Abstract
Osteoarticular tuberculosis (OATB) Aim: The authors made a clinical morphological assessment of tissue samples from patients admitted in Surgical Departments of the Emergency County Hospital of Craiova, Romania, between 1990 and 2015, proved as presenting tuberculous lesions of the spine in the Department of Pathology of the same Hospital. Materials and Methods: The studied material consisted of bone, joint and sometimes muscle tissue fragments resulted from biopsies or surgical excisions from 7 cases coming out of 54 patients investigated in the above-mentioned period of time, where the established histological diagnosis was tuberculosis (TB). For diagnostic confirmation, Ziehl-Neelsen staining has been used as a rule but, in some cases, immunohistochemistry was also used. Results: TB lesions have prevailed in men and around the age of 50 years. Thoracic segment of the spine was the most involved. Epithelioid and giant Langhans cells dominated the inflammatory cellular population. Necrosis was always present, usually in its classical acidophilic form. Fibrosis was almost always absent. On the whole, the granulomatous reaction was in almost half of the cases hyporeactive and disorganized. Conclusions: The clinical morphological profile of our series is fitting with data described in the literature. Because of its life threatening potential, spinal TB should be investigated thoroughly especially in its morphological features in order to obtain as quickly as possible an etiological diagnosis.
Keywords: Extrapulmonary tuberculosis, Spine tuberculosis, Bones, Joints
Introduction
Spinal tuberculosis (STB) or spondylitis or spondylodiscitis refers to an infection by Mycobacterium tuberculosis (Mt) affecting the intervertebral disk, the vertebral body itself or the posterior vertebral arch, with or without involvement of the spinal canal [1,2,3].
It is one of the oldest reported diseases in humans. Although discovered and described by Pott in 1776, skeletal changes, such as collapse of the vertebrae (Pott's disease), have been reported in pre-dynastic Egypt (3500-2650 BC), and Neolithic Sweden culturally associated with the earliest cattle breeders (3200-2300 BC) but molecular proofs of Mt presence were detected in 9,000-year-old human fossils and non-specific morphological changes consistent with tuberculosis were found in a fossil Homo erectus dated from the middle Pleistocene (490-510,000 years BP) [2,4,5,6,7,8].
Tuberculous spondylitis is the most common form of osteoarticular TB (OATB), representing alone 50% of all cases of OATB involvement. Osseous involvement by TB is, in its turn, reported as the most common site of extrapulmonary tuberculosis (EPTB) in Taiwan (with 24.5% of cases) to the third most common site in the United States (with 11.3% of cases, after pleural and lymph node involvement) [2,9,10,11,12,13,14].
Tuberculosis of the spine is a potentially life-threatening infection because it can produce neurological complications and, the most important, it is one of the most common world-wide causes of a kyphotic spinal deformity [15,16,17].
Moreover, there is a small number of cases of atypical spinal TB, not resembling with tuberculous spondylitis that often make diagnostic delays and even errors [18,19].
The aim of this study is to report some main clinical and especially morphological aspects of TB lesions of the spine admitted in Surgical Clinics and especially Orthopedic Clinic of the Emergency County Hospital of Craiova, Romania, and diagnosed in in the Departments of Clinical Laboratory and Pathology between 1990 and 2015.
Material and Methods
The study group consisted of 7 cases admitted and diagnosed in the above-mentioned period and medical unit with TB inflammatory lesions of the spine. The group was part of a larger series of 54 patients proved as presenting tuberculous lesions involving structures of the osteoarticular system which, in turn, were part of a series of 841 patients proved as presenting tuberculous lesions in extrapulmonary sites in the Department of Pathology in the studied period of time.
The studied material consisted of: (a) accompanying notes of tissue specimens coming from surgery rooms; (b) histological records, paraffin blocks and Hematoxylin-Eosin (HE) stained slides of each case from the Department of Pathology’s archives.
The study was of retrospective type and the assessed parameters were grouped in:
[I] Clinical parameters: general involvement of the spine; temporal distribution of cases; gender; age; suspicion of the etiological diagnosis at admission.
[II] Morphological parameters:
(1) Lesions’ site in the spine.
(b) Assessment of: granuloma cellularity; presence and type of necrosis; presence of fibrosis; the granulomatous lesions degree of differentiation.
(c) Clarification of atypical lesions or caseous necrosis as dominating aspect of the lesion but with a non-specific granulomatous reaction around.
Serial sections were cut from paraffin block and stained as follows:
- First section-Haematoxilin-Eosin (for first diagnosis)
- Second section-Ziehl-Neelsen staining (for identification of acid-fast bacilli)
- Immunohistochemical staining for Mt (for etiological confirmation). The antibody used is presented in Table 1. Positive external control was made on sections from cases with pulmonary TB known as positive for Mt on Ziehl-Neelsen stained slides.
Table 1.
Antibody used to identify Mt
| Antibody | Source | Dilution | Pretreatment |
| Mo a Hu Mt clone BGN-3875 | Novus Biologicals | 1:500 | 20 minutes Citrate buffer, pH 6 |
| Mt: Mycobacterium tuberculosis | |||
Histopathology was assessed and areas of interest selected utilizing a CX31 Olympus microscope using the ×4 magnification objective. For final image acquisition, optical planapochromate corrected objectives with magnifications of ×4, ×10, ×20 and ×40 were used in order to capture high quality micrographs.
The most significant images were acquired using a LiveViewPro II color CCD digital camera, saved directly on the computer and processed using the specialized image analysis software package analySIS Pro.
For some parameters, be they clinical or morphological, the need for an accurate assessment of the tuberculous inflammatory process required the development of allocation criteria of cases that generated stratification scales of cases according to each criterion.
Thus, for age evaluation, the scales are presented in Table 2.
Table 2.
Stratification scale for age
| Age period | Age | |
| P1 | Child (Ch) | 0-14 years |
| P2 | Adolescent (Ad) | 15-24 years |
| P3 | Young adult (YA) | 25-44 years |
| P4 | Mature adult (MA) | 45-64 years |
| P5 | Elderly (Eld) | >65 years |
In order to determine the degree of effectiveness of inflammatory complex intervention, we applied a modified granulomatous lesions classification system according to their organization, system proposed but only for lymph node lesions by Ramanathan et al., in 1999 [20] (Table 3).
Table 3.
Granulomas classification according to their degree of organization [modified after Ramanathan et al. (1999)]
| Type | Code* | Code** | Grade | Cells | Necrosis | |
| Hyp | G1 | Ia | Well diff | EC | Scarce | Absent/IN |
| Ib | EC+GLC | |||||
| R | G2 | II | m EC | AN Mi | ||
| M | ||||||
| L and P | ||||||
| Hypo | G3 | III | Poor diff | M | BN Ma | |
| i EC | ||||||
| L and P | ||||||
| A | G4 | IV | Dis | M | NCN | |
| L, P | ||||||
| PMN | ||||||
The data was processed and the graphs were drawn using the Microsoft Excel module of the Microsoft Office 2010 Professional software package.
Results
Clinical data
Cases with STB represented only a small part from the larger series with OATB (almost 15%) and even a smaller part from the entire review series of EPTB, meaning 1% of all investigated cases (Fig.1).
Figure 1.
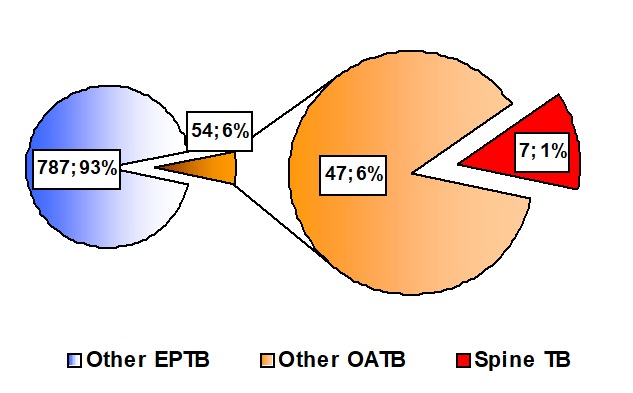
Spine involvement
Temporal evolution
As the Figure 2 shows, all STB cases were admitted in our hospital after 2010, representing the last five years period of our 26 years period of study of OATB.
Figure 2.

Temporal evolution of cases
If we compare the evolution trend with that of the larger series of OATB cases, we could observe that the OATB case on the whole had a descending trend during the studied period of time while the spine TB cases “exploded” in the last five years.
However, in this time, the number of cases varied from year to year (2 cases in 2010, one case in 2011, one case in 2013 and, finally, 2 cases in 2014), with a general decreasing trend.
Gender and Age
Most of our cases were males (Fig.3) but the lesions did not “avoid” the females.
Figure 3.
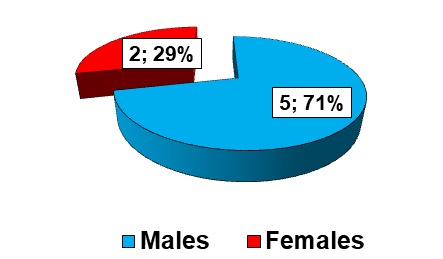
Gender distribution
The mean age was of 53,5 years. The youngest patient was a male of 33 years old and the oldest one was a female of 72 year old.
Females were both over 44 years old, belonging to the ”Mature Adult” and ”Elderly” categories while the Males were generally around 50 years old.
However, the youngest male patient was 33 year old, as mentioned before, and therefore included in the category ”Young Adult”, and the oldest male patient was 65 years old (Fig.4).
Figure 4.

Age distribution
Clinical suspicion
The diagnosis of TB was suspected in all cases excepting one (Fig.5).
Figure 5.

Clinical suspicion
Due to the improvements in imagistic examination offered by the new techniques of investigation such us computed tomography (CT) and magnetic resonance imaging (MRI), one could better reveal characteristic aspects like destructive lesions in one of the anterior margins of the body of a vertebra, multiple levels of involvement, with ”mirror” vertebral caries aspect, increasing loss of disc height (Fig.6) or larger sized paravertebral soft-tissue abscesses, often with calcifications and rim enhancement around (Fig.6b).
Figure 6.
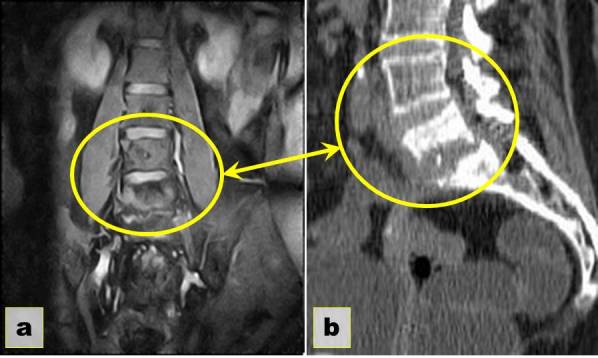
Spinal tuberculosis - L4-L5-S1 level (a) MRI coronal plane STIR 1: ”mirror” vertebral caries; (b) CT: Extensive erosive changes involving the inferior aspect of L5 and superior part of S1 with widened intervertebral space (yellow circles)
The seventh case was a 72 year old woman, who presented on the imagistic examination an area of osteolysis of the T12 vertebral body that had no suggestive features for TB.
Morphological data
Lesion site
As mentioned above, spinal involvement from all OATB studied cases was reduced in comparison with the “50%” reported in the literature [11,12,14,21].
However, the distribution on spine segments was somehow similar with the one reported in the literature, the main involved segment being the thoracic one, followed by the lumbar region (Fig.7).
Figure 7.
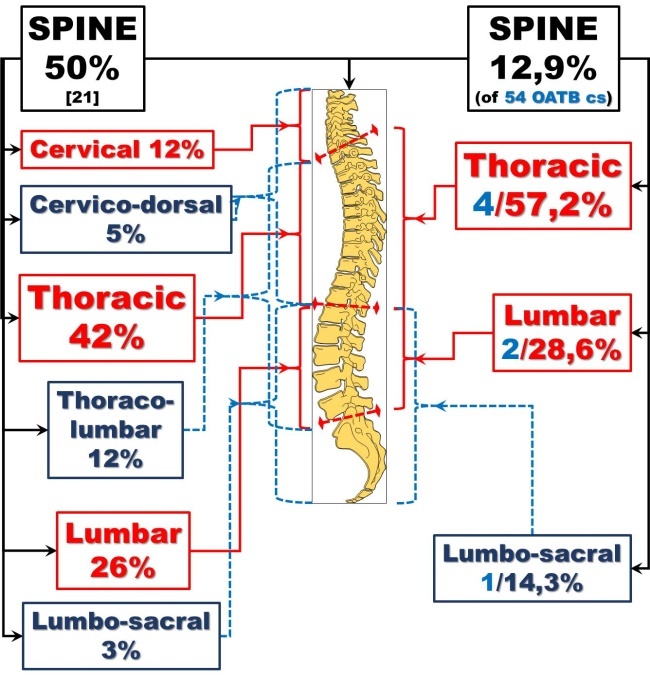
Site distribution
Second observation concerning the site concerned the type of spine tissue involved.
In more than half of the cases (4 cases) TB lesions involved both the vertebral bones and the intervertebral joint structures. In other two cases only the articular structures were involved, and in only one case only the vertebral bone harbored the TB lesion.
The third observation referred to the number of vertebrae affected by the tuberculous process.
Thus, there was only on case with only one vertebral body involved. In more than half of the cases (4 cases) two vertebrae were involved. In the remaining two cases three vertebrae were affected, in both case in the thoracic region.
Granuloma cellularity
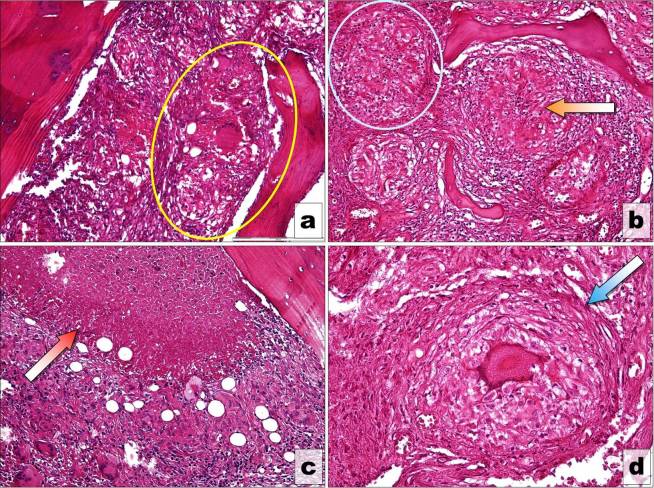
The inflammatory population of cells was dominated by the couple of macrophage cells: epithelioid cells and giant Langhans cells (Fig.8a and Fig.9a-b).
Figure 8.
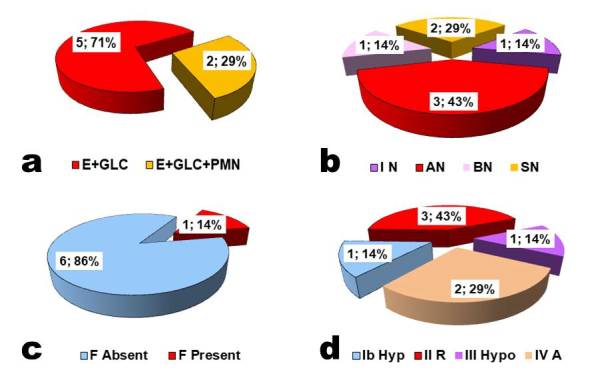
Granuloma morphology (a) Cell distribution; (b) Types of Necrosis; (c) Presence of Fibrosis; (d) Types of Granulomas
Figure 9.
Granuloma morphology (a) Giant Langhans cell granuloma producing bone erosion (yellow circle) H-E stain, X100; (b) Epithelioid granuloma (blue circle) and Incipient necrosis (orange arrow) (c) Acidophilic fine granular necrosis (red arrow); (d) Fibrosis around LGC granuloma (blue arrow)
However, in two cases neutrophils added to the inflammatory cellular population, signaling a superinfection of the TB inflammatory focus (Fig.8a).
Presence and type of necrosis
Necrosis was present in all cases and exhibited all its morphological variants. The most frequent variant observed was the classic acidophilic fine granular necrosis (Fig.8b and Fig.9c).
However, in one case the necrosis was incipient in the center of the granulomatous lesions (Fig.8b and 9b) and in another case the aspect was basophilic macrogranular.
In the remaining two cases, the classical, caseous aspect of the necrotic material was transformed by the superadded infection in purulent aspect.
Presence of fibrosis
The process of perilesional fibrosis was observed in only one of the seven cases, where the collagen fibers isolated the necrotic area inside the vertebral body of the T12 vertebra creating a cystic appearance on the imagistic investigations.
Granuloma differentiation
Putting together all morphological aspects of the granulomatous reaction, its general aspect had significant variations. On one hand, three of the cases presented type II, reactive granulomas, with both epithelioid and giant Langhans cells and classical acidophilic, fine granular necrosis. Other three cases, in turn, expressed hyporeactive and even areactive granulomas, the latter with the purulent transformation of the necrotic areas.
Lesions extension
Another characteristic of our series was the extension of the lesion from the initial site, by contiguity, in the paraspinal spaces (Fig.10a and c) and, moreover, generating cold abscesses (Fig.10b and d) found in sites far from the infectious focus, particularly in the sheaths of the psoas muscles.
Figure 10.
Extraspinal extension (a) Muscle involvement. (b) Presence of cold abscesses (c) Giant Langhans cell granuloma in the muscle (darck blue circle) H-E stain, X100; (d) IRM sagittal STIR 1: Anterior cold abscess and L4-L5-S1 arthritis (yellow circle)
Discussions
Clinical data
It is generally accepted, as we mentioned before, that spine involvement represents the largest part, around half of OATB cases [3,11,12,14]. But, as Figure 11 illustrates, the percentage varies in a wide range, depending on series reported [22,23,24,25,26,27,28,29,30,31,32], from more than 80% [22] to less than 40% [31,32].
Figure 11.

Comparison with other studies of STB presence
In this context, our study, with such a reduced number of cases with STB in such a long period of time, is a particular one for two reasons. The first is that, even if the studied period is very large (more than 25 years), the hospital is a general hospital where the Orthopedics and Pediatric Surgery departments are two of the sixteen surgical departments that provided EPTB cases. The second is a particularity of Romanian health care system that we mentioned in our previous studies on OATB [2,33,34], namely OATB lesions and especially STB lesions are still directed for treatment, including surgical procedures in dedicated hospitals.
Temporal evolution
The evolution of STB cases presence during the large period of time taken into consideration could be explained for the period with lack of cases by the above mentioned particularity of our national health care system, and then by the fact that patients had no history of tuberculosis and, therefore they addressed firstly following their complains to the specialist in bone and joint diseases.
Gender and Age
In our series the males prevailed with TB lesions of the spine.
But if we consider different reports from the literature (Fig.12) we could see that in some studies males prevailed [35,36,37] in other there was no significant predilection for one of the genders [38,39] and, surprisingly, there are studies where women are more significantly affected by TB in different regions of the spine [40,41].
Figure 12.
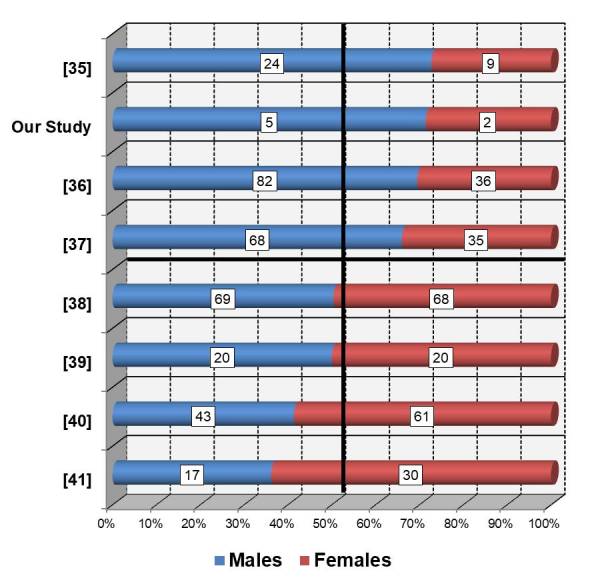
Comparison with other studies of Gender distribution
And these are only few of the numerous reports available. Therefore, we could not allege that in spine involvement, TB has a clear predilection for one of the genders.
We could say the same thing about the patients’ age.
Figure 13 illustrates clearly that TB infection ca involve the spine at any age. From the enormous amount of data we picked again only few reports [39,42,43,44,45,46,47] where we can see, for instance that the youngest patient was two years old [42,43] and the oldest patient was 92 year old [47]. Also, we can observe that there are series of patients with the mean age placed in the “young adult” period of life [42,43,44], other series with the age placed in the “mature adult” period of life [39,45,46], and surprisingly, there are series of patients where the mean age is higher than 70 years, in other words, an entire series of old patients [47].
Figure 13.

Comparison with other studies of Gender distribution
So, for the age too, we couldn’t allege that in spine involvement, TB has a clear predilection for one of the age groups or periods of life.
Morphological data
Lesion site
In the literature it is stated that thoracic and lumbar segments are the most affected spine regions by the Mt infection. Moreover, there is no consensus in defining spine regions.
Some studies use the classical anatomical description of spine regions. Other studies take into consideration the extension of the lesions to two neighboring anatomical regions and, therefore, introduce in the classification sub regions comprising two neighbor anatomical regions. We have chosen for exemplification the clinical extended classification (Fig.14).
Figure 14.
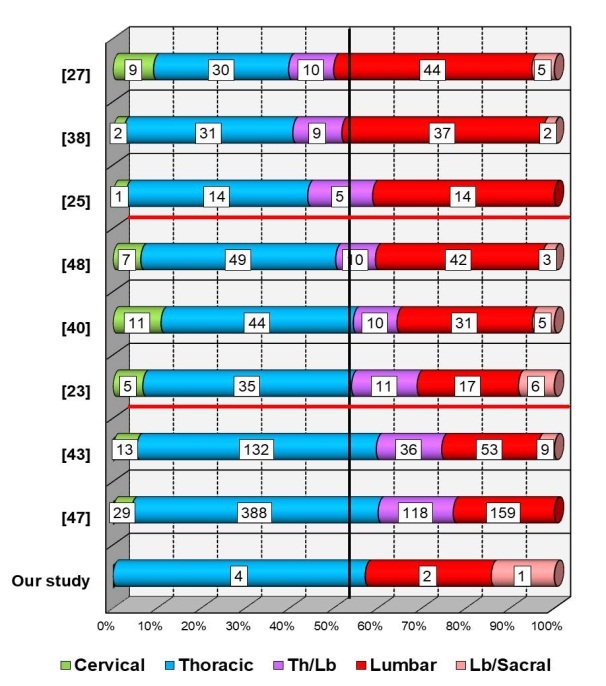
Comparison with other studies of spine segment involvement
Thus, there are studies where lesions placed in the inferior regions of the spine, including here also the border thoracic-lumbar sub region, are prevailing [25,27,38]. At the opposite side, there are studies where lesions placed in the upper part of the spine are prevailing [43,47]. Our study is included in this last category. Finally, there are studies where there is a balance between the involvement of upper and lower parts of the spine [23,40,48].
So, even in the different spine segments we couldn’t talk about a certain tropism of TB infection.
Morphology of the lesions
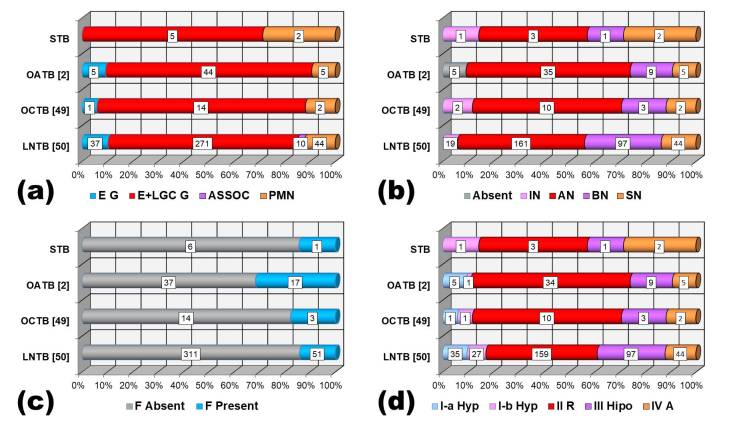
Except for the paper of Ramanathan et al [20], we didn’t find studies in the literature that focused on the analysis of microscopic morphological aspects of TB infection. Therefore, we used for comparison some previous studies of ours focused on other body systems affected by TB like lymph node system, oral cavity structures and, finally the osteoarticular system as a whole [2,33,34,49,50].
Thus, concerning the granuloma cellularity, in all sites, inflammatory cellular population was dominated by epithelioid and giant Langhans cells. Neutrophils were significantly present, in terms of percentage, only in spine lesions (Fig.15a).
Figure 15.
Fig.15. STB lesion morphology-comparison with other studies (a) Specific granuloma cells distribution; (b) Presence and types of necrosis; (c) Presence of Fibrosis; (d) Granuloma types of differentiation
In only few cases of other parts of osteoarticlar system necrosis was absent. Otherwise, necrosis was a constant presence in TB lesions of the studied body systems.
The main aspect of necrotic material was that of acidophilic, fine granular necrosis. However, in lymph node lesions and spine lesions almost half of the cases presented basophilic and purulent necrosis, aspects, suggesting a worse evolution of the inflammatory process (Fig.15b).
The fibrosis, as a sign of repair and healing, was usually absent in all the studied locations, except for the lesions in other parts of the osteoarticular system, where the healing process was present in almost one third of the cases (Fig.15c).
Finally, lymph node lesions and spine lesions presented a significant number of cases, over 40%, with poorly differentiated (grade III) granulomas and disorganized (grade IV) granulomas, suggesting a conflict with worse prognosis (Fig.15d).
Lesions extension
Extension of the lesions in the neighboring tissues and migration of the infection distantly from the initial lesion are events frequently observed in spine lesions, indicating a more severe and late disease stage. From this point of view too, data picked from the literature revealed a wide range of situations. In this respect, we have chosen some studies that were mentioning the presence of cold abscesses (Fig.16).
Figure 16.

Comparison with other studies of abscess presence
Cold abscesses are considered a frequent complication, but its true incidence is unknown. Many of these studies reported the significant presence of this type of migration of the TB infection, from more than 50% up to more than 80% of the cases [38,41,45,47,51,52].
Other studies found this complication in less than 50% of the cases, going to even less than 20% of the cases [53,54,55,56].
In our study, cold abscesses were a significant presence, meaning that our small series gathered together cases in late stages of the disease.
Another sign of severity is the number of vertebrae involved.
In the reports picked from the literature the average number of vertebrae involved varied between “2” and “5” [38,45,51,52,53,57,58,59], with an extreme number of 15 vertebrae involved described by Alothman et al [45] (Fig.17).
Figure 17.
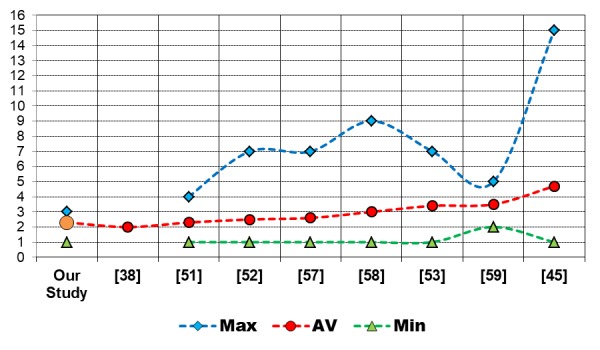
Comparison with other studies of number of vertebrae involved
In our study, the highest number of vertebrae involved was “3” and the average number was “2”.
Conclusions
The “profile” of our small series could be defined as follows: TB spine lesions appeared mainly in adult males, more often in the thoracic region, almost always with the involvement of more than one vertebral body and distant extension. The morphology of granulomatous reactions revealed in the majority of cases active, extending and destructive inflammatory with tendency towards worse evolution and superinfection.
The clinical morphological profile of our series is fitting with data described in the literature. Because of its life threatening potential, spinal TB should be investigated thoroughly especially in its morphological features in order to obtain as quickly as possible an etiological diagnosis.
Conflict of interests
The authors declare that they have no conflict of interests.
References
- 1.Guerado E, Cerván AM. Surgical treatment of spondylodiscitis. An update. Int Orthop. 2012;36(2):413–420. doi: 10.1007/s00264-011-1441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Plesea IE, Anusca DN, Procopie I, Huplea V, Niculescu M, Plesea RM, Ghelase SM, Lupascu-Ursulescu CV. The clinical-morphological profile of bone and joints tuberculosis-our experience in relation to literature data. Rom J Morphol Embryol. 2017;58(3):887–907. [PubMed] [Google Scholar]
- 3.Shikhare SN, Singh DR, Shimpi TR, Peh WC. Tuberculous osteomyelitis and spondylodiscitis. Semin Musculoskelet Radiol. 2011;15(5):446–458. doi: 10.1055/s-0031-1293491. [DOI] [PubMed] [Google Scholar]
- 4.Zink A, Haas CJ, Reischl U, Szeimies U, Nerlich AG. Molecular analysis of skeletal tuberculosis in an ancient Egyptian population. J Med Microbiol. 2001;50:355–366. doi: 10.1099/0022-1317-50-4-355. [DOI] [PubMed] [Google Scholar]
- 5.Nuorala E, Götherström T, Donoghue HD, Spigelman M, Liden K. MTB complex DNA in a Scandinavian Neolithic passage grave. Doctoral Dissertation in: Theses and Papers in Scientific Archaeology 6, Archaeological Research Laboratory, Stockholm University), paper I. Stockholm: Jannes Snabbtryck Kuvertproffset HB; 2004. [Google Scholar]
- 6.Tuli SM. Tuberculosis of the spine: a historical review. Clin Orthop Relat Res. 2007;460:29–38. doi: 10.1097/BLO.0b013e318065b75e. [DOI] [PubMed] [Google Scholar]
- 7.Kappelman J, Alçiçek MC, Kazanci N, Schultz M, Ozkul M, Sen S. First Homo erectus from Turkey and implications for migrations into temperate Eurasia. Am J Phys Anthropol. 2008;135(1):110–116. doi: 10.1002/ajpa.20739. [DOI] [PubMed] [Google Scholar]
- 8.Hershkovitz I, Donoghue HD, Minnikin DE, Besra GS, Lee OY, Gernaey AM, Galili E, Eshed V, Greenblatt CL, Lemma E, Bar-Gal GK, Spigelman M. Detection and molecular characterization of 9,000-year-old Mycobacterium tuberculosis from a Neolithic settlement in the Eastern Mediterranean. PLoS One. 2008;3(10):e3426–e3426. doi: 10.1371/journal.pone.0003426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin JN, Lai CH, Chen YH, Lee SS, Tsai SS, Huang CK, Chung HC, Liang SH, Lin HH. Risk factors for extrapulmonary tuberculosis compared to pulmonary tuberculosis. Int J Tuberc Lung Dis. 2009;13(5):620–625. [PubMed] [Google Scholar]
- 10.Peto HM, Pratt RH, Harrington TA, LoBue PA, Armstrong LR. Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006. Clin Infect Dis. 2009;49(9):1350–1357. doi: 10.1086/605559. [DOI] [PubMed] [Google Scholar]
- 11.De Backer, Vanhoenacker FM, Sanghvi DA. Imaging features of extraaxial musculoskeletal tuberculosis. Indian J Radiol Imaging. 2009;19(3):176–186. doi: 10.4103/0971-3026.54873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shrestha OP, Sitoula P, Hosalkar HS, Banskota AK, Spiegel DA. Bone and joint tuberculosis. University of Pennsylvania Orthopaedic Journal. 2010;20:23–28. [Google Scholar]
- 13.Santos FC, Nascimento AL, Lira LA, Lima JF, Montenegro Rde, Montenegro LM, Schindler HC. Bone tuberculosis: a case report on child. Rev Soc Bras Med Trop. 2013;46(2):249–251. doi: 10.1590/0037-8682-0010-2012. [DOI] [PubMed] [Google Scholar]
- 14.Ansari S, Amanullah MF, Ahmad K, Rauniyar RK. Pott’s spine: diagnostic imaging modalities and technology advancements. N Am J Med Sci. 2013;5(7):404–411. doi: 10.4103/1947-2714.115775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rajasekaran S. The problem of deformity in spinal tuberculosis. Clin Orthop Relat Res. 2002;398:85–92. doi: 10.1097/00003086-200205000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Jain AK1, Dhammi IK, Jain S, Mishra P. Kyphosis in spinal tuberculosis-Prevention and correction. Indian J Orthop. 2010;44(2):127–136. doi: 10.4103/0019-5413.61893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheung WY, Luk KD. Clinical and radiological outcomes after conservative treatment of TB spondylitis: is the 15 years’ follow-up in the MRC study long enough. Eur Spine J. 2013;22(Suppl 4):594–602. doi: 10.1007/s00586-012-2332-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sankaran-Kutty M. Atypical tuberculous spondylitis. Int Orthop. 1992;16(1):69–74. doi: 10.1007/BF00182990. [DOI] [PubMed] [Google Scholar]
- 19.Yu Y, Wang X, Du B, Yuan W, Ni B, Chen D. Isolated atypical spinal tuberculosis mistaken for neoplasia: case report and literature review. Eur Spine J. 2013;22(Suppl 3):S302–305. doi: 10.1007/s00586-012-2294-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ramanathan VD, Jawahar MS, Paramasivan CN, Rajaram K, Chandrasekar K, Kumar V, Palanimurugan K, Prabhakar R. A histological spectrum of host responses in tuberculous lymphadenitis. Indian J Med Res. 1999;109:212–220. [PubMed] [Google Scholar]
- 21.Sankaran B. Tuberculosis of Bones & Joints. Ind J Tub. 1993;40:109–118. [Google Scholar]
- 22.Bukharie HA, Al-Rubaish AM, Al-Zahrani A, Sadat-Ali M. Osteoarticular tuberculosis: how often is it missed. Southeast Asian J Trop Med Public Health. 2009;40(4):770–775. [PubMed] [Google Scholar]
- 23.Thampy S, Kishore S. An epidemiological study of skeletal tuberculosis. J Med Sci Clin Res. 2017;5(2):17536–17543. [Google Scholar]
- 24.Jutte PC, van Loenhout-Rooyackers, Borgdorff MW, van Horn. Increase of bone and joint tuberculosis in The Netherlands. J Bone Joint Surg. 2004;86(6):901–904. doi: 10.1302/0301-620x.86b6.14844. [DOI] [PubMed] [Google Scholar]
- 25.Mateo L, Ruiz Manzano, Olivé A, Manterola JM, Pérez R, Tena X, Prats M. Osteoarticular tuberculosis. Study of 53 cases. Med Clin (Barc) 2007;129(13):506–509. doi: 10.1157/13111371. [DOI] [PubMed] [Google Scholar]
- 26.Turgut M. Spinal tuberculosis (Pott’s disease): its clinical presentation, surgical management, and outcome. A survey study on 694 patients. Neurosurg Rev. 2001;24(1):8–13. doi: 10.1007/pl00011973. [DOI] [PubMed] [Google Scholar]
- 27.Sharma V, Anjum R, Choudhary V, Singh TP. Epidemiological pattern of osteoarticular tuberculosis in a teaching hospital of rural India: a prospective study. Int J Biomed Res. 2016;7(5):273–275. [Google Scholar]
- 28.Talbot JC, Bismil Q, Saralaya D, Newton DAG, Frizzel RM, Shaw DL. Musculoskeletal tuberculosis in Bradford - a 6-year review. Ann R Coll Surg Engl. 2007;89(4):405–409. doi: 10.1308/003588407X183328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mariconda M, Cozzolino A, Attingenti P, Cozzolino F, Milano C. Osteoarticular tuberculosis in a developed country. J Infect. 2007;54(4):375–380. doi: 10.1016/j.jinf.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Houshian S, Poulsen S, Riegels-Nielsen P. Bone and joint tuberculosis in Denmark: increase due to immigration. Acta Orthop Scand. 2000;71(3):312–315. doi: 10.1080/000164700317411942. [DOI] [PubMed] [Google Scholar]
- 31.Sandher DS, Al-Jibury M, Paton RW, Ormerod LP. Bone and joint tuberculosis: cases in Blackburn between 1988 and 2005. J Bone Joint Surg Br. 2007;89(10):1379–1381. doi: 10.1302/0301-620X.89B10.18943. [DOI] [PubMed] [Google Scholar]
- 32.Davies PD, Humphries MJ, Byfield SP, Nunn AJ, Darbyshire JH, Citron KM, Fox W. Bone and joint tuberculosis. A survey of notifications in England and Wales. J Bone Joint Surg Br. 1984;66(3):326–330. doi: 10.1302/0301-620X.66B3.6427232. [DOI] [PubMed] [Google Scholar]
- 33.Enache SD, Plesea IE, Anusca D, Zaharia B, Pop OT. Osteo-articular tuberculosis - a ten years case review. Rom J Morphol Embryol. 2005;46(1):67–72. [PubMed] [Google Scholar]
- 34.Huplea V, Stoica A, Ciobanu O, Calin G, Sterfârta A, Marin C, Plesea RM, Popescu MR, Plesea lE. Osteoarticular tuberculosis-an attempt of assessing of the main clinical morphological aspects. Curr Health Sci J. 2014;40(Suppl 14):42–50. [Google Scholar]
- 35.Dharmalingam M. Tuberculosis of the spine-the Sabah experience. Epidemiology, treatment and results. Tuberculosis. 2004;84:24–28. doi: 10.1016/j.tube.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 36.Sharifi-Mood B, Metanat M, Parsi M. Pott's disease: One of the most common manifestation of extrapulmonary tuberculosis in the Southeast of Iran. J Med Sci (Pakistan) 2006;6:674–677. [Google Scholar]
- 37.Pertuiset E, Beaudreuil J, Lioté F, Horusitzky A, Kemiche F, Richette P, Clerc-Wyel D, Cerf-Payrastre I, Dorfmann H, Glowinski J, Crouzet J, Bardin T, Meyer O, Dryll A, Ziza JM, Kahn MF, Kuntz D. Spinal tuberculosis in adults. A study of 103 cases in a developed country, 1980-1994. Med (Balt) 1999;78:309–320. doi: 10.1097/00005792-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 38.Park DW, Sohn JW, Kim EH, Cho DI, Lee JH, Kim KT, Ha KY, Jeon CH, Shim DM, Lee JS, Lee JB, Chun BC, Kim MJ. Outcome and management of spinal tuberculosis according to the severity of disease: a retrospective study of 137 adult patients at Korean teaching hospitals. Spine (Phila Pa 1976) 2007;32(4):E130–E135. doi: 10.1097/01.brs.0000255216.54085.21. [DOI] [PubMed] [Google Scholar]
- 39.Tasova Y, Sarpel T, Inal AS, Saltoglu N, Guzel R, Kurtaran B. A clinical review of 40 cases with tuberculous spondylitis in adults. Neurosurg Q. 2006;16:169–176. [Google Scholar]
- 40.Godlwana L, Gounden P, Ngubo P, Nsibande T, Nyawo K, Puckree T. Incidence and profile of spinal tuberculosis in patients at the only public hospital admitting such patients in KwaZulu-Natal. Spinal Cord. 2008;46:372–374. doi: 10.1038/sj.sc.3102150. [DOI] [PubMed] [Google Scholar]
- 41.Kim CJ, Song KH, Jeon JH, Park WB, Park SW, Kim HB, Oh MD, Choe KW, Kim NJ. A comparative study of pyogenic and tuberculous spondylodiscitis. Spine (Phila Pa 1976) 2010;35(21):E1096–E1100. doi: 10.1097/BRS.0b013e3181e04dd3. [DOI] [PubMed] [Google Scholar]
- 42.Solagberu BA, Ayorinde RO. Tuberculosis of the spine in Ilorin, Nigeria. East Afr Med J. 2001;78:197–199. doi: 10.4314/eamj.v78i4.9062. [DOI] [PubMed] [Google Scholar]
- 43.Sakho Y, Badiane SB, N'Dao AK, N'Diaye A, Gueye M, N'Diaye IP. Pott's disease in Senegal. Eur J Orthop Surg Traumatol. 2003;13:13–20. [Google Scholar]
- 44.Owolabi LF, Nagoda MM, Samaila AA, Aliyu I. Spinal tuberculosis in adults: A study of 87 cases in Northwestern Nigeria. Neurology Asia. 2010;15:239–244. [Google Scholar]
- 45.Alothman A, Memish ZA, Awada A, Al-Mahmood S, Al-Sadoon S, Rahman MM, Khan MY. Tuberculous spondylitis: analysis of 69 cases from Saudi Arabia. Spine (Phila Pa 1976) 2001;26:E565–E570. doi: 10.1097/00007632-200112150-00020. [DOI] [PubMed] [Google Scholar]
- 46.Rodriguez-Gomez M, Willisch A, Fernandez-Dominguez L, Lopez-Barros G, Garcia-Porrua C, Gonzalez-Gay MA. Luberculous spondylitis: epidemiologic and clinical study in non-HIV patients from northwest Spain. Clin Exp Rheumatol. 2002;20:327–333. [PubMed] [Google Scholar]
- 47.Maeda Y, Izawa K, Nabeshima T, Yonenobu K. Tuberculous spondylitis in elderly Japanese patients. J Orthop Sci. 2008;13:16–20. doi: 10.1007/s00776-007-1197-z. [DOI] [PubMed] [Google Scholar]
- 48.Mwachaka PM, Ranketi SS, Nchafatso OG, Kasyoka BM, Kiboi JG. Spinal tuberculosis among human immunodeficiency virus-negative patients in a Kenyan tertiary hospital: a 5-year synopsis. Spine J. 2011;11(4):265–269. doi: 10.1016/j.spinee.2011.01.033. [DOI] [PubMed] [Google Scholar]
- 49.Popescu MR, Plesea IE, Olaru M, Strâmbu IR, Fronie AI, Petrescu IO, Petrescu F, Stefâr?a A, Postolache P, Popescu M. Morphological aspects in tuberculosis of oral cavity-our experience and a review of the literature attempt. Rom J Morphol Embryol. 2015;56(3):967–987. [PubMed] [Google Scholar]
- 50.Popescu MR, Calin G, Strâmbu I, Olaru M, Balasoiu M, Huplea V, Zdrancota C, Plesea RM, Enache SD, Plesea IE. Lymph node tuberculosis-an attempt of clinico-morphological study and review of the literature. Rom J Morphol Embryol. 2014;55(2 Suppl):553–567. [PubMed] [Google Scholar]
- 51.Su SH, Tsai WC, Lin CY, Lin WR, Chen TC, Lu PL, Huang PM, Tsai JR, Wang YL, Feng MC, Wang TP, Chen YH. Clinical features and outcomes of spinal tuberculosis in southern Taiwan. J Microbiol Immunol Infect. 2010;43(4):291–300. doi: 10.1016/S1684-1182(10)60046-1. [DOI] [PubMed] [Google Scholar]
- 52.Colmenero JD, Jiménez-Mejías ME, Reguera JM, Palomino-Nicás J, Ruiz-Mesa JD, Márquez-Rivas J, Lozano A, Pachón J. Tuberculous vertebral osteomyelitis in the new millennium: still a diagnostic and therapeutic challenge. Eur J Clin Microbiol Infect Dis. 2004;23(6):477–483. doi: 10.1007/s10096-004-1148-y. [DOI] [PubMed] [Google Scholar]
- 53.Weng CY, Chi CY, Shih PJ, Ho CM, Lin PC, Chou CH, Wang JH, Ho MW. Spinal tuberculosis in non-HIV-infected patients: 10 year experience of a medical center in central Taiwan. J Microbiol Immunol Infect. 2010;43(6):464–469. doi: 10.1016/S1684-1182(10)60072-2. [DOI] [PubMed] [Google Scholar]
- 54.Alavi SM, Sharifi M. Tuberculous spondylitis: risk factors and clinical/paraclinical aspects in the south west of Iran. J Infect Public Health. 2010;3(4):196–200. doi: 10.1016/j.jiph.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 55.Mulleman D, Mammou S, Griffoul I, Avimadje A, Goupille P, Valat JP. Characteristics of patients with spinal tuberculosis in a French teaching hospital. Joint Bone Spine. 2006;73(4):424–427. doi: 10.1016/j.jbspin.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 56.Khorvash F, Javadi AA, Izadi M, Jonaidi Jafari, Ranjbar R. Spinal tuberculosis: a major public health hazard in Isfahan. Pak J Biol Sci. 2007;10(19):3400–3404. doi: 10.3923/pjbs.2007.3400.3404. [DOI] [PubMed] [Google Scholar]
- 57.Rasit AH, Razak M, Ting FS. The pattern of spinal tuberculosis in Sarawak General Hospital. Med J Malaysia. 2001;56(2):143–150. [PubMed] [Google Scholar]
- 58.Schlesinger N, Lardizabal A, Rao J, Rao J, McDonald R. Tuberculosis of the spine: experience in an inner city hospital. J Clin Rheumatol. 2005;11(1):17–20. doi: 10.1097/01.rhu.0000152144.91206.0c. [DOI] [PubMed] [Google Scholar]
- 59.Barrière V, Gepner P, Bricaire F, Blétry O, Caumes E. Current aspects of spinal tuberculosis: apropos of 16 case reports] Ann Med Interne (Paris) 1999;150(5):363–369. [PubMed] [Google Scholar]