Abstract
A 45-year old man, chronic smoker with a pancoast tumor due to squamous cell carcinoma has been described. The initial diagnosis of lung carcinoma was based on a scant tissue so the exact cell typing was not possible. The initial treatment consisted of platinum based chemotherapy and radiotherapy. He developed a left adrenal lesion on treatment. There was a possibility of metachronous primary. Also, a large tissue sample was required for tumor markers. The lung mass was difficult to access and was static on treatment. A left adrenal biopsy was considered to be more appropriate. A novel approach for left adrenal lesion with esophageal ultrasound using ultrasound bronchoscope (EUS-B) was successfully performed. This article is aimed at describing the use of EUS-B for transdiaphragmatic structures.
Keywords: EUS-B, Left adrenal, Transdiaphragmatic, FNAC
1. Introduction
The convex curvilinear endobronchial ultrasound (EBUS) had been developed as a procedure for sampling of the mediastinal lymph nodes required for staging the lung cancer. Subsequent to this EBUS was being used to access mediastinal masses too [1]. Recently, EBUS is being used for esophageal ultrasound also known as esophageal ultrasound with ultrasound bronchoscope (EUS-B) [1]. The dual use of the EBUS scope gives an improved diagnostic ability, and a greater safety margin as both transbronchial and transoesophgeal structures can be accessed under sedation in the same setting [1]. We have described a case where a transdiaphragmatic structure i.e. left adrenal lesion was biopsied using EUS-B.
2. Case report
A 45 year old man, welder by occupation, chronic smoker with smoking index of 17 pack years presented with backache radiating to right arm for 1 month. He had no significant past history except appendicectomy at the age of 10 years. The vital parameters were normal. The general examination revealed right-sided ptosis. There was no other general or systemic examination abnormality noted. The chest radiograph is shown in Fig. 1. The routine biochemical investigations, hematological investigations and enzyme linked immunosorbant assay for human immunodeficiency virus were normal. A computed tomography (CT) head, neck and thorax with contrast enhancement were performed. The patient was initially seen by the orthopedic surgeon, then by the neurologist and then the patient was referred to the pulmonologist. The diagnosis of pancoast tumor was made by the pulmonologist. The CT chest of the patient is given in Fig. 2 a, 2b, 2c and 2d. Endobronchial ultrasound (EBUS) using curvilinear probe guided fine needle aspiration cytology (FNAC) was performed, as the transthoracic approach was difficult owing to paratracheal location of tumor. The FNAC showed atypical cells suspicious of malignancy with CK 7 + and p40-. It was diagnosed as lung carcinoma but the typing was not possible. The surgical removal was not possible as the positron emission tomography (PET) scan showed inoperable tumor belonging to TNM stage IIIB. The performance staging was 2. So, he was started on chemotherapy with carboplatin and paclitaxel. After 2 cycles of chemotherapy, a sequential radiotherapy of 30 Gy was given. A repeat CT scan showed increase in the size of lesion from 4.5 cm to 4.9 cm. He also developed left adrenal lesion of 35 mm (Fig. 3). Another regimen was started with gemcitabine and cisplatinum. After 3 cycles, the lung lesions remained same in size but the adrenal lesion increased from 35 mm to 37 mm. So, a repeat biopsy for immunohistochemistry and genetic typing was required. Since the lung lesions had remained same in size, earlier result did not yield good tissue and adrenal metastasis versus metachronous primary was a dilemma, a left adrenal biopsy was performed with EUS-B (Fig. 4, video). The biopsy confirmed squamous cell carcinoma with Napsin-, CK +, p63 + and had PDL1 -5%, EGFR-wild type. There were no post-procedure complications. The therapy was switched over to Pembrolizumab.
Fig. 1.
Chest radiograph (PA) view showing a lesion in right apical region.
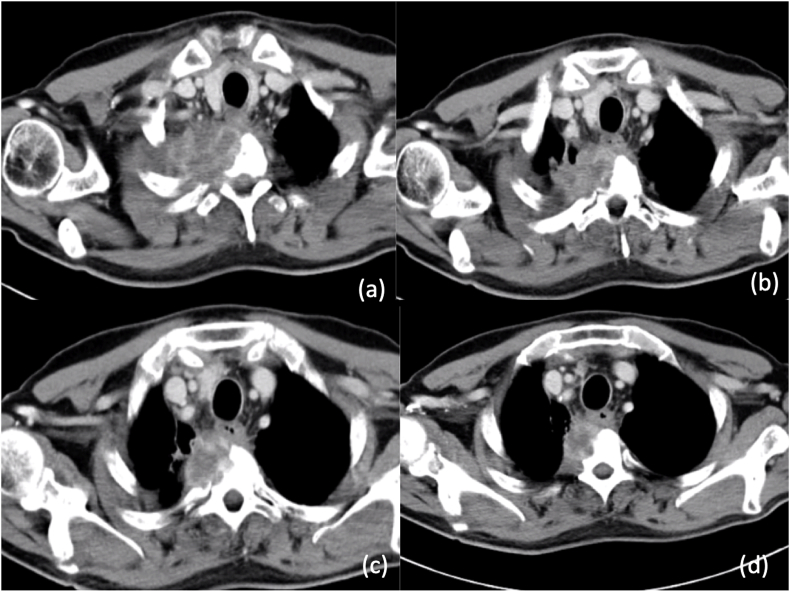
Fig. 2.
a, 2b: The computed tomography (CT) of chest at the time of presentation showing a mass in the right apex. of 55 mm with invasion 11 mm invasion of D2.
Fig. 3.
The CT abdomen on chemotherapy showing left adrenal metastasis.
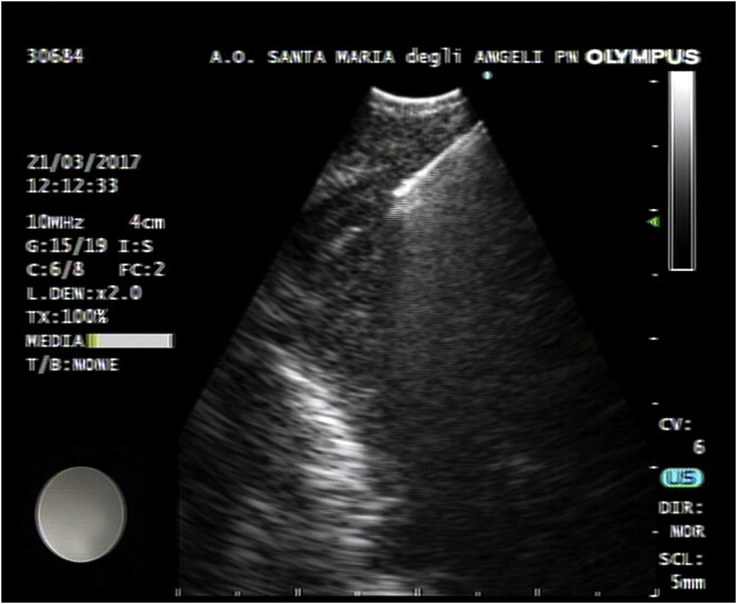
Fig. 4.
The endosonographic image of esophageal ultrasound with ultrasound bronchoscope (EUS-B) guided left adrenal biopsy.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.rmcr.2018.12.012.
The following is the supplementary data related to this article:
The video shows liver followed by aorta followed by metastasis of left adrenal. The biopsy needle is seen inserted into the lesion.
3. Discussion
EUS-B was first described in 2009. EUS-B-FNAC broadens the diagnostic yield of EBUS. Studies have described the usefulness of EUS-B-FNAC in lung cancer staging required for mediastinal nodes sampling [[1], [2], [3], [4], [5]]. A study by Herth et al., performed endoscopic staging with EBUS- transbronchial needle aspiration (TBNA) first and then the same scope was utilized for performing EUS-B-FNAC. Sensitivity for EUS-B-FNAC was 89% and that of EBUS-TBNA was 92%. The combined use of the scope could improve the sensitivity to 96% and negative predictive value to 95% in presence of mediastinal lymphnodes [6]. Thus, whenever an EBUS is performed for lung cancer EUS-B performed simultaneously, improves the yield of mediastinal lymphnodes. EUS-B has also been recently described for transdiaphragmatic structures. The use of EUS-B for the transdiaphragmatic structure widens the scope of EUS-B further as seen in our case.
The use of EUS-B for left adrenal was first described by Meena N et al., in 2015 [1]. The adrenal glands represent the fourth most common site of metastasis for lung cancer [7]. Benign adrenal adenomas are also common [8]. PET scan is not very useful in differentiating benign from malignant lesion [9]. The cytology is thus important for patients with carcinoma of lung and adrenal lesions. A dedicated EUS scope for transdiaphragmatic structures has certain advantages compared to EUS-B like, the EUS scope has a broader field of view and greater depth of view. Also, it can be angulated more easily, is more rigid, and is longer [3]. But in a series the left adrenal glands of a very tall gentleman (7′6″) has also been successfully biopsied. A randomised controlled trial has shown that left adrenal gland analysis by EUS-B has a similar high success rate in comparison to conventional EUS. Also, there have been no major complications with EUS-B for left adrenal reported so far [1,5,10]. Thus, if EUS-B guided FNAC of left adrenal lesion is combined with EBUS-TBNA, it broadens the diagnostic yield further [10].
The procedure for reaching the left adrenal on EUS-B is easy for those who have a basic knowledge in ultrasound and can perform EBUS. The EBUS for EUS-B is inserted from the mouth into the oesophagus. The vision in the stomach is not as good as that of bronchus.11 One is able to orient with the anatomy by the structures outside the lumen rather than the endoscopic vision unlike the bronchoscopy. The gastroesophageal sphincter is negotiated easily. As soon as the shingtor is crossed one sees the liver. The scope is kept in the middle of the liver (video). Then it is rotated to right and then backwards till abdominal aorta is seen (video). The scope is further rotated in the same direction i.e. clockwise to reach the left adrenal. The normal adrenal is seen like a seagull [1]. If there is metastasis it shows a hypoechoic area (video).11
Apart from the left adrenal gland the transdiaphragmatic structures that can be accessed by EUS-B are coeliac nodes and liver.1,11 The coeliac nodes lie in the same field as the adrenal. Morphologically the coeliac nodes are similar to adrenal when both are involved; the approach to each is also identical. The background cellularity is however useful in identifying the tissue of origin. Coeliac nodes are important to sample because 11% of lung cancer cases have coeliac LN [1]. FNAC of the liver metastasis for cytology is also easy because EUS-B FNAC of the liver involves small needle aspiration of a magnified image on which vascular structures can be easily avoided [1].
To conclude, EUS-B for transdiaphragmatic structures is easy, safe and useful for appropriate staging and diagnosis of lung cancers.
Conflicts of interest
The authors have no conflict of interest to declare.
Footnotes
Place of study: Department of Pulmonary Medicine, Santa Maria degli Angeli di Pordenone, Italy.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2018.12.012.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Meena N., Hulett C., Jeffus S., Bartter T. Left adrenal biopsy using the convex curvilinear ultrasound scope. Respiration. 2015;89:57–61. doi: 10.1159/000368370. [DOI] [PubMed] [Google Scholar]
- 2.Hwangbo B., Lee H.S., Lee G.K., Lim K.Y., Lee S.H., Lee H.Y., Lee J.Y., Zo J.I. Transoesophageal needle aspiration using a convex probe ultrasonic bronchoscope. Respirology. 2009;6:843–849. doi: 10.1111/j.1440-1843.2009.01590.x. [DOI] [PubMed] [Google Scholar]
- 3.Szlubowski A., Zielinski M., Soja J., Filarecka A., Orzechowski S., Pankowski J., Obrochta M., Wegrzyn J., Cmiel A. Accurate and safe mediastinal restaging by combined endobronchial and endoscopic ultrasound-guided needle aspiration performed by single ultrasound bronchoscope. Eur. J. Cardio. Thorac. Surg. 2014;46:262–266. doi: 10.1093/ejcts/ezt570. [DOI] [PubMed] [Google Scholar]
- 4.Crombag L.M.M.J., Annema J.T. Left adrenal gland analysis in lung cancer patients using the endobronchial ultrasound scope: a feasibility trial. Respiration. 2016;91:235–240. doi: 10.1159/000443991. [DOI] [PubMed] [Google Scholar]
- 5.Herth F.J., Krasnik M., Kahn N., Eberhardt R., Ernst A. Combined endoscopic-endobronchial ultrasound-guided fine-needle aspiration of mediastinal lymph nodes through a single bronchoscope in 150 patients with suspected lung cancer. Chest. 2010;138:790–794. doi: 10.1378/chest.09-2149. [DOI] [PubMed] [Google Scholar]
- 6.Quint L.E., Tummala S., Brisson L.J., Francis I.R., Krupnick A.S., Kazrooni E.A. Distribution of distant metastases from newly diagnosed non-small cell lung cancer. Ann. Thorac. Surg. 1996;62:246–250. doi: 10.1016/0003-4975(96)00220-2. [DOI] [PubMed] [Google Scholar]
- 7.Meena N., Hulett C., Jeffus S., Bartter T. Exploration under the dome: esophageal ultrasound with the ultrasound bronchoscope is indispensable. Endosc. Ultrasound. 2016;5:254–257. doi: 10.4103/2303-9027.187886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boland G.W.L., Dwamena B.A., Sangwaiya M.J., Goehler A.G., Blake M.A., Hahn P.F. Characterization of adrenal masses by using FDG PET: a systematic Review and meta-analysisof diagnostic test performance. Radiology. 2011;259:117–126. doi: 10.1148/radiol.11100569. [DOI] [PubMed] [Google Scholar]
- 9.Sanz-Santos J., Serra P., Andreo F., Torky M., Centeno C., Morán T. Transbronchial and transesophageal fine needle aspiration using a single ultrasound bronchoscope in the diagnosis of locoregional recurrence of surgically-treated lung cancer. BMC Pulm. Med. 2017;17:46. doi: 10.1186/s12890-017-0388-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bugalho A., de Santis M., Szlubowski A., Rozman A., Eberhardt R. Trans-esophageal endobronchial ultrasound-guided needle aspiration (EUS-B-NA): a road map for the chest physician. Pulmonol. 2018;24:32–41. doi: 10.1016/j.rppnen.2017.10.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The video shows liver followed by aorta followed by metastasis of left adrenal. The biopsy needle is seen inserted into the lesion.