Abstract
Objective:
This pre-planned secondary analysis of geriatric interdisciplinary home rehabilitation, which was initially found to shorten the postoperative length of stay in hospital for older individuals following hip fracture, investigated whether such rehabilitation reduced the numbers of complications, readmissions, and total days spent in hospital after discharge during a 12-month follow-up period compared with conventional geriatric care and rehabilitation.
Design:
Randomized controlled trial.
Setting:
Geriatric department, participants’ residential care facilities, and ordinary housing.
Subjects:
Individuals aged ⩾70 years with acute hip fracture (n = 205) were included.
Intervention:
Geriatric interdisciplinary home rehabilitation was individually designed and aimed at early discharge with the intention to prevent, detect, and treat complications after discharge.
Main measures:
Complications, readmissions, and days spent in hospital were registered from patients’ digital records and interviews conducted during hospitalization and at 3- and 12-month follow-up visits.
Results:
No significant difference in outcomes was observed. Between discharge and the 12-month follow-up, among participants in the geriatric interdisciplinary home rehabilitation group (n = 106) and control group (n = 93), 57 (53.8%) and 44 (47.3%) had complications (P = 0.443), 46 (43.4%) and 38 (40.9%) fell (P = 0.828), and 38 (35.8%) and 27 (29.0%) were readmitted to hospital (P = 0.383); the median total days spent in hospital were 11.5 and 11.0 (P = 0.353), respectively.
Conclusion:
Geriatric interdisciplinary home rehabilitation for older individuals following hip fracture resulted in similar proportions of complications, readmissions, and total days spent in hospital after discharge compared with conventional geriatric care and rehabilitation.
Keywords: Falls, home rehabilitation, randomized controlled trial, hip fracture
Introduction
During the last decade, accelerated discharge has been promoted and home rehabilitation teams have been set up to reduce the length of stay in hospital for older individuals with hip fracture. Home rehabilitation for older people living in ordinary housing and without severe cognitive impairment can improve physical activity,1 reduce the length of hospital stay,2 increase independence and confidence in performance of activities of daily living (ADL) without falling,1,2 and reduce the burden on caregivers.3
In a primary analysis, we recently showed that older individuals, including those with cognitive impairment and those living in residential care facilities, who undergo geriatric interdisciplinary home rehabilitation after hip fracture regain their walking ability comparably to those receiving conventional geriatric care and rehabilitation. The intervention group also had a significantly shorter postoperative length of hospital stay (median, six days).4
However, the evidence to support team-based home rehabilitation for older individuals with hip fracture is weak,5 and complications after discharge have been described in only limited detail. No effect on falls, mortality after discharge, or readmission has been reported.2,6,7 Furthermore, no previous study of team-based home rehabilitation has included people with severe cognitive impairment/dementia or those living in residential care facilities. As scientific data regarding complications are deficient,8 we sought to evaluate complications after discharge among persons who had sustained hip fractures, including individuals with cognitive impairment/dementia and those living in residential care facilities.
The aim of this secondary analysis was to evaluate whether geriatric interdisciplinary home rehabilitation for older individuals following hip fracture was associated with fewer complications, readmissions, and total days spent in hospital after discharge during a 12-month follow-up period compared with conventional geriatric care and rehabilitation.
Material and methods
Study design and participants
The randomized controlled trial of which this study is a part has been reported on previously,4 and the method is described briefly here. People with acute hip fracture aged 70 years and older and living in the municipality of Umeå were included. The study was conducted at the Geriatric Department of Umeå University Hospital, Sweden, and in participants’ homes. Participants, including those with cognitive impairment or dementia, were admitted from ordinary housing and residential care facilities. Those who fractured their hips in the hospital and those with pathological fractures (n = 17) were excluded from the study.
Procedure
Participants were consecutively randomized to the control treatment (conventional geriatric care and rehabilitation) or intervention (conventional geriatric care and rehabilitation with geriatric interdisciplinary home rehabilitation after discharge). The nurse on duty selected an envelope containing a concealed sequentially numbered lot before each patient arrived at the geriatric ward. Randomization was stratified according to housing (residence in a care facility or ordinary housing) and type of fracture (cervical or trochanteric).
Two researchers, blinded to group allocation, assessed the participants during hospitalization and at 3- and 12-month follow-up visits. The study was approved by the Ethical Committee of the Faculty of Medicine at Umeå University (DNR 08-053M) and registered with Current Controlled Trials Ltd (ISRCTN 15738119).
Control treatment
Geriatric care and rehabilitation consisted of a multidisciplinary and multifactorial intervention programme implemented at the ward beginning in 2000.9,10 The staff worked in teams to conduct comprehensive geriatric assessment, with regular meetings and individual care planning.
Intervention
Participants in the intervention group received the same geriatric care and rehabilitation as did those in the control group, but with the aim of early discharge from the hospital and continuation of rehabilitation in their homes for a maximum of 10 weeks. Participants were discharged from hospital when no serious medical obstacle existed and when they could manage basic transfers (such as getting in and out of bed and using the bathroom), and/or when they had the help they needed at home from next of kin or social home services.
The intervention began directly after discharge and has been described in detail previously.4 In short, the geriatric interdisciplinary home rehabilitation team, trained in comprehensive geriatric assessment, implemented the intervention with regular meetings and evaluation of participants’ individualized goals. The team focused on prevention, detection, and treatment of complications after discharge. All team members reported symptoms, such as delirium, pain, and sleeping disturbances, to the nurse and geriatrician, who assessed and treated the participants to minimize the risk of further complications. The nurse and geriatrician also evaluated pain medication use and participants’ ability to handle their medicines safely.
Baseline assessment
Data on heart disease at baseline included those on atrial fibrillation, cardiac failure, angina pectoris, previous heart surgery, pacemaker use, and history of myocardial infarction. Independence in personal ADL (bathing, dressing, toileting, transfer, continence, and feeding) was assessed using the Katz ADL Index11 and recorded as a binary variable.
The attending anaesthesiologist assessed participants’ general health before surgery using the American Society of Anesthesiologists Classification.12 Prescribed drugs at discharge were classified according to the Anatomical Therapeutic Chemical Classification System. Drug prescriptions were recorded as ‘yes’ or ‘no’; doses were not registered, and pro re nata drugs were not included. Length of stay in hospital was measured from admission to the geriatric ward until discharge.
Outcome assessments
An experienced geriatrician working at the ward and not blinded to group allocation registered all complications from patients’ digital records after study completion using a preset protocol. Complications, including orthopaedic complications and medical incidents, were classified as present or absent. Infections were divided into four groups: pneumonia/chest infections, urinary tract infections, superficial wound infections, and deep wound infections. Myocardial infarction and cardiac failure were registered separately and also as cardiovascular events. Participants with cardiac failure at baseline who were treated because of exacerbation of the disease during follow-up were considered to have cardiac failure as a complication. Data on falls were collected by asking participants at follow-up visits whether they had sustained any falls and by analysing their medical charts; in cases of cognitive impairment, next of kin and staff members were also asked about participants’ falls. The total number of falls, including syncopal falls, was recorded for events when participants unintentionally came to rest on the floor or ground.13 The total number of days spent in hospital and the number of readmissions during the year after discharge were registered. Delirium diagnoses during follow-up were based on the Organic Brain Syndrome (OBS) Scale14 and Mini-Mental State Examination (MMSE).15 These data were analysed by a blinded geriatrician to determine whether the participants fulfilled the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV)16 criteria. All complications were registered until the end of the study or until the participant declined to continue, died, or left the study for other reasons.
Statistical analysis
Baseline characteristics, complications, readmissions, and days in hospital were compared between the geriatric interdisciplinary home rehabilitation and control groups. Student’s t-test for independent samples was used when comparing normally distributed continuous variables. The Mann–Whitney U test was used for non-normally distributed continuous variables. Pearson’s chi-square test or Fisher’s exact test was used for dichotomous data. Subgroup analyses stratified according to types of housing and fracture comparing the numbers of complications, readmissions, and days spent in hospital between the intervention and control groups were performed.
A binary logistic model was used to calculate odds ratios of falling after discharge according to group allocation. In this model, observation time was registered as the time from discharge until the end of the study or until the participant declined participation, died, or left the study. Correlations between the covariates in the model were tested using Pearson’s and Spearman’s coefficients. The first model was adjusted for age and gender. The final model was adjusted for age, gender, observation time, and significant differences between the intervention and control groups at baseline (e.g. use of analgesics, antidepressants, and Parkinson medication).
All analyses were based on the intention-to-treat principle, that is, all available data were used according to initial allocation and irrespective of level of attendance. The significance level was set at P ⩽ 0.05. All tests were two tailed, and analyses were performed using the SPSS version 23.0 software (IBM Corporation, Armonk, NY, USA).
Results
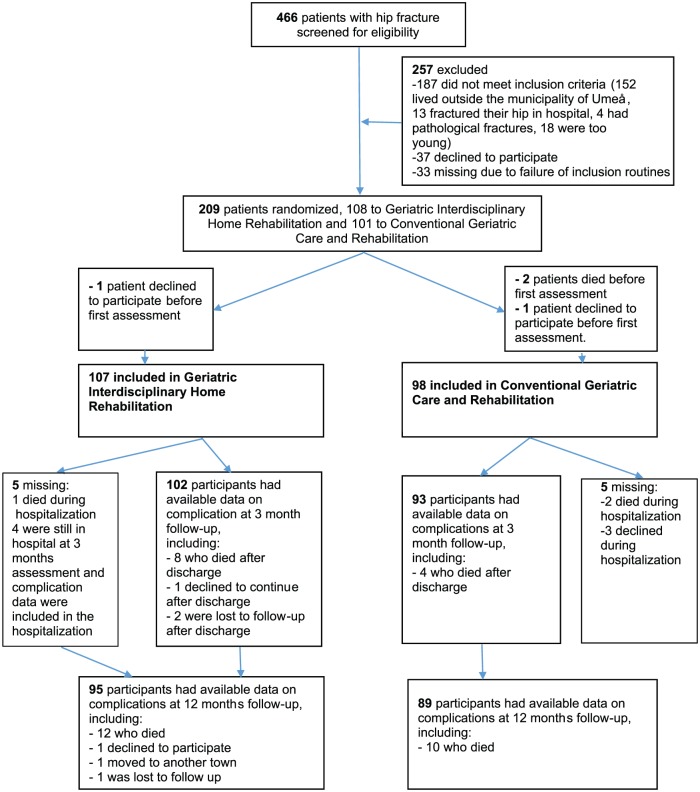
Of 466 people screened for eligibility, 205 persons were included (Figure 1). Losses and exclusions after randomization and periods of recruitment and follow-up have been described previously.4 The use of antidepressants, analgesics, and Parkinson medication differed between groups at baseline (Table 1).
Figure 1.
Flowchart showing the randomization and follow-ups at 3 and 12 months.
Table 1.
Baseline characteristics.
| Total |
GIHR |
Control |
P | |
|---|---|---|---|---|
| n = 205 | n = 107 | n = 98 | ||
| Age, mean ± SD (years) | 82.9 ± 6.7 | 83.2 ± 7.0 | 82.6 ± 6.4 | 0.543 |
| Females, n (%) | 147 (71.7) | 79 | 68 | 0.582 |
| Cervical fracture, n (%) | 148 (72.2) | 78 | 70 | 0.938 |
| Trochanteric fracture, n (%) | 57 (27.8) | 29 | 28 | 0.938 |
| Independent in P-ADL, n (%) | 92 (44.9) | 45 | 47 | 0.479 |
| Independent walking indoors, n (%) | 180 (87.8) | 95 | 85 | 0.815 |
| Living alone, n (%) | 147 (71.7) | 78 | 69 | 0.810 |
| Living in ordinary housing, n (%) | 142 (69.3) | 71 | 71 | 0.428 |
| Diagnoses and medical conditions | ||||
| Cancer, n (%) | 12 (5.9) | 6 | 6 | 1.000 |
| Dementia, n (%) | 103 (50.2) | 57 | 46 | 0.444 |
| Depression, n (%) (n = 203) | 77 (37.9) | 47 | 30 | 0.068 |
| Diabetes, n (%) | 32 (15.6) | 17 | 15 | 1.000 |
| Heart disease, n (%) | 105 (51.2) | 53 | 52 | 0.715 |
| Previous hip fracture, n (%) | 35 (17.1) | 20 | 15 | 0.647 |
| Previous wrist fracture, n (%) | 23 (11.2) | 9 | 14 | 0.267 |
| Pulmonary disease, n (%) | 25 (12.2) | 12 | 13 | 0.815 |
| Stroke, n (%) | 45 (22.0) | 21 | 24 | 0.502 |
| Number of comorbidities | ||||
| ⩾3, n (%) | 120 (58.5) | 66 | 54 | 0.416 |
| Assessments | ||||
| ASA grade 3–4, n (%) (n = 200) | 117 (58.5) | 61 | 56 | 1.000 |
| Barthel ADL-index, median (IQR) | 18 (13–20) | 18 (13–20) | 18 (13–20) | 0.961 |
| GDS, median (IQR) (n = 174) | 4.0 (2–6) | 4.0 (2–6) | 4.0 (2–6.2) | 0.269 |
| MMSE, median (IQR) (n = 199) | 19.0 (11–25) | 18.0 (11–25) | 19.0 (11–25) | 0.925 |
| Operative methods | ||||
| Internal fixation, n (%) | 48 (23.4) | 26 | 22 | 0.883 |
| Hemiarthroplasty, n (%) | 86 (42.0) | 43 | 43 | 0.694 |
| Sliding hip screw, n (%) | 41 (20.0) | 23 | 18 | 0.701 |
| Other methods, n (%) | 30 (14.6) | 15 | 15 | 0.950 |
| Concomitant fractures at baseline | ||||
| Pelvic fracture, n (%) | 1 (0.5) | 1 | 0 | |
| Proximal humerus fracture, n (%) | 3 (1.5) | 1 | 2 | |
| Wrist fracture, n (%) | 7 (3.4) | 5 | 2 | |
| Other fractures, n (%) | 3 (1.5) | 1 | 2 | |
| Sum | 14 (6.8) | 8 | 6 | |
| Medications at discharge | ||||
| Analgesics (ASA excluded), n (%) | 177 (86.3) | 87 | 90 | 0.047* |
| Antidepressants, n (%) | 75 (36.6) | 49 | 26 | 0.007* |
| Benzodiazepines, n (%) | 27 (13.2) | 15 | 12 | 0.866 |
| Beta-blockers, n (%) | 76 (37.1) | 42 | 34 | 0.596 |
| Diuretics, n (%) | 70 (34.1) | 36 | 34 | 0.991 |
| Neuroleptics, n (%) | 23 (11.2) | 10 | 13 | 0.505 |
| Parkinson medications, n (%) | 11 (5.4) | 10 | 1 | 0.020* |
GIHR: geriatric interdisciplinary home rehabilitation; SD: standard deviation; P-ADL: personal activities of daily living; ASA: acetylsalicylic acid; ASA grade: American Society of Anesthesiologists Classification; ADL: activities of daily living; GDS: Geriatric Depression Scale; IQR: interquartile range; MMSE: Mini-Mental State Examination.
Numbers in parentheses after a characteristic indicate that there are missing values. P = Differences between control and GIHR group according to Pearson’s chi-square, Student’s t-test, Mann–Whitney U test or Fisher’s exact test as appropriate.
P < 0.05.
No significant difference was present between the geriatric interdisciplinary home rehabilitation group (n = 106) and the control group (n = 93) in terms of complications or readmissions after discharge (Table 2). In total, 57 (53.8%) participants in the intervention group and 44 (47.3%) participants in the control group had complications (medical and surgical) after discharge (P = 0.443). After adjustment for age, gender, baseline differences, and observation time, the risk of falling during the period from discharge to the 12-month follow-up did not differ between the intervention and control groups (46/106 vs. 38/93; odds ratio = 0.99, 95% confidence interval = 0.53–1.88). Subgroup analyses stratified according to types of housing and fracture revealed no difference in the number of complications, readmissions, or days spent in hospital between the intervention and control groups (data not shown).
Table 2.
Complications during hospitalization and 12-month follow-up.
| Complications | During hospitalization |
Discharge–3 months |
3–12 months |
Discharge–12 months |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GIHR |
Control |
P | GIHR |
Control |
P | GIHR |
Control |
P | GIHR |
Control |
P | |
| n = 107 | n = 98 | n = 102 | n = 93 | n = 95 | n = 89 | n = 106 (%) | n = 93 (%) | |||||
| Infection | 51 | 41 | 0.486 | 13 | 9 | 0.653 | 27 | 23 | 0.820 | 36 (33.9) | 30 (32.3) | 0.917 |
| Pneumonia/chest infection | 13 | 9 | 0.646 | 3 | 1 | 0.623 | 8 | 9 | 0.888 | 11 (10.4) | 10 (10.8) | 1.000 |
| Urinary tract infection | 38 | 28 | 0.361 | 9 | 8 | 1.000 | 23 | 17 | 0.509 | 28 (26.4) | 23 (24.7) | 0.913 |
| Superficial wound infection | 4 | 4 | 1.000 | 0 | 0 | 0 | 1 | 0.484 | 0 | 1 (1.1) | 0.467 | |
| Deep wound infection | 2 | 1 | 1.000 | 1 | 0 | 1.000 | 0 | 0 | 1 (0.9) | 0 | 1.000 | |
| Cardiovascular event | 10 | 8 | 0.959 | 3 | 1 | 0.623 | 10 | 5 | 0.344 | 12 (11.3) | 6 (6.4) | 0.344 |
| Cardiac failure | 10 | 7 | 0.751 | 2 | 0 | 0.498 | 9 | 4 | 0.303 | 10 (9.4) | 4 (4.3) | 0.256 |
| Myocardial infarction | 1 | 1 | 1.000 | 1 | 1 | 1.000 | 2 | 1 | 1.000 | 3 (2.8) | 2 (2.2) | 1.000 |
| Deep vein thrombosis | 0 | 1 | 0.478 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| Pulmonary emboli | 2 | 0 | 0.499 | 0 | 1 | 0.477 | 0 | 0 | 0 | 1 (1.1) | 0.467 | |
| Stroke | 1 | 1 | 1.000 | 0 | 0 | 4 | 4 | 1.000 | 4 (3.8) | 4 (4.3) | 1.000 | |
| Gastric ulcer | 2 | 1 | 1.000 | 0 | 0 | 2 | 1 | 1.000 | 2 (1.9) | 1 (1.1) | 1.000 | |
| Decubital ulcers | 27 | 20 | 0.513 | 7 | 7 | 1.000 | 8 | 7 | 1.000 | 13 (12.3) | 13 (14.0) | 0.883 |
| Fallers | 24 | 19 | 0.717 | 26 | 22 | 0.896 | 32 | 29 | 0.999 | 46 (43.4) | 38 (40.9) | 0.828 |
| Falls | 33 | 27 | 0.662 | 44 | 36 | 0.773 | 119 | 77 | 0.768 | 163 | 113 | 0.700 |
| Additional fracture | 1 | 0 | 1.000 | 6 | 1 | 0.121 | 7 | 5 | 0.856 | 13 (12.3) | 6 (6.5) | 0.250 |
| Luxation | 2 | 0 | 0.499 | 2 | 0 | 0.498 | 0 | 0 | 2 (1.9) | 0 | 0.500 | |
| Reoperation | 5 | 4 | 1.000 | 5 | 1 | 0.215 | 3 | 4 | 0.714 | 8 (7.5) | 5 (5.4) | 0.741 |
| Deceased | 1 | 2 | 0.607 | 8 | 4 | 0.466 | 12 | 10 | 0.949 | 20 (18.9) | 14 (15.1) | 0.600 |
| Delirium | 84 | 69 | 0.242 | 37 (95) | 32 (88) | 0.835 | 32 (80) | 21 (79) | 0.104 | 47 (49.5)(n = 95) | 38 (42.7)(n = 89) | 0.439 |
| Days with delirium, median (IQR) | 3.0 (1–7) | 3.0 (0–7) | 0.745 | |||||||||
| LOS, median (IQR) | 17.0 (12–26) | 23.0 (17–32) | 0.003 | |||||||||
| Readmission after discharge | 15 | 10 | 0.542 | 27 | 23 | 0.820 | 38 (35.8) | 27 (29.0) | 0.383 | |||
| Number of readmissions after discharge | 17 | 13 | 0.443 | 41 | 40 | 0.729 | 58 | 53 | 0.426 | |||
| Days in hospital after discharge | 218 | 140 | 0.384 | 342 | 362 | 0.717 | 560 | 502 | 0.353 | |||
| Median days in hospital (IQR) after discharge | 9.0 (7–21) | 9.5 (2.5–29) | 0.384 | 10.0 (3–19) | 8.0 (2–29) | 0.717 | 11.5 (5–20) | 11.0 (3–36) | 0.353 | |||
GIHR: geriatric interdisciplinary home rehabilitation; IQR: interquartile range; LOS: length of stay.
Numbers in parentheses indicate that there are missing values. P = differences between control and GIHR group according to Pearson’s chi-square, Student’s t-test, Mann–Whitney U test, or Fisher’s exact test as appropriate. Length of stay = from admission to the geriatric ward until discharge.
Discussion
This secondary analysis showed that geriatric interdisciplinary home rehabilitation for older individuals with hip fracture did not reduce the number of complications, readmissions, or days spent in hospital after discharge compared with conventional geriatric care and rehabilitation.
Similarly, two previous studies found no significant difference in complications during acute hospital stay, readmissions, falls, or mortality after discharge between team-based home rehabilitation and control groups of older people with hip fracture.3,6 The length of follow-up for falls and readmissions, and the methodology used for data analysis, differed between these studies and this study, which renders comparison of the results difficult. One-year mortality rates were lower in the previous studies3,6 than in the present study. In another team-based home rehabilitation study conducted by Ziden et al.,7 the number of reported falls during the period from discharge to the 12-month follow-up was similar to that in our study and the mortality rate was lower; the authors did not report the number of readmissions. One possible explanation for the differences in mortality is that the previous team-based home rehabilitation studies3,6,7 excluded the most fragile individuals, those with dementia, and those living in residential care facilities. People with dementia represent a large proportion of older individuals with hip fracture.17 We considered the inclusion of people with dementia and those living in residential care facilities in this study to be important to improve the generalizability of the results. Previous studies have also indicated that such individuals benefit from rehabilitation after hip fracture,18–20 although the evidence is not strong.21
This study confirmed the high risk of falling after hip fracture among older individuals; 84/199 (42%) participants fell again during the period from discharge to the 12-month follow-up. This fall rate is higher than the expected fall rate among individuals in the community,22,23 which is not unexpected considering that the group included people from ordinary housing and residential care facilities. The total numbers of falls and individuals who fell in this study are comparable to the results of a previous randomized controlled trial with an in-patient multidisciplinary intervention, although the study populations differed.24 This study included individuals with both trochanteric and cervical hip fractures, whereas the previous study included only those with cervical fractures, and the proportion of individuals with dementia was larger in this study.
A reduced length of stay in hospital has also been reported among individuals with stroke and early supported discharge.25 The authors of a Cochrane report concluded that a co-ordinated multidisciplinary team can reduce the length of stay in hospital with no adverse impact on readmission, but also no effect on mortality.25 However, the participants included in that study were younger and had moderate disabilities, in contrast to the group of frail older individuals participating in the present study.
No significant difference in outcomes between the intervention and control groups was found in this study. One explanation might be that both groups initially received geriatric care and rehabilitation in hospital according to a multidisciplinary, multifactorial intervention programme. This programme has successfully reduced the occurrence of in-patient complications, including falls; it has also improved mobility and ADL performance in the short and long terms compared with conventional care.9,10,26 In addition, the presence of the geriatric interdisciplinary home rehabilitation team in the participants’ homes might has resulted in the detection of more complications and led to readmissions, contributing to information bias. Another possible explanation for the intervention’s inability to prevent complications and readmissions in this group of old people is that it was not sufficiently long or comprehensive.
Several multidisciplinary rehabilitation studies10,27–29 and cohort studies30–33 including old people with hip fracture have registered medical and orthopaedic complications only during acute hospital stay. However, a recent retrospective cohort study by Hansson et al.34 showed an association between complications registered ⩽six months after fracture and loss of function one year after fracture. This finding indicates the importance of evaluating complications after discharge in future studies.
The most serious consequence after hip fracture is death, and a shorter time in hospital might even be harmful for some people. In a recent study, Nordström et al.35 found an association between mortality and length of stay in hospital ⩽10 days for those discharged to short-term nursing homes. The median length of hospital stay in our study group was >10 days,4 and subgroup analyses according to types of housing and fracture revealed no difference between intervention and control groups in the number of complications, readmissions, or total days spent in hospital for one year after inclusion in the study.
The strengths of our study are that data on all complications were collected from interviews with participants, staff members, and next of kin and from medical records and analysed systematically. Furthermore, the participants were assessed by blinded researchers, and those with dementia and/or cognitive impairment were included. The study also has some limitations. Selection bias affected the group of participants with trochanteric fracture, as only those who required longer rehabilitation periods in hospital were eligible for randomization. This bias did not affect the comparison between the intervention and control groups, but may have altered external validity. Furthermore, randomization was not completely successful, as baseline medication prescriptions differed significantly between the intervention and control groups. No correction was made for multiple comparisons, but the regression analysis was adjusted for the differences at baseline.
Another limitation was that the ward staff were not blinded to group allocation, and the geriatricians are responsible for discharge handled in both groups, which may have influenced lengths of stay. Seven persons randomized to geriatric interdisciplinary home rehabilitation never received the team-based intervention, although all of these participants were included in the analysis. Six of these participants remained in hospital because of a lack of social services and were judged not to need geriatric interdisciplinary home rehabilitation once they were discharged. One participant was missed. In addition, fall calendars were not used, and the number of falls was likely underestimated considering the high proportion of cognitively impaired participants. Rib and vertebral fractures are known to be poorly documented and were probably under-reported because people with these fractures do not always seek medical care. Furthermore, the limited statistical power concerning complications in this study implies that the results should be interpreted with caution.
In conclusion, geriatric interdisciplinary home rehabilitation for older individuals with hip fracture, including people with cognitive impairment/dementia and those living in residential care facilities, resulted in similar proportions of complications, readmissions, and total days spent in hospital after discharge as did conventional geriatric care and rehabilitation. The high frequency of complications among individuals with hip fracture indicates that interventions aiming to prevent complications after discharge need to be more comprehensive than in this study. Further research investigating reasons for falls and mortality is required.
In addition, further analyses of subgroups of older individuals with hip fracture to determine who benefits the most from team-based geriatric interdisciplinary home rehabilitation, and examination of cost-effectiveness and effects on participants’ quality of life, would be of interest.
Clinical messages.
Geriatric interdisciplinary home rehabilitation, which was initially found to shorten the postoperative length of stay in hospital for older individuals following hip fracture, resulted in similar proportions of complications after discharge as did conventional geriatric care and rehabilitation.
Multiple complications after discharge are common among individuals with hip fracture, and the best way of reducing their occurrence remains unclear.
Acknowledgments
The authors thank all study participants, the staff at the geriatric ward, and the home rehabilitation team at the University Hospital of Umeå. The authors thank Helen Abrahamsson, Eva Elinge, and Anita Persson for their co-operation.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the University of Umeå and County Council of Västerbotten, the Foundation of the Medical Faculty, the Swedish Dementia Association, the Swedish Research Council 2014 (grant K2014-99X-22610-01-6), and the Strategic Research Program in Care Sciences, Sweden.
ORCID iD: Monica Berggren  https://orcid.org/0000-0001-5529-0648
https://orcid.org/0000-0001-5529-0648
References
- 1. Ziden L, Frändin K, Kreuter M. Home rehabilitation after hip fracture. A randomized controlled study on balance confidence, physical function and everyday activities. Clin Rehabil 2008; 22: 1019–1033. [DOI] [PubMed] [Google Scholar]
- 2. Crotty M, Whitehead CH, Gray S, et al. Early discharge and home rehabilitation after hip fracture achieves functional improvements: a randomized controlled trial. Clin Rehabil 2002; 16: 406–413. [DOI] [PubMed] [Google Scholar]
- 3. Crotty M, Whitehead C, Miller M, et al. Patient and caregiver outcomes 12 months after home-based therapy for hip fracture: a randomized controlled trial. Arch Phys Med Rehabil 2003; 84: 1237–1239. [DOI] [PubMed] [Google Scholar]
- 4. Karlsson Å, Berggren M, Gustafson Y, et al. Effects of geriatric interdisciplinary home rehabilitation on walking ability and length of hospital stay after hip fracture: a randomized controlled trial. J Am Med Dir Assoc 2016; 17: 464.e9–464.e15. [DOI] [PubMed] [Google Scholar]
- 5. Donohue K, Hoevenaars R, McEachern J, et al. Home-based multidisciplinary rehabilitation following hip fracture surgery: what is the evidence? Rehabil Res Pract 2013; 2013: 875968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tinetti ME, Baker DI, Gottschalk M, et al. Home-based multicomponent rehabilitation program for older persons after hip fracture: a randomized trial. Arch Phys Med Rehabil 1999; 80: 916–922. [DOI] [PubMed] [Google Scholar]
- 7. Ziden L, Kreuter M, Frändin K. Long-term effects of home rehabilitation after hip fracture – 1-year follow-up of functioning, balance confidence, and health-related quality of life in elderly people. Disabil Rehabil 2010; 32: 18–32. [DOI] [PubMed] [Google Scholar]
- 8. Swedish Council on Health Technology Assessment. Rehabilitation of older people with hip fracture-interdisciplinary teams: a systematic review. Report number 235, 2015. Stockholm: Swedish Council on Health Technology Assessment (SBU). [Google Scholar]
- 9. Lundström M, Olofsson B, Stenvall M, et al. Postoperative delirium in old patients with femoral neck fracture: a randomized intervention study. Aging Clin Exp Res 2007; 19: 178–186. [DOI] [PubMed] [Google Scholar]
- 10. Stenvall M, Olofsson B, Lundström M, et al. A multidisciplinary, multifactorial intervention program reduces postoperative falls and injuries after femoral neck fracture. Osteoporos Int 2007; 18: 167–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA 1963; 185: 914–919. [DOI] [PubMed] [Google Scholar]
- 12. Owens WD, Felts JA, Spitznagel EL, et al. ASA physical status classifications: a study of consistency of ratings. Anesthesiology 1978; 49: 239–243. [DOI] [PubMed] [Google Scholar]
- 13. Jensen J, Lundin-Olsson L, Nyberg L, et al. Fall and injury prevention in older people living in residential care facilities. A cluster randomized trial. Ann Intern Med 2002; 136: 733–741. [DOI] [PubMed] [Google Scholar]
- 14. Berggren D, Gustafson Y, Eriksson B, et al. Postoperative confusion after anesthesia in elderly patients with femoral neck fractures. Anesth Analg 1987; 66: 497–504. [PubMed] [Google Scholar]
- 15. Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12: 189–198. [DOI] [PubMed] [Google Scholar]
- 16. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association, 2000. [Google Scholar]
- 17. Seitz DP, Adunuri N, Gill SS, et al. Prevalence of dementia and cognitive impairment among older adults with hip fractures. J Am Med Dir Assoc 2011; 12: 556–564. [DOI] [PubMed] [Google Scholar]
- 18. Huusko TM, Karppi P, Avikainen V, et al. Randomised, clinically controlled trial of intensive geriatric rehabilitation in patients with hip fracture: subgroup analysis of patients with dementia. BMJ 2000; 321: 1107–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stenvall M, Berggren M, Lundström M, et al. A multidisciplinary intervention program improved the outcome after hip fracture for people with dementia – subgroup analyses of a randomized controlled trial. Arch Gerontol Geriat 2012; 54: e284–e289. [DOI] [PubMed] [Google Scholar]
- 20. Seitz DP, Gill SS, Austin PC, et al. Rehabilitation of older adults with dementia after hip fracture. J Am Geriatr Soc 2016; 64: 47–54. [DOI] [PubMed] [Google Scholar]
- 21. Smith TO, Hameed YA, Cross JL, et al. Enhanced rehabilitation and care models for adults with dementia following hip fracture surgery. Cochrane Database Syst Rev 2015; 6: CD010569. [DOI] [PubMed] [Google Scholar]
- 22. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med 1988; 319: 1701–1707. [DOI] [PubMed] [Google Scholar]
- 23. Campbell AJ, Borrie MJ, Spears GF, et al. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing 1990; 19: 136–141. [DOI] [PubMed] [Google Scholar]
- 24. Berggren M, Stenvall M, Olofsson B, et al. Evaluation of a fall-prevention program in older people after femoral neck fracture: a one-year follow-up. Osteoporos Int 2008; 19: 801–809. [DOI] [PubMed] [Google Scholar]
- 25. Langhorne P, Baylan S. Early Supported Discharge T. Early supported discharge services for people with acute stroke. Cochrane Database Syst Rev 2017; 7: CD000443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stenvall M, Olofsson B, Nyberg L, et al. Improved performance in activities of daily living and mobility after a multidisciplinary postoperative rehabilitation in older people with femoral neck fracture: a randomized controlled trial with 1-year follow-up. J Rehabil Med 2007; 39: 232–238. [DOI] [PubMed] [Google Scholar]
- 27. Vidan M, Serra JA, Moreno C, et al. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc 2005; 53: 1476–1482. [DOI] [PubMed] [Google Scholar]
- 28. Watne LO, Torbergsen AC, Conroy S, et al. The effect of a pre- and postoperative orthogeriatric service on cognitive function in patients with hip fracture: randomized controlled trial (Oslo Orthogeriatric Trial). BMC Med 2014; 12: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Prestmo A, Hagen G, Sletvold O, et al. Comprehensive geriatric care for patients with hip fractures: a prospective, randomised, controlled trial. Lancet 2015; 385: 1623–1633. [DOI] [PubMed] [Google Scholar]
- 30. Roche JJ, Wenn RT, Sahota O, et al. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 2005; 331: 1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pedersen SJ, Borgbjerg FM, Schousboe B, et al. A comprehensive hip fracture program reduces complication rates and mortality. J Am Geriatr Soc 2008; 56: 1831–1838. [DOI] [PubMed] [Google Scholar]
- 32. Dy CJ, Dossous PM, Ton QV, et al. The medical orthopaedic trauma service: an innovative multidisciplinary team model that decreases in-hospital complications in patients with hip fractures. J Orthop Trauma 2012; 26: 379–383. [DOI] [PubMed] [Google Scholar]
- 33. Sathiyakumar V, Greenberg SE, Molina CS, et al. Hip fractures are risky business: an analysis of the NSQIP data. Injury 2015; 46: 703–708. [DOI] [PubMed] [Google Scholar]
- 34. Hansson S, Rolfson O, Åkesson K, et al. Complications and patient-reported outcome after hip fracture. A consecutive annual cohort study of 664 patients. Injury 2015; 46: 2206–2211. [DOI] [PubMed] [Google Scholar]
- 35. Nordström P, Michaelsson K, Hommel A, et al. Geriatric rehabilitation and discharge location after hip fracture in relation to the risks of death and readmission. J Am Med Dir Assoc 2016; 17: 91.e1–e7. [DOI] [PubMed] [Google Scholar]