Abstract
The purpose of this study was to examine factors that influence physical activity among residents in assisted living. This was a secondary data analysis using baseline data from a function-focused care intervention study including 171 residents from 4 assisted living facilities. Using structural equation modeling, we found that mood, satisfaction with staff and activities, and social support for exercise were directly associated with time spent in physical activity. Gender, cognition, depression, and comorbidities were indirectly associated with physical activity and accounted for 13% of the total variance in physical activity. Implications for future research and social work practice are presented.
Keywords: Assisted living, environment, physical activity, residential care, satisfaction
In recent decades, assisted living (AL) has become the fastest growing residential care setting for older adults in the United States (Park, Zimmerman, Kinslow, Shin, & Roff, 2012). AL is broadly defined as a residential care setting that provides personal care services, 24-hour assistance, and social and health-related services for older adults (National Center for Assisted Living, 2015). There are no state requirements for employing social workers within AL facilities, although social workers in these settings help in the transition to the AL setting and for ongoing psychological counseling for long-term adjustment and optimization of quality of life. When working with older adults to help place them in appropriate settings of care social workers must understand that, unlike nursing homes that provide skilled nursing services with strict regulations in regard to medical oversight and management, AL provides some health services but is primarily designed to support residents and maximize their autonomy and independence. Based on the 2010 National Survey of Residential Care Facilities, more than 730,000 adults in the United States are living in AL or residential care (Park-Lee et al., 2011) and this number is expected to dramatically increase with the growth of the older population (Grabowski, Stevenson, & Cornell, 2012; Spetz, Trupin, Bates, & Coffman, 2015). One of the key challenges in providing care for residents in AL is maintaining their levels of physical activity and functional ability over time. Physical activity is defined as any body movement that works your muscles and requires more energy than resting. Walking, running, dancing, swimming, yoga, bathing, dressing, and gardening are a few examples of physical activity.
Evidence suggests that increased levels of physical activity in this population can help prevent falls (Cameron, Murray, Gillespie, Robertson, Hill, Cumming, & Kerse, 2010; McMahon et al., 2016), reduce symptoms of depression (Harvey, Chastin, & Skelton, 2015; Park, Han, & Kang, 2014; Williams & Tappen, 2008) and maintain cognitive and functional abilities (Hatch & Lusardi, 2010). In addition, older adults who engage in regular physical activity are more likely to remain in AL and avoid transitions to higher levels of care, such as nursing homes (Tighe et al., 2008).
Despite the benefits associated with physical activity, most older adults do not meet the recommended guidelines of 30 minutes of moderate physical activity per day (DHHS, 2008; Nelson et al., 2007). In fact, residents in AL spend the majority of their time engaged in sedentary behaviors with very low levels of moderate-to-vigorous physical activity (Hall & McAuley, 2011; Resnick, Galik, Gruber-Baldini, & Zimmerman, 2010a; Wyrick, Parker, Grabowski, Feuling, & Ng, 2008). The explanation for this limited activity among residents in long-term care is complex, involving resident characteristics such as their personal determination and motivation to engage in physical activity, their health status and associated comorbidities, type and amount of social support and relationships with individuals in the facility as well as family and friends, and the culture, policies and physical environment of the facility (e.g., are residents allowed to use wheelchairs in the dining room). Unfortunately, older adults in AL are at increased risk for inadequate social support due to declines in physical health and other risk factors, such as depression, cognitive impairment, and limited mobility (Winningham & Pike, 2007). Having a better understanding of the factors that influence physical activity levels among residents can help social workers in these settings to encourage residents to optimize the time they spend in physical activity. For example, social workers can provide motivational interventions, help residents’ access assistive devices and thereby assure that the environment is appropriate, and/or work with families to partner with care staff in encouraging residents to participate in bathing and dressing as this is the best way for them to improve their health and quality of life.
Factors related to physical activity among al residents
To organize the many factors that influence physical activity among residents in AL, it is helpful to use a social ecological model. The social ecological model incorporates intrapersonal factors, interpersonal factors, the environment, and policy-related issues. Intrapersonal factors influencing physical activity among residents include age, gender, education, and marital status (Lin, Yeh, Chen, & Huang, 2010). Those who are older, female, and less educated are less likely to engage in physical activity (Chen, Li, & Yen, 2015; Lin et al., 2010). Likewise, physical health such as the number of comorbid-ities and actual diagnoses (e.g., arthritis) and mental health, specifically whether or not the individual has symptoms of depression, influence physical activity levels among residents (Chen et al., 2015; Victor et al., 2016; Yuh-Min, 2010). Some research suggests that other intrapersonal factors, such as resilience and self-efficacy, could be mediating the relationship between health status and physical activity (Benjamin, Edwards, Ploeg, & Legault, 2014; Hall & McAuley, 2011; Resnick & D’Adamo, 2011).
Interpersonal factors that influence physical activity include resident-to-resident social interactions through participation in activities as well as perceived social support from staff and family members. Examples of meaningful social relationships to help residents engage in physical activity include such things as having one resident encourage another resident to participate in an exercise class, having a staff member encourage and help a resident walk or self-propel to the dining room for meals, or having a family member go for a walk with a resident during a visit versus just sitting in the room with the resident. These types of interactions can contribute to a greater quality of life with improved physical health and psychological well-being for residents (Horowitz & Vanner, 2010; Perkins, Ball, Kemp, & Hollingsworth, 2013; Street & Burge, 2012). Social support and encouragement from staff and family have the potential to improve engagement in physical and social activities among residents in long-term care settings (Benjamin et al., 2014; Victor et al., 2016). More research is needed to explore how social relation-ships with facility staff, family members, or other residents serve to foster or impede residents’ levels of physical activity in AL settings.
Residents in AL have identified that positive social interactions and participation in activities influence their satisfaction with the environment (Park et al., 2012; Resnick, Galik, Gruber-Baldini, & Zimmerman, 2010b). The physical environment in AL (e.g., physical space, amenities, sense of community) can influence the type and amount of physical activity performed by the residents. The influence of the physical environment is particularly true for individuals at advanced ages (Greenfield, 2012; Lawton, 1977). Barriers in the environment, such as lack of designated areas for exercise, limited exercise equipment, dim internal lighting of the building, and uneven surfaces, can create impediments to physical activity for residents (Benjamin et al., 2014; Kalinowski et al., 2012). Other environmental concerns such as uneven surfaces and a lack of suitable outdoor walking paths can make it challenging for residents to utilize outside areas for activity purposes (Benjamin et al., 2014; Chen, 2010). Moreover, environments that afford opportunities for residents to engage in physical and social activities can contribute to improved satisfaction and preserved functional abilities (Horowitz & Vanner, 2010; Resnick, Galik, Gruber-Baldini, & Zimmerman, 2011).
In addition to the physical environment, there is a social and psychological dimension to the environment involving relationships with others (Engel et al., 2016). Psychological well-being and social engagement of residents can also influence physical activity (Street & Burge, 2012; van Dyck, Teychenne, McNaughton, De Bourdeaudhuij, & Salmon, 2015; Wood-Nartker, Guerin, & Beuschel, 2014; Yang & Stark, 2010). Gaining a better understanding of the factors that influence physical activity among AL residents will help guide social workers in these settings via one-on-one work or in working as a member of the healthcare team to develop successful interventions that focus on increasing the time residents spend in physical activity. In doing so, the social worker will help improve residents’ health, well-being, and quality of life. Therefore, the purpose of this study was to test the impact of intrapersonal factors (age, gender, depression, comorbidities), interpersonal factors (support from staff to participate in physical activity, perceived relationships with staff), and environmental factors (resident perceptions of the physical environment and social activities provided) on the physical activity of residents in AL. Specifically, it was hypothesized that controlling for depression, cognition, comorbidities, and gender, residents who reported higher levels of satisfaction with their environment in terms of staff relationships and support, social activities, and the physical space would be more likely to engage in physical activity.
Methods
Design
This study examined baseline data from a randomized controlled trial, Testing the Impact of a Function-Focused Care (FFC) Intervention in AL (Table 1). FFC includes three components as part of the intervention all of which are implemented by a research nurse who works with an identified in-house function-focused care champion. This individual is most commonly a nurse, social worker, nursing assistant, or activities director. The FFC Intervention is designed to help residents engage in physical activity during all care interactions. Examples of FFC activities performed by residents include walking to the bathroom rather than using a commode chair, participating in bathing and dressing at their highest level, going to an exercise class, participating in a walk-to-dine program, and participating in recreational activities that have some degree of physical activity such as chair Tai Chi classes or Bingo games in which the resident walks to get his or her prize.
Table 1.
Components of the Function Focused Care for Assisted Living Intervention (FFC-AL).
| Components | Function-Focused Care Intervention |
|---|---|
| Component I: Evaluation of Intraindividual Factors | • Comprehensive baseline evaluation using an approved assessment for residents (e.g., Maryland Assisted Living Functional Assessment), the Person-Environment Fit assessment and input from social work and therapists and nursing staff as relevant. |
| • Training of a facility identified Function-Focused Care Coordinator to maintain function-focused care at the end of the study. | |
| • Evaluation and management of factors that influence function and physical activity such as anemia and vitamin D deficiency. | |
| Component II: Interpersonal Factors |
• Education of staff, residents, and families about the value of physical activity and how to integrate physical activity into all routine care activities. |
| • Self-efficacy-based motivational interventions for staff, residents, and families to motivate all to engage in function-focused care activities. | |
| • Self-efficacy-based motivational interventions for staff, residents, and families to motivate all to engage in function-focused care activities. | |
| • Development of short- and long-term goals with residents. | |
| • Development of long-term goals with residents written on a Goal Attainment Scale. | |
| • Evaluation of residents’ perspective of their social supports for physical activity. | |
| Component III: Environment and Policy Assessments | • Comprehensive evaluation of the indoor/outdoor environment to optimize function and physical activity of residents and make recommendations to changes. |
| • Review of facility policies and philosophies with facility owners/managers/staff to alter these to facilitate a focus on optimizing function and physical activity (don’t allow the use of wheelchairs in the dining room so all have to at least transfer to a dining room chair). |
The parent study was a 12-month study in which settings were randomized to the FFC Intervention in AL or the control intervention which involved education only and focused on teaching staff, families, and residents about the value of physical activity and how to incorporate it into routine daily activities. The study was reviewed and approved by a university-based Institutional Review Board. Residents were recruited from four AL facilities, two of which sites were stand-alone AL facilities that were owned and operated by the same company. One of the sites had 99-bed occupancy and the other 265 beds. The other two sites were owned and operated by a different company and were both part of continuing care retirement communities. One of these sites had 143 beds and the other 131 beds. All sites had in-house rehabilitation services and various activity programs typically found in AL settings (e.g., art, music). Reported staffing ratios were 12:1 within all sites.
Sample
The parent study included a sample of 171 residents, all of whom were included in the secondary analysis done in this study. Eligibility was based on being aged 65 years or older, currently living in the setting, and scoring at least 11 on the Mini-Mental State Examination (MMSE) (Folstein, Folstein, McHugh, 1975). Residents were excluded from the study if they were receiving hospice services. A five-item Evaluation to Sign Consent (ESC) questionnaire was used to guide the determination of residents’ capacity to provide consent to research (Resnick, Gruber-Baldini, Pretzer-Aboff, Galik, Custis Buie, Russ, & Zimmerman, 2007). The items assure that the resident is aware of what is involved with participating in the research, can state what to do if they no longer want to participate in the study, and can identify the risks associated with the study. If the resident did not pass the ESC, he or she was asked to assent to the study, and consent was obtained from the resident’s legally authorized representative.
A total of 494 residents were evaluated for participation in the study; of these, 123 (25%) were not eligible because they were deceased by the time they were approached (n = 14), in hospice (n = 8), in rehabilitation (n = 6), discharged from AL or in the hospital (n = 21), non-communicative (n = 64), or aged younger than 65 years (n = 10). One-hundred seventy-seven residents or proxies refused to consent (36%), and 185 residents consented (37%) to participate. Of the 185 consented residents, five (3%) were ineligible because they scored less than 11 on the MMSE. Nine (5%) individuals voluntarily withdrew after consenting and before collection of baseline data, leaving the final sample of 171 participants.
Measures
Descriptive information related to demographic characteristics (age, marital status, gender, race, education) and number of comorbidities was collected. Additional data were obtained related to the amount of time participants spent engaging in physical activity, psychosocial factors including depression and perceived social support, and residents’ satisfaction with the AL environment.
Physical activity
Data were collected on the amount of time residents spent actively engaging in physical activity using the Physical Activity Survey for Long-Term Care (PAS-LTC) (Resnick & Galik, 2007). The PAS-LTC includes all the physical activity commonly done in long-term care settings within six subscales: locomotion, personal care activities, structured exercise, recreational activities, caretaking activities, and repetitive behavior. Participants self-reported the amount of time they spend engaging in each of these activities on the day of testing. This information was then confirmed by the nursing assistant working with the resident on the day of testing. Prior testing supported evidence of interrater reliability of the PAS-LTC with intraclass correlations ranging from .83 to .94. There was some evidence of validity of the measure with significant correlations between PAS-LTC recorded during the evening and night shifts and the number of counts of activity per the ActiGraph (r = .60 and r = .57, p < .05 respectively) and the kcals estimated (r = .58 and r = .60, p < .05, respectively). Although not significant, the PAS-LTC completed during the day shift and total activity based on the PAS-LTC showed correlations of .40 or greater with the ActiGraph activity counts and kcals. Lastly, in prior use, the PAS-LTC was well received by the nursing assistants and easily completed.
Mood
Mood was measured using the 5-item Geriatric Depression Scale (GDS) (Hoyl et al., 1999). Participants were asked to respond either negatively or affirmatively to statements that describe symptoms of depression based on their experience in the previous week. A score of two or greater on the GDS is considered to be indicative of probable depression. The 5-item GDS has been used in numerous research studies with older adults in long-term care settings and is short and easy for them to complete. Prior testing supported internal consistency with an alpha coefficient and validity of the instrument based on comparisons with clinical definitions of depression (Hoyl et al., 1999).
Social support for exercise
Residents’ social support for exercise was evaluated using the revised Social Support for Exercise Scale (SSEHS) (Casado, Resnick, Zimmerman, Nahm, Orwig, Macmillan, & Magaziner, 2009). Social support around exercise is critical from a motivational perspective for residents. Participants were asked about their perception of support from friends, family, and experts (i.e., staff) to engage in exercise and physical activity. A list of 10 statements related to support for exercise were presented to participants (e.g., provides reminders and encouragement to exercise, helps plan exercise-related activities, offers to exercise with you), and they were asked to indicate whether such support was provided by friends, family, and/or experts. Prior use of the SSEHS in the older population provided evidence of internal consistency and construct validity based on a significant difference in social support for exercise between those who were versus were not exposed to the intervention (Casado et al., 2009).
Satisfaction with assisted living environment
Participants were asked to report their levels of satisfaction with AL using the Resident Satisfaction Index (RSI) (Sikorska-Simmons, 2001). This measure was selected as it focused specifically on the resident’s satisfaction with their living situation (i.e., the AL setting). The RSI includes five subscales that represent residents’ perceptions of health care, housekeeping services, physical environment (e.g., lack of personal space, sense of community), relationships with staff (e.g., are staff kind and caring), and physical and social activities (e.g., satisfaction with the activities offered, opportunities to participate in interesting activities). Because this study was focused on environmental factors that influenced physical activity, housekeeping services (e.g., quality of cleaning, staff cleaning skills, and facility maintenance) were not included because they were not deemed relevant to this topic. Prior research (Sikorska-Simmons, 2001) supported internal consistency (Cronbach’s alpha overall of .92; subscales .77–.86) and validity based on factor analysis and significant correlations with psychological well-being.
Data analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) software program, version 17.0. Descriptive statistics including means, proportions, and ranges were used to describe the sample. To explore the factors that influence physical activity among residents in AL, structural equation modeling was used to test the proposed model. Specifically, it was hypothesized that controlling for depression, cognition, comorbidities, and gender, residents who reported higher levels of satisfaction with their environment would be more likely to engage in physical activity.
Model testing was done using structural equation modeling and the AMOS statistical program (Arbuckle, 1997). The sample covariance matrix was used as input and a maximum likelihood solution sought. The chi-square statistic divided by degrees of freedom and the Steigers Root Mean Square Error of Approximation (RMSEA) were used to estimate model fit. The larger the probability associated with the chi-square divided by degrees of freedom the better the fit of the model to the data. A ratio of ≤3 is considered to be a good fit (Bollen, 1989; Loehlin, 1998). The RMSEA is a population-based index and consequently is insensitive to sample size. A RMSEA of <0.10 is considered good, and <0.05 is very good. Path significance (i.e., significance of the Lambda values) was based on the Critical Ratio (CR), which is the parameter estimate divided by an estimate of the standard error. A CR >2 in absolute value was considered significant (Arbuckle, 1997). Significance for path estimates was set at p ≤ 0.05. Significant differences in model fit were based on significant change between the χ2 and degrees of freedom of each model.
Results
The average age of participants was 87.7 years old (SD = 5.7), and the majority of participants were female (n = 136, 80%) and Caucasian (n = 160, 94%) with a small percentage of African Americans (n = 8, 4.5%), one Asian, one Native American, and one undeclared individual (Table 2). Most participants were widowed (n = 136, 80%), with some individuals reported as married (n = 17, 10%), never married (n = 8, 5%), and divorced (n = 10, 6%). Participants had a mean MMSE score of 23.2 (SD = 4.9) and reported 13.4 (SD = 3.1) years of education. On average, participants reported engaging in 162.9 minutes (SD = 81.4) of physical activity per day and the majority of activity was related to personal care (101.5 minutes, SD = 51.9 or activities such as bathing, dressing, and grooming). The mean score on the GDS was 1.7 (SD = 1.3), with a score of two or greater considered to be indicative of depression (Hoyl et al., 1999). Finally, resident satisfaction averaged 17.4 (SD = 2.9) out of a possible 21 points on the RSI.
Table 2.
Participant demographics and characteristics (N = 171).
| Variable | Mean (SD) | n (%) |
|---|---|---|
| Age | 87.7 (5.7) | |
| Education (years) | 13.4 (3.1) | |
| Cognition (MMSE) | 23.2 (4.9) | |
| Total number of diagnoses | 7.6 (3.6) | |
| Female | 136 (80%) | |
| Caucasian | 160 (94%) | |
| African American | 8 (4.5%) | |
| Asian | 1 (.001%) | |
| Native Americans | 1 (.001%) | |
| Other | 1 (.001%) |
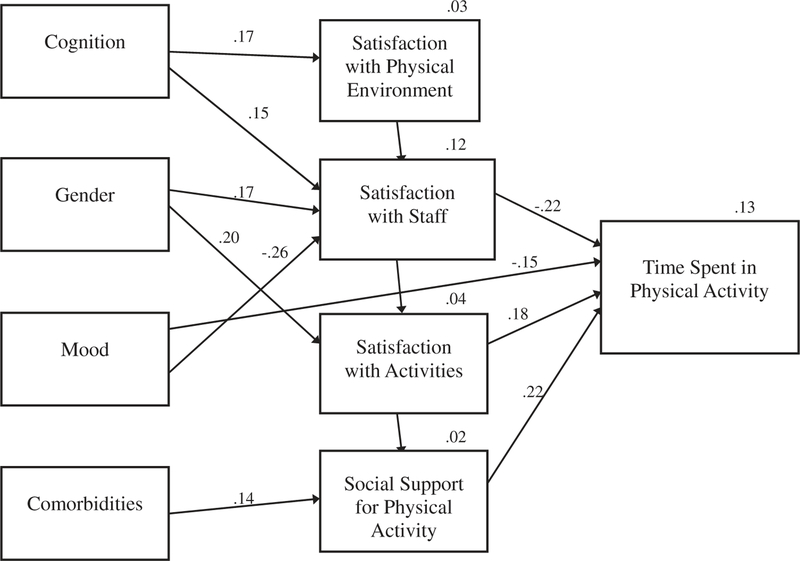
The full model tested 29 hypothesized paths. Of these, 10 were initially significant (Figure 1). The full model, however, did not fit with the data (χ2/df = 3.89, p = .001, RMSEA = .13). Testing of a revised model with nonsignificant paths removed resulted in a statistically significant improvement in the model fit (p ≤ 0.05). The revised model had a χ2/df ratio of 2.59 (p = .001) and a RMSEA of .097. Results of the revised model testing are shown in Table 3. Cognition, mood, and gender were associated with satisfaction with the physical environment and accounted for 3% of the variance in satisfaction with the physical environment. Similarly, cognition, mood, and gender were significantly associated with satisfaction with relationships with staff and accounted for 12% of the variance in satisfaction with relationships. Those that were more intact, less depressed, and female were more satisfied with the physical environment and social interactions with staff. Gender was associated with satisfaction with activities and accounted for 4% of the variance in satisfaction with social activities.
Figure 1.
Path analysis for model with significant paths only.
Table 3.
Model path estimates for significant paths only.
| Physical Activity |
||||
|---|---|---|---|---|
| Significant Model Paths | Path Estimate | p | ||
| Satisfaction with staff | ← | Gender | 0.167* | 0.033 |
| Satisfaction with activities | ← | Gender | 0.199* | 0.015 |
| Satisfaction with staff | ← | Mood | −0.260** | 0.001 |
| Satisfaction with physical environment | ← | Cognition | 0.173* | 0.039 |
| Total physical activity | ← | Satisfaction with staff | −0.224** | 0.005 |
| Total physical activity | ← | Satisfaction with activities | 0.176* | 0.024 |
| Total physical activity | ← | Social support for exercise | 0.216** | 0.003 |
Note: p < .05;
p < 0.01.
Depressive symptoms, satisfaction with relationships with staff, activities offered within the setting and social support from experts (i.e., staff) to exercise were all directly associated with total time in physical activity. Those that were less satisfied with staff relationships, more satisfied with activities, and had more social support from experts in the setting spent more time in physical activity. Gender, cognition, depression, and total number of comorbidities were indirectly associated with time spent in physical activity. Together all variables accounted for 13% of the total variance in physical activity.
Discussion
The results of this study contribute to an increased understanding of the factors that influence physical activity among residents in AL settings. The revised model with significant paths only had a good fit with the data and explained 13% of the total variance in physical activity levels. Although a number of factors directly or indirectly influence physical activity, such as satisfaction with staff and activities, social support from staff, mood, cogni-tion, and comorbidities, there was still a large percentage of variance in physical activity left unexplained. Interventions by social workers to augment the factors known to influence physical activity should be considered such as decreasing depression of the residents and exploring with residents their feelings about staff and activities offered. Other factors that might be considered in future research to more comprehensively explain physical activity include such things as the residents’ self-efficacy expectations related to physical activity, their fear of falling or injury when engaging in physical activity including functional tasks and additional organizational resources such as staffing levels (Benjamin et al., 2014; Chen, 2010; Resnick & D’Adamo, 2011).
Approximately half (47%) of the participants screened positively for depression. This is considerably higher than what is typically found in residential care settings, which ranges from 10 to 14% depending on the criteria used to identify depression (Boorsma et al., 2012; Watson, Zimmerman, Cohen, & Dominik, 2009). The direct and indirect associations between depression and physical activity found in this study were consistent with previous findings demonstrating an inverse relationship between depression and physical activity (Lee & Park, 2008; Salguero, MartínezGarcía, Molinero, & Márquez, 2011). Additionally, it has been shown that engaging in physical activity serves as a protective factor in depression among older adults (Lee, Lee, Brar, Rush, & Jolley, 2014; Rhyner & Watts, 2016). Social workers in AL settings have a major role in both direct counseling of residents with depression as well as trying to encourage resident involvement in activities that can decrease depression such as going to activities, engaging with family or doing life review projects (Kramer, 2013; Monahan, 2015). In addition, future research should continue to investigate interventions that target the treatment of depression through exercise-based programs that could support the improvement in physical activity in older adults and the ways in which social workers can help residents engage in physical activity.
Characteristics of the social environment, including social support from staff and residents’ satisfaction with social activities, were important predictors of physical activity among participants in this study. Social support has repeatedly been identified as a significant factor in residents’ health outcomes and life satisfaction (Benjamin et al., 2014; Resnick et al., 2010b; Victor et al., 2016). Prior research suggests that inadequate staffing at the organizational level and insufficient time available for staff to encourage residents’ engagement during their day are key barriers to physical activity (Baert, Gorus, Calleeuw, De Backer, & Bautmans, 2016; Benjamin et al., 2014). In addition, satisfaction with social activities was positively associated with the amount of time residents spend being physically active. These findings have clear implications for practice in residential care settings such that offering activities residents enjoy could encourage them to leave their own apartments and go to the site of the activity thereby increasing physical activity. Social programming and recreational activities (e.g., outings, classes, gardening, special events) should be tailored around the capacities and preferences of the residents to increase participation and provide opportunities for mean-ingful social interactions among residents (Park et al., 2012). In addition, providing activities that are enjoyable but also build in some physical activity may further increase the amount of time engaged in physical activity (e.g., Physical Activity Bingo). Some studies have noted the importance of activities designed to meet residents’ individualized, but more research should examine how social activities can contribute to the physical health and activity levels of residents. Investing in activities that are resident centered are particularly useful (Hanson et al., 2014; Horowitz & Vanner, 2010) and engaging residents in activities, particularly physically focused activities, that are relevant to them and they enjoy may help to prevent resident turnover and avoid adverse health outcomes associated with sedentary lifestyles. Social workers in these settings have a critical role in helping to identify residentcentered options for each resident.
Although social support from staff to participate in physical activity was directly related to time spent in physical activity, residents’ satisfaction with staff was negatively associated with their engagement in physical activity. It is possible that residents who are more satisfied with staff relationships were less likely to be physically active because they preferred spending time interacting one-on-one with staff in their rooms instead of doing such things as participating in physical activity programs within the setting or walking in the hallways or to the dining room or activity room to engage with others. Ongoing consideration of the relationships of residents with staff and the impact that this has on physical activity is needed, and opportunities exist to implement specialized training programs for staff to motivate residents to engage in physical activity on a daily basis. Specifically, it may be helpful to note if the individual staff member engages in physical activity him or herself and/or expresses negative or positive perspectives about physical activity.
Satisfaction with the physical environment in terms of lacking personal space, feeling at home in the setting or feeling that there was a sense of community, was not related to the physical activity of residents. The lack of a relationship may be due to limited variance in that the residents were generally positive about the overall setting environment. A more specific focus on how the environment might influence physical activity and examining policies that are designed to enhance physical activity of residents, such as having easy access to outside walking paths or an exercise room, is needed to better evaluate the AL environment and impact on physical activity.
Cognition was the only factor associated with the individuals’ assessment of the physical environment such that persons with cognitive impairment were less satisfied with their environment. This may be because these residents were less inhibited in rating their satisfaction with the environment and therefore more likely to respond negatively in comparison with residents who were cognitively intact. Since it is estimated that 42% of AL residents have dementia and this number is expected to increase in the future (Caffrey et al., 2012), more focus on the needs and preferences of these residents as well as their ability to assess the environment should be examined. Prior research has shown that characteristics of the physical environment which promote resident dignity are associated with fewer neuropsychiatric symptoms and improved quality of life among residents with dementia (Bicket et al., 2010). Additional research should continue to explore how the physical environment influences the daily activities of residents, and environmental modifications that could have therapeutic benefits for residents with dementia should be the focus of future studies.
Limitations
This study was limited in that it only included a relatively small, homogenous sample of AL residents across four settings. Consequently, the findings are limited by sample selectivity and cannot be generalized to all AL residents. Further research is needed to confirm these findings in other geographic locations with a diverse population of residents. This study also only included baseline data collected at a single point in time and was therefore correlational in nature. In addition, the measures were all based on self-report from participants, and thus, the results may have been influenced by recall and social desirability.
Conclusion
This study supports the hypothesis that physical and social environments can play a role in residents’ engagement in physical activity. The findings from this study demonstrate the importance of examining physical activity from a multidimensional perspective through the evaluation of intraindividual, interpersonal, and environmental factors. In addition, it strengthens evidence that staff-resident relationships are particularly important for maintaining the health and well-being of residents and should be the focus on future interventions in AL settings. Social workers in these settings are needed to help evaluate intraindividual factors such as depression and implement interventions to decrease depression and encourage physical activity, to help identify resident preferences with regard to physical activity (e.g., did they previously like to walk, bike, go shopping, play golf), implement interpersonal interactions to motivate residents to engage in physical activity, and help family and friends do likewise.
It is also important to consider that physical activity levels of residents may largely be dependent on the programs, exercise facilities, and staffing resources available to them at the organizational level, and less reflective of individuals’ physical or functional limitations. Social workers can work with other members of the healthcare team to identify programs and activities that are resident centered and will encourage participation. Lastly, further research examining characteristics of the built environment and organizational practices and policies that support physical activity in AL settings is needed.
Acknowledgments
This research was supported by Robert Wood Johnson Foundation through the Interdisciplinary Nursing Quality Research Initiative Grant Program.
Footnotes
Conflict of interest
The authors have no financial or personal conflicts with this paper.
References
- Arbuckle J (1997). Amos user’s guide, version 3.6. Chicago, IL: Small Waters Corporation. Baert V, Gorus E, Calleeuw K, De Backer W, & Bautmans I (2016). An administrator’s perspective on the organization of physical activity for older adults in long-term care facilities. Journal of the American Medical Directors Association, 17(1), 75–84. doi: 10.1016/j.jamda.2015.08.011 [DOI] [PubMed] [Google Scholar]
- Benjamin K, Edwards N, Ploeg J, & Legault F (2014). Barriers to physical activity and restorative care for residents in long-term care: A review of the literature. Journal of Aging & Physical Activity, 22(1), 154–165. doi: 10.1123/japa.2012-0139 [DOI] [PubMed] [Google Scholar]
- Bicket MC, Samus QM, McNabney M, Onyike CU, Mayer LS, Brandt J, & Rosenblatt A (2010). The physical environment influences neuropsychiatric symptoms and other outcomes in assisted living residents. International Journal of Geriatric Psychiatry, 25(10), 1044–1054. doi: 10.1002/gps.2460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA (1989). Structural equations with latent variables New York, NY: Wiley-Interscience. [Google Scholar]
- Boorsma M, Joling K, Dussel M, Ribbe M, Frijters D, van Marwijk HJ, & van Hout H (2012). The incidence of depression and its risk factors in Dutch nursing homes and residential care homes. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 20(11), 932–942. doi: 10.1097/JGP.0b013e31825d08ac [DOI] [PubMed] [Google Scholar]
- Caffrey C, Sengupta M, Park-Lee E, Moss A, Rosenoff E, & Harris-Kojetin L (2012). Residents living in residential care facilities: United States, 2010. NCHS Data Brief, 91,1–18. [PubMed] [Google Scholar]
- Cameron I, Murray G, Gillespie L, Robertson M, Hill K, Cumming R, & Kerse N (2010). Interventions for preventing falls in older people in nursing care facilities and hospitals. The Cochrane Library. [DOI] [PubMed]
- Casado B, Resnick B, Zimmerman S, Nahm E, Orwig D, Macmillan K, & Magaziner J (2009). Social support for exercise by experts in older women post-hip fracture. Journal of Women & Aging, 21(1), 48–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Li Y, & Yen M (2015). Gender differences in the predictors of physical activity among assisted living residents. Journal of Nursing Scholarship, 47(3), 211–218. doi: 10.1111/jnu.2015.47.issue-3 [DOI] [PubMed] [Google Scholar]
- Chen YM (2010). Perceived barriers to physical activity among older adults residing in long-term care institutions. Journal of Clinical Nursing, 19(3–4), 432–439. [DOI] [PubMed] [Google Scholar]
- Engel L, Chudyk A, Ashe M, McKay H, Whitehurst D, & Bryan S (2016). Older adults’ quality of life: Exploring the role of the built environment and social cohesion in community-dwelling seniors on low income. Social Science & Medicine, 164(1), 1–11. doi: 10.1016/j.socscimed.2016.07.008 [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, & McHugh PR (1975). Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198. doi: 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- Grabowski DC, Stevenson DG, & Cornell PY (2012). Assisted living expansion and the market for nursing home care. Health Services Research, 47(6), 2296–2315. doi: 10.1111/hesr.2012.47.issue-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield EA (2012). Using ecological frameworks to advance a field of research, practice, and policy on aging-in-place initiatives. The Gerontologist, 52(1), 1. doi: 10.1093/geront/gnr108 [DOI] [PubMed] [Google Scholar]
- Hall KS, & McAuley E (2011). Examining indirect associations between physical activity, function, and disability in independent-and assisted-living residents. Journal of Physical Activity & Health, 8(5), 716–723. doi: 10.1123/jpah.8.5.716 [DOI] [PubMed] [Google Scholar]
- Hanson HM, Hoppmann CA, Condon K, Davis J, Feldman F, Friesen M, . . . Ashe, M. C (2014). Characterizing social and recreational programming in assisted living. Canadian Journal on Aging, 33(3), 285–295. doi: 10.1017/S0714980814000178 [DOI] [PubMed] [Google Scholar]
- Harvey JA, Chastin SF, & Skelton DA (2015). How sedentary are older people? A systematic review of the amount of sedentary behavior. Journal of Aging & Physical Activity, 23(3), 471–487. doi: 10.1123/japa.2014-0164 [DOI] [PubMed] [Google Scholar]
- Hatch J, & Lusardi MM (2010). Impact of participation in a wellness program on functional status and falls among aging adults in an assisted living setting. Journal of Geriatric Physical Therapy, 33(2), 71–77. [PubMed] [Google Scholar]
- Horowitz B, & Vanner E (2010). Relationships among active engagement in life activities and quality of life for assisted-living residents. Journal of Housing for the Elderly, 24(2), 130–150. doi: 10.1080/02763891003757056 [DOI] [Google Scholar]
- Hoyl MT, Alessi CA, Harker JO, Josephson KR, Pietruszka FM, Koelfgen M, & Rubenstein LZ (1999). Development and testing of a five-item version of the Geriatric Depression Scale. Journal of the American Geriatrics Society, 47(7), 873–878. doi: 10.1111/j.1532-5415.1999.tb03848.x [DOI] [PubMed] [Google Scholar]
- Kalinowski S, Wulff I, Kölzsch M, Kopke K, Kreutz R, & Dräger D (2012). Physical activity in nursing homes- barriers and facilitators: A cross-sectional study. Journal of Aging & Physical Activity, 20(4), 421. doi: 10.1123/japa.20.4.421 [DOI] [PubMed] [Google Scholar]
- Kramer BJ (2013). Social workers’ roles in addressing the complex end-of-life care needs of elders with advanced chronic disease. Journal of Social Work in End-Of-Life & Palliative Care, 9(4), 308–330. doi: 10.1080/15524256.2013.846887 [DOI] [PubMed] [Google Scholar]
- Lawton MP (1977). An ecological theory of aging applied to elderly housing. JAE, 31(1), 8. doi: 10.2307/1424527 [DOI] [Google Scholar]
- Lee H, Lee J, Brar JS, Rush EB, & Jolley CJ (2014). Physical activity and depressive symptoms in older adults. Geriatric Nursing, 35, 37–41. doi: 10.1016/j.gerinurse.2013.09.005 [DOI] [PubMed] [Google Scholar]
- Lee Y, & Park K (2008). Does physical activity moderate the association between depressive symptoms and disability in older adults? International Journal of Geriatric Psychiatry, 23 (3), 249–256. doi: 10.1002/(ISSN)1099-1166 [DOI] [PubMed] [Google Scholar]
- Lin YC, Yeh MC, Chen YM, & Huang LH (2010). Physical activity status and gender differences in community-dwelling older adults with chronic diseases. Journal of Nursing Research, 18(2), 88–97. doi: 10.1097/JNR.0b013e3181dda6d8 [DOI] [PubMed] [Google Scholar]
- Loehlin J (1998). Latent variable models. Mahwah, NJ: Lawrence Erlbaum Associates. McMahon SK, Wyman JF, Belyea MJ, Shearer N, Hekler EB, & Fleury J (2016). Combining motivational and physical intervention components to promote fall-reducing physical activity among community-dwelling older adults: A feasibility study. American Journal of Health Promotion, 30(8), 638–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monahan K (2015). The use of humor, jesting, and playfulness with traumatized elderly. Social Work in Mental Health, 13(1), 17–29. doi: 10.1080/15332985.2014.899943 [DOI] [Google Scholar]
- National Center for Assisted Living. (2015). What is assisted living? Retrieved from http://www.ahcancal.org/ncal/about/assistedliving/Pages/What-is-Assisted-Living.aspx
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, & Castaneda-Sceppa C (2007). Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Medicine & Science in Sports & Exercise, 39(8), 1435–1445. doi: 10.1249/mss.0b013e3180616aa2 [DOI] [PubMed] [Google Scholar]
- Park NS, Zimmerman S, Kinslow K, Shin HJ, & Roff LL (2012). Social engagement in assisted living and implications for practice. Journal of Applied Gerontology, 31(2), 215–238. doi: 10.1177/0733464810384480 [DOI] [Google Scholar]
- Park S, Han KS, & Kang C (2014). Effects of exercise programs on depressive symptoms, quality of life, and self-esteem in older people: A systematic review of randomized controlled trials. Applied Nursing Research, 27(4), 219–226. doi: 10.1016/j.apnr.2014.01.004 [DOI] [PubMed] [Google Scholar]
- Park-Lee E, Caffrey C, Sengupta M, Moss AJ, Rosenoff E, & Harris-Kojetin LD (2011). Residential care facilities: A key sector in the spectrum of long-term care providers in the United States. NCHS Data Brief, (78), 1. [PubMed] [Google Scholar]
- Perkins MM, Ball MM, Kemp CL, & Hollingsworth C (2013). Social relations and resident health in assisted living: An application of the convoy model. The Gerontologist, 53 (3), 495–507. doi: 10.1093/geront/gns124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Physical Activity Guidelines Advisory Committee. (2008). Physical activity guidelines advisory committee report, 2008 Washington, DC: US Department of Health and Human Services, A1–H14. [Google Scholar]
- Resnick B, & D’Adamo C (2011). Factors associated with exercise among older adults in a continuing care retirement community. Rehabilitation Nursing, 36(2), 47–53. [DOI] [PubMed] [Google Scholar]
- Resnick B, & Galik E (2007). The reliability and validity of the Physical Activity Survey in Long-Term Care. Journal of Aging & Physical Activity, 15(4), 439–458. [DOI] [PubMed] [Google Scholar]
- Resnick B, Galik E, Gruber-Baldini A, & Zimmerman S (2010a). Perceptions and performance of function and physical activity in assisted living communities. Journal of the American Medical Directors Association, 11(6), 406–414. [DOI] [PubMed] [Google Scholar]
- Resnick B, Galik E, Gruber-Baldini AL, & Zimmerman S (2010b). Satisfaction with assisted living: The unexplored role of physical activity. Geriatric Nursing, 31, 197–205. [DOI] [PubMed] [Google Scholar]
- Resnick B, Galik E, Gruber-Baldini A, & Zimmerman S (2011). Testing the effect of function-focused care in assisted living. Journal of the American Geriatrics Society, 59(12), 2233–2240. [DOI] [PubMed] [Google Scholar]
- Resnick B, Gruber-Baldini AL, Pretzer-Aboff I, Galik E, Custis Buie V, Russ K, & Zimmerman S (2007). Reliability and Validity of the Evaluation to Sign Consent Measure. The Gerontologist, 47(1), 69–77. [DOI] [PubMed] [Google Scholar]
- Rhyner KT, & Watts A (2016). Exercise and depressive symptoms in older adults: A systematic meta-analytic review. Journal of Aging & Physical Activity, 24(2), 234–246. doi: 10.1123/japa.2015-0146 [DOI] [PubMed] [Google Scholar]
- Salguero A, Martínez-García R, Molinero O, & Márquez S (2011). Physical activity, quality of life and symptoms of depression in community-dwelling and institutionalized older adults. Archives of Gerontology and Geriatrics, 53(2), 152–157. doi: 10.1016/j.archger.2010.10.005 [DOI] [PubMed] [Google Scholar]
- Sikorska-Simmons E (2001). Development of an instrument to measure resident satisfaction with assisted living. Journal of Applied Gerontology, 20(1), 57–73. doi: 10.1177/073346480102000104 [DOI] [Google Scholar]
- Spetz J, Trupin L, Bates T, & Coffman JM (2015). Future demand for long-term care workers will be influenced by demographic and utilization changes. Health Affairs, 34(6), 936–945. doi: 10.1377/hlthaff.2015.0005 [DOI] [PubMed] [Google Scholar]
- Street D, & Burge SW (2012). Residential context, social relationships, and subjective well- being in assisted living. Research on Aging, 34(3), 365–394. doi: 10.1177/0164027511423928 [DOI] [Google Scholar]
- Tighe SK, Leoutsakos J-MS, Carlson M, Onyike CU, Samus Q, & Baker A (2008). The association between activity participation and time to discharge in the assisted living setting. International Journal of Geriatric Psychiatry, 23, 586–591. doi: 10.1002/gps.1940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dyck D, Teychenne M, McNaughton SA, De Bourdeaudhuij I, & Salmon J (2015). Relationship of the perceived social and physical environment with mental health-related quality of life in middle-aged and older adults: Mediating effects of physical activity. PLoS One, 10(3), 1–16. doi: 10.1371/journal.pone.0120475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor CR, Rogers A, Woodcock A, Beighton C, Cook DG, Kerry SM, . . . Harris TJ (2016). What factors support older people to increase their physical activity levels? An exploratory analysis of the experiences of PACE-Lift trial participants. Archives of Gerontology and Geriatrics, 67, 1–6. doi: 10.1016/j.archger.2016.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson LC, Zimmerman S, Cohen LW, & Dominik R (2009). Practical depression screening in residential care/assisted living: Five methods compared with gold standard diagnoses. The American Journal of Geriatric Psychiatry, 17(7), 556–564. doi: 10.1097/JGP.0b013e31819b891c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams CL, & Tappen RM (2008). Exercise training for depressed older adults with Alzheimer’s disease. Aging & Mental Health, 12(1), 72–80. doi: 10.1080/13607860701529932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winningham R, & Pike N (2007). A cognitive intervention to enhance institutionalized older adults’ social support networks and decrease loneliness. Aging & Mental Health, 11 (6), 716–721. doi: 10.1080/13607860701366228 [DOI] [PubMed] [Google Scholar]
- Wood-Nartker J, Guerin DA, & Beuschel E (2014). Environmental cues: Their influence within assisted living facilities. Health Environments Research & Design Journal, 7(3), 120–143. doi: 10.1177/193758671400700309 [DOI] [PubMed] [Google Scholar]
- Wyrick S, Parker D, Grabowski D, Feuling H, & Ng A (2008). Relationships among walking aids, physical activity, depression, fatigue, and perceived health in assisted-living residents – A pilot study. Journal of Applied Gerontology, 27(4), 511–522. doi: 10.1177/0733464808315288 [DOI] [Google Scholar]
- Yang H, & Stark S (2010). The role of environmental features in social engagement among residents living in assisted living facilities. Journal of Housing for the Elderly, 24(1), 28–43. doi: 10.1080/02763890903547062 [DOI] [Google Scholar]
- Yuh-Min C (2010). Perceived barriers to physical activity among older adults residing in long-term care institutions. Journal of Clinical Nursing, 19(3), 432–439. doi: 10.1111/j.1365-2702.2009.02990.x [DOI] [PubMed] [Google Scholar]