Abstract
BACKGROUND:
Due to their high aesthetic outcome and long-term predictability, laminate veneers have become a common restorative procedure for anterior teeth. However, because of the variety in the preparation designs and the material types, the clinician faces a dilemma of which approach to use.
AIM:
To compare the survival rate of dental veneers according to different preparation designs and different material types. The sub-aim is to reach a favourable preparation design and material based on scientific evidence.
METHODS:
Comprehensive electronic search of the dental literature via PUBMED, MEDLINE and Scopus databases was performed using the following keywords: “porcelain veneers”, “composite veneers”, “all-ceramic veneers”, “success of porcelain veneers”, “preparation design”, “preparation geometry”, “patient’s satisfaction”. Additionally, references from the selected studies and reviews were searched for more information.
RESULTS:
Under the limitations of the available literature, the clinician preference is the decisive factor for choosing the preparation design. Nonetheless, incisal overlap preparation seems to have the most predictable outcome from all the preparation designs.
CONCLUSION:
Porcelain veneers show excellent aesthetic results and predictable longevity of the treatment, while composite veneers can be considered as a good conservative option, but with less durability.
Keywords: laminate veneers, anterior teeth, restorative procedure, survival rate of dental veneers
Introduction
Since 1930s dental veneers have been used to improve the aesthetic and protection of teeth (Calamia, 1988) [1], the indications of dental veneers include: 1) discoloured teeth due to many factors such as tetracycline staining, fluorosis, amelogenesis imperfect, age and others 2) restoring fractured and worn teeth 3) abnormal tooth morphology 4) correction of minor malposition 5) Intra-oral repair of fractured crown and bridge facings [2], [3], [4]. Unfavourable conditions of dental veneers include 1) patients with parafunctional habits such as bruxism 2) edge to edge relation 3) poor oral hygiene 4) insufficient enamel [5], [6]. Many studies reported positive clinical outcomes veneers, with a survival rate of 91% in 20 years [7] dental veneers are considered a predictable aesthetic correction of anterior teeth.
The materials of dental veneers have evolved remarkably, early materials that had been used had many disadvantages such as the materials needed to be too thick to cover any discolouration, difficulty to polish which can cause abrasion of the opposing dentition and easy to stain [8], [9]. Researchers and dental material manufacturers have aimed to develop new materials with better aesthetic characteristics through the years. In 1975 laminate veneers were introduced as a better material of choice to mask the dentition, the restorations were 1 mm in thickness and were made from a cross-linked polymeric veneer [10]. The use of laminate veneers resulted in a better aesthetic outcome and less chair time [11]. The progress of developing new materials reached porcelain in the 1980s when enamel was etched, and the porcelain surface was treated to improve the bonding [12], [13].
The desire for more durable aesthetic outcomes did not confine to improve the material type only; new preparation designs were introduced to the field of dental veneers. There are four different main designs of teeth preparation commonly mentioned in the literature (Figure 1): 1) window preparation: in which the incisal edge of the tooth is preserved 2) feather preparation: in which the incisal edge of the tooth is prepared Bucco-palatable, but the incisal length is not reduced 3) bevel preparation: in which the incisal edge of the tooth is prepared Bucco-palatable, and the length of the incisal edge is reduced slightly (0.5-1 mm) 4) incisal overlap preparation: in which the incisal edge of the tooth is prepared Bucco-palatable, and the length is reduced (about 2 mm), so the veneer is extended to the palatal aspect of the tooth [14], [15], [16], [17].
Figure 1.
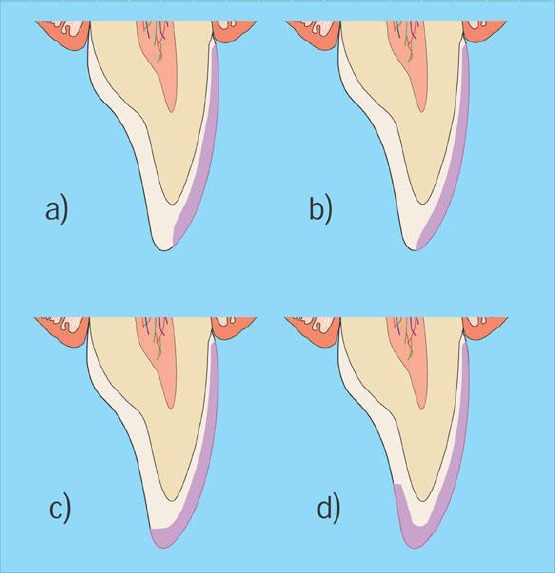
Showing common veneer preparations a) window b) feather c) bevel d) incisal overlap [17]
Influence of preparation design on the survival of dental veneers
Different opinions have been reported about superior preparation design over the others. In fact, due to the great variety in the materials, preparations designs and luting cement, favourable approaches to restore teeth with veneers have been controversial.
This review aims to compare the survival rate of dental veneers according to different preparation designs and different material types. The sub-aim is to reach a favourable preparation design and material based on scientific evidence.
One important aspect to investigate is the tooth preparation of dental veneers and how it might affect the fracture resistant of the material and reinforcement of the abutment tooth. Unfortunately, clinical trials that investigate the survival rate of dental veneers according to preparation designs are few, the criteria of investigation would include more than one factor which can affect the outcome of the treatment [16], [18]. In contrast, many in vitro studies have been conducted to evaluate the influence of different preparations design. Although such studies do not mimic the actual clinical environments and factors, they can provide criteria and guidelines for the clinician and further clinical investigations [5]. Table 1 illustrates the results of multiple in vitro studies regarding the influence of preparation design.
Table 1.
In vitro studies that investigated the influence of preparation design on dental veneers
| Study | Preparation design | Method of loading | Number of samples | Survival probability | Conclusion | Remarks |
|---|---|---|---|---|---|---|
| (Highton & Caputo 1987) [26] | Incisal overlap- chamfer FL Window preparation Slight labial preparation only Unprepared |
Four directions: Central vertical Distal vertical Central inclined Distal inclined |
4 (one of each) | High Moderate Low Lowest |
Labial, proximal, incisal and gingival reduction is recommended. | Samples were photoelastic teeth |
| (Castelnuovo et al. 2000) [14] | Incisal overlap (1mm)-chamfer finish line Butt joint incisal reduction (1mm) Feather edge preparation Deep incisal overlap(4mm) Unprepared |
Static loading at a 90-degree angle to the palatal surface of the sample | 50 (10 each) | Moderate High High Low Control |
Butt joint incisal reduction and feather edge prep. Provide the best retention to the restoration. Deep incisal overlap is not recommended | - |
| (Stappert et al. 2005) [16] | Incisal overlap (2mm) butt joint Deep incisal overlap (3mm)- butt joint Window preparation Unprepared |
Dynamic loading and thermal cycling 135-degree angle in the masticatory stimulator | 64 (16 each) | High Low Low Control |
Incisal overlap provides the best support. Deep preparation is not necessary. | - |
| (Zarone et al. 2005) [28] | Incisal overlap - chamfer FL Window preparation |
Static loading at the long axis of the tooth | 4 | High Low |
Incisal overlap is a better design than window prep. | Samples were 3D computerised models |
| (Schmidt et al. 2011) [31] | Incisal reduction – chamfer FL Incisal reduction – butt joint |
Static loading at a 90-degree angle to the palatal surface of the sample | 32 (8 each) | Low High |
Having a chamfer FL increase the failure rate of the veneer | Amount of existing tooth structure was considered in the study |
| (Lin et al. 2012) [23] | Incisal reduction – butt joint Three quarter preparation |
Static loading at a 125-degree angle of the palatal surface of the sample | 48 (12 each) | High Moderate |
Three-quarter prep. Requires stronger material for support | Influence of restorative materials was included in the study |
| (Alghazzawi et al. 2012) [32] | Incisal reduction – butt joint Three quarter preparation |
Dynamic loading at a 135-degree angle of the palatal surface of the sample | 60 (30 each) | High High |
No significant difference between the two preparations | - |
General concepts
Some features of the preparation design are highly recommended in the majority of the literature and lab studies. For example, restricting the preparation to enamel is considered to be a critical factor for a favourable bonding strength, thus more durable outcome [6], [18], [19], [20]. Additionally, preserving the interproximal contact is recommended in most of the literature and studies, this is due to preserving more enamel and tooth structure, allowing a positive seat for cementation in a conservative approach [16], [21], [22], [23]. However, the clinician might face certain situations where removing the interproximal contact can provide better aesthetic results such as malaligned teeth or diastema [24], [25]. Moreover, the amount of labial reduction concurrent at 0.4-0.7 mm for ceramic veneers [1], [3], [15]. This is due to the enamel thickness in the anterior teeth, according to Ferrari et al., (1991) [3], the enamel thickness of 114 extracted anterior teeth was 1.0 to 2.1 mm at the incisal third, 0.6 to 1.0 mm at the middle third and 0.3 to 0.5 at the gingival third, therefore, minimal preparation is advisable.
Preparation designs
Although there are different opinions and different results in studies that investigate the influence of preparation design on the survival of the restoration. It seems that incisal overlap preparation provides the best support for the restoration and distributes occlusal forces over a larger surface area. In the window preparation, the occlusal stress is highly concentrated on the incisal third which may lead to fracture of the restoration. Also, incisal translucency can be better achieved when the incisal edge is reduced [14], [16], [23], [26]. However, it is controversial whether it is favourable to add a chamfer finish line palatable or have a shoulder finish line (butt joint). Troedson and Dérand (1999) [27] and Zarone et al., (2005) [28] reported that it is required to have a chamfer finish line palatable for the restoration to tolerate the occlusal stress.
In contrast, Castelnuovo et al., (2000) [14] suggested that having a chamfer finish line doesn’t add to the longevity of the restoration.
Additionally, they reported that veneers with butt-joint finish line could provide more than one path of insertion (Figure 2). However, having a single path of insertion can be considered as an advantage because it prevents any displacement of the veneer during cementation. Eventually, the study stated that an overlap preparation with chamfer finish line does not decrease the longevity and predictability of the treatment.
Figure 2.
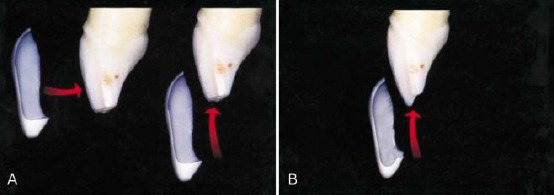
Incisal overlap with shoulder finish line (A) provide more than one path of insertion while incisal overlap with chamfer finish line (B) provide only one path of insertion (Castelnuovo et al., 2000) [14]
Ultimately, the biting force of the anterior teeth is considered to be low (100 – 200 N) (Carlsson 1973) [29] and with the absence of a strong well-conducted clinical study, the decision of preparation design is the clinician preference mainly, while incisal overlap can always be chosen to re-establish anterior guidance (Hahn et al., 2000) [30].
Influence of material type on the survival of dental veneers
A range of materials are available in the market to restore aesthetic/functional complications by the mean of veneering teeth; the most common material is porcelain, resin composite. Each material type has its unique composition, optical characteristics and fabrication process. Thus, it can be expected that the treatment outcome and longevity will differ according to the material used (Font et al. 2006) [33]. Table 2 shows multiple clinical studies that investigated the survival rate of dental veneers with a variety of material types.
Table 2.
Clinical studies are illustrating the survival rate of dental veneers. Adapted from Peumans et al., (2000) [18]
| Study | Type of study | Number of veneers (number of patients) | Observation period | Survival rate | Remarks |
|---|---|---|---|---|---|
| Porcelain laminate veneers (PLVs) | |||||
| (Peumans et al., 1998) [43] | Prospective | 87 (25 patients) | 5 years | 93% | - |
| (Meijering et al., 1998) [61] | Prospective | 263 (112 patients) | 2.5 years | 100% | - |
| (Dumfahrt & Schäffer 2000) [62] | Retrospective | 191 (72 patients) | 1 – 10 years | 91% in 10 years | Failure increase when PLVs are bonded to dentin |
| (Magne et al,. 2000) [63] | Prospective | 48 (16 patients) | 4.5 years | 100% | - |
| (Smales & Etemadi 2003) [48] | Retrospective | 110 (50 patients) | Up to 7 years | 95% | Compared two different preparation designs as well |
| (Chen et al., 2005) [64] | Retrospective | 546 (not mentioned) | 2.5 years | 99% | All patients had tetracycline staining |
| (Granell et al., 2010) [65] | Prospective | 323 (70 patients) | 3 – 11 years | 87% over 11 years | Failure increased with the presence of composites and bruxism |
| (Beier et al., 2011) [47] | Retrospective | 318 (84 patients) | Up to 20 years | 94% in 5 y. – 93% in 10 y. - 82% in 20 y. |
50% of the patient were diagnosed with bruxism |
| (Layton & Walton 2012) [7] | Prospective | 499 (155 patients) | Up to 21 years | 96% in 10 y. 91% in 20 y. |
Bonding to enamel is a critical factor for survival |
| Resin composites- direct and indirect (DC –IC) | |||||
| (Peumans et al., 1997) [59] | Prospective | 87 (23 patients) | 5 years | 89% | DC-Main failure due to wear |
| (Meijering et al., 1998) [61] | Prospective | 263 (112 patients) | 2.5 years | 90% for IC - 74% for DC |
Results for DC and IC |
| (Wolff et al., 2010) [54] | Retrospective | 327 (101 patients) | 5 years | 79% | Result for DC |
| (Gresnigt et al., 2012) [60] | Prospective | 96 (23 patients) | 3.4 years | 87% | Split mouth design- no difference between composite type- all DC |
Porcelain veneers
One of the most common materials that are used to fabricate laminate veneers is feldspathic porcelain (Figure 3).
Figure 3.

A case showing before and after the treatment with porcelain veneers (Nalbandian & Millar 2009) [38]
The main component of feldspathic porcelain is feldspar; a naturally occurring glass which contains silicon oxide, aluminium oxide, potassium oxide and sodium oxide (Layton & Walton 2012) [7]. Feldspathic porcelain has many advantages; the material is very thin so it can be almost translucent which result in an appearing natural restoration. Also, it requires minimal tooth preparation. Therefore enamel can be preserved. Moreover, it is possible to etch feldspathic porcelain with hydrofluoric acid which gives a great bonding strength to the remaining enamel (Calamia 1982, Nicholls 1988, Stacey 1993, Layton & Walton 2012) [7], [12], [34], [35]. Nevertheless, feldspathic porcelain has some disadvantages. The fabrication of feldspathic porcelain can be done by two methods: the refractory die technique and the platinum foil technique (Horn 1983, Plant & Thomas 1987, Clyde & Gilmour 1988) [13], [15], [36], these methods are technique sensitive and the fabricated veneer requires good care prior to bonding (Layton & Walton 2012) [7]. Additionally, masking heavy discoloured teeth can be difficult because the porcelain is very thin. Moreover, it was reported that etching the inner surface of the porcelain can cause micro-cracks which can lead to decrease the flexural strength of the porcelain and eventually fracture the veneer (Yen et al., 1993) [37].
New ceramic systems have been developed recently such as IPS e.max press from Ivoclar Vivadent ©, leucite is added to the glass matrix in order to increase the strength of the ceramic (Rasetto et al., 2001) [39], however, such new systems lack well-conducted clinical studies that investigate the success of using them as laminate veneers. Thus, future studies in this field are required.
Adhesion complex
The adhesion complex between porcelain, luting composite and enamel is considered to be a great advantage of porcelain veneers. It has been reported that the bonding strength of that complex is around 63 MPa while the bond between composite and enamel is about 31 MPa and between composite and porcelain alone is 33 MPa (Stacey 1993) [35]. Also, some in vitro studies suggest that extracted teeth that are restored with porcelain veneers have regained their original strength (Andreasen et al., 1992, Stokes & Hood 1993) [40], [41]. This can explain the low failure rate (0 – 5%) in clinical studies due to debonding of the porcelain veneer especially when parafunctional habits are missing, (Rucker et al. 1990, Kihn & Barnes 1998, Peumans et al., 1998) [42], [43], [44]. Respectively, some authors reported that when porcelain veneers are bonded to composite rather than enamel, porcelain veneers tend to have a higher failure rate (Dunne & Millar 1993, Shaini et al., 1997) [45], [46].
Longevity of porcelain veneers
Many studies investigated the longevity of porcelain veneers. Beier et al., (2011) [47] reported in a retrospective clinical study a survival rate of 94.4% after five years and 93.5% after ten years; they found the main reason for failure is a ceramic fracture. A randomised clinical trial done by Layton and Walton (2012) [7] showed similar results, with a survival rate of 96% after ten years and 91% after 20 years. Also, Smales and Etemadi (2003) [48] reported a survival rate of 95% for porcelain veneers throughout 7 years. It is essential to stress that these studies and others that reported high survival rate of porcelain veneers had a strict assessment of remaining enamel and bonding systems. As a result, careful, conservative preparation and optimum isolation during cementation are required to ensure predictable outcomes.
There are other studies which reported a lower survival rate for porcelain veneers. A retrospective study of 2,563 veneers in 1,177 patients done by Burke and Lucarotti (2009) [49] reported a survival rate of 53% over 10 years. The material type of the veneers was not reported. Moreover, the study evaluated veneers that were done by the general dental service, and thus, it is possible that preparations of teeth did not meet the criteria of specialists’ level. Another retrospective study was done by Shaini et al., (1997) [46] reported a survival rate of 47% in 7 years. The veneers were done by undergraduate students and staff member at Birmingham University in the United Kingdom. The study reported that over 90% of veneers were placed on unprepared teeth, this can be a reason for high failure rate as it is suggested that the bond to aprismatic enamel is much weaker than prepared enamel (Perdigão & Geraldeli 2003, Layton & Walton 2012) [7], [50].
The high survival rates that are reported by well-designed clinical studies suggest that feldspathic porcelain can act as a reliable and effective material to restore anterior teeth.
Resin composite
Resin-based composites are restorative materials that have mainly the following three compositions: 1) resin matrix 2) inorganic filler 3) coupling agent. The most commonly used monomer in the resin is Bis-GMA which has a higher molecular weight than methyl methacrylate resins. Therefore, the polymerisation shrinkage of Bis-GMA (7.5%) is significantly less than that of methyl methacrylate resins (22%). Wide range of fillers such as quartz have been added to composites through the years, the addition of fillers offers many advantages like: 1) reduction of the polymerisation shrinkage 2) reduction of coefficient thermal expansion of the monomer 3) improve mechanical characteristics 4) some metallic fillers such as barium provide better radiopacity. The bonding between the resin and the filler is achieved by the use of coupling agents i.e. salines, the most commonly one that is used in resin composite is γ-MPTS. Dental composites can be categorised according to the particle size of the filler traditional composites have a mean particle size of 10-20 µm, on the other hand, micro filled composites have a mean particle size of 0.02 µm. new generations of composites are introduced by the dental company through the years, aiming for better aesthetic and physical properties (Bonsor & Pearson 2012, Van Noort 2013) [51], [52].
It was thought once that composites in the anterior area would be replaced with porcelain veneers due to their success (Garber 1989) [53]. However, the aesthetic and physical properties of resin composite have improved remarkably lately. Thus, it has been used extensively in clinical practice (Wolff et al. 2010) [54]. The main advantage of composite veneer is that it can be used directly, resulting in less chair time with good initial aesthetic. Nonetheless, composite veneers are more prone to discolouration and wear (Wakiaga et al. 2004) [55]. Additionally, the clinician skill in placing, finishing and polishing the composite plays a major factor in the aesthetic outcome.
Composite veneers do not require heavy preparations. Therefore enamel can be preserved for good adhesion. It is documented that the bonding strength between etching porcelain and enamel is greater than resin composite and enamel (Lacy et al., 1988, Nicholls 1988, Lu et al., 1992) [34], [56], [57]. Correspondingly, it has been reported that composite veneers do not significantly restore the stiffness of the prepared tooth (Reeh & Ross 1994) [58]. Although composite veneers can be made indirectly in dental laboratories, the used composite is essentially the same one that is applied directly. Thus, it shares the same physical properties and limitations of direct composite restorations such as polymerisation shrinkage (Van Noort 2013) [52].
Longevity of composite veneers
The survival rate of composite veneers in many clinical studies is constant. Peumans et al. (1997) [59] placed 87 direct composite veneers for 23 patients; they reported a survival rate of 89% after 5 years. Wolff et al., (2010) [54] did a retrospective study on 327 direct composite veneers for 101 patients; the estimated survival rate was 80% after 5 years. A recent randomised control trial to compare two different types of composites reported a survival rate of 87% in over 3 years (Gresnigt et al., 2012) [60]. The use of resin composite to veneer the anterior teeth is justifiable; it is a fast procedure with the good aesthetic outcome and reasonable longevity (Figure 4).
Figure 4.

A case showing before and after treatment with direct composite veneers (Nalbandian & Millar 2009) [38]
Patients’ satisfaction
Generally, aesthetic satisfaction is a complex process as it is considered subjective [38], [61]. However, some factors may play an important role in patients’ satisfaction such as the durability of the final aesthetic outcome, the required amount of teeth preparation for the material type and the cost of the treatment.
Many clinical studies that evaluated the longevity of porcelain veneers have also considered patients’ satisfaction of the treatment, the range of satisfaction in these studies is 80-100 % [43], [44], [46]. Other studies have been conducted to evaluate patients’ satisfaction with different material types for veneers. Meijering et al., (1997) [67] compared patients’ response to three different types of veneers restorations after two years: feldspathic porcelain, direct composite and indirect composite. Porcelain veneers had the best response from patients (93%) followed by indirect composite veneers (82%) and lastly direct composite veneers (67%). In contrast, Nalbandian and Millar (2009) [38] found no statistical difference between patients’ response to composite veneers and porcelain veneers. These two studies might be subjected to bias, the degree of preoperative discolouration or malposition can affect the grade of transformation postoperatively, and thus, affect the response of the patient.
From the result of the previous studies, it can be concluded that porcelain veneers can provide a predictable aesthetic acceptance, while composite veneers can be the treatment of choice for patients who appreciate minimally invasive approaches.
Conclusion
The influence of preparation design and material type on the success of dental veneers is controversial. Usually, the clinician preference decides the preparation geometry. Nevertheless, veneers with incisal coverage seem to have better aesthetic and more predictable outcomes, while having a chamfer finish line palatable seems to be unnecessary and limiting the preparation to a butt-join finish line is more sensible. According to multiple clinical studies, porcelain veneers have excellent aesthetic results, the longevity of the treatment and patient’s satisfaction; the most critical factors to ensure a successful treatment are to obtain bonding to enamel and absence of parafunctional habits. Respectively, composite veneers provide good aesthetic outcome and patient’s satisfaction; however, due to its physical properties and to the bonding strength when compared to porcelain veneers, composite veneers tend to fail significantly faster than porcelain veneers. Further clinical trials are needed to evaluate different types of composites and new ceramic systems for longer observation time.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Calamia J. The etched porcelain veneer technique. The New York state dental journal. 1988;54(7):48. PMid:3050646. [PubMed] [Google Scholar]
- 2.RCSE. National Clinical Guidelines 1997. GTA, Editor. England. 1997 [Google Scholar]
- 3.Ferrari M, Patroni S, Balleri P. Measurement of enamel thickness in relation to reduction for etched laminate veneers. The International journal of periodontics & restorative dentistry. 1991;12(5):407–413. [PubMed] [Google Scholar]
- 4.Tjan AH, Dunn JR, Sanderson IR. Microleakage patterns of porcelain and castable ceramic laminate veneers. The Journal of prosthetic dentistry. 1989;61(3):276–282. doi: 10.1016/0022-3913(89)90127-3. https://doi.org/10.1016/0022-3913(89)90127-3. [DOI] [PubMed] [Google Scholar]
- 5.Hui K, et al. A comparative assessment of the strengths of porcelain veneers for incisor teeth dependent on their design characteristics. British dental journal. 1991;171(2):51–55. doi: 10.1038/sj.bdj.4807602. https://doi.org/10.1038/sj.bdj.4807602 PMid:1873094. [DOI] [PubMed] [Google Scholar]
- 6.Sheets CG, Taniguchi T. Advantages and limitations in the use of porcelain veneer restorations. The Journal of prosthetic dentistry. 1990;64(4):406–411. doi: 10.1016/0022-3913(90)90035-b. https://doi.org/10.1016/0022-3913(90)90035-B. [DOI] [PubMed] [Google Scholar]
- 7.Layton DM, Walton TR. The up to 21-year clinical outcome and survival of feldspathic porcelain veneers: accounting for clustering. The International journal of prosthodontics. 2012;25(6):604–612. PMid:23101040. [PubMed] [Google Scholar]
- 8.Johnson WW. Use of laminate veneers in pediatric dentistry: present status and future developments. Pediatr Dent. 1982;4(1):32–7. PMid:6757880. [PubMed] [Google Scholar]
- 9.McLaughlin G. Porcelain fused to tooth--a new esthetic and reconstructive modality. The Compendium of continuing education in dentistry. 1984;5(5):430–435. PMid:6388991. [PubMed] [Google Scholar]
- 10.Faunce F, Faunce A. The use of laminate veneers for restoration of fractured or discolored teeth. Texas dental journal. 1975;93(8):6–7. PMid:1065053. [PubMed] [Google Scholar]
- 11.Toh C, Setcos J, Weinstein A. Indirect dental laminate veneers—an overview. Journal of dentistry. 1987;15(3):117–124. doi: 10.1016/0300-5712(87)90067-4. https://doi.org/10.1016/0300-5712(87)90067-4. [DOI] [PubMed] [Google Scholar]
- 12.Calamia JR. Etched porcelain facial veneers: a new treatment modality based on scientific and clinical evidence. The New York journal of dentistry. 1982;53(6):255–259. [PubMed] [Google Scholar]
- 13.Horn H. A new lamination: porcelain bonded to enamel. The New York state dental journal. 1983;49(6):401. PMid:6350953. [PubMed] [Google Scholar]
- 14.Castelnuovo J, et al. Fracture load and mode of failure of ceramic veneers with different preparations. The Journal of prosthetic dentistry. 2000;83(2):171–180. doi: 10.1016/s0022-3913(00)80009-8. https://doi.org/10.1016/S0022-3913(00)80009-8. [DOI] [PubMed] [Google Scholar]
- 15.Clyde J, Gilmour A. Porcelain veneers: a preliminary review. British dental journal. 1988;164(1):9. doi: 10.1038/sj.bdj.4806328. https://doi.org/10.1038/sj.bdj.4806328 PMid:3276348. [DOI] [PubMed] [Google Scholar]
- 16.Stappert CF, et al. Longevity and failure load of ceramic veneers with different preparation designs after exposure to masticatory simulation. The Journal of prosthetic dentistry. 2005;94(2):132–139. doi: 10.1016/j.prosdent.2005.05.023. https://doi.org/10.1016/j.prosdent.2005.05.023 PMid:16046967. [DOI] [PubMed] [Google Scholar]
- 17.Walls A, Steele J, Wassell R. Crowns and other extra-coronal restorations: porcelain laminate veneers. British dental journal. 2002;193(2):73–82. doi: 10.1038/sj.bdj.4801489. https://doi.org/10.1038/sj.bdj.4801489 PMid:12199127. [DOI] [PubMed] [Google Scholar]
- 18.Peumans M, et al. Porcelain veneers: a review of the literature. Journal of dentistry. 2000;28(3):163–177. doi: 10.1016/s0300-5712(99)00066-4. https://doi.org/10.1016/S0300-5712(99)00066-4. [DOI] [PubMed] [Google Scholar]
- 19.Friedman M. Multiple potential of etched porcelain laminate veneers. The Journal of the American Dental Association. 1987;115:83E–87E. doi: 10.14219/jada.archive.1987.0317. https://doi.org/10.14219/jada.archive.1987.0317. [DOI] [PubMed] [Google Scholar]
- 20.Rufenacht CR, Berger RP. Fundamentals of esthetics. first ed. Quintessence Chicago; 1990. [Google Scholar]
- 21.Gilmour A, Stone D. Porcelain laminate veneers: a clinical success? Dental update. 1993;20(4):167–9. 171-3, PMid:8405617. [PubMed] [Google Scholar]
- 22.King DG. Methods and materials for porcelain veneers. Current opinion in cosmetic dentistry. 1994:45–50. [PubMed] [Google Scholar]
- 23.Lin T, et al. Fracture resistance and marginal discrepancy of porcelain laminate veneers influenced by preparation design and restorative material in vitro. Journal of dentistry. 2012;40(3):202–209. doi: 10.1016/j.jdent.2011.12.008. https://doi.org/10.1016/j.jdent.2011.12.008 PMid:22198195. [DOI] [PubMed] [Google Scholar]
- 24.Gribble A. Multiple diastema management: an interdisciplinary approach. Journal of Esthetic and Restorative Dentistry. 1994;6(3):97–102. doi: 10.1111/j.1708-8240.1994.tb00841.x. https://doi.org/10.1111/j.1708-8240.1994.tb00841.x. [DOI] [PubMed] [Google Scholar]
- 25.Rouse JS. Full veneer versus traditional veneer preparation: a discussion of interproximal extension. The Journal of prosthetic dentistry. 1997;78(6):545–549. doi: 10.1016/s0022-3913(97)70003-9. https://doi.org/10.1016/S0022-3913(97)70003-9. [DOI] [PubMed] [Google Scholar]
- 26.Highton R, Caputo AA. A photoelastic study of stresses on porcelain laminate preparations. The Journal of prosthetic dentistry. 1987;58(2):157–161. doi: 10.1016/0022-3913(87)90168-5. https://doi.org/10.1016/0022-3913(87)90168-5. [DOI] [PubMed] [Google Scholar]
- 27.Troedson M, Dérand T. Effect of margin design, cement polymerization, and angle of loading on stress in porcelain veneers. The Journal of prosthetic dentistry. 1999;82(5):518–524. doi: 10.1016/s0022-3913(99)70049-1. https://doi.org/10.1016/S0022-3913(99)70049-1. [DOI] [PubMed] [Google Scholar]
- 28.Zarone F, et al. Influence of tooth preparation design on the stress distribution in maxillary central incisors restored by means of alumina porcelain veneers: a 3D-finite element analysis. Dental materials. 2005;21(12):1178–1188. doi: 10.1016/j.dental.2005.02.014. https://doi.org/10.1016/j.dental.2005.02.014 PMid:16098574. [DOI] [PubMed] [Google Scholar]
- 29.Carlsson GE. Bite force and chewing efficiency. Frontiers of oral physiology. 1973;1:265–292. doi: 10.1159/000392726. https://doi.org/10.1159/000392726. [DOI] [PubMed] [Google Scholar]
- 30.Hahn P, Gustav M, Hellwig E. An in vitro assessment of the strength of porcelain veneers dependent on tooth preparation. Journal of oral rehabilitation. 2000;27(12):1024–1029. doi: 10.1046/j.1365-2842.2000.00640.x. https://doi.org/10.1046/j.1365-2842.2000.00640.x PMid:11251771. [DOI] [PubMed] [Google Scholar]
- 31.Schmidt KK, et al. Influence of preparation design and existing condition of tooth structure on load to failure of ceramic laminate veneers. The Journal of prosthetic dentistry. 2011;105(6):374–382. doi: 10.1016/S0022-3913(11)60077-2. https://doi.org/10.1016/S0022-3913(11)60077-2. [DOI] [PubMed] [Google Scholar]
- 32.Alghazzawi TF, et al. The failure load of CAD/CAM generated zirconia and glass-ceramic laminate veneers with different preparation designs. The Journal of prosthetic dentistry. 2012;108(6):386–393. doi: 10.1016/S0022-3913(12)60198-X. https://doi.org/10.1016/S0022-3913(12)60198-X. [DOI] [PubMed] [Google Scholar]
- 33.Font AF, et al. Choice of ceramic for use in treatments with porcelain laminate veneers. Med Oral Patol Oral Cir Bucal. 2006;11:E297–302. [PubMed] [Google Scholar]
- 34.Nicholls J. Tensile bond of resin cements to porcelain veneers. The Journal of prosthetic dentistry. 1988;60(4):443–447. doi: 10.1016/0022-3913(88)90245-4. https://doi.org/10.1016/0022-3913(88)90245-4. [DOI] [PubMed] [Google Scholar]
- 35.Stacey GD. A shear stress analysis of the bonding of porcelain veneers to enamel. The Journal of prosthetic dentistry. 1993;70(5):395–402. doi: 10.1016/0022-3913(93)90073-w. https://doi.org/10.1016/0022-3913(93)90073-W. [DOI] [PubMed] [Google Scholar]
- 36.Plant C, Thomas G. Porcelain facings: a simple clinical and laboratory method. British dental journal. 1987;163(7):231–234. doi: 10.1038/sj.bdj.4806249. https://doi.org/10.1038/sj.bdj.4806249 PMid:3314944. [DOI] [PubMed] [Google Scholar]
- 37.Yen T-W, Blackman RB, Baez RJ. Effect of acid etching on the flexural strength of a feldspathic porcelain and a castable glass ceramic. The Journal of prosthetic dentistry. 1993;70(3):224–233. doi: 10.1016/0022-3913(93)90056-t. https://doi.org/10.1016/0022-3913(93)90056-T. [DOI] [PubMed] [Google Scholar]
- 38.Nalbandian S, Millar B. The effect of veneers on cosmetic improvement. British Dental Journal. 2009;207(2):E3–E3. doi: 10.1038/sj.bdj.2009.609. https://doi.org/10.1038/sj.bdj.2009.609 PMid:19629085. [DOI] [PubMed] [Google Scholar]
- 39.Rasetto FH, Driscoll CF, Fraunhofer JA. Effect of light source and time on the polymerization of resin cement through ceramic veneers. Journal of Prosthodontics. 2001;10(3):133–139. doi: 10.1111/j.1532-849x.2001.00133.x. https://doi.org/10.1111/j.1532-849X.2001.00133.x PMid:11641840. [DOI] [PubMed] [Google Scholar]
- 40.Andreasen FM, et al. Treatment of crown fractured incisors with laminate veneer restorations. An experimental study. Dental Traumatology. 1992;8(1):30–35. doi: 10.1111/j.1600-9657.1992.tb00223.x. https://doi.org/10.1111/j.1600-9657.1992.tb00223.x. [DOI] [PubMed] [Google Scholar]
- 41.Stokes A, Hood J. Impact fracture characteristics of intact and crowned human central incisors. Journal of oral rehabilitation. 1993;20(1):89–95. doi: 10.1111/j.1365-2842.1993.tb01518.x. https://doi.org/10.1111/j.1365-2842.1993.tb01518.x PMid:8429427. [DOI] [PubMed] [Google Scholar]
- 42.Kihn PW, Barnes DM. The clinical longevity of porcelain veneers: a 48-month clinical evaluation. The Journal of the American Dental Association. 1998;129(6):747–752. doi: 10.14219/jada.archive.1998.0317. https://doi.org/10.14219/jada.archive.1998.0317. [DOI] [PubMed] [Google Scholar]
- 43.Peumans M, et al. Five-year clinical performance of porcelain veneers. Quintessence international (Berlin, Germany 1985) 1998;29(4):211–221. [PubMed] [Google Scholar]
- 44.Rucker LM, et al. Porcelain and resin veneers clinically evaluated:2-year results. The Journal of the American Dental Association. 1990;121(5):594–596. doi: 10.14219/jada.archive.1990.0225. https://doi.org/10.14219/jada.archive.1990.0225 PMid:2229737. [DOI] [PubMed] [Google Scholar]
- 45.Dunne S, Millar B. A longitudinal study of the clinical performance of porcelain veneers. British dental journal. 1993;175(9):317–321. doi: 10.1038/sj.bdj.4808314. https://doi.org/10.1038/sj.bdj.4808314 PMid:8251248. [DOI] [PubMed] [Google Scholar]
- 46.Shaini F, Shortall A, Marquis P. Clinical performance of porcelain laminate veneers. A retrospective evaluation over a period of 6.5 years. Journal of oral rehabilitation. 1997;24(8):553–559. doi: 10.1046/j.1365-2842.1997.00545.x. https://doi.org/10.1046/j.1365-2842.1997.00545.x PMid:9291247. [DOI] [PubMed] [Google Scholar]
- 47.Beier US, et al. Clinical performance of porcelain laminate veneers for up to 20 years. The International journal of prosthodontics. 2011;25(1):79–85. [PubMed] [Google Scholar]
- 48.Smales RJ, Etemadi S. Long-term survival of porcelain laminate veneers using two preparation designs: a retrospective study. The International journal of prosthodontics. 2003;17(3):323–326. [PubMed] [Google Scholar]
- 49.Burke F, Lucarotti P. Ten-year outcome of porcelain laminate veneers placed within the general dental services in England and Wales. Journal of dentistry. 2009;37(1):31–38. doi: 10.1016/j.jdent.2008.03.016. https://doi.org/10.1016/j.jdent.2008.03.016 PMid:18538912. [DOI] [PubMed] [Google Scholar]
- 50.Perdigão J, Geraldeli S. Bonding characteristics of self-etching adhesives to intact versus prepared enamel. Journal of Esthetic and Restorative Dentistry. 2003;15(1):32–41. doi: 10.1111/j.1708-8240.2003.tb00280.x. https://doi.org/10.1111/j.1708-8240.2003.tb00280.x PMid:12638771. [DOI] [PubMed] [Google Scholar]
- 51.Bonsor S, Pearson G. A Clinical Guide to Applied Dental Materials. 1st ed. Churchill Livingstone; 2012. [Google Scholar]
- 52.Van Noort R. Introduction to Dental Materials. 4th ed. Elsevier Health Sciences; 2013. [Google Scholar]
- 53.Garber D. Direct composite veneers versus etched porcelain laminate veneers. Dental clinics of North America. 1989;33(2):301–304. PMid:2656322. [PubMed] [Google Scholar]
- 54.Wolff D, et al. Recontouring teeth and closing diastemas with direct composite buildups: a clinical evaluation of survival and quality parameters. Journal of dentistry. 2010;38(12):1001–1009. doi: 10.1016/j.jdent.2010.08.017. https://doi.org/10.1016/j.jdent.2010.08.017 PMid:20826192. [DOI] [PubMed] [Google Scholar]
- 55.Wakiaga JM, et al. Direct versus indirect veneer restorations for intrinsic dental stains. The Cochrane Library. 2004 doi: 10.1002/14651858.CD004347.pub2. https://doi.org/10.1002/14651858.CD004347.pub2. [DOI] [PubMed] [Google Scholar]
- 56.Lacy AM, et al. Effect of porcelain surface treatment on the bond to composite. The Journal of prosthetic dentistry. 1988;60(3):288–291. doi: 10.1016/0022-3913(88)90270-3. https://doi.org/10.1016/0022-3913(88)90270-3. [DOI] [PubMed] [Google Scholar]
- 57.Lu R, et al. An investigation of the composite resin/porcelain interface. Australian dental journal. 1992;37(1):12–19. doi: 10.1111/j.1834-7819.1992.tb00827.x. https://doi.org/10.1111/j.1834-7819.1992.tb00827.x PMid:1567289. [DOI] [PubMed] [Google Scholar]
- 58.Reeh ES, Ross GK. Tooth stiffness with composite veneers: a strain gauge and finite element evaluation. Dental Materials. 1994;10(4):247–252. doi: 10.1016/0109-5641(94)90069-8. https://doi.org/10.1016/0109-5641(94)90069-8. [DOI] [PubMed] [Google Scholar]
- 59.Peumans M, et al. The 5-year clinical performance of direct composite additions to correct tooth form and position. Clinical oral investigations. 1997;1(1):12–18. doi: 10.1007/s007840050003. https://doi.org/10.1007/s007840050003 PMid:9552812. [DOI] [PubMed] [Google Scholar]
- 60.Gresnigt MM, Kalk W, Özcan M. Randomized controlled split-mouth clinical trial of direct laminate veneers with two micro-hybrid resin composites. Journal of dentistry. 2012;40(9):766–775. doi: 10.1016/j.jdent.2012.05.010. https://doi.org/10.1016/j.jdent.2012.05.010 PMid:22664565. [DOI] [PubMed] [Google Scholar]
- 61.Meijering A, et al. Survival of three types of veneer restorations in a clinical trial: a 2.5-year interim evaluation. Journal of dentistry. 1998;26(7):563–568. doi: 10.1016/s0300-5712(97)00032-8. https://doi.org/10.1016/S0300-5712(97)00032-8. [DOI] [PubMed] [Google Scholar]
- 62.Dumfahrt H, Schäffer H. Porcelain laminate veneers. A retrospective evaluation after 1 to 10 years of service: Part II--Clinical results. The International journal of prosthodontics. 2000;13(1):9. PMid:11203615. [PubMed] [Google Scholar]
- 63.Magne P, et al. Clinical performance of novel-design porcelain veneers for the recovery of coronal volume and length. The International journal of periodontics & restorative dentistry. 2000;20(5):440–457. [PubMed] [Google Scholar]
- 64.Chen J-H, et al. Clinical evaluation of 546 tetracycline-stained teeth treated with porcelain laminate veneers. Journal of dentistry. 2005;33(1):3–8. doi: 10.1016/j.jdent.2004.06.008. https://doi.org/10.1016/j.jdent.2004.06.008 PMid:15652162. [DOI] [PubMed] [Google Scholar]
- 65.Granell R, et al. A clinical longitudinal study 323 porcelain laminate veneers. Period of study from 3 to 11 years. Population. 2010;3:12. doi: 10.4317/medoral.15.e531. [DOI] [PubMed] [Google Scholar]
- 66.Christensen GJ, Christensen RP. Clinical Observations of Porcelain Veneers: A Three-Year Report. Journal of Esthetic and Restorative Dentistry. 1991;3(5):174–179. doi: 10.1111/j.1708-8240.1991.tb00994.x. https://doi.org/10.1111/j.1708-8240.1991.tb00994.x. [DOI] [PubMed] [Google Scholar]
- 67.Meijering A, et al. Patients'satisfaction with different types of veneer restorations. Journal of dentistry. 1997;25(6):493–497. doi: 10.1016/s0300-5712(96)00067-x. https://doi.org/10.1016/S0300-5712(96)00067-X. [DOI] [PubMed] [Google Scholar]


