Abstract
AIM:
To measure the level of Systemic Lupus Erythematosus awareness among visitors in PHC at KAMC and to explores the factors which influence the Systemic Lupus Erythematosus awareness.
METHODS:
The study was a cross-sectional study conducted between February and September 2018 in four primary health care centers belong to King Abdulaziz Medical City. The study participants were male and female adult visitors to the centers` age from 18 to 60 years of age. The sample size was 400 participants. The participants were enrolled via a random convenience sampling method. Study data was collected using a self-administered questionnaire. Analytic statistics were done using the Chi-square (χ2) test for associations and/or the difference between two categorical variables. A P-value ≤ 0.05 was considered statistically significant.
RESULTS:
The awareness about Systemic Lupus Erythematosus among male and female was not statistically significant as (P = 0.304), but there was a statistically significant difference according to education level. Visitors with high school education are aware of Systemic Lupus Erythematosus than those with a lower level of education (Primary & Middle school) who are not aware of the Systemic Lupus Erythematosus by (P = 0.023).
CONCLUSION:
The study shows that this survey is valuable and beneficial to the community as it helps people to assess their knowledge about Systemic Lupus Erythematosus and become aware of this disease, as well as awareness of Systemic Lupus Erythematosus should be promoted among the community.
Keywords: Systemic Lupus Erythematosus, Awareness, Health promotion, Rheumatology
Introduction
Systemic lupus erythematosus (SLE) is a chronic inflammatory autoimmune disease that occurs when the immune system assaults the tissues of the body and its organs. Systemic means that SLE can affect the body’s various organs, including the skin, joints, brain, blood cells, kidneys, lungs, and heart. Lupus refers to the butterfly rash on the patient’s face, which is similar to the whitish outline marking on the middle of wolves’ faces. Erythematosus means the rash is reddish to purplish in color. Accordingly, four types of lupus can be identified: systemic lupus erythematosus, neonatal lupus, drug-induced lupus, and cutaneous lupus erythematosus. However, lupus erythematosus is the most common classification [1], [2].
The epidemiological studies was estimated that the prevalence of SLE was 241 per 100,000 people in North America which is the highest and the lowest incidence was 0.3 per 100,000 person yearly noticed in South Africa which is the lowest. SLE affected more women than men for all age and ethnic groups. Women of reproductive age (15-45) are often affected, and the rate of females to males is 9 to 1 [1], [2], [3].
Likewise, scientists trust that human genetic studies will structure our understanding of the premise of individual hereditary vulnerability to SLE. These studies will help to detect the person who will have a high probability of having SLE in the future [1].
Treatment of SLE will help to control disease progression and inhibit further complications. However, at the moment, there is no definitive medication or drug for treating SLE. SLE is usually very active when diagnosed for the first time. At this stage, high doses of drugs like glucocorticoids may be required to restrain the disease’s progression and stop organ harm, and this is the cornerstone of the treatment. However, despite advanced treatment SLE-associated infection and renal failure still increase mortality and this remains a major burden in management plans for patients [5], [6].
Addressing patient worries and fears about drug therapy, including treatment costs, side effects, and complications can increase the treatment adherence, fulfillment, and enhanced wellbeing results alongside psychological and behavioral interventions, which can be effective for decreasing weariness as well as enhancing strength in patients with SLE. Social help can assist patients with SLE accomplish positive thinking and a feeling of becoming stronger.
Despite numerous advances in the diagnosis and treatment of SLE and associated comorbid conditions, such as loss of physical, social, and emotional functioning, this disease remains a source of significant morbidity and mortality. Indeed, even with the expected changes in general mortality over the last five decades, a patient diagnosed at 20 years of age still has a one in six chance of dying by the age of 35 and a higher probability of a shortened lifespan; in addition, SLE has a severe and pervasive influence on patients’ self-esteem, resulting in emotional challenges, fear of rejection, stigmatization, social isolation, and loss of independence [8], [9].
On the other hand, there are some studies that stress the importance of raising awareness and educating the public about SLE by clarifying the nature of the disease, its direct causes, treatment methods, and control mechanisms; for example, awareness activities directed to both the overall society and health care workers in particular can advise them to reduce delays in diagnosis and ensure early transfer to specialist care.
In Riyadh, Saudi Arabia a study conducted in 2015 among students at King Saud University showed that the level of awareness about SLE among students is low. Workshops or campaigns are required to enhance awareness and correct misunderstandings [10].
In Taif, Saudi Arabia a study undertaken in 2017 that involved many of the Kingdom’s regions reported a high prevalence of less than optimal awareness and knowledge of SLE among the Saudi adult population [11].
In India, a study (2017) among the general population to assess their SLE awareness and knowledge found that the majority of participants had insufficient knowledge of its status as a rare disease that occurs in the population [12].
A 2018 study conducted among students at King Faisal University in Al-Hassa, Saudi Arabia found that most students have low awareness and some misunderstandings regarding SLE. Awareness programs are presumed able to increase awareness about SLE, as these campaigns have confirmed that greater public awareness may be useful in managing and controlling the disease and its associated complications [13].
Along with awareness activity, qualitative research is thought to be able to elicit patient knowledge and viewpoints, such as patients’ philosophies, misconceptions about the disease, and perceptions about new therapy or interventions, including monoclonal antibodies (mAb) therapy or immuno-suppression medications [7].
The main aim of the study is to evaluate the awareness of SLE among patients to primary health care clinics at King Abdulaziz Medical City (KAMC) in Riyadh and highlight the factors that influence SLE awareness, health promotion, information needed, and educational support.
Methods
The study was a cross-sectional study conducted between February and September 2018 in four primary health care centers belonging to KAMC: the Health Care Specialty Center (HCSC); King Abdulaziz Housing Clinics (Iskan); the National Guard Comprehensive Specialized Clinic (NGCSC), and King Abdulaziz Housing Clinics (Dirab).
Each of the four centers delivers primary curative and preventive health services, and consists of walk-in services, a minor emergency room setting, and an appointment booking system for patients to obtain treatment and counseling for acute and chronic medical conditions. The study participants were male and female adult visitors to the centers aged between 18 and 60.
The sample size was calculated by the Openepi website. The population of the KAMC-PHC as per the latest report was found to be around 420,000 people in 2017. They were distributed as follows: 200,000 patients in the HCSC, 100,000 patients in the NGCSC, 70,000 patients in King Abdulaziz Housing Clinics (Dirab), and 50,000 patients in King Abdulaziz Housing Clinics, (Iskan). Using a 95% confidence interval and 5% margin of error, the calculated minimum sample size was expected to be 384, which was modified to 400 to compensate for incomplete questionnaires.
The proportion of participants from each of the four centers was based on the clinic catchment area as follows: HCSC serves a population of around 200,000 people, thus accounts for approximately 47.6% of the sample size, equal to 190 participants; NGCSC serves around 100,000 people, accounting for approximately 23.8% of the sample size, equal to 95 participants; Dirab center serves around 70,000 people, accounting for approximately 16.6% of the sample size, equal to 67 participants; and Iskan serves around 50,000 people, accounting for approximately 11.9% of the sample size, equal to 48 participants.
Study data were collected using a self-administered questionnaire. The questionnaire used was developed by Sullivan [2], and was adopted by the researchers to meet the study main objectives after a literature review of similar studies.
The questionnaire was written in simple Arabic, and included the following sections: demographic data, and questions about knowledge, attitudes, and beliefs regarding SLE. Two research experts revised the questionnaire, and a pilot study was conducted with ten participants to confirm and verify the instrument’s validity.
The participants were enrolled via a random convenience sampling method. Patients to the four primary care centers were approached while sitting in the waiting area. The investigator explained the purpose of study to each participant and obtained verbal and documented consent to participate in the study before administering the questionnaire. All data were coded, entered, and analyzed using the Statistical Package for the Social Sciences, version 23 (SPSS 23). Continuous variables were reported in terms of means and standard deviation, while categorical variables were described using frequencies and percentages. Analytic statistics were performed using the chi-squared χ2) test for associations and/or the difference between two categorical variables. A P value of ≤ 0.05 was considered statistically significant.
Approval for the study was obtained from King Abdullah International Medical Research Center, the Ministry of the National Guard, Kingdom of Saudi Arabia. The participants were fully informed regarding voluntary participation, privacy, anonymity, and confidentiality of the data were ensured and the Declaration of Helsinki ethical rules were followed.
Results
Table 1 show that the majority of PHC patients included in the study were female (58.7%), while males made up 41.3% (Figure 1A).
Table 1.
Frequencies, distribution, and percentages of socio-demographic variables
| VARIABLES | NO | % |
|---|---|---|
| Sex | ||
| Male | 165 | 41.3 |
| Female | 235 | 58.7 |
| Age | ||
| Mean (SD) | 35.89 ± 12.04 | |
| Min age | 25 | |
| Max age | 66 | |
| Occupation | ||
| Student | 43 | 10.8 |
| Housewife | 91 | 22.8 |
| Government employee | 124 | 31.0 |
| Non-government employee | 50 | 12.4 |
| Unemployed | 72 | 18.0 |
| Retired | 20 | 5.0 |
| Education | ||
| Primary school | 18 | 4.5 |
| Middle school | 10 | 2.5 |
| High school | 190 | 47.5 |
| College | 23 | 5.8 |
| Graduated | 93 | 23.3 |
| Post-graduation studies | 21 | 5.3 |
| Can read and write name only | 16 | 4.0 |
| Non-literate | 29 | 7.3 |
| Marital status | ||
| Single | 131 | 32.8 |
| Married | 203 | 50.7 |
| Widowed | 22 | 5.5 |
| Divorced | 44 | 11.0 |
| No. of dependent family members | ||
| 0-1 | 169 | 42.3 |
| 2-3 | 62 | 15.4 |
| 4 | 35 | 8.8 |
| 5 | 31 | 7.8 |
| 6 | 56 | 14.0 |
| ≥ 7 | 47 | 11.7 |
Figure 1.
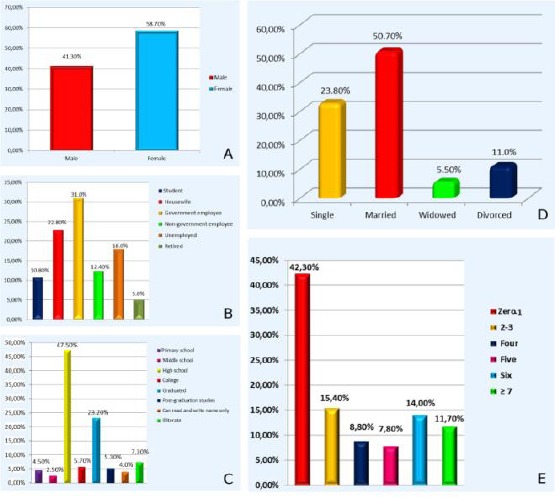
Distribution of visitors according to A) gender; B) occupation; C) education; D) marital status; E) number of dependents
The mean age of patients was 35.98 yrs. old (± 12.04) with most being government employees (31.0%), followed by housewives, the unemployed, non-government employees, students, and the retired at 22.8%, 18%, 12.4%, 10.8%, 5%, respectively (Figure 1B).
The majority of PHC patients (47.5%) included in the study had some high school; they were followed by graduates, the non-literate, college students, post-graduates, primary school, those able to read and write only their names, and those with middle school at 23.3%, 7.3%, 5.8%, 5.3%, 4.5%, 4%, and 2.5%, respectively (Figure 1C).
Most study participants were married (50.7%), while single, divorced, and widowed participants constituted 32.8%, 11%, and 5.5%, respectively (Figure 1D).
The majority of participants (42.3%) had no or only one dependent family member while those with 2–3, 4, 5, 6, or equal to or more than seven made up 15.4%, 8.8%, 7.8%, 14%, and 11.7% of the participants, respectively (Figure 1E).
As shown in Table 2, 56.8% of patients had heard the term “SLE.” The most common way participants recognized the disease was from the internet (online resources) (35.2%) as the majority of them had not been diagnosed with SLE (85.5%).
Table 2.
Awareness of systemic lupus erythematosus frequencies and percentages
| NO | Questions | N | % |
|---|---|---|---|
| 7 | Have you ever heard of the term “systemic lupus erythematosus”? | ||
| Yes | 227 | 56.8 | |
| No | 148 | 37.0 | |
| Don’t know | 25 | 6.50 | |
| 8 | Through which of the following sources did you hear about systemic lupus erythematosus? (You can choose more than one option) | ||
| Heard from a doctor | 31 | 13.7 | |
| Internet/online resources | 80 | 35.2 | |
| TV | 11 | 4.9 | |
| Radio | 14 | 6.2 | |
| Newspaper or magazines | 8 | 3.5 | |
| Friend or colleague | 65 | 28.6 | |
| Other (specify) ____________________________ | 18 | 7.9 | |
| 9 | Have you been diagnosed with systemic lupus erythematosus? | ||
| Yes | 58 | 14.5 | |
| No | 343 | 85.5 | |
| 10 | Do you know anyone who has systemic lupus erythematosus? | ||
| Family member | 44 | 11.0 | |
| Relatives | 62 | 15.5 | |
| Colleague | 46 | 11.5 | |
| No one | 246 | 61.5 | |
| Others (please specify) _________________________ | 2 | 0.5 | |
| 11 | Is systemic lupus erythematosus contagious? | ||
| Yes | 99 | 24.8 | |
| No | 108 | 27.0 | |
| Don’t know | 193 | 48.2 | |
| 12 | Is systemic lupus erythematosus fatal? | ||
| Yes | 141 | 35.3 | |
| No | 85 | 21.2 | |
| Don’t know | 174 | 43.5 | |
| 13 | Systemic lupus erythematosus is an autoimmune disease, which means: | ||
| There is no cause (the body fights itself) | 103 | 25.8 | |
| There are tumors | 64 | 16.0 | |
| It is hereditary | 119 | 29.8 | |
| Don’t know | 110 | 27.4 | |
| Other (please specify) __________________ | 4 | 1.0 | |
| 14 | Does systemic lupus erythematosus mostly affect females? | ||
| Yes | 156 | 39.0 | |
| No | 46 | 11.5 | |
| Don’t know | 198 | 49.5 | |
| 15 | Does systemic lupus erythematosus affect any organ/part in the body? | ||
| Yes | 174 | 43.5 | |
| No | 48 | 12.0 | |
| Don’t know | 178 | 44.5 | |
| 16 | What organs can be affected by systemic lupus erythematosus? (You can choose more than one option) | ||
| Kidney | |||
| Blood | 106 | 26.8 | |
| Heart | 29 | 7.3 | |
| Eyes | 23 | 5.8 | |
| Liver | 5 | 1.3 | |
| Skin | 47 | 11.8 | |
| Joints | 30 | 7.5 | |
| Lungs | 3 | 0.8 | |
| All of above | 64 | 16.0 | |
| Don’t know | 92 | 23.0 | |
| Others (Please specify) _______ | |||
| 17 | The following are symptoms of systemic lupus erythematosus. | ||
| Rash | 57 | 14.3 | |
| Alopecia | 42 | 10.5 | |
| Joint pain | 59 | 14.8 | |
| Hematuria | 9 | 2.3 | |
| Photosensitivity | 12 | 3.0 | |
| Don’t know | 114 | 28.5 | |
| All of the above | 107 | 26.8 | |
| 18 | Systemic lupus erythematosus can be diagnosed with a single blood test. | ||
| Yes | 139 | 34. 8 | |
| No | 95 | 23.7 | |
| Don’t know | 166 | 41.5 | |
| 19 | Systemic lupus erythematosus can be prevented. | ||
| Yes | 162 | 40.5 | |
| No | 79 | 19.7 | |
| Don’t know | 159 | 39.8 | |
| 20 | Systemic lupus erythematosus is a treatable disease. | ||
| Yes | 165 | 41.2 | |
| No | 83 | 20.8 | |
| Don’t know | 152 | 38.0 | |
| 21 |
Systemic lupus erythematosus is an illness with few complications. Yes No Don’t know |
157 82 161 |
39.2 20.6 40.2 |
| 22 | The treatment for of systemic lupus erythematosus is: | ||
| Chemotherapy | 104 | 26.0 | |
| Steroids | 73 | 18.2 | |
| Malaria medications | 77 | 19.3 | |
| Combination of above medications | 47 | 11.7 | |
| Others | 1 | 0.3 | |
| Don’t know | 98 | 24.5 | |
| 23 | Can lupus erythematosus disease affect the fertility of men and women? | 165 | 41.3 |
| Yes | 59 | 14.8 | |
| No | 176 | 44.0 | |
| Don’t know | |||
| 24 | Systemic lupus erythematosus causes fetal abnormalities or recurrent abortions in the affected mother. | ||
| Yes | 201 | 50.3 | |
| No | 52 | 13.0 | |
| Don’t know | 147 | 36.7 | |
| 25 | Should awareness of systemic lupus erythematosus be promoted? | ||
| Yes | 345 | 86.3 | |
| No | 9 | 2.3 | |
| Don’t know | 46 | 11.4 |
Most of the participants did not know anyone with SLE (61.5%) and the majority did not know that SLE is not contagious (48.2%) but could be fatal (43.5%). Most believed that SLE was a hereditary disease and classified SLE in this way (29.8%).
The majority did not know SLE mostly affects females (49.5%). They also did not know that SLE can affect any organs in the body (44.5%). Indeed 26.8% believed that only the kidney could be affected by systemic lupus erythematosus.
Most of the patients did not know the major symptoms of SLE (28.5%) and 41.5% did not know the main laboratory tests for SLE; 40.5% did not know whether SLE could be prevented although most believed that SLE is a treatable disease (41.2%).
The majority of participants did not know the complications of SLE (40.2%) and 26% believed that a treatment of SLE was chemotherapy. Most did not know that SLE can affect the fertility of men and women (44.0%), although they knew that SLE causes fetal abnormalities or recurrent abortions in the affected mother (50.3%).
Finally, the majority of participants believed that awareness of SLE should be promoted (86.3%); the score for awareness of SLE (n = 400) indicated that 64.7% of participant were unaware of SLE, while 35.3% were aware of SLE.
Table 3 shows the correlations between socio-demographic variables (gender, education, do you know anyone who has systemic lupus erythematosus?) and awareness of SLE. Awareness about SLE by gender was not statistically significant (P = 0.304), but there was a statistically significant difference according to education level. Participants with high school education were more aware than those with a lower level of education (primary and middle school) (P = 0.023).
Table 3.
Correlations between socio-demographic variables and awareness
| Socio-demographic variables | Awareness of systemic lupus erythematosus | χ2 | P value | |||
|---|---|---|---|---|---|---|
| Aware | Unaware | |||||
| No | % | No | % | |||
| Gender | 1.058 | 0.304 | ||||
| Male | 63 | 44.7 | 102 | 39.4 | ||
| Female | 58 | 54.9 | 157 | 60.6 | ||
| Education | 12 | 8.5 | 9.457 | 0.023* | ||
| Primary school | 28 | 19.9 | 31 | 12.0 | ||
| Middle school | 42 | 29.8 | 63 | 24.3 | ||
| High school | 21 | 14.9 | 82 | 31.7 | ||
| College | 28 | 19.9 | 29 | 11.2 | ||
| Graduated | 10 | 7.1 | 44 | 17.0 | ||
| Post-graduation studies | 0 | 0 | 10 | 309 | ||
| Can read and write name only | 0 | 0 | 0 | 0 | ||
| Illiterate | 0 | 0 | ||||
| Do you know anyone who has systemic lupus erythematosus? | 10.082 | 0.020* | ||||
| Family member | 16 | 11.3 | 28 | 10.8 | ||
| Relatives | 18 | 12.8 | 44 | 17.0 | ||
| Colleague | 15 | 10.6 | 31 | 12.0 | ||
| No one | 92 | 65.2 | 154 | 59.5 | ||
| Others (please specify) | 0 | 0 | 2 | 0.8 | ||
Furthermore, there was a statistically significant correlation between knowing a person with SLE and awareness (P = 0.020); this means that if the participants did not know a person with SLE before they will be unaware of SLE and its nature or manifestations.
Thus, the major factors that affect SLE knowledge and attitude are education level and knowing someone who have been diagnosed previously with SLE and is coping with it.
Discussion
The main aim of this study was to assess the awareness of the patients in the primary heath care of KAMC about SLE, its clinical manifestations, diagnosis, treatment, complications, and comorbidities as well as explore the possible factors that influence SLE awareness, such as adequate health promotion and clinical awareness-raising.
The study was carried out in four primary health care centers belonged to KAMC in Riyadh. The centers are the HCSC; King Abdulaziz Housing Clinics (Iskan); the NGCSC, and King Abdulaziz Housing Clinics (Dirab). As found in a similar local study [10], 40% have previously heard the term SLE. As well as the 2nd local study [13], 55.9% have previously heard the term SLE.
The 400 participants in this study were chosen from the waiting area in the clinics using random convenience sampling. The fact that females are more frequently reported having the disease than males. This is attributable to the fact that women are more expected to get SLE than males. Most of the participants were government employees (31.0%) and the majority had studied at high school; 50.7% of participants were married with/without dependent family members.
The study clarifies that 56.8% of participants had heard the term “systemic lupus erythematosus” and the most common way that they recognized the disease was through the internet (online resources).
The vast majority had not been diagnosed with SLE and did not know that SLE is not contagious and fatal. However, they believed that the kidney is the only organ that can be affected by SLE. As found in a similar local study11, more than 50% of participant believed that SLE don’t have renal manifestation while some study conclude that one of major reason of death among SLE patients is renal failure.
The onset of the disease is slow with new symptoms occurring over weeks, months, and sometimes years. The most common initial symptoms of lupus in patients are unspecified complaints of fatigue and health malaise. Many patients experience sporadic or persistent high temperatures with gradual loss of weight and poor appetite. Ultimately, patients progress to developing certain clinical symptoms because one or more parts of the body are affected. Skin and mucous membranes are usually the most affected by the disease. Symptoms may include various forms of skin rash, photosensitivity, and mouth ulcers. In one-third of the affected patients, the characteristic butterfly rash occurs in the center of a patient`s face [4], [5].
SLE has been found to have serious complications in previous studies, which range from renal failure to death. Early death is common in males with skin manifestations who are under 16 years old at the time of diagnosis while the possibility of late death is frequently seen in patients over 30 years at the time of diagnosis. Overall death was significantly high in older patients and in those with established kidney disease [6], [7].
In terms of SLE diagnostic patterns, the participants did not know the possible laboratory tests for diagnosing SLE; they believed that SLE is a treatable sickness where the main treatment is chemotherapy. Moreover, a great number did not know the minor or major complications of SLE. Diagnosis depends on the availability of a range of signs and symptoms with some laboratory tests involving blood and urine, and sometimes biopsy to exclude further disease. Symptoms and signs sometimes do not appear observable at any time, which makes it difficult to diagnose the disease in a timely manner. The American College of Rheumatology has listed 11 criteria to differentiate SLE from other diseases; if many of them are reported in clinical settings they may indicate the presence of SLE. This criterion roughly signifies the common clinical symptoms of people with this disease. To diagnose this disease, at least four of these 11 criteria must be met at any given time. However, experienced physicians are able to diagnose it even if patients present with fewer than four criteria.
Most of the participants in our study were unaware of SLE. This indicates poor knowledge about the disease. There were no statistically significant differences in awareness about SLE between males and females (P = 0.304), but there was statistically significant differences according to education levels (P = 0.023), and between knowing a person who had been diagnosed with SLE and caring for him or her (P = 0.020).
Finally, most participants believed that awareness of SLE should be promoted in the community, whether in hospitals or schools, to enhance knowledge about the disease and its nature in a different way; it was recommended that clinical workshops be conducted, short videotapes or medical flyers be used, and face-to-face discussions be held along with support groups and online resources.
Limitations: This study was geographically limited and only included the patients to primary healthcare clinics at KAMC in Riyadh. Therefore, it may not be possible to generalize the results. Recall bias is also possible.
Recommendations: There is a need for public awareness activities to educate people about SLE, its clinical manifestations, diagnosis, treatment, and complications; although it is not a contagious disease that requires isolation, it may be fatal if neglected.
In conclusion, the study shows that this survey is valuable and beneficial to the community as it helps people to assess their knowledge about SLE and become more aware of the disease.
Acknowledgments
A sincere appreciation to King Abdulaziz Medical City and to the participants who supported the research. Furthermore, we would like to thank eScienta (www.eScienta.com) for English language editing.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Kimberly RP. Research advances in systemic lupus erythematosus. Jama. 2001;285(5):650–2. doi: 10.1001/jama.285.5.650. https://doi.org/10.1001/jama.285.5.650 PMid:11176876. [DOI] [PubMed] [Google Scholar]
- 2.Sullivan S. Development of a Systemic Lupus Erythematosus Knowledge Questionnaire: The Relationship among Disease Proximity, Educational Exposure and Knowledge. Development. 2016 [Google Scholar]
- 3.Moriarty T, O'sullivan M, Tam A, Goncalves RM, Wall JG. Systemic lupus erythematosus in Portugal: Diagnosis and disease awareness from 1970 to 2001. European journal of epidemiology. 2003;18(10):995–9. doi: 10.1023/a:1025854611531. https://doi.org/10.1023/A:1025854611531 PMid:14598930. [DOI] [PubMed] [Google Scholar]
- 4.Khan A, Shah MH, Nauman M, Hakim I, Shahid G, Niaz P, Sethi H, Aziz S, Arabdin M. Clinical manifestations of patients with Systemic Lupus Erythematosus (SLE) in Khyber Pakhtunkhwa. JPMA. The Journal of the Pakistan Medical Association. 2017;67(8):1180–5. PMid:28839301. [PubMed] [Google Scholar]
- 5.Strand V, Galateanu C, Pushparajah DS, Nikai E, Sayers J, Wood R, Vollenhoven RV. Limitations of current treatments for systemic lupus erythematosus: a patient and physician survey. Lupus. 2013;22(8):81926. doi: 10.1177/0961203313492577. https://doi.org/10.1177/0961203313492577 PMid:23817511. [DOI] [PubMed] [Google Scholar]
- 6.Heller T, Ahmed M, Siddiqqi A, Wallrauch C, Bahlas S. Systemic lupus erythematosus in Saudi Arabia: morbidity and mortality in a multiethnic population. Lupus. 2007;16(11):908–14. doi: 10.1177/0961203307081112. https://doi.org/10.1177/0961203307081112 PMid:17971366. [DOI] [PubMed] [Google Scholar]
- 7.La Paglia GM, Leone MC, Lepri G, Vagelli R, Valentini E, Alunno A, Tani C. One year in review 2017: systemic lupus erythematosus. Clinical and experimental rheumatology. 2017;35(4):551. PMid:28721860. [PubMed] [Google Scholar]
- 8.Sutanto B, Singh-Grewal D, McNeil HP, O'Neill S, Craig JC, Jones J, Tong A. Experiences and perspectives of adults living with systemic lupus erythematosus: thematic synthesis of qualitative studies. Arthritis care & research. 2013;65(11):1752–65. doi: 10.1002/acr.22032. https://doi.org/10.1002/acr.22032 PMid:23609952. [DOI] [PubMed] [Google Scholar]
- 9.Ippolito A, Petri M. An update on mortality in systemic lupus erythematosus. Clinical & Experimental Rheumatology. 2008;26(5):S72. PMid:19026147. [PubMed] [Google Scholar]
- 10.Omair MA, Al Ohali SM, Abdulkarim FA, Madhi HA, Alghamdi LA. Awareness and Misconceptions of Female Students in King Saud University on Systemic Lupus Erythematosus. Rheumatology (Sunnyvale) 2015;5:165. https://doi.org/10.4172/2161-1149.1000165. [Google Scholar]
- 11.Althobiti SD, Alharthi TF, Alam SS, Althobiti EO. World Journal Of Pharmaceutical Research. 2017 [Google Scholar]
- 12.Zaaba NAAB, Gheena To study the Awareness of the General Public on Systemic Lupus Erythematosus (SLE) International Journal of Current Research. 2017;9(02):46382–46385. [Google Scholar]
- 13.AlKhalaf AA, Ghaleb R, Al Shawaf MH, Abdrabalnabi AA, Al-Shabib AA, Al-Khatem AH, Al Malak YT, Al Qattan HA, Al-Khalaf HE. Awareness of Systemic Lupus Erythematosus among Students in King Faisal University. Egyptian Journal of Hospital Medicine. 2018;70(6) https://doi.org/10.12816/0044350. [Google Scholar]
- 14.Al-Arfaj AS, Al-Balla SR, Al-Dalaan AN, Al-Saleh SS, Bahabri SA, Mousa MM, Sekeit MA. Prevalence of systemic lupus erythematosus in central Saudi Arabia. Saudi medical journal. 2002;23(1):87–9. PMid:11938371. [PubMed] [Google Scholar]
- 15.Rees F, Doherty M, Grainge MJ, Lanyon P, Zhang W. The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies. Rheumatology. 2017;56(11):1945–61. doi: 10.1093/rheumatology/kex260. https://doi.org/10.1093/rheumatology/kex260 PMid:28968809. [DOI] [PubMed] [Google Scholar]
- 16.Lateef A, Petri M. Unmet medical needs in systemic lupus erythematosus. Arthritis research & therapy. 2012;14(4):S4. doi: 10.1186/ar3919. https://doi.org/10.1186/ar3919 PMid:23281889 PMCid: PMC3535719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferucci ED, Johnston JM, Gaddy JR, Sumner L, Posever JO, Choromanski TL, Gordon C, Lim SS, Helmick CG. Prevalence and Incidence of Systemic Lupus Erythematosus in a Population-Based Registry of American Indian and Alaska Native People, 2007–2009. Arthritis & rheumatology. 2014;66(9):2494–502. doi: 10.1002/art.38720. https://doi.org/10.1002/art.38720 PMid:24891315 PMCid: PMC4617772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Somers EC, Marder W, Cagnoli P, Lewis EE, DeGuire P, Gordon C, Helmick CG, Wang L, Wing JJ, Dhar JP, Leisen J. Population-based incidence and prevalence of systemic lupus erythematosus: The Michigan lupus epidemiology and surveillance program. Arthritis & rheumatology. 2014;66(2):369–78. doi: 10.1002/art.38238. https://doi.org/10.1002/art.38238 PMid:24504809 PMCid: PMC4198147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ellis CB. Systemic Lupus Erythematosus and Pregnancy in Ireland: Complex yet Manageable. Crit Care Obst&Gyne. 2016;2:2. [Google Scholar]
- 20.Alyoussuf A, Alassar B, Mohammed O, Mirghani H, Amirthalingam P. Pattern of Systemic Lupus Erythematosus in Tabuk, Saudi Arabia. 2016; 5(2):23–28. [Google Scholar]
- 21.Feldman CH, Hiraki LT, Liu J, Fischer MA, Solomon DH, Alarcón GS, Winkelmayer WC, Costenbader KH. Epidemiology and sociodemographics of systemic lupus erythematosus and lupus nephritis among US adults with Medicaid coverage, 2000–2004. Arthritis & Rheumatology. 2013;65(3):753–63. doi: 10.1002/art.37795. https://doi.org/10.1002/art.37795 PMid:23203603 PMCid: PMC3733212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis & Rheumatology. 1997;40(9):1725. doi: 10.1002/art.1780400928. https://doi.org/10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]
- 23.Jakes RW, Bae SC, Louthrenoo W, Mok CC, Navarra SV, Kwon N. Systematic review of the epidemiology of systemic lupus erythematosus in the Asia-Pacific region: Prevalence, incidence, clinical features, and mortality. Arthritis care & research. 2012;64(2):159–68. doi: 10.1002/acr.20683. https://doi.org/10.1002/acr.20683 PMid:22052624. [DOI] [PubMed] [Google Scholar]
- 24.Kuhn A, Bonsmann G, Anders HJ, Herzer P, Tenbrock K, Schneider M. The diagnosis and treatment of systemic lupus erythematosus. Deutsches Ärzteblatt International. 2015;112(25):423. doi: 10.3238/arztebl.2015.0423. https://doi.org/10.3238/arztebl.2015.0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lim SS, Bayakly AR, Helmick CG, Gordon C, Easley KA, Drenkard C. The incidence and prevalence of systemic lupus erythematosus, 2002–2004: the Georgia Lupus Registry. Arthritis & rheumatology. 2014;66(2):357–68. doi: 10.1002/art.38239. https://doi.org/10.1002/art.38239 PMid:24504808 PMCid: PMC4617771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Manson JJ, Isenberg DA. The pathogenesis of systemic lupus erythematosus. Neth J Med. 2003;61(11):343–6. PMid:14768716. [PubMed] [Google Scholar]
- 27.Robson MG, Walport MJ. Pathogenesis of systemic lupus erythematosus (SLE) Clinical & Experimental Allergy. 2001;31(5):678–85. doi: 10.1046/j.1365-2222.2001.01147.x. https://doi.org/10.1046/j.1365-2222.2001.01147.x. [DOI] [PubMed] [Google Scholar]
- 28.Abid N, Khan AS, Otaibi FH. Systemic lupus erythematosus (SLE) in the eastern region of Saudi Arabia. A comparative study. Lupus. 2013;22(14):1529–33. doi: 10.1177/0961203313500548. https://doi.org/10.1177/0961203313500548 PMid:23934402. [DOI] [PubMed] [Google Scholar]
- 29.Houman MH, Smiti-Khanfir M, Ghorbell IB, Miled M. Systemic lupus erythematosus in Tunisia: demographic and clinical analysis of 100 patients. Lupus. 2004;13(3):204–11. doi: 10.1191/0961203303lu530xx. https://doi.org/10.1191/0961203303lu530xx PMid:15119551. [DOI] [PubMed] [Google Scholar]
- 30.Elfving P, Puolakka K, Kautiainen H, Virta LJ, Pohjolainen T, Kaipiainen-Seppänen O. Mortality and causes of death among incident cases of systemic lupus erythematosus in Finland 2000–2008. Lupus. 2014;23(13):1430–4. doi: 10.1177/0961203314543919. https://doi.org/10.1177/0961203314543919 PMid:25057036. [DOI] [PubMed] [Google Scholar]
- 31.Barton-Ellis C. Systemic Lupus Erythematosus and Pregnancy in Ireland: Complex yet Manageable. Critical Care Obstetrics and Gynecology. 2016;2(2) [Google Scholar]
- 32.Archenholtz B, Burckhardt CS, Segesten K. Quality of life of women with systemic lupus erythematosus or rheumatoid arthritis: Domains of importance and dissatisfaction. Quality of Life Research. 1999;8(5):411–6. doi: 10.1023/a:1008915115370. https://doi.org/10.1023/A:1008915115370 PMid:10474282. [DOI] [PubMed] [Google Scholar]
- 33.Hassett AL, Li T, Radvanski DC, Savage SV, Buyske S, Schiff SA, Katz PP. Assessment of health-related family role functioning in systemic lupus erythematosus: Preliminary validation of a new measure. Arthritis care & research. 2012;64(9):1341–8. doi: 10.1002/acr.21676. https://doi.org/10.1002/acr.21676 PMid:22438284. [DOI] [PubMed] [Google Scholar]
- 34.Alballa SR. Systemic lupus erythematosus in Saudi patients. Clinical rheumatology. 1995;14(3):3426. doi: 10.1007/BF02208351. https://doi.org/10.1007/BF02208351. [DOI] [PubMed] [Google Scholar]
- 35.Farinha F, Freitas F, Águeda A, Cunha I, Barcelos A. Concerns of patients with systemic lupus erythematosus and adherence to therapy–a qualitative study. Patient preference and adherence. 2017;11:1213. doi: 10.2147/PPA.S137544. https://doi.org/10.2147/PPA.S137544 PMid:28761334 PMCid: PMC5522825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale: application to patients with multiple sclerosis and systemic lupus erythematosus. Archives of neurology. 1989;46(10):1121–3. doi: 10.1001/archneur.1989.00520460115022. https://doi.org/10.1001/archneur.1989.00520460115022 PMid:2803071. [DOI] [PubMed] [Google Scholar]


