Abstract
Purpose
Vesicle-associated membrane protein 8 (VAMP8) is a soluble N-ethylmaleimide-sensitive factor receptor protein that participates in autophagy by directly regulating autophagosome membrane fusion and has been reported to be involved in tumor progression. Nevertheless, the expression and prognostic value of VAMP8 in breast cancer (BC) remain unknown. This study aimed to evaluate the clinical significance and biological function of VAMP8 in BC.
Methods
A total of 112 BC samples and 30 normal mammary gland samples were collected. The expression of VAMP8 was assessed in both BC tissues and normal mammary gland tissues via a two-step immunohistochemical detection method.
Results
The expression of VAMP8 in BC tissues was significantly higher than that in normal breast tissues. Furthermore, increased VAMP8 expression was significantly correlated with tumor size (p=0.007), lymph node metastasis (p=0.024) and recurrence (p=0.001). Patients with high VAMP8 expression had significantly lower cumulative recurrence-free survival and overall survival (p<0.001 for both) than patients with low VAMP8 expression. In multivariate logistic regression and Cox regression analyses, lymph node metastasis and VAMP8 expression were independent prognostic factors for BC.
Conclusion
VAMP8 is significantly upregulated in human BC tissues and can thus be a practical and potentially effective surrogate marker for survival in BC patients.
Keywords: Autophagy, Breast neoplasms, Prognosis, Recurrence, VAMP8 protein
INTRODUCTION
Breast cancer (BC) is the leading cause of cancer mortality in women with an incidence of 660,000 new cases per year in China. Moreover, the number of BC deaths and cases has substantially increased in the past few years. Despite advancements in prevention, diagnosis, surgical techniques, and adjuvant therapy, the overall prognosis and survival of patients with BC have not satisfactorily improved [1]. Currently, Tumor-Node-Metastasis stage, molecular type, histological grade, pathological type, and lymph node metastasis are prominent prognostic risk factors in patients with BC [2]. However, these factors alone cannot explain differences in patient prognosis. Therefore, additional novel markers that are involved in patient prognosis need to be identified.
The soluble N-ethylmaleimide-sensitive factor activating protein receptor (SNARE) family is a superfamily of small proteins containing more than 35 members in mammals, with varying sizes and complex structures [3]. Being essential components for cellular activities, SNARE proteins are involved in the progression of various tumors [4,5]. Vesicle-associated membrane protein 8 (VAMP8) was first identified as an endosomal SNARE that participates in diverse biological functions including endosomal fusion, exocytosis of glucose transporter type 4 and insulin, regulation of exocytosis in secretory cells, sequential granule-to-granule fusion, and autophagy. Additionally, autophagy has been previously reported to partially participate in tumorigenesis and progression. Autophagy may exert distinct effects on different tumor cell types and during different stages of tumor progression even within the same tumor. Although studies on autophagy in BC patients have led to encouraging results, the potential role of autophagy regulation in BC progression remains unclear. Until now, the majority of studies have demonstrated that anticancer strategies mediate autophagy in patients with BC [6]. In addition, the level of VAMP8 has been shown to regulate malignant transformation [7]. Therefore, whether VAMP8, the main factor in autophagy regulation, is involved in BC progression needs to be urgently investigated.
In this study, we statistically evaluated the correlation of VAMP8 expression and pathological features with clinical prognosis in BC patients to determine its use as a prognostic factor in BC patients.
METHODS
Patients
Between January 2008 and December 2009, all BC patients treated with modified radical mastectomy at the Division of Breast Surgery, affiliated with China Medical University were considered for this retrospective study, excluding patients who were lost to follow-up or had died. Patients who had undergone other surgical procedures were also excluded. A total of 112 eligible patients were finally included in the study. In addition, breast tissue samples from 30 non-cancer patients were obtained as controls. All patients were female, with a median age of 52 years (range, 29–82 years), without prior chemotherapy, radiation therapy, or other related treatment. None of the patients had tumors in any other organ. Follow-up occurred for at least 8 years or until patient death. This study was approved by the First Affiliated Hospital Ethics committee of China Medical University (IRB approval number: AF-SOP-07-1.1-01), following the current regulations of the Chinese government as well as the Declaration of Helsinki. Informed consent was provided from the patients.
Immunohistochemistry
Rabbit anti-human VAMP8 polyclonal antibody (1:300) was purchased from Abcam (Cambridge, UK), and the Ultrasensitive™ S-P Kit (strept avidin-biotin complex) was purchased from Zhongshan Jinqiao Biotechnology Co. (Beijing, China). Dewaxing was performed using conventional methods, and ethylenediaminetetraacetic acid was used to carry out antigen retrieval. All procedures were carried out according to the specifications of the kit. Each section was randomly examined in five high-magnification fields (×200) to calculate a VAMP8 expression score, which took into account both staining intensity and percentage of positive cells. The staining intensity was given one of the following four scores: no color was scored as 0, pale brown as 1, claybank as 2, and deep brown as 3. The percentage of positive cells was also scored, as follows: <5% positive cells was scored as 0, 5%–25% as 1, 26%–50% as 2, 51%–75% as 3, and >75% as 4. The total expression score was calculated by multiplying the staining intensity and percentage of positive cells scores. Cases without VAMP8 expression (−) had a score of 0 or 1, while cases with VAMP8 expression (+) had a score of ≥2 [7]. Based on the scores, patients were classified into the following two groups: low VAMP8 expression (<4) and high VAMP8 expression (>4). Each slide was independently examined and scored by two pathologists in a blinded fashion.
Statistical analysis
Data analysis and graph plotting were performed with SPSS version 17.0 (SPSS Inc., Chicago, USA). Categorical variables were expressed as absolute and relative frequencies and compared by the chi-square test, and descriptive variables between groups were compared using nonparametric tests. A logistic regression model was used to estimate recurrence in multivariate analyses. Survival analyses were performed using the log-rank and Cox regression methods. Two-sided tests were used in all analyses. The significance level was set at p<0.05.
RESULTS
Expression of VAMP8 in breast cancer tissues
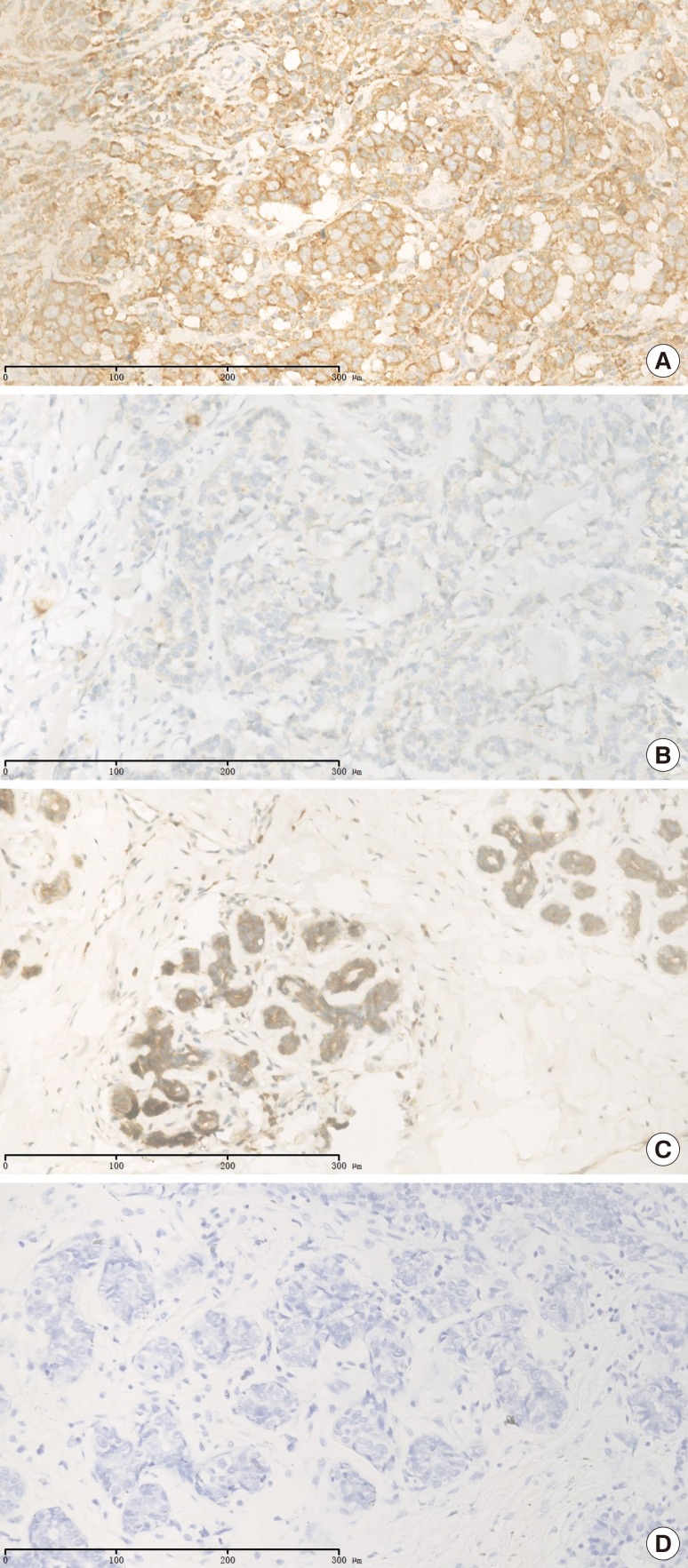
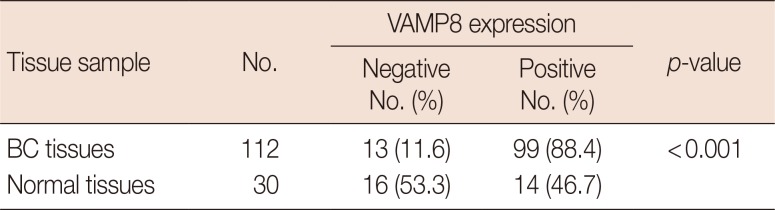
Immunohistochemical staining was used to observe the expression levels of VAMP8 in BC tissues and normal breast tissues, as well as its subcellular location. As shown in Figure 1, VAMP8 was mainly located at the cell membrane, but not in the nucleus or cytoplasm. In addition, a statistically significant difference in the expression of VAMP8 was found between BC tissues and normal tissues; 99 (88.4%) BC tissues had VAMP8 expression, while only 14 (46.7%) normal tissues showed any VAMP8 expression (p<0.001) (Table 1).
Figure 1. Immunohistochemical staining of vesicle-associated membrane protein 8 in breast cancer (BC) and normal breast tissue (×200). (A) Representative positive staining in BC. (B) Representative negative staining in BC. (C) Representative positive staining in normal breast. (D) Representative negative staining in normal breast.
Table 1. The expression levels of VAMP8 in breast cancer tissues and normal breast tissues.
VAMP8=vesicle-associated membrane protein 8; BC=breast cancer.
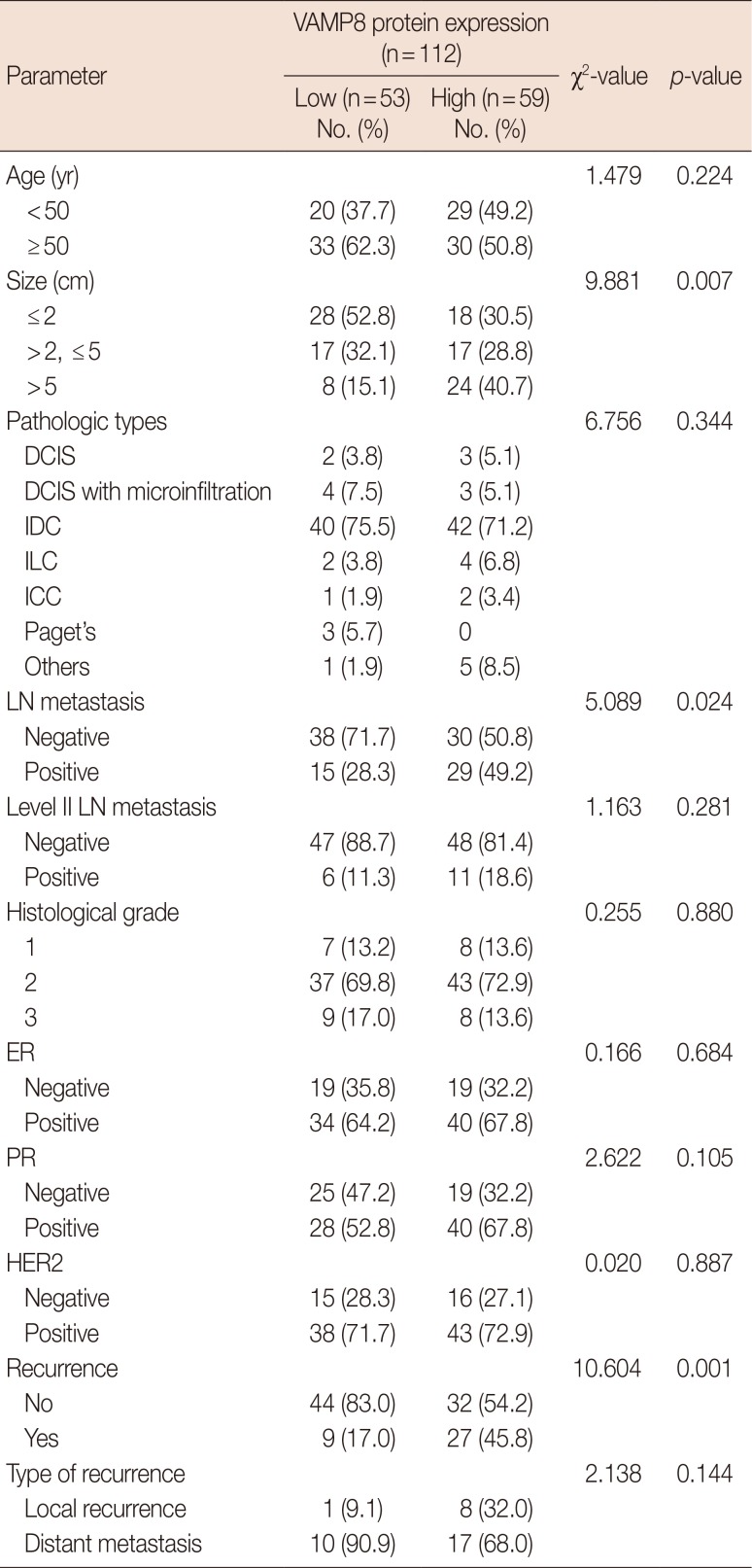
Association between the expression of VAMP8 and clinical parameters in patients with breast cancer
The associations of clinical parameters with VAMP8 expression are shown in Table 2. The expression of VAMP8 was significantly associated with tumor size (p=0.007), lymph node metastasis (p=0.024), and recurrence (p=0.001); however, there was no significant association between VAMP8 expression and age, estrogen receptor expression, progesterone receptor expression, pathological type, or histological classification.
Table 2. Association between VAMP8 expression and clinicopathological parameters.
VAMP8 =vesicle-associated membrane protein 8; DCIS=ductal carcinoma in situ; IDC=invasive ductal carcinoma; ILC=invasive lobular carcinoma; ICC=invasive cribriform carcinoma; LN=lymph node; ER=estrogen receptor; PR=progesterone receptor; HER2=human epidermal growth factor receptor 2.
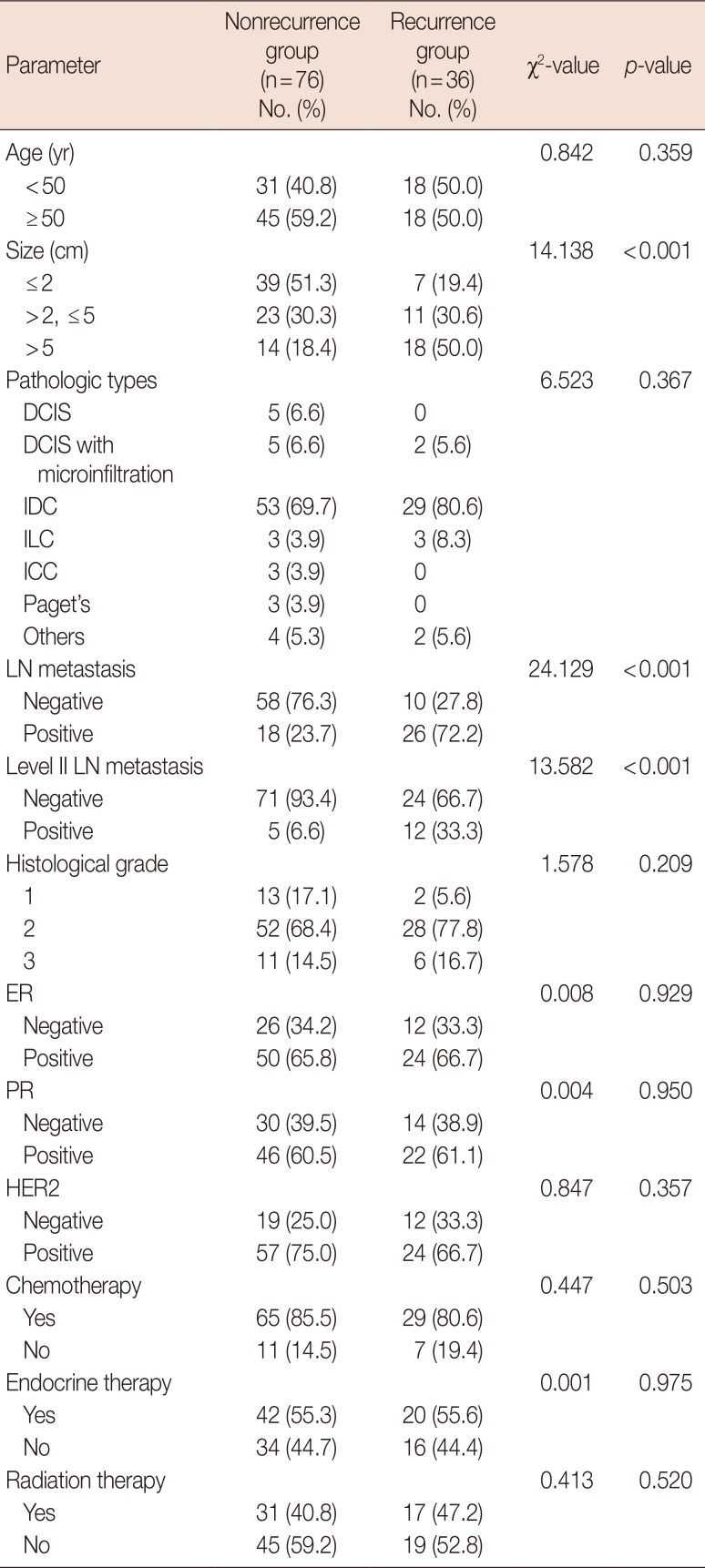
Risk factors for recurrence
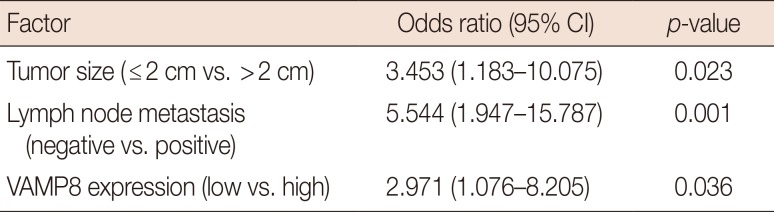
The associations of clinical parameters with BC recurrence are summarized in Table 3. Tumor size and the presence of lymph node metastasis or level II lymph node metastasis were significantly associated with BC recurrence (p<0.001, p<0.001, and p<0.001, respectively). Subsequently, to better understand of the role of VAMP8 expression in tumor recurrence, we performed logistic regression analysis on all parameters that were found to be correlated with tumor recurrence. As shown in Table 4, with regard to tumor recurrence, tumor size (≤2 cm vs. >2 cm), lymph node metastasis (negative vs. positive), and VAMP8 protein expression (low vs. high) were identified as statistically significant independent factors (p=0.023, p=0.001, and p=0.036, respectively).
Table 3. Clinicopathological parameters and two groups of the BC patients.
BC=breast cancer; DCIS=ductal carcinoma in situ; IDC=invasive ductal carcinoma; ILC=invasive lobular carcinoma; ICC=invasive cribriform carcinoma; LN=lymph node; ER=estrogen receptor; PR=progesterone receptor; HER2=human epidermal growth factor receptor 2.
Table 4. Risk factors associated with tumor recurrence in BC patients.
BC=breast cancer; CI=confidence interval; VAMP8=vesicle-associated membrane protein 8.
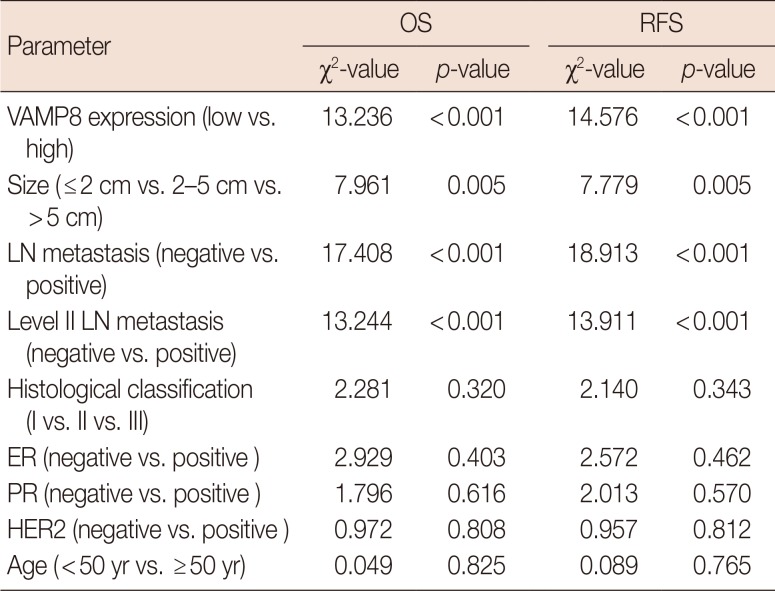
Prognostic value of VAMP8 for survival
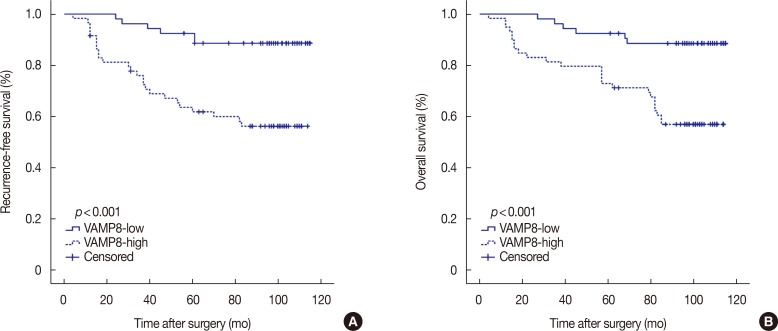
To further explore the role of VAMP8 in BC patient survival, we performed univariate Cox regression analysis after Kaplan-Meier analysis. As shown in Table 5, there were significant differences in recurrence-free survival (RFS) and overall survival (OS) between patients with high and low expression of VAMP8. Moreover, BC patients were stratified into groups based on VAMP8 expression, and differences in prognosis between the groups were examined. Higher VAMP8 expression indicated earlier tumor recurrence (p<0.001) and lower OS (p<0.001) (Figure 2). Large tumor size (>5 cm) and the presence of lymph node metastasis or level II lymph node metastasis were also associated with lower cumulative RFS and OS, consistent with the results of previous studies (Table 5).
Table 5. Prognostic performance of clinical parameters in the univariate Cox analysis.
OS=overall survival; RFS=recurrence-free survival; VAMP8=vesicle-associated membrane protein 8; LN=lymph node; ER=estrogen receptor; PR=progesterone receptor; HER2=human epidermal growth factor receptor 2.
Figure 2. Kaplan-Meier analysis by vesicle-associated membrane protein 8 (VAMP8) expression in 112 breast cancer patients. (A) Recurrence-free survival. (B) Overall survival.
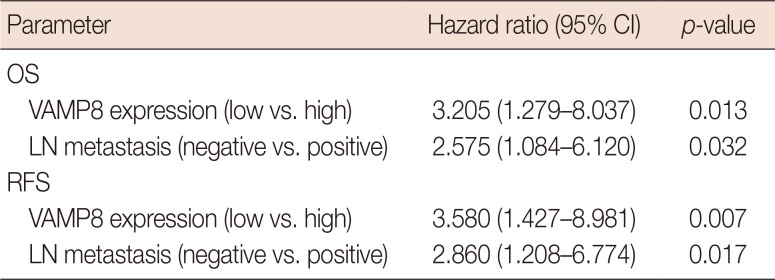
In Kaplan-Meier analysis, four clinical characteristics were considered to be potential risk factors for BC patient survival, namely, VAMP8 expression, tumor size, lymph node metastasis and level II lymph node metastasis. Hence, we subjected these parameters to multivariate Cox proportional hazard regression analysis. As summarized in Table 6, high VAMP8 expression and the presence of lymph node metastasis were significantly associated with lower OS and RFS and were thus independent adverse prognostic factors in patients with BC.
Table 6. Prognostic performance of clinical parameters in the multivariate Cox regression analysis.
CI=confidence interval; OS=overall survival; VAMP8=vesicle-associated membrane protein 8; LN=lymph node; RFS=recurrence-free survival.
DISCUSSION
BC is the second-highest cause of cancer-related mortality [8], and more than 90% of deaths in BC patients are caused by metastasis or recurrence [9,10,11]. One of the mechanisms by which BC development could be controlled is autophagy, both as a tumor-suppressive process in early stages of progression and as a protumorigenic process, critical for tumor maintenance and therapeutic resistance during later stages [12,13]. Despite the substantial advancement in our understanding of the role of autophagy in BC [6], the process remains incompletely understood and warrants further clarification. This study revealed the utility of VAMP8 expression in predicting recurrence and progression in BC patients after modified radical mastectomy, suggesting that better understanding of autophagic mechanisms may help us establish better systems for predicting prognosis in patients with BC.
Autophagy has been shown to impact recurrence and survival in multiple ways. Chemotherapy resistance is a serious problem that puzzles researchers and threatens patient survival. Autophagy can enhance chemotherapy resistance through various pathways such as heat shock factor 1/autophagy-related protein 7 [14,15] and reactive oxygen species/extracellular signal-regulated kinase (ROS/ERK) [16,17], which reduces the effect of chemotherapy and increases the recurrence rate, thereby affecting OS. Autophagy can also reduce anoikis [18], a form of cell death that results from the loss of cell contact with the extracellular matrix or neighboring cells. Cancer cells that acquire resistance to anoikis are more likely to survive after detachment from the primary tumor and disseminate throughout the body [18]. Accordingly, autophagy has been shown to increase the metastatic ability of tumor cells, thereby affecting disease prognosis [12]. One study reported that autophagy can protect tumor cells from apoptosis or necrosis by providing the cells with nutrients under conditions of cellular stress [19]. This interdependence of autophagy and apoptosis also affects prognosis [20]. Therefore, we hypothesized that VAMP8, as a member of the SNARE family, plays an important role by regulating autophagy and apoptosis in BC and is thus involved in progression.
It is well known that the fusion of autophagosomes with lysosomes is key for the degradation of autophagosomes and their contents during autophagy [21]. However, the current studies examining autophagy are all aimed at better understanding early regulatory events, and few studies have focused on the late phases of autophagy. Multiple members of the SNARE family, including VAMP7, VAMP8, and vesicle transport through interaction with t-SNAREs homolog 1B, can affect the fusion of autophagosomes with lysosomes [22]. VAMP8 has been reported to have an indispensable role in many cellular processes [23,24,25]. Chen et al. [7] found that VAMP8 could activate autophagy and was responsible for drug resistance via autophagy and that VAMP8 depletion led to a marked increase in the numbers of cell in the G0/G1 phase. It is well known that ERK2 promotes the migration of tumor cells by inhibiting the expression of ras-related protein Rab-17 (RAB17) and liprinb2, and that the tumor suppressor gene RAB17 plays a role in antitumor invasion by interacting with VAMP8 [26,27]. VAMP8 is overexpressed in BC, but the expression of VAMP8 is higher in ductal carcinoma in situ than in invasive ductal carcinoma [27]. Interestingly, we found that, higher VAMP8 expression was associated with a relatively higher recurrence risk and lower RFS and OS. Thus, VAMP8 may play a dual role in BC, but its mechanism of action remains unclear.
Here, we examined VAMP8 expression using immunohistochemistry. High expression of VAMP8 was markedly correlated with tumor size, lymph node metastasis and recurrence, which has not been previously reported. It has been reported that the expression of VAMP8 is significantly associated with increased OS and reduced risk of disease progression and that expression of VAMP8 is an independent factor for favorable pathology and survival outcomes [27]. However, in this study, we obtained conflicting results, and a previous study also found that VAMP8 expression was correlated with unfavorable prognostic indicators, reduced OS and RFS, and high rates of tumor recurrence in glioblastoma multiforme [7]. Notably, biases involving selection criteria, tissue preservation, determination of cutoff value for VAMP8 expression, racial differences, and regional differences, among others, may lead to errors in analyses; however, our results also indicate that VAMP8 might play a dual role in BC and thus warrants in-depth study.
Footnotes
This study was partly supported by a grant from the National Natural Science Foundation of China (81773163).
CONFLICT OF INTEREST: The authors declare that they have no competing interests.
References
- 1.Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 2.Dowsett M, Dunbier AK. Emerging biomarkers and new understanding of traditional markers in personalized therapy for breast cancer. Clin Cancer Res. 2008;14:8019–8026. doi: 10.1158/1078-0432.CCR-08-0974. [DOI] [PubMed] [Google Scholar]
- 3.Peng RW, Abellan E, Fussenegger M. Differential effect of exocytic SNAREs on the production of recombinant proteins in mammalian cells. Biotechnol Bioeng. 2011;108:611–620. doi: 10.1002/bit.22986. [DOI] [PubMed] [Google Scholar]
- 4.Lau SK, Boutros PC, Pintilie M, Blackhall FH, Zhu CQ, Strumpf D, et al. Three-gene prognostic classifier for early-stage non small-cell lung cancer. J Clin Oncol. 2007;25:5562–5569. doi: 10.1200/JCO.2007.12.0352. [DOI] [PubMed] [Google Scholar]
- 5.Hasan N, Hu C. Vesicle-associated membrane protein 2 mediates trafficking of alpha5beta1 integrin to the plasma membrane. Exp Cell Res. 2010;316:12–23. doi: 10.1016/j.yexcr.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Zarzynska JM. The importance of autophagy regulation in breast cancer development and treatment. Biomed Res Int. 2014;2014:710345. doi: 10.1155/2014/710345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen Y, Meng D, Wang H, Sun R, Wang D, Wang S, et al. VAMP8 facilitates cellular proliferation and temozolomide resistance in human glioma cells. Neuro Oncol. 2015;17:407–418. doi: 10.1093/neuonc/nou219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gomes LR, Terra LF, Wailemann RA, Labriola L, Sogayar MC. TGF-β1 modulates the homeostasis between MMPs and MMP inhibitors through p38 MAPK and ERK1/2 in highly invasive breast cancer cells. BMC Cancer. 2012;12:26. doi: 10.1186/1471-2407-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fang Y, Chen Y, Yu L, Zheng C, Qi Y, Li Z, et al. Inhibition of breast cancer metastases by a novel inhibitor of TGFβ receptor 1. J Natl Cancer Inst. 2013;105:47–58. doi: 10.1093/jnci/djs485. [DOI] [PubMed] [Google Scholar]
- 10.Langlands FE, Horgan K, Dodwell DD, Smith L. Breast cancer subtypes: response to radiotherapy and potential radiosensitisation. Br J Radiol. 2013;86:20120601. doi: 10.1259/bjr.20120601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 12.Fung C, Lock R, Gao S, Salas E, Debnath J. Induction of autophagy during extracellular matrix detachment promotes cell survival. Mol Biol Cell. 2008;19:797–806. doi: 10.1091/mbc.E07-10-1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martinet W, Agostinis P, Vanhoecke B, Dewaele M, De Meyer GR. Autophagy in disease: a double-edged sword with therapeutic potential. Clin Sci (Lond) 2009;116:697–712. doi: 10.1042/CS20080508. [DOI] [PubMed] [Google Scholar]
- 14.Santagata S, Hu R, Lin NU, Mendillo ML, Collins LC, Hankinson SE, et al. High levels of nuclear heat-shock factor 1 (HSF1) are associated with poor prognosis in breast cancer. Proc Natl Acad Sci U S A. 2011;108:18378–18383. doi: 10.1073/pnas.1115031108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Desai S, Liu Z, Yao J, Patel N, Chen J, Wu Y, et al. Heat shock factor 1 (HSF1) controls chemoresistance and autophagy through transcriptional regulation of autophagy-related protein 7 (ATG7) J Biol Chem. 2013;288:9165–9176. doi: 10.1074/jbc.M112.422071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin CJ, Lee CC, Shih YL, Lin TY, Wang SH, Lin YF, et al. Resveratrol enhances the therapeutic effect of temozolomide against malignant glioma in vitro and in vivo by inhibiting autophagy. Free Radic Biol Med. 2012;52:377–391. doi: 10.1016/j.freeradbiomed.2011.10.487. [DOI] [PubMed] [Google Scholar]
- 17.Cheng P, Ni Z, Dai X, Wang B, Ding W, Rae Smith A, et al. The novel BH-3 mimetic apogossypolone induces Beclin-1- and ROS-mediated autophagy in human hepatocellular carcinoma [corrected] cells. Cell Death Dis. 2013;4:e489. doi: 10.1038/cddis.2013.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim YN, Koo KH, Sung JY, Yun UJ, Kim H. Anoikis resistance: an essential prerequisite for tumor metastasis. Int J Cell Biol. 2012;2012:306879. doi: 10.1155/2012/306879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Degenhardt K, Mathew R, Beaudoin B, Bray K, Anderson D, Chen G, et al. Autophagy promotes tumor cell survival and restricts necrosis, inflammation, and tumorigenesis. Cancer Cell. 2006;10:51–64. doi: 10.1016/j.ccr.2006.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prietsch RF, Monte LG, da Silva FA, Beira FT, Del Pino FA, Campos VF, et al. Genistein induces apoptosis and autophagy in human breast MCF-7 cells by modulating the expression of proapoptotic factors and oxidative stress enzymes. Mol Cell Biochem. 2014;390:235–242. doi: 10.1007/s11010-014-1974-x. [DOI] [PubMed] [Google Scholar]
- 21.Ganley IG, Wong PM, Gammoh N, Jiang X. Distinct autophagosomal-lysosomal fusion mechanism revealed by thapsigargin-induced autophagy arrest. Mol Cell. 2011;42:731–743. doi: 10.1016/j.molcel.2011.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moreau K, Renna M, Rubinsztein DC. Connections between SNAREs and autophagy. Trends Biochem Sci. 2013;38:57–63. doi: 10.1016/j.tibs.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Zhu D, Zhang Y, Lam PP, Dolai S, Liu Y, Cai EP, et al. Dual role of VAMP8 in regulating insulin exocytosis and islet β cell growth. Cell Metab. 2012;16:238–249. doi: 10.1016/j.cmet.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 24.Zhao P, Yang L, Lopez JA, Fan J, Burchfield JG, Bai L, et al. Variations in the requirement for v-SNAREs in GLUT4 trafficking in adipocytes. J Cell Sci. 2009;122(Pt 19):3472–3480. doi: 10.1242/jcs.047449. [DOI] [PubMed] [Google Scholar]
- 25.Behrendorff N, Dolai S, Hong W, Gaisano HY, Thorn P. Vesicle-associated membrane protein 8 (VAMP8) is a SNARE (soluble N-ethylmaleimidesensitive factor attachment protein receptor) selectively required for sequential granule-to-granule fusion. J Biol Chem. 2011;286:29627–29634. doi: 10.1074/jbc.M111.265199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.von Thun A, Birtwistle M, Kalna G, Grindlay J, Strachan D, Kolch W, et al. ERK2 drives tumour cell migration in three-dimensional microenvironments by suppressing expression of Rab17 and liprin-β2. J Cell Sci. 2012;125(Pt 6):1465–1477. doi: 10.1242/jcs.092916. [DOI] [PubMed] [Google Scholar]
- 27.Diaz-Vera J, Palmer S, Hernandez-Fernaud JR, Dornier E, Mitchell LE, Macpherson I, et al. A proteomic approach to identify endosomal cargoes controlling cancer invasiveness. J Cell Sci. 2017;130:697–711. doi: 10.1242/jcs.190835. [DOI] [PMC free article] [PubMed] [Google Scholar]