Abstract
Introduction
In the early 1990s, a comprehensive cancer control (CCC) approach was developed in the United States (US). In 2003, the US-Affiliated Pacific Islands (USAPI) adopted the CCC approach through a regional coalition, the Cancer Council of the Pacific Islands (CCPI). Using the CCC approach, the CCPI developed jurisdiction-specific cancer coalitions and initiated their respective cancer plans.
Methods
The evolution of the CCC approach and the history of the CCPI regional coalition are reviewed. The outcomes of the regional approach for cancer control in the USAPI are described to illustrate the possibilities, value-added and innovation of using a CCC strategy in a multi-national coalition based in a resource-limited environment.
Results
The CCC approach enabled the CCPI to (1) harmonize cancer control efforts between the six USAPI jurisdictions, (2) represent the USAPI cancer needs as a single voice, and (3) develop a regional cancer control strategy. Outcomes include (1) a regional cancer registry, (2) three sequential regional CCC plans, (3) leveraged resources for the USAPI, (4) enhanced on-site technical assistance and training, (5) improved standards for cancer screening, (6) evidence-based cancer control interventions adapted for the USAPI.
Conclusion
The regional CCPI coupled with the CCC approach is an effective engine of change. The CCC strategies enabled navigation of the political, geographic, cultural, and epidemiologic Pacific environment. The regional partners have been able to harmonize cancer control efforts in resource-limited settings. Regional cancer coalitions may be effective in the global arena for cancer control between communities, states, or countries.
Keywords: Pacific, CCPI, USAPI, Regionalization, Global cancer control, Comprehensive cancer control
Introduction
Comprehensive cancer control (CCC) is an “integrated and coordinated approach to reducing cancer incidence, morbidity, and mortality through prevention, early detection, treatment, rehabilitation and palliation” [1]. CCC as a strategic approach to addressing cancer issues within communities (at any level, from cities to nations) is characterized by
collaboration among diverse multi-sectoral stakeholders to reduce duplication of effort and maximize exist-ing resources
use of data to drive priority actions and use of research results to identify evidence-based interventions to implement priorities
development and implementation of a written strategic plan to guide cancer control efforts that takes into account the cultural context and healthcare delivery system of the jurisdiction.
CCC as a concept began in the US in the early 1990s. Internationally, the same concept has been described as “national cancer control planning” or national cancer control plan (NCCP) development and implementation. The Union for International Cancer Control defines an NCCP as a “sustainable strategic plan to control cancer, based on the country’s cancer burden, cancer risk factor prevalence, and the resources available to implement the plan in the context of the socio-economic environment and healthcare system in that country” [2].
CCC plans or NCCPs are typically 5-year strategic plans that cover the full continuum of cancer care, from prevention to survivorship. The plan includes broad goals, measurable objectives, and evidence-based strategies to address each area of the continuum. It is the role of the multi-sectoral group of stakeholders within the community to implement the plan. Because of the comprehensive nature of plans and the likelihood that not all the resources needed to implement the full plan are readily available, stakeholders choose specific areas of work or priorities, for plan implementation within the 5-year period of the plan life-cycle [3]. Once priority objectives are chosen, stake-holders choose relevant evidence-based strategies within the plan to implement.
Benefits of comprehensive cancer control planning
The underlying premise, and the promise, of CCC is that collaborative action among stakeholders will yield greater results in addressing the burden of cancer than individual organizations acting alone. In short, the benefits of CCC planning rest in the idea that the whole is greater than the sum of its parts [1].
Specifically, the benefits of CCC planning are [1]
development of a multi-sectoral partnership that has a shared, comprehensive perspective about how to address cancer issues, rather than a fragmented focus on only one type of cancer or cancer risk factor
reallocation of existing and identification of new resources to address cancer control gaps
increased use of evidence to guide cancer programs and policies
reduced duplication of effort and increased efficiency across cancer control organizations
speaking with one voice to increase political and social support for cancer control efforts.
Ultimately, the intended impacts of implementation of CCC plans are decreased morbidity, decreased mortality, decreased health disparities, and increased quality of life for citizens [4].
Historical context: US and international comprehensive cancer control planning efforts
The CCC movement in the US began around 1994, when several national organizations including the Centers for Disease Control and Prevention (CDC), the National Cancer Institute (NCI), the American Cancer Society (ACS), the American College of Surgeons (ACOS), the North American Association of Central Cancer Registries (NAACCR), and others came together to support states, tribes, and territories and Pacific Island Jurisdictions as they developed and implemented written CCC plans [1]. This partnership expanded over time and is now called the Comprehensive Cancer Control National Partnership (CCCNP) whose mission is to assist CCC coalitions in the US with sustained implementation of CCC plans [5]. The CCCNP conducted a series of cancer control leadership institutes, or training sessions, for leaders of state, tribe/tribal organization, territory, and USAPI jurisdiction CCC coalitions from 2000 to 2010, which led to the expansion of development of CCC plans [6].
The CDC began funding the National Comprehensive Cancer Control Program (NCCCP) in 1998 (https://www.cdc.gov/cancer/ncccp/about.htm). Today, the NCCCP supports the implementation of cancer plans in all 50 states, the District of Columbia, Puerto Rico, seven tribes/tribal organizations, and six US-Affiliated Pacific Island (USAPI) jurisdictions.
In 2006, the CDC, ACS, NCI, and UICC began working together to move the CCC model to other countries, with the development and delivery of a series of training. The first international cancer control leadership forum (Forum) was held in Latin America in 2006 [7]. Additional Forums were held in 2007 and 2008, with select countries. In 2013, the US NCI Center for Global Health began a renewed effort to engage countries in national cancer control planning efforts and restarted the Forums [8].
Like in the US, international cancer control partners have come together to support countries as they develop and implement national cancer control plans. In 2012, NCI worked with its partners to create the International Cancer Control Partnership (ICCP). The ICCP has been instrumental in the delivery of the Forums and has established a web-portal (http://www.iccp-portal.org/) to assist countries as they develop and implement national cancer plans [ 9]. The ICCP recently completed a review of national cancer control plans [10] which found that effective cancer control planning can guide countries in making the right investments towards improving cancer outcomes [11].
Methods
Adapting the CCC approach to the Pacific
The CCC approach has been applied in politically and geo-graphically defined communities such as tribes, states, US territories, and internationally at a country level. Below, the authors describe the history, structure, and utility of the ccc approach based in a Pacific regional multi-national, multi-cultural coalition, the Cancer Council of the Pacific Islands (CCPI), and posit the following questions: Can the CCC approach be effectively used for cancer control across multi-national, multi-cultural settings?
The historical narrative of the regional CCC approach in the USAPI described below speaks to the innovation, significance, challenges, and limitations of a multi-national regional coalition.
Evolution of a regional approach to cancer control in the Pacific
The USAPI jurisdictions (Fig. 1) are spread across the Pacific Ocean, north and south of the equator, spanning more than one million square miles. The USAPI jurisdictions include two US Territories (American Samoa, Guam), a US Commonwealth (Commonwealth of the Northern Mariana Islands), and three sovereign island nations (Federated States of Micronesia (including the States of Chuuk, Kosrae, Pohnpei, and Yap states), the Republic of Palau (Belau), and the Republic of the Marshall Islands). The total population of the USAPI is approximately 450,000. Each of the respective island jurisdictions has unique languages and cultures. Small populations dispersed over hundreds of islands and islets, separated by thousands of miles of ocean, is a challenging environment in which to deliver healthcare. Significant health disparities exist between the respective populations of the U.S. continent and USAPI jurisdictions due to multiple complex factors, including historical, social, cultural, environmental, and economic factors. Health disparities also exist within the USAPI themselves, most notably between populations living on the main or central island and those living in the outer islands far from the most populated areas [12].
Fig. 1.
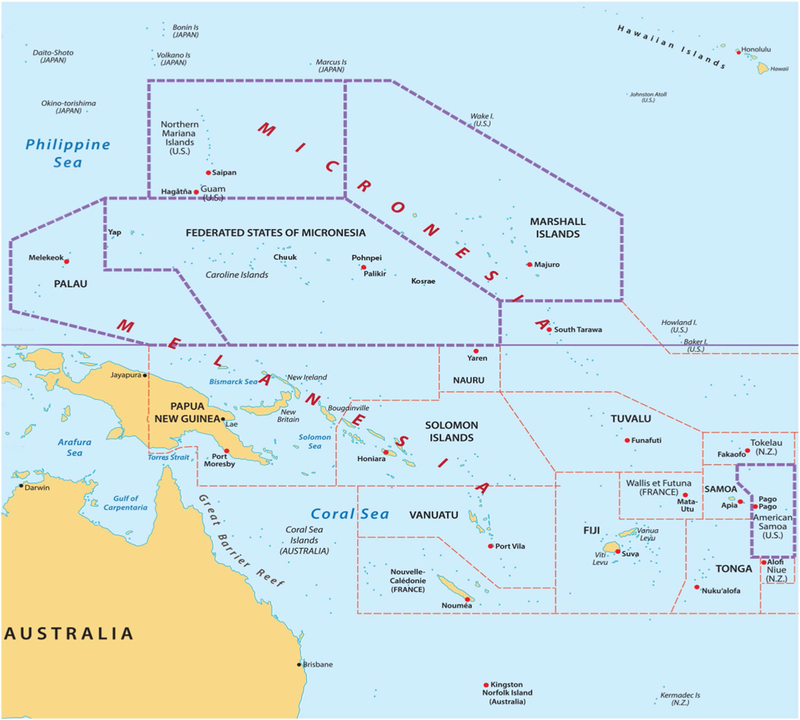
Map of the US-Affiliated Pacific Island Jurisdictions https://www.123rf.com/profile_rusak
Westernization of the USAPI has resulted in an increase in unhealthy behaviors, including an increase in tobacco and alcohol use, decrease in physical activity, and an increase in non-native foods which are of little nutritional value. As a result, non-communicable diseases (NCDs) are a significant threat to the health of the USAPI. Cancer is now the second leading cause of death in most USAPI jurisdictions (Fig. 2) [12].
Fig. 2.
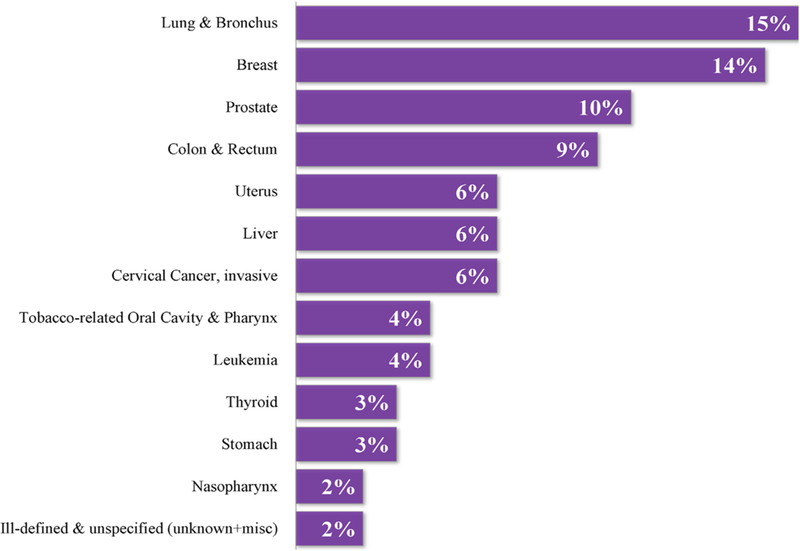
Proportional distribution of adult cancers in the USAPI, 2007–2015 Pacific Regional Central Cancer Registry, University of Hawai’i
Between 1990 and 1997, USAPI clinicians reported rising numbers of late- stage cancers throughout the USAPI. In 1997, Pacific-based community champions actively sought partnerships to assess the regional cancer burden and to fund the development of a Pacific, USAPI-focused organization to address the apparent rising cancer burden. In 1999, an effort to understand the north Pacific cancer burden was funded by the Nuclear Claims Tribunal of the Republic of the Mar-shall Islands (RMI). The cancer data in each Micronesian jurisdiction, including Nauru, Kiribati, Republic of Palau, RMI, FSM, Guam, and the CNMI, were collected and categorized using different methods and definitions. In many jurisdictions, cancer data were incomplete and not systematically collected. There was no basis for comparison of data [13–16].
In 2000, the Intercultural Cancer Council (ICC), a US national organization representing populations with dispro-portionate burdens of cancer included the USAPI into their core mission. The ICC provided a wider platform for Pacific advocacy. In 2002, the US National Cancer Institute (NCI) Center to Reduce Cancer Health Disparities responded to the USAPI requests through a new cancer project called the Pacific Cancer Initiative. The NCI funding was extended through an existing NCI grant (U01 CA086105 02) to Papa Ola Lōkahi, a Native Hawai’ian health organization. Administration and oversight of the Pacific Cancer Initiative were handled by the Department of Family Medicine and Community Health at the John A. Burns School of Medicine, University of Hawai’i [17]. The purpose of the Pacific Cancer Initiative was to (1) convene a cancer coalition with representation from all the USAPI health services, with members who were appointed by their respective jurisdiction ministers or directors of health, and (2) assess cancer-related health capacity and gaps in the region.
The results of the assessments, conducted across all USAPI jurisdictions, were the foundation for regional and jurisdiction-specific cancer priorities and plans. Further assessments and data gathering, such as the information dis-played in Table 1, inform the current regional cancer priorities and strategies [17–19]. As noted in Table 1, many of the prevalent cancers in the USAPI are associated with tobacco and or with obesity. The prevalence of oral cavity cancers is also very high in some jurisdictions due to the widespread use of betel nut from young ages. These cancer risk factors are modifiable. Many of the cancers may be detected at earlier stages with screening and through physical examinations. The 5-year mortality of preventable cancers and or cancers that may be detected early is significant.
Table 1.
Adult cancer cases in the USAPI
| USAPI adult can-cers 2007–2015 (20 years and older) | Counts | Tobacco-related (lung & OC&P) (%) | Tobacco-related OC&P (%) | Tobacco OC&P as a % of total tobacco | Obesity-related (%) | Screening test available (%) | Early physical diagnosis (%) | % dead within 5 years of diagnosis |
|---|---|---|---|---|---|---|---|---|
| Guam | 2,843 | 58 | 2 | 6 | 30 | 41 | 17 | 35 |
| FSM | 579 | 63 | 12 | 32 | 20 | 29 | 11 | 67 |
| RMI | 442 | 60 | 2 | 9 | 17 | 38 | 8 | 57 |
| CNMI | 316 | 65 | 7 | 27 | 36 | 38 | 15 | 36 |
| Pohnpei | 262 | 69 | 13 | 30 | 22 | 34 | 12 | 64 |
| Palau | 250 | 56 | 8 | 23 | 21 | 27 | 16 | 65 |
| Am Samoa | 212 | 73 | 1 | 18 | 57 | 40 | 29 | 33 |
| Yap State, FSM | 155 | 62 | 21 | 52 | 19 | 28 | 14 | 55 |
| Chuuk State, FSM | 118 | 55 | 3 | 9 | 18 | 24 | 7 | 81 |
| Kosrae State, FSM | 44 | 52 | 7 | 18 | 14 | 23 | 5 | 91 |
OC oral cavity, P pharynx
In the second year of the Pacific Cancer Initiative, the CCPI was convened to serve as the focal point for cancer-related efforts in the region. The CCPI provides the over-all direction for regional CCC efforts. CCPI members are appointed from each jurisdiction by their respective directors of health.
In 2003, working with the CCPI, the University of Hawai’i was designated the bona fide agent for the USAPI to apply for and receive funds from the CDC National Comprehensive Cancer Control Program (NCCCP). With the NCCCP resources, CCC coalitions and plans were developed in each of the respective USAPI jurisdictions. There are 10 cancer coalitions: Five in the FSM (one coalition in each of the respective FSM States and a National FSM coalition) and one cancer coalition for each of the remaining five USAPI jurisdictions. By 2006, the local cancer coalitions were mature and were able to compete for CDC NCCCP funding directly. Whereas the relationship between the CCPI, the University of Hawai’i, and the USAPI juris-dictions was deemed successful, each of the USAPI juris-dictions provided funding from their NCCCP funds to continue the work of the CCPI and the University of Hawai’i. Technical assistance to the USAPI jurisdictions to evaluate, revise, and implement their respective CCC plans has continued through this relationship.
The CCPI also began developing the first Pacific regional CCC plan in 2005; the completed plan covered 2007–2012. The regional plan [20] (which can be accessed here) serves as a roadmap for USAPI and key partners to achieve cancer control by working towards defined priorities. The regional plan is informed by the six jurisdiction CCC plans (Guam, CNMI, American Samoa, Palau, RMI, and the Federated States of Micronesia, which currently has 1 national plan with state-specific activities and indicators). There is close collaboration between cancer control leaders, programs and coalitions and their NCD counterparts as a logical way to maximize and leverage resources for cancer and other chronic diseases. The 2018–2022 regional plan is near completion.
Results
Pacific regional cancer control programs and partners (PRCP)
The CCPI and the University of Hawai’i, using the CCC approach, were able to recognize several significant deficiencies in cancer prevention and control in the region: (1) accurate data and information regarding cancer rates, morbidity, and mortality were missing, (2) a multi-level, multi-sector stakeholder partnership at the jurisdiction, regional, and international level was required to address many of the respective USAPI cancer control needs, and (3) there were no existing systematic, data-driven, specific cancer prevention and control plans. A Pacific Regional Cancer Control Program and Partners (PRCP) organization evolved (Fig. 3). The CCPI became the coordinating and advisory body for the organization. The Pacific Islands Health Officers Association (PIHOA) served as the policy advisory group to the CCPI, as PIHOA members are the ministers, secretaries, or directors of health for their respective jurisdiction [21].
Fig. 3.
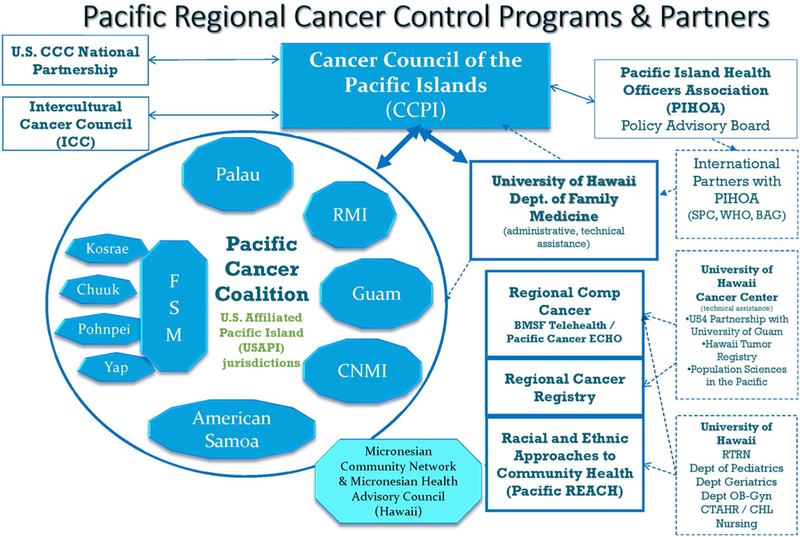
Pacific regional cancer control partners (PRCP)
In 2007, in response to the dearth of cancer data and information, the CCPI and the University of Hawai’i applied for a CDC National Program of Cancer Registries (NPCR) cooperative agreement. The cooperative agree-ment provided the funding to develop a population-based Pacific Regional Central Cancer Registry (PRCCR). The PRCCR provides cancer registry staff, training, and technical assistance in each jurisdiction, including the four FSM States.
To complement the CCPI cancer risk reduction efforts at the jurisdiction level, the University of Hawai’i applied for and was awarded a CDC Racial and Ethnic Approaches to Community Health (REACH) Center of Excellence in the Elimination of Disparities (CEED) in breast and cervical cancer cooperative agreement in 2007. The REACH programs were implemented in each of the respective USAPI jurisdictions. REACH emphasizes a policy, systems, and environmental (PSE) approach as a means to make the default choice in cancer risk environments a healthy behav-ior [22, 23].
Limitations in funding, trained health personnel, and healthcare infrastructure have challenged cancer screening efforts in many parts of the USAPI. There was no systematic screening for colorectal cancer or mammography cancer screening in the FSM and the RMI. Pap test screening in the FSM, RMI, and Republic of Palau was hindered by the lack of an on-site pathologist and daunting geographic isolation of segments of the population. To adjust to the environmental and resource reality, alternative methods for population-based screening for cancers of the breast, cervix, and colon have been investigated and developed as resources allow. Distance pathology services using digital microscopy are being explored to provide pathology services. Visual inspection of the cervix with acetic acid (VIA) has replaced the Pap smear in some locations, and clinical breast exams and ultrasound are used to detect breast cancer in the FSM. The CCPI and the University of Hawai’i provided the technical assistance and planning which enabled resource-appropriate standards of cancer care, especially cancer screening methods [24].
Cancer research has been identified as a gap in the regional and the respective USAPI local comprehensive cancer plans. The CCPI in conjunction with its university partners has completed evaluation research in cervical cancer screening and has investigated the use of a urine-based HPV DNA test for cervical cancer. The research gap was discussed with the CCPI and the target community. The organizational design and CCC process enhanced effective participatory community engagement to evaluate and monitor the research efforts. The University of Hawai’i Cancer Center through an NCI U54 disparities grant and its Hawai’i Tumor Registry has augmented the research and Pacific Regional Cancer Registry efforts in the USAPI since 2007.
Working across the cancer prevention and control continuum has linked the Pacific Cancer Partnership with programs that also address health disparities, tobacco control, obesity reduction, healthy nutrition, infectious diseases (Hepatitis B, Hepatitis C, HPV) vaccinations, increased physical activity, increased human health resource development and capacity, and cancer-focused programs (breast and cervical cancer screening programs). These domains are associated with cancer etiology, risk factors, and out-comes. Working with tobacco control, non-communicable disease obesity, nutrition, and health workforce training programs has been beneficial for all programs.
In 2010, the USAPI Directors of Health declared a State of Emergency to bring focus to the NCD epidemic in the USAPI and mobilize resources. To harmonize efforts, the NCD-associated programs (tobacco, diabetes, and cancer) in Guam, the FSM, RMI, and Palau were managed under a single NCD director within the respective health ministries.
The regional and jurisdiction-specific infrastructure components have set the stage for addressing cancer in the Pacific region, in a way that is self-directed. The organizational components include policy bodies (PIHOA), aca-demic partners (University of Hawai’i), funding and technical assistance organizations (WHO, CDC), and research partners (UH John Burns School of Medicine, UH Cancer Center).
Discussion
The USAPI jurisdictions developed a regional organization, the CCPI, to address cancer control in the Pacific. CCC principles and strategies have been used by the CCPI to develop a larger partnership organization and regional Pacific-centric collaborative to address the USAPI cancer prevention and control needs. The CCC methodology provided a planning methodology for the CCPI and the PRCP to (1) harmonize cancer control efforts between nine multi-lateral, multi-cultural Pacific jurisdictions, (2) represent the USAPI cancer control needs as a single voice in the global environment, and (3) facilitate cancer control planning and implementation with the respec-tive USAPI jurisdiction coalitions. The outcomes of the regional work includes (1) developing a USAPI regional population-based cancer registry (CDC National Program of Cancer Registries-funded Pacific Regional Central Cancer Registry), (2) developing and implementing dynamic regional CCC plans which are informed by the respective USAPI jurisdiction-specific cancer plans, (3) leveraging funding and resources for ongoing cancer prevention and control work in the USAPI, (4) developing on-site technical assistance programs and training for the cancer coalitions in the USAPI, (5) changing standards of care for cancer screening and prevention to fit the resource and cultural nuances of the USAPI, (6) developing and scaling relevant evidence-based interventions for cancer control in the USAPI environment, and (7) leveraging human and funding resources for larger NCD efforts that also address the World Health Organization’s global NCD and cancer control targets.
Having a structured cancer organization and planning process has made linkages across programs with overlapping or similar goals possible. Whereas many of the cancer risk factors such as tobacco, obesity, physical exercise, nutrition, health policy, lack of a trained workforce, and social determinants of health are part of the business of other programs and health organizations, collaboration was necessary and strategic. Working with and across NCD, tobacco, and health workforce development programs has become the operational norm in the USAPI.
Limitations
There are several limitations of regionalization. Development of the CCPI as a functional multi-national, multi-cultural coalition requires time and a long view of cancer control. The regional effort identified a common goal (addressing a rising cancer burden), a need to work together to be more visible and have greater agency in the global setting, and a need to come together to leverage resources. Without a common set of identified needs for cancer control, regional coalition building would be difficult. However, establishing common goals and priorities is a long, arduous process.
At various times in the history of the CCPI, the Pacific partners waxed and waned in their participation and interest in the regional partnership and its planning efforts. Maintaining constant communications and a strong relationship with the respective USAPI directors and partner leadership is crucial to maintaining organizational stability. Constant effort through a central CCPI secretariat is necessary.
Personnel should include a dedicated full-time, paid, cancer coalition Program Manager in each jurisdiction, as well as the participatory engagement of the respective civil society leadership. Dedicated personnel and a regional secretariat require government or grant funds.
Applications
The USAPI regional model has been functional in a multi-cultural, multi-national, resource-limited environment. A regional model could be applied in various global settings, including (1) island communities with common health goals, (2) low-income countries in a particular geographic location to synergize human and financial resources, (3) communities or provinces (defined by geography) within a larger country, and (4) communities with cancer disparities (defined by socio-economic status, rurality, ethnicity, gender, immigration status) within a larger country.
Conclusion
The CCPI, a Pacific-based regional coalition, has been an effective engine of change for cancer prevention and control in the USAPI and Pacific. The CCPI has adopted and applied the CCC approach and coalition building strategies to navigate the political, geographic, demographic, and epidemiologic seascape of the USAPI at the jurisdiction and regional levels. The CCPI with its multi-level regional partners has been able to harmonize cancer control efforts in countries with culturally, linguistically, economically, and politically diverse environments. Regional cancer coalitions linked to stakeholder organizations may be effective in the global arena to effectively harmonize the efforts of individual communities, states, or countries.
Acknowledgments
The authors would like to acknowledge the individuals who were instrumental in founding the CCPI in 2003. They are Dr. Harold Freeman (NCI), Dr. Johnny Hedson (Pohnpei, FSM), Dr. Victor Tofaeono (AS), Dr. Victor Ngaden (deceased—Yap, FSM), Wincener David (Pohnpei, FSM), Dr. Kamal Gunawardane (RMI), Dr. Richter Yow (Yap, FSM), Dr. Livinson Taulung (Kosrae, FSM), Dr. Robin Shearer (CNMI), Dr. Sheldon Riklon (RMI), Jocelyn Songsong (CNMI), Margaret Sesepasara (AS), Dr. Vita Skilling (Kosrae, FSM), Yorah Demei (ROP), Dr. Francisca Soaladaob (ROP), Dr. Kino Ruben (Chuuk, FSM), and Rosalie Zabala (deceased—Guam).
Funding This publication was supported by Centers for Disease Control and Prevention Cooperative Agreement Numbers 17NU58DP006312 (Pacific Regional Central Cancer Registry 2017–2022), NU58DP006335 (American Samoa CCC 2017–2022), NU58DP006348 (CNMI CCC 2017–2022), NU58DP006269 (Guam CCC 2017–2022), NU58DP006303 (FSM CCC 2017–2022), NU58DP006336 (RMI CCC 2017–2022), NU58DP006289 (Palau CCC 2017–2022), NU58DP005810 (REACH 2014–2018), DP003906 (PRCCR 2012–2017), DP000976 (PRCCR 2007–2012), DP000777 (American Samoa CCC 2012–2017), DP00847 (CNMI CCC 2012– 2017), DP000781 (Guam CCC 2012–2017), DP000779 (FSM CCC 2012–2017), DP000826 (RMI CCC 2012–2017), and DP003939 (Palau CCC 2012–2017), along with the National Cancer Institute 2U54CA143727. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention, the National Cancer Institute, or the Department of Health and Human Services.
References
- 1.Given LS, Black B, Lowry G, Huang P, Kerner JF (2005) Collaborating to conquer cancer: a comprehensive approach to cancer control. Cancer Causes Control 16(1):3–14 [DOI] [PubMed] [Google Scholar]
- 2.The Union for International Cancer Control (UICC) ECLE (2012) Supporting national cancer control planning: a toolkit for Civil Society Organisations (CSOs) Geneva [Google Scholar]
- 3.Given LS, Hohman K, Graaf L, Rochester P, Belle-Isle L (2010) From planning to implementation to outcomes: comprehensive cancer control implementation building blocks. Cancer Causes Control 21(12):1987–1994 [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (2016) National Comprehensive Cancer Control Program Logic Model Centers for Disease Control and Prevention, Online [Google Scholar]
- 5.Comprehensive Cancer Control National Partnership (2018) Comprehensive cancer control national partnership website https://www.cccnationalpartners.org. Accessed 11 Aug 2018 [DOI] [PMC free article] [PubMed]
- 6.Hohman K, Rochester P, Kean T, Belle-Isle L (2010) The CCC National Partnership: an example of organizations collaborat-ing on comprehensive cancer control. Cancer Causes Control 21(12):1979–1985 [DOI] [PubMed] [Google Scholar]
- 7.Isle LB, Plescia M, La Porta M, Shepherd W (2010) In conclusion: looking to the future of comprehensive cancer control. Can-cer Causes Control 21(12):2049–2057 [DOI] [PubMed] [Google Scholar]
- 8.National Cancer Institute (2018) Cancer control leadership forums https://www.cancer.gov/about-nci/organization/cgh/research/cancer-control-leadership-forums. Accessed 11 Aug 2018
- 9.International Cancer Control Partnership (2018) Developing a NCCP https://www.iccp-portal.org/developing-nccp. Accessed 11 Aug 2018
- 10.Romero Y, Trapani D, Johnson S, Tittenbrun Z, Given L, Hohman K, Stevens L, Torode JS, Boniol M, Ilbawi AM (2018) National cancer control plans: a global analysis. Lancet Oncol 19(10):e546–e555. 10.1016/S1470-2045(18)30681-8 [DOI] [PubMed] [Google Scholar]
- 11.International Cancer Control Partnership (2018) Achieving mesurable progress towards the NCD targets: the importance of National Cancer Control Plans (NCCPs) UICC, online [Google Scholar]
- 12.Pacific Regional Central Cancer Registry (2018) Cancer in the US Affiliated Pacific Islands 2007–2012 University of Hawai’i, online [Google Scholar]
- 13.Palafox NA, Yamada S, Ou AC, Minami JS, Johnson DB, Katz AR (2004) Cancer in Micronesia. Pac Health Dialog 11(2):78–83 [PubMed] [Google Scholar]
- 14.Katz AR, Palafox NA, Johnson DB, Yamada S, Ou AC, Minami JS (2004) Cancer epidemiology in the freely associated U.S. Pacific Island jurisdictions: challenges and methodologic issues. Pac Health Dialog 11(2):84–87 [PubMed] [Google Scholar]
- 15.Ou AC, Waidubu G, Etheredge GD, Palafox NA (2004) Epide-miology of cancer in the Republic of Nauru. Pac Health Dialog 11(2):101–106 [PubMed] [Google Scholar]
- 16.Ou AC, Kienene T, Tenaua K, Etheredge GD, Palafox NA (2004) Epidemiology of cancer in the Republic of Kiribati. Pac Health Dialog 11(2):88–93 [PubMed] [Google Scholar]
- 17.Palafox NA, Tsark JU (2004) Cancer in the US Associated Pacific Islands (USAPI): history and participatory development. Pac Health Dialog 11(2):8–13 [PubMed] [Google Scholar]
- 18.Gunawardane K, Demei Y (2004) Cancer Council of the Pacific Islands: speaking with one voice. Pac Health Dialog 11(2):14–16 [PubMed] [Google Scholar]
- 19.Palafox NA, Gunawardane K, Demei Y (2006) Pacific island partnership: the Pacific cancer initiative. J Cancer Educ 21(1 Suppl):S87–S90. 10.1207/s15430154jce2101s_15 [DOI] [PubMed] [Google Scholar]
- 20.Cancer Council of the Pacific Islands (2015) USAPI Pacific Regional Comprehensive Cancer Control Plan 2012–2017 Department of Family Medicine and Community Health, John A. Burns School of Medicine, University of Hawai’i-Manoa [Google Scholar]
- 21.Cancer Council of the Pacific Islands (2018) Cancer Council of the Pacific Islands http://www.pacificcancer.org/programs/cancer-council-of-the-pacific-islands.html. Accessed 11 Aug 2018
- 22.Nitta M, Tanner C, Narvarte K, Luces P, Silverio A, Zabala R, Navasca D, Sy A, Palafox NA (2015) Policy, system, and environment strategies to promote physical activity and healthy food sources to address Guam’s disparate non-communicable disease burden. J Health Care Poor Underserved 26(2 Suppl):96–103. 10.1353/hpu.2015.0057 [DOI] [PubMed] [Google Scholar]
- 23.Nitta M, Navasca D, Tareg A, Palafox NA (2017) Cancer risk reduction in the US Affiliated Pacific Islands: utilizing a novel policy, systems, and environmental (PSE) approach. Cancer Epi-demiol 50:278–282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American College of Obstetrics and Gynecology (2015) Committee Opinion No. 624: cervical cancer screening in low-resource settings. Obstet Gynecol 125(2):526–528. 10.1097/01.AOG.0000460763.59152.9e [DOI] [PubMed] [Google Scholar]


