Abstract
Background:
Tobacco use is one of the major public health threats nowadays. Smoking can affect everybody organ. Health professionals should play pivotal roles in tobacco control, and their attitude and practice toward tobacco use can affect the health of the community. Therefore, assessing and influencing physicians’ attitudes and practice are one of the alternatives to reduce smoking prevalence in the community. We aimed to assess smoking status among medical physicians in the West Bank, Palestine to better understand their future role in any smoking cessation program.
Material and methods:
A cross-sectional study using the World Health Organization Global Health Professional Survey questionnaire was conducted. A non-probability sampling technique from a total of 6500 physicians registered in the Palestinian Medical Association in the West Bank was used.
Results:
The age ranged from 23 to 78 years with a mean of 34.92 years. Current smokers represented 60.3%. Of them, 18.5% were both cigarettes and water pipe smokers. The main reason that motivates the physician to smoke is experimenting (57.9%). Also stress (31.8%) and social pressure (26.4%) were of the most common causes to start smoking. Almost all medical doctors have a high level of knowledge regarding the health consequences of smoking. Smokers were less likely to hold favorable attitudes toward smoking cessation and support tobacco control policy compared with non-smokers (P-values < .05).
Conclusions:
Physicians’ degree of awareness and knowledge about their role in aiding patients to quit smoking are high. However, smokers’ attitudes toward smoking cessation programs need to be improved to increase their involvement in such interventional programs.
Keywords: Palestine, physicians, smoking, tobacco, water pipe
Introduction
Health professionals especially medical physicians are a group of people who help in identifying, preventing, or treating illness based on their professional knowledge and skills. Therefore, they can be a motivation for their patients to feel confident in refusing habits that are harmful to their health and to make patients more aware about their health conditions.1–3 In terms of tobacco control, one of the alternative ways to prevent and reduce smoking prevalence among the community is to influence attitudes and practice of health professionals positively and to increase the awareness of their professional responsibility. Because of these considerations, health professionals should play pivotal roles in tobacco control, and their attitude and practice toward tobacco use can affect the health of the community and the country in general.1–3
According to the statistics of the World Health Organization (WHO), there are more than 1 billion smokers in the world. Globally, the use of tobacco products is increasing, although it is decreasing in high-income countries, killing up to half of all users (5.4 million people a year—an average of one person every 6 s—and accounts for one in 10 adult deaths worldwide).4
Smoking can affect everybody organ, leaving the smoker at increased risk of lung and cervical cancers, respiratory disease, cardiovascular disease, stroke, osteoporosis, rheumatoid arthritis, impotence, infertility, ectopic pregnancy, miscarriage, low birth weight babies, and many other disorders.4–6
In the meanwhile, tobacco use is one of the biggest public health threats the world has ever faced. Tobacco users who die prematurely deprive their families of income, raise the cost of health care, and hinder economic development.4,5 It is a risk factor for six of the eight leading causes of deaths in the world.4 Most of these deaths occur in low- and middle-income countries, and this disparity is expected to widen further over the next several decades. If current trends continue, WHO anticipated that by 2030, tobacco will kill more than 8 million people worldwide each year, with 80% of those are premature deaths among people living in low- and middle-income countries. The Global Youth Tobacco Survey reported that the trend for tobacco smoking in the Eastern Mediterranean Region is increasing, along with the use of other forms of tobacco such as shisha (water pipe); this increase is mostly due to the low price of tobacco in the region and the weak policies of tobacco control.5
Significant insights regarding the smoking epidemic can be obtained from studying specific subgroups of interest within the population, such as adolescents, women, and health professionals.6 The best way to reduce one’s risk of developing tobacco-related diseases is to stop smoking.7 Physicians are highly respected in their communities and people turn to them for advice, so they should act as positive role models. However, they often do not seriously address the issue of smoking or perhaps smoke themselves, which makes it even more difficult to discuss this problem with their patients or take an active role in anti-smoking efforts.8,9 Studies have shown that a decline in smoking rates among physicians often precedes a similar reduction in the general population.10,11 Such a reduction in smoking rates was observed in most Westernized countries.12 Having recognizing the important role of physicians in tobacco control, the Tobacco Free Initiative, WHO started a project, the Global Health Professional survey, to estimate the prevalence of tobacco use among health professionals and to determine the smoking habits, knowledge and attitude toward tobacco control of health professionals in several countries around the world.5 In this study, we aimed to establish an estimate of the prevalence of smoking among physicians in Palestine, and to explore their attitude toward issues related to smoking to understand their future role in a smoking cessation interventional program.
Methodology
Study design and settings
A cross-sectional study was conducted. The study was carried out in and during the medical association activities in the West Bank during the period of January to March 2015. This setting was chosen because most of the Palestinian physicians who practice medicine are registered in this association.
Study population and sampling techniques
The study population was all registered medical physicians in the medical association in the different 11 governorates of the West Bank (6500 physicians). The sample collected according to the distribution of the registered physicians for each city proportionally from the total sample (estimated to be 600 subjects).13 Clearly, the Northern cities (Nablus, Tubas, Qalqilya, Jenin, Tulkarem, and Selfit) were 36.8% of the sample, the Southern cities (Hebron and Bethlahem) were 33.5%, and the Middle cities (Ramallah, Jerusalem, and Jericho) were 29.6%. If available at the time of the study, a physician was included regardless of his or her age. A non-probability (convenient) sampling technique was used. In total, 600 physicians were invited to participate and only 502 completed the questionnaire and therefore were finally recruited (response rate = 83.6%). Nearly, 80.1% of the study participants were males.
Data collection
A previously standardized and validated self-administered questionnaire was used as the study instrument.14 The questionnaire (The World Health Organization Global Health Professional Survey Questionnaire) was used with some minor additional questions that were added on the socio-demographic section to meet the Palestinian situation. The questionnaire included the following five sections: (1) socio-demographic characteristics; (2) cigarettes use; (3) knowledge, attitudes about smoking and tobacco control; (4) practice on tobacco smoking, behavior, and cessation; and (5) water pipe smoking. The questionnaire was translated from English to Arabic language and was translated back in English to check accuracy. The translated questionnaire (Arabic version) was used and pre-tested by a convenient sample of 20 participants of the study population before use to ensure the clarity, time, ease of administration, and to test the reliability and the validity of the questionnaire. Refinements were made on the basis of the feedback from the pilot testing. Nearly, 15-20 min were needed to fill the questionnaire.
The questionnaire was distributed through the subcommittees of medical association in different governorates of West Bank and filled by the registered physicians. Data for this study was gathered through several weeks (January to March 2015).
Ethical consideration
The study was approval by An-Najah National University Institutional Review Board (IRB; archived number 08/June/2014) and from the Palestinian medical association. Participation was voluntary and a signed informed consent was obtained from each participant before filling the questionnaire. Participant’s privacy and confidentiality were assured.
Data analysis plan
The Statistical Package of Social Sciences (SPSS) (version 20) was used for data analysis.15 Qualitative variables were presented using frequency and percentages and displayed as tables. The associations between the study variables were assessed using the non-parametric Chi-square test with a P-value of less than .05 was always considered significant.
Results
Socio-demographic characteristics and prevalence of smoking
We have invited 600 physicians. Only 502 physicians completed and returned the questionnaire and, therefore, were finally recruited for this study (response rate = 83.6%). Nearly 80.1% of the participants were male. The mean age and standard deviation (SD) were 34.92 ± 11.3 years among the total study population. Nearly, 32.9% were having higher degree of medicine (MD followed by specialty in medicine and/or a research PhD).
Indeed, non-smokers represented 39.7%. However, those who smoke cigarettes only were 20.9% and those who smoke water pipe only were also 20.9%. Those who smoke both (cigarettes and water pipe) were 18.5%. Therefore, the total prevalence of current smoking (regardless of the type of smoking) was 60.3% (ie, 20.9% + 20.9% + 18.5%; Figure 1). Smokers were more likely to be males compared with non-smokers (P-value < .001). Furthermore, there were significant differences between smokers and non-smokers in regard to type of specialty and professional status (P-values < .05). Table 1 shows the socio-demographic characteristics of the study population by smoking status.
Figure 1.
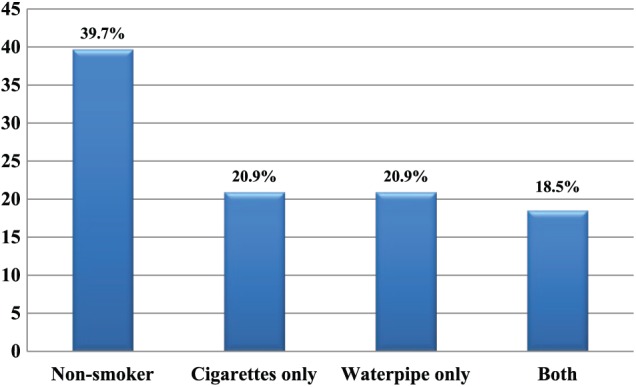
Prevalence of current smoking among different types of smoking (Y-axis represents percentages).
Table 1.
Socio-demographic characteristics of the study participants by smoking status (n = 502).
| Variable | Non-smoker, n (%) | Smoker, n (%) | χ2, P-value |
|---|---|---|---|
| Gender | |||
| Male | 273 (67.9%) | 129 (32.1%) | <.001 |
| Female | 30 (30%) | 70 (70%) | |
| City | |||
| North cities (Nablus, Tubas, Qalqilya, Jenin, Tulkarem, Selfit) | 104 (56.2%) | 81 (43.8%) | .329 |
| South cities (Hebron, Bethlahem) | 107 (63.7%) | 61 (36.3%) | |
| Middle cities (Ramallah, Jerusalem, Jericho) | 92 (61.7%) | 57 (38.3%) | |
| Age | |||
| Mean, SD | 34.71 ± 10.17 | 35.26 ± 12.93 | .014* |
| Marital status | |||
| Married | 196 (62.8%) | 116 (37.2%) | .148 |
| Other (single, divorce, and widow) | 107 (56.3%) | 83 (43.7%) | |
| Education | |||
| Higher degree of medicine (PhD, specialist) | 103 (62.4%) | 62 (37.6%) | .508 |
| First degree of medicine (master, bachelor, others) | 200 (59.3%) | 137 (40.7%) | |
| Type of specialty | |||
| Surgical (ENT, OBS/GYN, anesthesia) | 105 (66.5%) | 53 (33.5%) | .044 |
| Non surgical (internal medicine, pediatrics) | 98 (61.2%) | 62 (38.8%) | |
| Others (trainee/intern, academy) | 56 (49.6%) | 57 (50.4%) | |
| GP | 44 (62.0%) | 27 (38.0%) | |
| Professional status | |||
| Trainee/intern | 52 (48.1%) | 56 (51.9%) | .009 |
| Resident | 91 (65.9%) | 47 (34.1%) | |
| Attending physician | 140 (60.9%) | 90 (39.1%) | |
| Others (academy, director, vice director, head of department) | 20 (67.9%) | 6 (23.1%) | |
| Workplace | |||
| Hospitals (governmental, private, and NGO) | 244 (61.6%) | 152 (38.4%) | .445 |
| Non hospitals (private clinic, primary health care, and private medical centers) | 45 (54.2%) | 38 (45.8%) | |
| Both (hospital and private clinic) | 14 (60.9%) | 9 (39.1%) | |
Abbreviations: ENT, ear, nose, and throat specialist; GP, general practitioner; NGO, non-governmental organization; OBS/GYN, obstetrician and gynecologist; PhD, doctor of philosophy; SD, standard deviation.
t-test P-value.
Furthermore, about 39.5% of the physicians were current cigarettes smokers, while 12.2% of them were ex-cigarettes smokers and 48.4% never tried cigarettes smoking. The mean age ± SD of starting cigarettes smoking was 20.08 ± 2.95 years. The overall mean ± SD number of cigarettes smoked per day of the currently smokers was 16.48 ± 9.43. For male physicians, it was 16.82 ± 9.45 cigarettes per day, compared with 9.28 ± 8.89 for females (P-value = .003). Nearly, 41% of smokers answered that they are not ready to quit smoking within the next 6 months and only 23% reported they are thinking to quit within the coming 6 months.
The main reason that motivates the physician to smoke is experimenting (57.9%). Also stress (31.8%) and social pressure (26.4%) were of the most common causes to start smoking.
Knowledge of health effects associated with smoking
Only a minority of the physicians (2.0%) disagreed that smoking is harmful to their health, and this was significantly higher among the current smokers group (P-value = .015). Less than half (39.5%) of physicians reported that they disagree or unsure regarding the statement “neonatal death is associated with passive smoking”; and this was significantly higher among current smokers group (P-value = .003). Less than one-fifth of physicians (15.4%) reported that they disagree or unsure regarding the statement “maternal smoking during pregnancy increases the risk of Sudden Infant Death Syndrome,” and this was not significant among current smokers group compared with non-current smokers one (P-value = .565). Moreover, more than one-tenth of the physicians (12.2%) disagreed or were unsure that passive smoking increases the risk of heart disease in non-smoking adults (P-value = .019). However, only a minority of the physicians (6.2%) disagreed or were unsure that paternal smoking increases the risk of lower respiratory tract illnesses in children (P-value = .022). Table 2 shows more details regarding knowledge of adverse effects of smoking among the studied population.
Table 2.
Smoking knowledge stratified by smoking status of the participants (N = 502).
| Variable | Total, N (%) | Smoker, n (%) | Non-smoker, n (%) | χ2, P-value |
|---|---|---|---|---|
| Smoking is harmful to health | ||||
| Disagree | 10 (2.0%) | 9 (90.0%) | 1 (10.0%) | .015 |
| Unsure | 15 (3.0%) | 13 (86.7%) | 2 (13.3%) | |
| Agree | 477 (95.0%) | 281 (58.9%) | 196 (41.1%) | |
| Neonatal death association with passive smoking | ||||
| Disagree | 40 (8.0%) | 33 (82.5%) | 7 (17.5%) | .003 |
| Unsure | 158 (31.5%) | 101 (63.9%) | 57 (36.1%) | |
| Agree | 304 (60.6%) | 169 (55.6%) | 135 (44.4%) | |
| Increased risk of Sudden Infant Death Syndrome with maternal smoking during pregnancy | ||||
| Disagree | 15 (3.0%) | 11 (73.3%) | 4 (26.7%) | .565 |
| Unsure | 62 (12.4%) | 38 (61.3%) | 24 (38.7%) | |
| Agree | 425 (84.7%) | 254 (59.8%) | 171 (40.2%) | |
| Increased risk of lung disease in passive smokers | ||||
| Disagree | 5 (1.0%) | 4 (80.0%) | 1 (20.0%) | .229 |
| Unsure | 44 (8.8%) | 31 (70.5%) | 13 (29.5%) | |
| Agree | 453 (90.2%) | 268 (59.2%) | 185 (40.8%) | |
| Increased risk of heart disease in passive smokers | ||||
| Disagree | 10 (2.0%) | 10 (100.0%) | 0 (0.0%) | .019 |
| Unsure | 51 (10.2%) | 34 (66.7%) | 17 (33.3%) | |
| Agree | 441 (87.8%) | 259 (58.7%) | 182 (41.3%) | |
| Increased risk of lower respiratory tract illnesses in case of paternal smoking | ||||
| Disagree | 5 (1.0%) | 4 (80.0%) | 1 (20.0%) | .022 |
| Unsure | 26 (5.2%) | 22 (84.6%) | 4 (15.4%) | |
| Agree | 471 (93.8%) | 277 (58.8%) | 194 (41.2%) | |
| Advising smoker patients to avoid smoking around children | ||||
| Disagree | 6 (1.2%) | 5 (83.3%) | 1 (16.7%) | .183 |
| Unsure | 14 (2.8%) | 11 (78.6%) | 3 (21.4%) | |
| Agree | 482 (96.0%) | 287 (59.5%) | 195 (40.5%) | |
Attitudes toward tobacco smoking
Interestingly, it was found that less than half of the physicians (42.8%) disagreed or were unsure that the health professionals serve as role models for their patients and the public. As expected, these percentages were significantly higher among the smokers group compared with non-smokers (P-value = .014). Regarding the statement that “a health professional should set a good example by not smoking,” significantly higher percentage of the smokers who reported this statement were disagreed or unsure compared with non-smokers (P-value = .000). The difference between current and non-current smokers regarding the statement “patient’s chances of quitting smoking will increase if a health professional advises him or her to quit” was also statistically significant (P-value = .012), as more of those who disagreed were smokers. As expected, there is a significant difference (P-value = .001) between smokers and non-smokers in the belief that health professionals should routinely advise their smoking patients to quit smoking; a higher percent of those who disagree were smokers.
Surprisingly, 20.9% of physicians were against or unsure about the need to receive a specific training on cessation techniques, and these percentages were borderline significant (higher among smokers, P-value = .055). Minority of the physicians (2.6%) disagreed that health professionals should speak to community groups about smoking, and this was significantly higher among the smokers (P-value = .001). Only a minority of the physicians (3.6%) have negative attitude toward prohibition of smoking in enclosed public places, and this was significantly higher among the smokers (P-value = .000). Surprisingly, 25.9% of physicians were against or unsure that the health warnings on cigarette packages should be in big print, and these percentages were significantly higher among the current smokers (P-value = 0.010). Further details about physicians’ attitude toward smoking are in Table 3.
Table 3.
Smoking attitudes stratified by smoking status of the participants (N = 502).
| Variable | Total, N (%) | Smoker, n (%) | Non-smoker, n (%) | χ2, P-value |
|---|---|---|---|---|
| Health professionals serve as role models for their patients and the public | .014 | |||
| Disagree | 109 (21.7%) | 62 (56.9%) | 47 (43.6%) | |
| Unsure | 106 (21.1%) | 77 (72.6%) | 29 (27.4%) | |
| Agree | 287 (57.2%) | 164 (57.1%) | 123 (42.9%) | |
| Health professionals set a good example by not smoking | <.001 | |||
| Disagree | 41 (8.2%) | 38 (92.7%) | 3 (7.3%) | |
| Unsure | 36 (7.2%) | 26 (72.2%) | 10 (27.8%) | |
| Agree | 425 (84.7%) | 239 (56.2%) | 186 (43.8%) | |
| Patient’s chances of quitting smoking will increase if a health professional advises him or her to quit | .012 | |||
| Disagree | 58 (11.6%) | 44 (75.9%) | 14 (24.1%) | |
| Unsure | 162 (32.3%) | 102 (63.0%) | 60 (37.0%) | |
| Agree | 282 (56.2%) | 157 (55.7%) | 125 (44.3%) | |
| Asking about patients’ smoking habits | .225 | |||
| Disagree | 6 (1.2%) | 3 (50.0%) | 3 (50.0%) | |
| Unsure | 22 (4.4%) | 17 (77.3%) | 5 (22.7%) | |
| Agree | 474 (94.4%) | 283 (59.7%) | 191 (40.3%) | |
| Advising patients to quit smoking | .012 | |||
| Disagree | 16 (3.2%) | 12 (75.0%) | 4 (25.0%) | |
| Unsure | 30 (6.0%) | 25 (83.3%) | 5 (16.7%) | |
| Agree | 456 (90.8%) | 266 (58.3%) | 190 (41.7%) | |
| Smokers are less likely to advise people to stop smoking | .061 | |||
| Disagree | 82 (16.3%) | 59 (72.0%) | 23 (28.0%) | |
| Unsure | 149 (29.7%) | 88 (59.1%) | 61 (40.9%) | |
| Agree | 271 (54.0%) | 156 (57.6%) | 115 (42.4%) | |
| Receiving training on cessation techniques | .055 | |||
| Disagree | 31 (6.2%) | 21 (67.7%) | 10 (23.3%) | |
| Unsure | 74 (14.7%) | 53 (71.6%) | 21 (28.4%) | |
| Agree | 397 (79.1%) | 229 (57.7%) | 168 (42.3%) | |
| Speaking to community groups about smoking | .001 | |||
| Disagree | 13 (2.6%) | 11 (84.6%) | 2 (15.4%) | |
| Unsure | 51 (10.2%) | 41 (80.4%) | 10 (19.6%) | |
| Agree | 438 (87.3%) | 251 (57.3%) | 187 (42.7%) | |
| Prohibition of smoking in enclosed public places | <.001 | |||
| Disagree | 18 (3.6%) | 18 (100.0%) | 0 (0.0%) | |
| Unsure | 32 (6.4%) | 25 (78.1%) | 7 (21.9%) | |
| Agree | 452 (90.0%) | 260 (57.5%) | 192 (42.5%) | |
| Health warnings on cigarette packages in a big print | .010 | |||
| Disagree | 48 (9.6%) | 37 (77.1%) | 11 (22.9%) | |
| Unsure | 82 (16.3%) | 55 (67.1%) | 27 (32.9%) | |
| Agree | 372 (74.1%) | 211 (56.7%) | 161 (43.3%) | |
| Ban of tobacco sales to children and adolescents | .892 | |||
| Disagree | 3 (0.6%) | 2 (66.7%) | 1 (33.3%) | |
| Unsure | 4 (0.8%) | 2 (50.0%) | 2 (50.0%) | |
| Agree | 495 (98.6%) | 299 (60.4%) | 196 (39.6%) | |
| Ban of sport sponsorships by tobacco industry | .030 | |||
| Disagree | 24 (4.8%) | 20 (83.3%) | 4 (16.7%) | |
| Unsure | 62 (12.4%) | 41 (66.1%) | 21 (33.9%) | |
| Agree | 416 (82.9%) | 242 (58.2%) | 174 (41.8%) | |
| Ban on the advertising of tobacco products | .001 | |||
| Disagree | 16 (3.2%) | 15 (93.8%) | 1 (6.2%) | |
| Unsure | 54 (10.8%) | 40 (74.1%) | 14 (25.9%) | |
| Agree | 432 (86.1%) | 248 (57.4%) | 184 (42.6%) | |
| Smoke-free hospitals and health care centers | <.001 | |||
| Disagree | 13 (2.6%) | 13 (100.0%) | 0 (0.0%) | |
| Unsure | 24 (4.8%) | 22 (91.7%) | 2 (8.3%) | |
| Agree | 465 (92.6%) | 268 (57.6%) | 197 (42.4%) | |
| Increase price of tobacco products sharply | <.001 | |||
| Disagree | 143 (28.5%) | 127 (88.8%) | 16 (11.2%) | |
| Unsure | 105 (20.9%) | 62 (59.0%) | 43 (41.0%) | |
| Agree | 254 (50.6%) | 114 (44.9%) | 140 (55.1%) | |
Worksite practice
Most of the physicians (94.8%) were urban resident. Regarding the availability of a smoke-free policy at workplace, 31.9% of participants reported that it was available, while 5.6% self-reported that smoking rooms were available. Interestingly, 45.2% reported that no smoking policy was available. Table 4 presents the smoking practice and policy at workplace by smoking status.
Table 4.
Worksite practice stratified by smoking status of the participants (N = 502).
| Variable | Total, N (%) | Smoker, n (%) | Non-smoker, n (%) | χ2, P-value |
|---|---|---|---|---|
| Workplace/practice location | .773 | |||
| Urban | 476 (94.8%) | 289 (60.7%) | 187 (39.3%) | |
| Rural | 22 (4.4%) | 12 (54.5%) | 10 (45.5%) | |
| Camp | 4 (0.8%) | 2 (50.0%) | 2 (50.0%) | |
| Sort of smoke-free policy available in workplace | .618 | |||
| Smoking policy is available in workplace | 160 (31.9%) | 135 (59.5%) | 92 (40.5%) | |
| No smoking policy is in workplace | 227 (45.2%) | 94 (58.8%) | 66 (41.2%) | |
| Smoking rooms are available | 28 (5.6%) | 20 (71.4%) | 8 (28.6%) | |
| No smoking allowed at all in the building | 87 (17.3%) | 54 (62.1%) | 33 (37.9%) | |
| Availability of traditional remedies (eg, acupuncture, herbal teas) | 43 (8.6%) | 30 (69.8%) | 13 (30.2%) | .187 |
| Availability of self-help materials(eg, health education booklets) | 147 (29.3%) | 87 (59.2%) | 60 (40.8%) | .729 |
| Availability of counseling | 353 (70.3%) | 210 (59.5%) | 143 (40.5%) | .540 |
| Availability of medications (nicotine gum, patch, bupropion) | 129 (25.7%) | 78 (60.5%) | 51 (39.5%) | .977 |
| Usage of traditional remedies (eg, acupuncture, herbal teas) | 38 (7.6%) | 23 (60.5%) | 15 (39.5%) | .982 |
| Usage of self- help materials(eg, health education booklets) | 150 (29.9%) | 82 (54.7%) | 68 (45.3%) | .089 |
| Usage of counseling | 367 (73.1%) | 220 (59.9%) | 147 (40.1%) | .755 |
| Usage of medications (nicotine gum, patch, bupropion) | 108 (21.5%) | 66 (61.1%) | 42 (38.9%) | .857 |
| Preparation physician feels when counseling patients on how to stop smoking | <.001 | |||
| Very well prepared | 231 (46.0%) | 116 (50.2%) | 115 (49.8%) | |
| Somewhat prepared | 204 (40.6%) | 142 (69.6%) | 62 (30.4%) | |
| Not at all prepared | 67 (13.3%) | 45 (67.2%) | 22 (32.8%) | |
| Ever received any formal training in smoking cessation approaches to use with patients | .163 | |||
| No. did not | 285 (56.8%) | 164 (57.5%) | 121 (42.5%) | |
| Formal training during medical study | 61 (12.2%) | 44 (72.1%) | 17 (27.9%) | |
| Formal training during specialization programs | 25 (5.0%) | 17 (68.0%) | 8 (32.0%) | |
| Special conferences, seminars or workshops | 131 (26.1%) | 78 (59.5%) | 53 (40.5%) | |
Water pipe smoking practice
The mean age of starting water pipe smoking was 24.19 ± 7 years old. Nearly, 39% of the physicians were current smoker, and 5% were ex-smokers of water pipe. In the meanwhile, 33.5% were daily smokers, 35.5% were weekly smokers, and 31% were monthly water pipe smokers.
Discussion
Prevalence of smoking among physicians
To the best of our knowledge, this is the first study addressing the issue of smoking among medical doctors in the Palestinian society. One of the main findings was that the prevalence of smoking among physicians is higher than the general population in Palestine and some nearby countries. In our study, non-smokers represented 39.7%. However, the overall prevalence of current smoking (regardless of the type of smoking) was 60.3%, Figure 1. According to the Palestinian Central Bureau of statistics, the percentage of individuals aged 18 years and above that reported as smokers in the State of Palestine was about 22%, of which 27% in the West Bank and 15% in Gaza Strip.16 Data collected in our study showed a high prevalence of water pipe smoking which was equal to cigarettes smoking among physicians, and this is unlike other countries. For example, cigarettes were the most common form of used tobacco products in each of Bahrain, Kuwait, and Saudi Arabia, followed by water pipes then by cigars. In Kuwait, the prevalence of current smoking among physicians was 30.4%, 18.4% of the physicians were of current cigarettes smokers, while 12% of water pipe.17–19 In Egypt, the overall prevalence for current physicians smoking was 51.1%, cigarettes were also found to be the most common type of smoking with prevalence of 37.1% followed by water pipe (12.9%), and 10.7% smoke both of them.20 In Israel, the overall smoking prevalence was lower than our results where only 16.7% of the physicians found to be current smokers.21
The higher prevalence rate of smoking in our study compared with other countries could be explained by the stressful conditions and the overloaded systems on physicians in our hospitals. Furthermore, our political situation could have played a role. These conditions could have constricted the time and place to have some activities to release the stress among physicians other than smoking. Indeed, smoking prevalence was found to be nearly significant in some neighboring Arab countries with unstable political situations. For example, in Egypt, Syria, and Iraq, the prevalence of smoking among male physicians was found to be 90% (40.5% in general male population), 41% (60% in general male population), and 31% (30.84% in general male population), respectively.20,22,23 These results are in accordance with our study which might imply that unstable political conditions could have a role.
Socio-demographic characteristics by smoking status
When stratified by sex, two-thirds of males were current smokers while only one-third of females were current smokers. This could be largely explained by the social unacceptability of female smoking in traditional societies. In Iraq, none of the female physicians were smokers. In Egypt, nearly 22.7% of female physicians were current smokers. In Syria, 11.4% of female physicians were current smokers. In Israel, no significant difference was found between current male and female physicians smoking as 19% of male physicians were current smokers compared with 14% among females.20–23
Compared with a study carried out in Turkey, our study showed that there was no significant difference between different levels of medicine education with slightly higher prevalence of current smoking for higher degree. This is opposite to the results in Turkey, where the smoking rate was found to decrease with increased levels of education.24 In terms of specialty, the highest prevalence reported for surgical one, followed by general practitioner, then medical specialty. This was similar to results in a study carried out in Israel, where internists were less likely to be smokers than their peers in surgical specialties.21
Looking at the Professional status among physicians, we found that the highest prevalence of current smokers belonged to administrative and academic physicians, followed by residents, then attending physicians, and the least belonged to trainee or interns. While in Southwest Saudi Arabia, the highest prevalence of current smokers was among residents.18 Compared with a study conducted in Jordan at King Hussein Medical Center, there was no difference in resident and specialist subgroups.25 However, in Israel, the results were similar to our finding.21 Our results could be explained by that spending more hours under stressful duty like surgical operations may increase the prevalence of smoking.
Cigarettes smoking practice
In our study, 39.4% of the physicians were current cigarettes smokers, while 12.2% of them were ex-cigarettes smokers and 48.4% never tried cigarettes smoking. It is considered high comparing this percentage to Kuwait and Israel. In Kuwait, current cigarette smokers’ physicians were 18.4% while 15.8% were ex-smokers.17 In Israel, 16.7% of the medical physicians were current smokers, 23.3% were past smokers, and 60% were never smokers. In Jordan, the prevalence of current cigarettes smoking at King Hussein Medical Center was a little bit higher (43%) than reported in our study. In Istanbul, it has been found that health care professionals had higher prevalence (43.9% were currently smokers and 15.5% were ex-smokers).17,21,24,26
The mean ± SD age of starting smoking was 20.08 ± 2.95 years. These finding was consistent with other studies performed in Turkey and Laos.27–29 The overall mean ± SD number of cigarettes smoked per day of the currently smokers was 16.5 ± 9.4 in our study. However, for male physicians, it was 16.8 ± 9.5 cigarettes per day, and for females, it was 9.3 ± 8.9. Although not comparable, it worth mentioning that in São Paulo, Brazil, the overall mean ± SD was found to be 16.3 ± 7.8 cigarettes per day. The study reported that females’ mean ± SD daily consumption of cigarettes was 14.1 ± 8.8 cigarettes, compared with 17.7 ± 6.8 among males with no statistically significant differences. In Syria, male current daily smokers were found to smoke 21 ± 0.7 (mean ± SD) cigarettes per day while females reported smoking 14 ± 1.7 (mean ± SD) cigarettes per day.23,29
Reason for starting smoking
The main reason that drives the physicians to smoke was found to be experimenting (57.9%). As well, the majority of them reported that it is the stress that causes them to start smoking (31.8%), which was the most common reason of starting smoking in South Western Saudi Arabia (67.9%). Nearly, 26.4% of smoker physicians stated that the reason was the social pressure; this was the most common reason of starting smoking in Pakistani male physicians and in Eastern Saudi Arabia physicians (66.7%).18,30,31
Knowledge and attitudes
Physicians who smoke were found to be less knowledgeable regarding the hazards of smoking and have less favorable attitude toward tobacco control. This finding was similar to that found in other studies conducted in Kuwait, Bahrain, Japan, Egypt, and Oman. The opposite has been found in a study in Laos where smokers have more positive attitudes toward anti-smoking than non-smokers.19,20,27,31,32 Our results could be explained by that there is a correlation between knowledge, attitude, and practice in human behavior. So having a high level of knowledge might lead to positive attitudes and good practice.
In our study, the majority of the physicians (95.0%) agreed that smoking is harmful to their health which is comparable to the result of a study in Turkey, China, and Iran, where only a slightly (1.2%) of physicians show disagreement to the above statement. In Bosnia, however, nearly all respondents agreed.28,33,34 This high level of agreement may be due to their high level of education regarding issues related to health. In this study, non-smokers were more likely to have knowledge regarding the increased risk of lung and heart diseases in non-smoking adults and lower respiratory tract illnesses such as pneumonia in exposed children than smokers. And this has also been found by a study in China.34 Nearly, 60.6% of physicians knew that neonatal death is associated with passive smoking, while in China only 49% of physicians knew that, and in Lakes region only 27.2% of the physicians had no knowledge about this.28,35 This low level of knowledge may be explained by the fact that neonatal death is multi-factorial process not directly due to smoking effect.
In this study, the lowest agreement (57.8%) was for the statement “health professionals who smoke are less likely to advise people to stop smoking”; this finding was similar to the one found in studies performed in Kuwait and Bahrain and in China.17,34 On the other hand, less than half of respondents did not believe that an increase in tobacco prices would have an impact on the prevalence of smoking; this was similar to the research findings in Istanbul and in Lakes region (41.6%).24,28 These responses might be explained by that smoking is an addictive behaviors and physicians are usually considered a higher economical class were price elevation is not an issue of concern for them.
The majority of our physicians (84.7%) agreed that a health professional should set a good example by not smoking; this was similar to the results found in a Chinese study (80.0%). In Italy and Laos, most of physicians believed on this also. However, significantly higher percentages of the current smokers who answer this statement were disagreed or unsure such as the findings from an Estonian study.27,35–37 Furthermore, the majority of the physicians in our study (92.6%) have positive attitude toward having a smoke-free hospitals and health care centers, and it was found that a same percent of Chinese physicians had also agreed on this. In contrast, in Mexico only 65% were in favor of banning smoking from their workplaces.34,38 Physicians who were current smokers were more likely to be against this, because they spend much of their stressed times in the hospitals when they will be in need for smoking.
The need for specific training for counseling patients to stop smoking was reported by the majority (84.4%) of physicians in this study. This means that physicians are welling to quit smoking only under some kind of encouragements and motivations which emphasizes indeed for such a training and intervention program for them. More non-current smokers had positive attitude toward prohibition of smoking in enclosed public places than current smokers did; this is comparable to findings from other studies in the Arab world.17,20,23,19
Worksite practice
Less than half of physicians (43.2%) received any formal training in smoking cessation approaches to use with patients, the same has been found in a study in Bosnia, but this percent was higher than that found in Iraq (33.3%), Kuwait (12.7%), Bahrain (11.6%), China (27.6%), São Paulo (7%), and Mongolia (11.2%), while lower than that in Riyadh (68%).1,17,22,34,39 Regarding the preparation that the physicians feel when they are counseling their patients on how to stop smoking, less than half of physicians (46.0%) self-reported that they feel very well prepared. This was lower than that found in Syria (61.4%) and Italy, but was higher than that in Egypt (16.8%), Yerevan (35%), and Bosnia (36%).20,23,27,33,40
Interestingly, 45.2% of participants noted that no smoking policy was available at their workplace which is in accordance with another study in China (50%).32
This study could be limited by the non-probability sampling technique which might limit the generalizability of the findings. However, this technique was used due to inaccessibility to every physician, and that trying to visit physicians at their workplace could have been related to a significant effect on the their response rate due to their occupancy and time needed for questionnaire filling. Although the response rate was nearly 83.6% (502 subjects recruited out of 600 invited), we do believe that this was a very good response rate for such an informative group of medical doctors.
Conclusions and Recommendations
The prevalence of smoking among our physicians is higher than that of the general population and the nearby countries. Non-smokers had more positive attitudes and higher support toward anti-smoking compared with current smokers. Many physicians believed that they are not yet ready to be health educators on smoking.
We believe that policymakers, especially those working in health fields, are the most appropriate people to be role models for stopping smoking because they would have a greater appreciation of the regulations due to their position. This will lead to the implementation of the government’s smoke-free policy throughout the entire health system in Palestine. We strongly recommend that courses in tobacco control treatment should be offered or even mandated within the curriculum and to become one of the requirements for graduation or specialization. A focused and sustained anti-smoking campaign by the health facilities and the Ministry of Health may also be useful in controlling the smoking epidemic among the medical physicians.
Acknowledgments
The authors are grateful to all participants in this study for the time they devoted and their understanding.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: HAZ and SM designed and coordinated the study protocol. HAZ drafted the manuscript. AH and DS collected the data. HAZ, AH, and DS conducted the statistical analysis. AH and DS helped in drafting the manuscript. AH and MG helped in drafting the final version of the manuscript and editing the writing. All authors read and approved the final manuscript.
Availability of Data and Materials: Data are all contained within the article.
Ethical Approval: The study aims, protocols, and the informed consent forms were approved by the Institutional Review Board (IRB) at An-Najah National University (IRB archived number 08/June/2014).
Informed Consent: All authors gave their consent for publication of the manuscript to HAZ to be the corresponding author.
ORCID iD: Hamzeh Al Zabadi  https://orcid.org/0000-0002-0721-9561
https://orcid.org/0000-0002-0721-9561
References
- 1. Whitehouse E, Lai J, Golub JE, Farley JE. A systematic review of the effectiveness of smoking cessation interventions among patients with tuberculosis. Pub Health Action. 2018;8:37–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mistry R, Jones AD, Pednekar MS, et al. Antenatal tobacco use and iron deficiency anemia: integrating tobacco control into antenatal care in urban India. Reprod Health. 2018;15:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Khefacha Aissa S, Ghali H, Ben Rejeb M, et al. Smoking attitudes and behavior of the hospital staff Sahloul (Sousse, Tunisia). Rev Mal Respir. 2018;35:256–263. [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization. Tobacco. http://www.who.int/en/news-room/fact-sheets/detail/tobacco. Accessed July 22, 2014.
- 5. World Health Organization. Tobacco or Health Program: Guidelines for Controlling and Monitoring the Tobacco Epidemic. Geneva, Switzerland: World Health Organization; 1997. [Google Scholar]
- 6. Center for Disease Control and Prevention. 2006. Surgeon General’s Report: The Health Consequences of Involuntary Exposure to Tobacco Smoke. Atlanta, GA: Center for Disease Control and Prevention; 2014. [PubMed] [Google Scholar]
- 7. Fowler G. Educating physicians in smoking cessation. Tobacco Control. 1993;2:5–6. [Google Scholar]
- 8. Kawakami M, Nakamura S, Fumimoto H, Takizawa J, Baba M. Relation between smoking status of physicians and their enthusiasm to offer smoking cessation advice. Intern Med. 1997;36:162–165. [DOI] [PubMed] [Google Scholar]
- 9. Almerie MQ, Matar HE, Salam M, et al. Cigarettes and waterpipe smoking among medical students in Syria: a cross-sectional study. Int J Tuberculosis Lung Dis. 2008;12:1085–1091. [PMC free article] [PubMed] [Google Scholar]
- 10. Van Reek J, Adriaanse H. Smoking by physicians in Scandinavia: 1952-1989. Scand J Social Med. 1991;19:256–259. [DOI] [PubMed] [Google Scholar]
- 11. Scott HD, Tierney JT, Buechner JS, Waters WJ., Jr. Smoking rates among Rhode Island physicians: achieving a smoke-free society. Am J Prevent Med. 1992;8:86–90. [PubMed] [Google Scholar]
- 12. Samuels N. Smoking among hospital physicians in Israel and their attitudes regarding anti-smoking legislation. Public Health. 1997;111:285–288. [DOI] [PubMed] [Google Scholar]
- 13. Naing L, Winn T, Rusli BN. Practical issues in calculating the sample size for prevalence studies. Arch Orofacial Sci. 2006;1:9–14. [Google Scholar]
- 14. Regional Office for the Eastern Mediterranean; World Health Organization. Global health professionals survey. https://www.who.int/tobacco/surveillance/ghps/en/. Published 2005.
- 15. SPSS Inc. SPSS 16 for Windows. Statistical Package for the Social Sciences. Chicago, IL: SPSS Inc; 2007. www.spss.com. [Google Scholar]
- 16. Palestinian Central Bureau of Statistics. Final Report of the Palestinian Family Survey 2010. Ramallah, Palestine: Palestinian Central Bureau of Statistics; 2013. [Google Scholar]
- 17. Behbehani NN, Hamadeh RR, Macklai NS. Knowledge of and attitudes towards tobacco control among smoking and non-smoking physicians in 2 Gulf Arab states. Saudi Med J. 2004;25:585–591. [PubMed] [Google Scholar]
- 18. Mahfouz AA, Shatoor AS, Al-Ghamdi BR, et al. Tobacco use among health care workers in southwestern Saudi Arabia. Biomed Res Int. 2013;2013:960292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bener A, Gomes J, Anderson JA, Abdullah S. Smoking among health professionals. Med Educ. 1994;28:151–157. [DOI] [PubMed] [Google Scholar]
- 20. Sabra AA. Smoking attitudes, behaviours and risk perceptions among primary health care personnel in urban family medicine centers in Alexandria. J Egypt Pub Health Assoc. 2007;82:43–64. [PubMed] [Google Scholar]
- 21. Shkedy Y, Feinmesser RM, Mizrachi A. Smoking habits among Israeli hospital physicians: a survey and historical review. Israel Med Assoc J. 2013;15:339–341. [PubMed] [Google Scholar]
- 22. Baey HA, Nadhim N, Wahhudi MM, Hashim HM, Ali OH, Shamkhi BA. Smoking among health care providers, identification of associated factors in Hilla city during the year 2011. Med J Babylon. 2011;8:69–81. [Google Scholar]
- 23. Maziak W, Mzayek F, Asfar T, Hassig SE. Smoking among physicians in Syria: do as I say, not as I do! Ann Saudi Med. 1999;19:253–256. [DOI] [PubMed] [Google Scholar]
- 24. Tas D, Okutan D, Kaya H, Kartaloglu Z, Bozkanat E. Smoking prevalence among military health personnel in Istanbul. Tur Toraks Der. 2009;10:15–19. [Google Scholar]
- 25. El-Khushman HM, Sharara AM, Al-Laham YM, Hijazi MA. Cigarette smoking among health care workers at King Hussein Medical Center. J Hosp Med. 2008;3:281–284. [DOI] [PubMed] [Google Scholar]
- 26. Shishani K, Nawafleh H, Sivarajan Froelicher E. Jordanian nurses’ and physicians’ learning needs for promoting smoking cessation. Prog Cardiovasc Nurs. 2008;23:79–83. [DOI] [PubMed] [Google Scholar]
- 27. Sychareun V, Phengsavanh A, Hansana V, Phommachanh S, Mayxay M, Tomson T. Health policymakers’ knowledge and opinions of physicians smoking and tobacco policy control in Lao PDR. BMC Pub Health. 2012;12:816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Demiralay R. The behavior and attitude of physicians in the lakes region towards smoking. Turkish J Med Sci. 2003;33:329–334. [Google Scholar]
- 29. Guazzelli AC, Terra Filho M, Fiss E. Tabagismo entre médicos da Região do ABC Paulista. J Brasil Pneumol. 2005;31:516–522. [Google Scholar]
- 30. Al-Mobeeriek A, Al-Zaki A, Al-Duhailan L, Al-Habboubi T. Prevalence of smoking among health care providers in eastern province, Saudi Arabia. Pak Oral Dental J. 2008;28:295–300. [Google Scholar]
- 31. Al-Lawati JA, Nooyi SC, Al-Lawati AM. Knowledge, attitudes and prevalence of tobacco use among physicians and dentists in Oman. Ann Saudi Med. 2009;29:128–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Meshefedjian GA, Gervais A, Tremblay M, Villeneuve D, O’Loughlin J. Physician smoking status may influence cessation counseling practices. Can J Pub Health. 2010;101:290–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hodgetts G, Broers T, Godwin M. Smoking behaviour, knowledge and attitudes among family medicine physicians and nurses in Bosnia and Herzegovina. BMC Fam Pract. 2004;5:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhou J, Abdullah AS, Pun VC, Huang D, Lu S, Luo S. Smoking status and cessation counseling practices among physicians, Guangxi, China, 2007. Prevent Chronic Dis. 2010;7:A15. [PMC free article] [PubMed] [Google Scholar]
- 35. Li C. A case study of barriers to implementing a smoke free policy in community health service centers in Wuxi, China [electronic thesis and dissertation repository]. Emory University, Atlanta, GA. http://discovere.emory.edu/primo_library/libweb/action/display.do?tabs=detailsTab&ct=display&fn=search&doc=ETD%2f25593%2f945kf&indx=1&recIds=ETD%2f25593%2f945kf&recIdxs=0&elementId=0&renderMode=poppedOut&displayMode=full&frbrVersion=&frbg=&&dscnt=0&scp.scps=scope%3A%28repo%29%2Cscope%3A%2801EMORY_ALMA%29%2CEmory_PrimoThirdNode&tb=t&vl(38512462UI1)=all_items&vid=discovere&mode=Basic&srt=rank&tab=emory_catalog&dum=true&vl(freeText0)=A%20case%20study%20of%20barriers%20to%20implementing%20a%20smoke%20free%20policy%20in%20community%20health%20service%20centers%20in%20Wuxi%2C%20China&dstmp=1543868699354. Published 2007.
- 36. Ficarra MG, Gualano MR, Capizzi S, et al. Tobacco use prevalence, knowledge and attitudes among Italian hospital health care professionals. Eur J Pub Health. 2011;21:29–34. [DOI] [PubMed] [Google Scholar]
- 37. Parna K, Rahu K, Rahu M. Smoking habits and attitudes towards smoking among Estonian physicians. Public Health. 2005;119:390–399. [DOI] [PubMed] [Google Scholar]
- 38. Tapia-Conyer R, Cravioto P, de la Rosa B, Galvan F, Garcia-de la, Torre G, Kuri P. Cigarette smoking: knowledge and attitudes among Mexican physicians. Salud Publica Mex. 1997;39:507–512. [DOI] [PubMed] [Google Scholar]
- 39. Al-Shahri MZ, Al-Almaie SM. Promotion of non-smoking: the role of primary health care physicians. Ann Saudi Med. 1997;17:515–517. [DOI] [PubMed] [Google Scholar]
- 40. Perrin PC, Merrill RM, Lindsay GB. Patterns of smoking behavior among physicians in Yerevan, Armenia. BMC Pub Health. 2006;6:139. [DOI] [PMC free article] [PubMed] [Google Scholar]


