Abstract
Among medical students, neurosceince is considered a notoriously difficult subject. This challenges faculty to teach preclinical neurology in more engaging, efficient, and prioritized ways. Traditional approaches to neuroscience instruction typically begin with neuroanatomy and advance to clinical problem solving after this foundation of knowledge is in place. Over the past 45 years, neurology faculty at Mayo Clinic Alix School of Medicine have developed and iteratively refined an inverted approach called The Basic Four. The Basic Four uses authentic clinical scenarios as the basis for neuroscience instruction and incorporates principles from cognitive load theory to calibrate load on students’ working memory. This perspective describes The Basic Four and illustrates how cognitive load theory can be used to enhance case-based learning.
Keywords: case-based learning, cognitive load theory, undergraduate medical education, neuroanatomy, neuroscience
Introduction
Introducing preclinical medical students to neuroanatomic localization poses challenges to learner and teacher alike. Novice learners often perceive neuroscience to be complex, esoteric, and formidable—so much so that the term “neurophobia” has been coined to describe the apprehension with which they approach it.1-6 Students often have little neuroscience background, and retention of neuroscience knowledge into the clinical years is poor.7 For these reasons, the task of teaching neuroanatomy has been called “difficult and unenviable.”8
Compounding these challenges are trends in medical education, including initiatives to shorten medical school training,9 incorporate new content into medical school curricula,10-12 and undertake various other curricular reforms. Current and projected shortages of neurologists also highlight the need to recruit more students into the specialty.13 Thus, faculty are compelled to teach neuroscience in more engaging, efficient, and prioritized ways.
Over the years, neurology faculty at the Mayo Clinic Alix School of Medicine have responded to these challenges by developing an innovative approach to clinical neuroscience instruction called The Basic Four. The original version of this approach was conceived in 1972 by Dr Burton Sandok, a Mayo Clinic neurologist, later department chair, then medical school dean, known for his ability to teach and simplify complex concepts.14 It has since been iteratively refined and revised by numerous neurology faculty and used to teach neuroscience to more than 1700 preclinical medical students in both small and large group settings. In this perspective, we aim to describe The Basic Four approach and illustrate how cognitive load theory (CLT) can be used to enhance case-based learning. This is not a one-size-fits-all approach, but rather an example of how learning theory can enrich and inform neuroscience instruction.
Overview of The Basic Four Approach
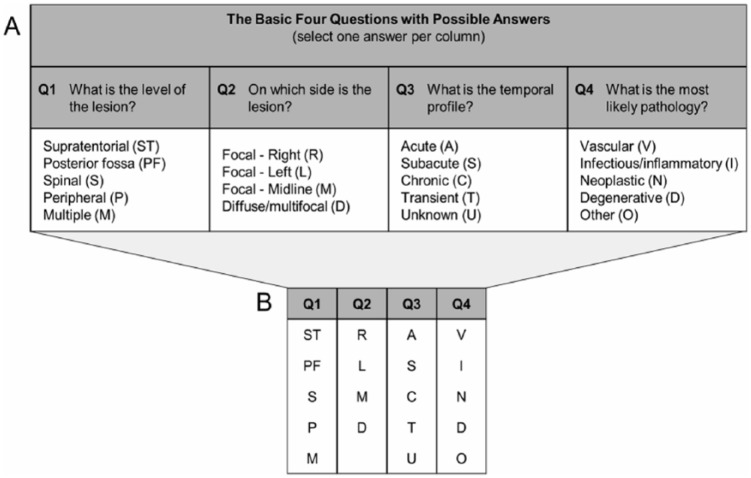
The Basic Four represents a type of case-based learning15 in which students are presented with authentic clinical cases (in a variety of formats) and prompted to answer four questions (Q1-4, Figure 1A). This standardized set of questions guides students through the tasks of neuroanatomic localization (Q1-2) and differential diagnosis (Q3-4), allowing novice students to reach possible diagnoses with relative ease. This process serves as a springboard for subsequent inquiry into basic and clinical neuroscience concepts. Figure 1B shows the shorthand version of The Basic Four as it appears in all course materials. Because the same set of questions is applied to every clinical scenario, students quickly internalize these abbreviated question-and-answer groupings.
Figure 1.
The Basic Four.
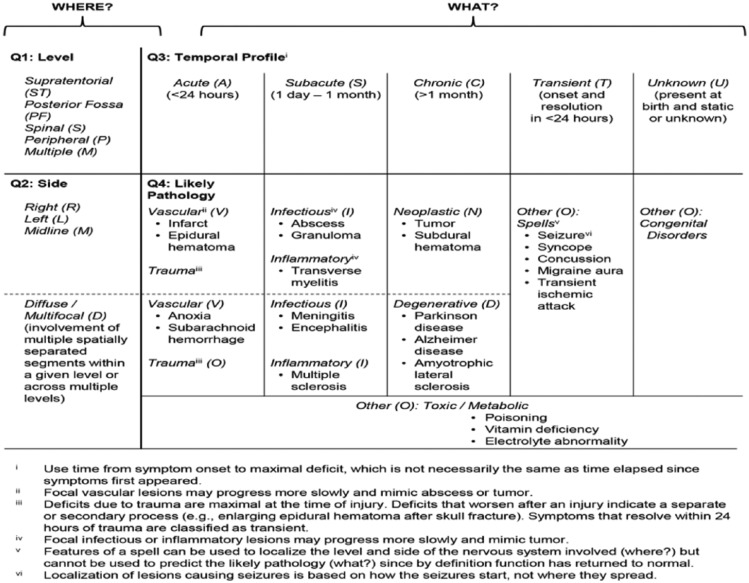
Table 1 provides six illustrative clinical scenarios, their Basic Four formulations, and a possible diagnosis for each. Guidelines for applying The Basic Four are provided in Figure 2, which can also serve as a handout for learners. These guidelines summarize “first principles” of neuroanatomy8 (eg, ipsilateral face and limb involvement suggests a contralateral supratentorial lesion) and physiology (eg, a process that starts acutely is likely to be vascular in nature), which can be learned and applied without any previous neuroscience training. Initial cases are very simple (Table 1, case 1) but increase in complexity (Table 1, case 6) and fidelity (through the use of video clips and a simulated patient encounter) as the course progresses and students’ knowledge base grows.
Table 1.
Examples of The Basic Four applied to clinical scenarios to localize a lesion and generate a possible diagnosis.
| Sample cases | Basic Four formulation |
|||
|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | |
| Case 1: A 6-year-old girl with surgically corrected congenital heart defect complains of headaches, which have increased in severity over several days, along with the development of left-sided weakness. Her temperature is 38.8°C. Physical examination shows a hemiparesis involving the left face, arm, and leg. | ST | R | S | I |
| Diagnosis: Cerebral abscess | ||||
| Case 2: A 50-year-old man presents with a 6-month history of progressive gait unsteadiness. On examination, he falls when he closes his eyes. There is weakness in the feet. Muscle stretch reflexes are absent at the knees and ankles and diminished in the arms. Joint position and vibration sense are absent at the toes and ankles. Touch and pain are absent below the midcalf. | P | D | C | D |
| Diagnosis: Diabetic peripheral neuropathy | ||||
| Case 3: A 35-year-old man experiences three episodes during which he felt a prickling numbness spreading from his left thumb up the arm and to his left face, followed by involuntary jerking of the arm. The episodes lasted about 2 min. Neurologic examination between episodes is normal. Electroencephalogram (EEG) shows a spike focus in the right central-parietal area. | ST | R | T | O |
| Diagnosis: Focal seizures with Jacksonian march | ||||
| Case 4: An 18-year-old man in military training camp becomes ill. He complains of headache, chills, fever, and cough. The next day, he develops worsening headache and neck stiffness followed by progressive confusion, somnolence, and finally coma. On examination, his temperature is 39.2°C. He is unresponsive to vigorous stimulation and has nuchal rigidity. Pupillary, corneal, and gag reflexes are normal. | M | D | S | I |
| Diagnosis: Bacterial meningitis | ||||
| Case 5: A 68-year-old woman experiences the sudden onset of nausea and dizziness with voice hoarseness. Neurologic examination reveals absent perspiration on the left side of her face, a small left pupil, and left eyelid dropping. The left palate is drooping, and the left gag reflex is absent. There is loss of pain and temperature sensation on the left face and right body, incoordination of the left arm and leg, and nystagmus. | PF | L | A | V |
| Diagnosis: Lateral medullary infarct | ||||
| Case 6: A 23-year-old woman awoke 2 days ago with numbness and tingling in her toes. Over the next 24 h, the sensory symptoms spread up her legs, and she developed urinary urgency. On examination, she has a spastic-ataxic gait. Romberg test is positive. Strength is normal. Muscle stretch reflexes increased in the legs with bilateral Babinski signs. The anal reflex is preserved. Vibratory sense is absent below the iliac crest; joint position sense is moderately reduced. There is mild loss of touch and pin sensation below the umbilicus. | S | M | S | I |
| Diagnosis: Transverse myelitis due to multiple sclerosis | ||||
Figure 2.
In this fashion, The Basic Four approach uses clinical reasoning as the starting point for neuroscience instruction, encouraging students to develop cognitive schemata from worked examples. Notably, Basic Four problems are intended to be the means by which students learn neuroscience, rather than simply an opportunity for students to apply previously learned concepts. This represents an inversion of more traditional approaches, which typically begin with neuroanatomy and advance to clinical problem solving after this foundation of knowledge is in place.
Rationale for The Basic Four Approach
Case-based learning has been shown to positively impact a number of relevant learning outcomes across a variety of subject areas,15 including neuroanatomy16-19 and neurologic reasoning.20,21 Case-based learning is also recognized as a way to foster interest in neurology.22 The Basic Four method seeks to further optimize this approach by incorporating principles of CLT.
CLT posits that learning is most effective when instruction is aligned with human capacity for information processing. According to CLT, information processing is most acutely constrained by the limited capacity of working memory, which can hold only a few discrete elements at any given time.23 If the elements being held in working memory interact (requiring simultaneous processing), working memory becomes further constrained.24 In this fashion, the capacity of working memory varies between learners and within the same learner at different times.
Neuroanatomic localization and neurologic clinical reasoning are complex tasks that can easily exceed the processing capacity of novice learners, resulting in cognitive overload.25 Three types of cognitive load can strain working memory: extraneous load (effort required to cope with factors not directly related to the task at hand, such as interruptions or dense lecture slides), intrinsic load (effort required to process the inherent complexity of new information, such as lateral medullary syndrome), and germane load (effort required to build cognitive schemata through which one understands new concepts, such as upper versus lower motor neurons). For novice learners without preexisting cognitive schemata or mental representations (eg, first-year medical students learning neuroanatomy), intrinsic load is particularly hefty.22
When total cognitive load exceeds working memory capacity, learning is impaired.24 CLT can inform strategies to prevent working memory overload and optimize allocation of cognitive resources during case-based learning by reducing extraneous load, titrating intrinsic load to the learner’s level, and optimizing germane load.24
The Basic Four approach aims to reduce extraneous load by providing a consistent approach to neuroanatomic localization that is maintained throughout the entire neuroscience course, including large group lectures, small group sessions, weekly tests, the final examination, and a simulated patient encounter. In each setting, The Basic Four is presented in the same format and order with consistent abbreviations (Figure 1). Thus, no cognitive load is wasted deciphering new formats or harmonizing discrepant structures, and students’ working memory can be more fully devoted to learning. Table 2 outlines additional ways in which The Basic Four tries to reduce extraneous load.
Table 2.
The Basic Four application of cognitive load theory principles to decrease extraneous load.
| Principle | The Basic Four application |
|---|---|
| Maintain consistent structure and format | Clinical cases are presented consistently (patient history, then examination findings), and Basic Four questions are written consistently (four columns, uniform abbreviations) throughout the neuroscience course. |
| Provide worked examples | Students are encouraged to study solved clinical cases with answers and explanations to all Basic Four questions as worked examples before attempting solutions on their own. |
| Facilitate completion of partially solved problems | Answers to a subset of The Basic Four questions are provided, allowing students to complete the remaining questions on their own. The Basic Four approach as a whole also generates a partial solution to clinical cases by identifying a probable pathophysiologic category (eg, vascular), after which students are asked to generate a prioritized list of more specific diagnoses (eg, subarachnoid hemorrhage). |
| Avoid split attention | The Basic Four is presented as an integrated set (in the shorthand version) immediately after corresponding clinical cases, allowing students to focus their attention. |
| Employ dual modality | Clinical cases and any accompanying images or videos are projected on a screen while a large or small group leader facilitates discussion and offers verbal explanations to The Basic Four questions. Off-loading some information to the auditory system avoids overloading the visual system. |
| Replace transient with permanent information | Students are given a one-page summary of The Basic Four rules while working through initial examples to alleviate the strain on working memory. As they work more examples, fewer references to this printed resource are required. |
| Employ the goal-free principle | The Basic Four does not aim to provide a single diagnosis; rather, it guides students to the most likely disease category from which to generate a list of possible diagnoses. |
The Basic Four approach seeks to manage intrinsic load by simplifying and constraining the tasks of neuroanatomic localization and differential diagnosis generation. Notably, the number of interacting elements is restricted to four, the maximum capacity for simultaneous manipulation by working memory. Isolating these elements initially is intended to manage intrinsic load for novice learners. Over time, intrinsic load may be further reduced by viewing The Basic Four as two pairs of questions, with Q1 and Q2 answering “where” and Q3 and Q4 answering “what.” This is an example of “chunking,” which reduces interactivity and thereby lessens intrinsic load.26 Table 3 outlines other ways in which The Basic Four seeks to manage intrinsic load.
Table 3.
The Basic Four application of cognitive load theory principles to manage intrinsic load.
| Principle | The Basic Four application |
|---|---|
| Restrict number of elements | The Basic Four comprises only four questions, each with restricted number of four to five possible answers. |
| Isolate interactive elements | The Basic Four questions (Q1-4) are initially answered individually, minimizing element interactivity. |
| Provide chunking strategies | Over time, students chunk The Basic Four questions, with Q1-2 answering “where” is the lesion and Q3-4 answering “what” is the lesion; repeated use of The Basic Four also facilitates the development of pattern recognition, enabling students to rapidly identify the most likely pathology for classic disease presentations. |
| Progress from simple to complex | Initial case scenarios are very simple and straightforward but become more complex as students’ knowledge of neuroscience grows. Initial cases are written succinctly and include only relevant information. Later cases challenge students to sort through extraneous information and provide more verisimilitude to real clinical encounters. |
| Progress from low to high fidelity | The Basic Four is initially used with low-fidelity written case scenarios. The fidelity of these written scenarios can be increased by incorporating photographs or video recordings from actual patients. Students then progress to higher fidelity cases, applying The Basic Four to a simulated patient encounter at the end of their first-year neuroscience course and to actual patients during their neurology clerkship. |
Once extraneous load has been minimized and intrinsic load titrated, newly liberated working memory capacity can be allocated to germane load. The Basic Four approach attempts to optimize germane load by varying clinical problem-solving tasks, which has been shown to enhance learning.24 Course instructors can apply this “variability principle”27 by interweaving clinical cases with similar presentations but different causes (eg, progressive myelopathy due to infection, disk herniation, or spinal meningioma) and different presentations of the same cause (eg, cerebral ischemia). This optimizes germane load and encourages students to maintain a broad differential diagnosis. Table 4 outlines additional ways in which The Basic Four approach can optimize germane load.
Table 4.
The Basic Four application of cognitive load theory principles to optimize germane load.
| Principle | The Basic Four application |
|---|---|
| Introduce contextual interference via random ordering of tasks | Disorders covered in lecture and their corresponding clinical cases are presented in different orders. Weekly clinical problem-solving sessions using The Basic Four are cumulative, including both recent and previously learned concepts. |
| Employ the variability principle | Cases featuring similar clinical presentations but different underlying causes are intermixed. |
| Encourage self-explanation | Students are asked to justify their answers to The Basic Four questions based on relevant neuroanatomy and pathophysiology principles. |
| Encourage imagination | Students are encouraged to write their own clinical cases and formulate answers to The Basic Four questions. Well-written questions are incorporated into the neuroscience course for subsequent use by other students. |
Clinical reasoning is a complex, iterative task that involves both analytic and non-analytic strategies and is influenced by contextual cues.28 The Basic Four aims to introduce novice learners to this process by facilitating the creation of initial hypotheses about the nature of a patient’s problem. It answers the questions “where?” and “what?” but does not aim to answer the question “why?” (ie, by providing a specific diagnosis or definitive explanation for the patient’s problem). Instead, The Basic Four guides students to a disease category from which to generate a list of diagnostic possibilities. This exemplifies the use of nonspecific goals, which reduce cognitive load for novice learners, improve their problem-solving strategies, and facilitate transfer of learning to new contexts (the “goal-free principle,” Table 2).29,30
Discussion
The Basic Four is a practical, clinically oriented approach to teaching neuroanatomy and neuroscience that seeks to optimize case-based learning by incorporating principles of CLT. This approach illustrates how educators can apply evidence-based learning theories to common pedagogical strategies to increase their effectiveness—a recommended strategy for combatting neurophobia and promoting neurophilia.31
The Basic Four approach is particularly well-suited for novice learners, allowing them to engage in part-task practice with increasing complex written case scenarios.32 Importantly, The Basic Four is suitable for use with a variety of instructional modalities (eg, large group lectures, small group sessions, face-to-face teaching, online learning modules, and other digital learning tools) and can also be used in simulated or real clinical settings, such as those encountered during clerkships. In this fashion, The Basic Four accommodates increasing task complexity and fidelity, which allows for vertical integration of neurology curricula31 and may facilitate transfer of knowledge from classroom settings to subsequent patient care.25 Repeated use of The Basic Four may also improve retention, an important initial step toward ensuring students acquire the essential neurologic skills needed for high-quality patient care.33
The nervous system is a highly complex and nuanced biological entity, and The Basic Four, like any conceptual framework, presents only a partial view of reality.34 Seasoned neurologists will recognize its shortcomings and identify exceptions. For example, carpal tunnel syndrome often presents as a focal, chronic lesion but is rarely caused by a neoplasm (the resulting Basic Four diagnosis). However, it is important for medical educators to recognize oversimplification as an asset to early learners. Instructors tend to underestimate the difficulty of assimilating new information because they have the benefit of existing cognitive schemata,35 whereas learners face the more demanding task of schema construction.24 Strategic simplifications, such as those offered by The Basic Four, aid in this process by teaching students the “rules” before they learn the “exceptions.”
Conclusions
Traditional approaches to preclinical neuroscience instruction typically begin with neuroanatomy and advance to clinical problem solving after this foundation of knowledge is in place. The Basic Four inverts this approach by first providing a scaffold or cognitive schema for solving clinical problems, then populating this scaffold with relevant knowledge of neuroanatomy, physiology, and pathology. The Basic Four illustrates how CLT can be used to enhance case-based learning in an effort to make the process of learning neuroscience more efficient, effective, and enjoyable. This, in turn, may foster interest in neurology and help combat neurophobia. Further study is needed to measure the impact of The Basic Four approach on relevant outcomes such as performance on standardized tests, clinical clerkship evaluations, and recruitment of medical students into neurology.
Acknowledgments
The authors wish to acknowledge the late Dr Burton Sandok (1937-2011) for developing the original version of The Basic Four, the faculty of the Mayo Clinic Alix School of Medicine first-year neuroscience course for their dedication to teaching clinical neurology, and the hundreds of medical students whose enthusiasm for learning and insightful questions have inspired ongoing refinements of The Basic Four approach.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: KES, JKC-G, and ANLH contributed to the study concept, study design, and drafting of the manuscript. All authors approved the final manuscript.
References
- 1. Jozefowicz RF. Neurophobia: the fear of neurology among medical students. Arch Neurol. 1994;51:328–329. [DOI] [PubMed] [Google Scholar]
- 2. Zinchuk AV, Flanagan EP, Tubridy NJ, Miller WA, McCullough LD. Attitudes of US medical trainees toward neurology education: “neurophobia”—a global issue. BMC Med Educ. 2010;10:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pakpoor J, Handel AE, Disanto G, Davenport RJ, Giovannoni G, Ramagopalan SV. National survey of UK medical students on the perception of neurology. BMC Med Educ. 2014;14:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Abulaban AA, Obeid TH, Algahtani HA, et al. Neurophobia among medical students. Neurosciences. 2015;20:37–40. [PMC free article] [PubMed] [Google Scholar]
- 5. Solorzano GE, Jozefowicz RF. Neurophobia: a chronic disease of medical students. Neurology. 2015;85:1–2. [DOI] [PubMed] [Google Scholar]
- 6. Shiels L, Majmundar P, Zywot A, Sobotka J, Lau CSM, Jalonen TO. Medical student attitudes and educational interventions to prevent neurophobia: a longitudinal study. BMC Med Educ. 2017;17:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mateen FJ, D’Eon MF. Neuroanatomy: a single institution study of knowledge loss. Med Teach. 2008;30:537–539. [DOI] [PubMed] [Google Scholar]
- 8. Chang BS, Molnar Z. Practical neuroanatomy teaching in the 21st century. Ann Neurol. 2015;77:911–916. [DOI] [PubMed] [Google Scholar]
- 9. Raymond JR, Sr, Kerschner JE, Hueston WJ, Maurana CA. The merits and challenges of three-year medical school curricula: time for an evidence-based discussion. Acad Med. 2015;90:1318–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Skochelak SE. A decade of reports calling for change in medical education: what do they say? Acad Med. 2010;85:S26–S33. [DOI] [PubMed] [Google Scholar]
- 11. Lucey CR. Medical education: part of the problem and part of the solution. JAMA Intern Med. 2013;173:1639–1643. [DOI] [PubMed] [Google Scholar]
- 12. Gonzalo JD, Dekhtyar M, Starr SR, et al. Health systems science curricula in undergraduate medical education: identifying and defining a potential curricular framework. Acad Med. 2017;92:123–131. [DOI] [PubMed] [Google Scholar]
- 13. Larsen DP, Santini VE. Increasing student recruitment into neurology: joining the family. Neurology. 2015;84:2302–2303. [DOI] [PubMed] [Google Scholar]
- 14. Valdez CK. Dr. Burton Sandok, who helped start Mayo Medical School, had passion for neurology. The Post Bulletin. http://www.postbulletin.com/news/local/dr-burton-sandok-who-helped-start-mayo-medical-school-had/article_66dc2be0-a779-536d-8a30-f4a3123eba7d.html. Published 2011. Accessed November 29, 2017.
- 15. McLean SF. Case-based learning and its application in medical and health-care fields: a review of worldwide literature. J Med Educ Curric Dev. 2016;3:39–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Greenwald RR, Quitadamo IJ. A mind of their own: using inquiry-based teaching to build critical thinking skills and intellectual engagement in an undergraduate neuroanatomy course. J Undergrad Neurosci Educ. 2014;12:A100–A106. [PMC free article] [PubMed] [Google Scholar]
- 17. Kennedy S. Using case studies as a semester-long tool to teach neuroanatomy and structure-function relationships to undergraduates. J Undergrad Neurosci Educ. 2013;12:A18–A22. [PMC free article] [PubMed] [Google Scholar]
- 18. Gelb D. Neuro-logic: the principles of lesion localization in patients with neurological symptoms. Mededportal. 2006;2:181. doi: 10.15766/mep_2374-8265.181. [DOI] [Google Scholar]
- 19. Sheldon JP. A neuroanatomy teaching activity using case studies and collaboration. Teach Psychol. 2000;27:126–128. [Google Scholar]
- 20. Strowd R, Kwan A, Cruz T, Gamaldo C, Salas R. A guide to developing clinical reasoning skills in neurology: a focus on medical students. Mededportal. 2015;11:10163. doi: 10.15766/mep_2374-8265.10163. [DOI] [Google Scholar]
- 21. Levin M, Cennimo D, Chen S, Lamba S. Teaching clinical reasoning to medical students: a case-based illness script worksheet approach. Mededportal. 2016;12:10445. doi: 10.15766/mep_2374-8265.10445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Javaid MA, Chakraborty S, Cryan JF, Schellekens H, Toulouse A. Understanding neurophobia: reasons behind impaired understanding and learning of neuroanatomy in cross-disciplinary healthcare students. Anat Sci Educ. 2018;11:81–93. [DOI] [PubMed] [Google Scholar]
- 23. Miller GA. The magical number seven, plus or minus two: some limits on our capacity for processing information. Psychol Rev. 1956;63:8111–8197. [PubMed] [Google Scholar]
- 24. Young JQ, van Merriënboer J, Durning S, Ten Cate O. Cognitive load theory: implications for medical education: AMEE Guide No. 86. Med Teach. 2014;36:371–384. [DOI] [PubMed] [Google Scholar]
- 25. Leppink J, Duvivier R. Twelve tips for medical curriculum design from a cognitive load theory perspective. Med Teach. 2016;38:669–674. [DOI] [PubMed] [Google Scholar]
- 26. Boshuizen HP, Schmidt HG. On the role of biomedical knowledge in clinical reasoning by experts, intermediates and novices. Cogn Sci. 1992;16:153–184. [Google Scholar]
- 27. van Merriënboer JJ, Sweller J. Cognitive load theory in health professional education: design principles and strategies. Med Educ. 2010;44:85–93. [DOI] [PubMed] [Google Scholar]
- 28. Yazdani S, Hosseinzadeh M, Hosseini F. Models of clinical reasoning with a focus on general practice: a critical review. J Adv Med Educ Prof. 2017;5:177–184. [PMC free article] [PubMed] [Google Scholar]
- 29. Ayres P. Why goal-free problems can facilitate learning. Contemp Educ Psychol. 1993;12:376–381. [Google Scholar]
- 30. Burns BD, Vollmeyer R. Goal specificity effects on hypothesis testing in problem solving. Quarter J Exp Psychol. 2002;55A:241–261. [DOI] [PubMed] [Google Scholar]
- 31. Shelley BP, Chacko TV, Nair BR. Preventing “neurophobia”: remodeling neurology education for 21st-century medical students through effective pedagogical strategies for “neurophilia.” Ann Indian Acad Neurol. 2018;21:9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Vandewaetere M, Manhaeve D, Aertgeerts B, Clarebout G, Van Merriënboer JJ, Roex A. 4C/ID in medical education: how to design an educational program based on whole-task learning: AMEE Guide No. 93. Med Teach. 2015;37:4–20. [DOI] [PubMed] [Google Scholar]
- 33. Nicholl DJ, Appleton JP. Clinical neurology: why this still matters in the 21st century. J Neurol Neurosurg Psychiatry. 2015;86:229–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bordage G. Conceptual frameworks to illuminate and magnify. Med Educ. 2009;43:312–319. [DOI] [PubMed] [Google Scholar]
- 35. Norman GR, Tugwell P, Feightner JW, Muzzin LJ, Jacoby LL. Knowledge and clinical problem-solving. Med Educ. 1985;19:344–356. [DOI] [PubMed] [Google Scholar]