis Res Ther 2018;20(1):76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kraus VB, Kilfoil TM, Hash TW 2nd, McDaniel G, Renner JB, Carrino JA, et al. Atlas of radiographic features of osteoarthritis of the ankle and hindfoot. Osteoarthritis Cartilage. 2015;23(12):2059–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burnett SJ, Hart DJ, Spector TD. A radiographic atlas of osteoarthritis. London: Springer-Verlag; 1994. [Google Scholar]
- 30.Menz HB, Munteanu SE, Landorf KB, Zammit GV, Cicuttini FM. Radiographic classification of osteoarthritis in commonly affected joints of the foot. Osteoarthritis Cartilage. 2007;15(11):1333–8. [DOI] [PubMed] [Google Scholar]
- 31.Leyland KM, Gates LS, Nevitt M, Felson D, Bierma-Zeinstra SM, Conaghan PG, et al. Harmonising measures of knee and hip osteoarthritis in population-based cohort studies: an international study. Osteoarthritis Cartilage. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Doty JF, Coughlin MJ. Hallux valgus and hypermobility of the first ray: facts and fiction. Int Orthop. 2013;37(9):1655–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Menz HB, Roddy E, Marshall M, Thomas MJ, Rathod T, Myers H, et al. Demographic and clinical factors associated with radiographic severity of first metatarsophalangeal joint osteoarthritis: cross-sectional findings from the Clinical Assessment Study of the Foot. Osteoarthritis Cartilage. 2015;23(1):77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Galli MM, Hyer CF. Hallux rigidus: what lies beyond fusion, resectional arthroplasty, and implants. Clin Podiatr Med Surg 2011;28(2):385–403, ix. [DOI] [PubMed] [Google Scholar]
- 35.Decoster LC, Bernier JN, Lindsay RH, Vailas JC. Generalized joint hypermobility and its relationship to injury patterns among NCAA lacrosse players. J Athl Train. 1999;34(2):99–105. [PMC free article] [PubMed] [Google Scholar]
- 36.Decoster LC, Vailas JC, Lindsay RH, Williams GR. Prevalence and features of joint hypermobility among adolescent athletes. Arch Pediatr Adolesc Med 1997;151(10):989–92. [DOI] [PubMed] [Google Scholar]
- 37.Jansson A, Saartok T, Werner S, Renstrom P. General joint laxity in 1845 Swedish school children of different ages: age- and gender-specific distributions. Acta Paediatr. 2004;93(9):1202–6. [DOI] [PubMed] [Google Scholar]