Abstract
Background:
The outcomes after posterior cruciate ligament reconstruction (PCLR) have been shown to be inferior to those of anterior cruciate ligament reconstruction. There is a lack of knowledge regarding prognostic factors of PCLR outcomes.
Purpose:
To explore the effect of injury mechanism and concomitant ligament injuries on patient-reported outcomes at 2-year follow-up after PCLR.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
A total of 373 patients who underwent primary PCLR and who were registered in the Norwegian Knee Ligament Registry were included. The Knee injury and Osteoarthritis Outcome Score (KOOS) was used as the patient-reported outcome measure. At 2-year follow-up, 252 patients (68%) had completed the KOOS. Multiple regression analysis was used to evaluate the effects of injury activity and multiligament injuries on the KOOS outcomes.
Results:
In the adjusted and unadjusted regression analyses, patients injured during sports reported significantly better outcome at 2-year follow-up after PCLR than patients injured during other activities (P < .001) according to all KOOS subscales. Adjusted analysis was as follows for the KOOS subscales: Symptoms (regression coefficient [β], 7.0; 95% CI, 1.9-12.2), Pain (β, 13.4; 95% CI, 8.0-18.9), Activities of Daily Living (β, 12.6; 95% CI, 7.1-18.1), Sport/Recreation (β, 15.3; 95% CI, 8.0-22.5), and Quality of Life (β, 13.5; 95% CI, 7.1-20.0). In the unadjusted analysis, patients with isolated PCL injuries reported higher scores in the Sport/Recreation subscale (β, –7.9; 95% CI, –15.5 to –0.3). The difference was not significant in the adjusted analysis. No other significant differences in KOOS outcomes were found between isolated and multiligament injuries.
Conclusion:
Patients injured in sports reported better outcomes at 2 years after PCLR as compared with patients injured in other activities. Multiligament injuries involving the PCL do not seem to predict a worse outcome than for isolated PCL injuries.
Keywords: PCL, knee, ligament registry, multiligament
An injury to the posterior cruciate ligament (PCL) is considered a serious but rare event. This is even more so the case for multiligament knee injuries involving the PCL. Injury to the PCL has been reported to account for 2.4% of American high school knee injuries.27 Another study reported that injury to the PCL occurred in 1% to 44% of all knee injuries.25 The PCL has an intrinsic healing capability; however, healing of the PCL may occur in a nonanatomic position if the injury is not recognized within the first weeks. This can result in an elongated PCL and a knee with increased laxity to posterior translation of the tibia and lack of or reduced function of the healed ligament.6,25,29 In the majority of PCL injuries, there are concomitant injuries to other ligaments, menisci, or cartilage.14,18 Other injured ligaments may not have the same intrinsic healing capability as the PCL, and the combined injuries may lead to a severely destabilized knee. Therefore, multiligament knee injures involving a PCL tear are most often treated surgically.
Over the past few years, there has been an increased focus on PCL reconstruction (PCLR).15,20 The reported outcomes following PCLR are not as good as for anterior cruciate ligament (ACL) reconstruction, and they are far from excellent.19 It is unclear why the outcomes are inferior. In attempts to improve them, new techniques with double-bundle reconstruction have been developed.7,16,26 Most studies conclude that the subjective outcomes following single- and double-bundle reconstruction are similar,7,15,20 although the objective outcomes seem to be better for reconstruction with a double bundle.11,20,26 This may imply that there are other important factors that affect the outcome after injury and reconstruction. To improve future outcomes after PCLR, information about prognostic factors is important.
To our knowledge, no previous studies have investigated prognostic factors for outcomes after PCLR. As reported ACL reconstruction outcomes are superior to those for PCLR, and given that a higher proportion of ACL injuries are caused by sports injuries, injury activity might be of importance for outcome.18 Previous reports on multiligament injuries have shown good to excellent outcome following surgical reconstruction of such severe knee injuries.8,9,13 The objective of the present study was to investigate the effect of injury mechanism (sports vs nonsports injuries) and the severity of the ligament injury (multiligament injuries vs isolated PCL injury) on patient-reported outcome at 2-year follow-up after PCLR.
Methods
Included in this study were patients from the Norwegian Knee Ligament Registry, which was established in 2004. The main objective of the registry was to prospectively register all surgical procedures on knee ligaments in Norway and to monitor the outcomes. Every hospital in Norway reports cruciate ligament reconstructions to the registry; both primary and revision procedures are reported. Approximately 86% of performed procedures are reported to the registry.31 The patients complete the Knee injury and Osteoarthritis Outcome Score (KOOS) questionnaire preoperatively and at 2, 5, and 10 years postoperatively. Informed consent is obtained from all patients. The surgeon completes a form postoperatively, with information regarding the findings and specifications of the performed procedure. The registry has been described in more detail in previous studies.3–5,31
Patients
A total of 373 patients who had undergone primary PCLR were registered in the Norwegian Knee Ligament Registry between 2004 and 2013. In the present study, all patients who completed the KOOS at the 2-year follow-up were included, representing a total of 252 (68%) patients, with a loss to follow-up of 121 (32%) patients. About one-third of the patients had an isolated PCL injury, and two-thirds had a multiligament injury. Only patients treated with repair or reconstruction of the associated injured structures were considered to have multiligament injuries. Baseline characteristics of the included patients and those lost to follow-up are shown in Table 1. The median patient age at the time of surgery was 35 years (range, 14-67 years). Of the patients included, 112 (44%) were female. Grafts used for reconstruction were divided into autologous hamstring or other. This was done because the hamstring is the most prevalent graft used in the registry, and all the other graft options are relatively small in number when each is compared against it.
TABLE 1.
Baseline Characteristics at the Time of PCL Reconstruction of the Patients Included in the Study Cohort and the Patients Lost to Follow-upa
| Study Cohort (n1) | Lost to Follow-up (n2) | |
|---|---|---|
| Age at surgery, y (n1 = 252, n2 = 121), median (range) | 35 (14-67) | 27 (15-62) |
| Time from injury to surgery, mo (n1 = 249, n2 = 118), median (range) | 12 (0-240) | 12 (0-204) |
| Sex: female (n1 = 252, n2 = 121) | 112 (44)b | 37 (31) |
| Activity at time of injury (n1 = 247, n2 = 117) | ||
| Sports | 137 (55)b | 48 (40) |
| Other than sports | 110 (43)b | 69 (57) |
| Unknown | 5 (2) | 4 (3) |
| Concomitant (n1 = 252, n2 = 121) | ||
| Ligament injuryc | ||
| Isolated PCL injury | 79 (31) | 36 (35) |
| Multiligament injury | 173 (69) | 78 (65) |
| Meniscal lesion | 59 (23) | 32 (26) |
| Cartilage lesion | 99 (39) | 40 (33) |
| Other injuryd | 12 (5) | 11 (9) |
| PCL graft (n1 = 242, n2 = 117) | ||
| Hamstrings | 172 (68) | 83 (69) |
| Other | 70 (28) | 34 (28) |
| Unknown | 10 (4) | 4 (3) |
| Preoperative KOOS, mean (95% CI) | ||
| Pain (n1 = 168, n2 = 84) | 60.7 (57.4-67.0) | 64.5 (60.2-68.8) |
| Symptoms (n1 = 171, n2 = 85) | 65.2 (62.5-67.9) | 68.8 (65.2-72.4) |
| ADL (n1 = 167, n2 = 82) | 66.4 (62.9-69.9) | 71.1 (66.5-75.7) |
| Sport/Recreation (n1 = 166, n2 = 83) | 24.6 (20.7-28.5) | 30.9 (25.3-36.5) |
| QoL (n1 = 168, n2 = 84) | 28.1 (25.1-31.1) | 29.8 (25.4-34.2) |
aData are reported as n (%) unless otherwise indicated. ADL, Activities of Daily Living; KOOS, Knee injury and Osteoarthritis Outcome Score; PCL, posterior cruciate ligament; QoL, Quality of Life.
bStatistically significant difference, P < .05.
cAnterior cruciate ligament, medial collateral ligament, lateral collateral ligament, posterolateral corner.
dNeural injury, arterial injury, fracture, tendon rupture.
KOOS Questionnaire
The KOOS questionnaire is a self-administered knee function score consisting of 42 questions divided into 5 subscales: Pain, Symptoms, Activities of Daily Living, Sport/Recreation, and Quality of Life. It was developed in the 1990s by Roos et al.23 The KOOS includes the Western Ontario and McMaster Universities Osteoarthritis Index in its complete and original format, and it is a validated and reliable tool for measuring the knee function of patients with osteoarthritis and for several types of knee injury, including those to the ACL, meniscus, and cartilage.22 Scoring for each subscale ranges from 0 (worst) to 100 (best). A difference of 8 to 10 points in a subscale is usually considered a clinically relevant effect.2 The recommendation is to evaluate each subscale independently when considering outcome measures.22
Statistical Analysis
Statistical analyses were performed with SPSS (v 22.0; IBM). The study’s objective was to evaluate the effect of injury activity and concomitant knee ligament injuries on patient-reported outcome, as measured by KOOS outcomes after PCLR. At first, crude mean KOOS scores for patients with isolated PCL injuries and multiligament injuries were estimated. Then, patients were put into 2 categories: those injured during sports and those injured during other activities. Crude mean KOOS scores were calculated for each activity group. Linear regression analyses were then performed. In unadjusted analyses, the factors of interest (ie, injury activity and multiligament injuries) were included separately as independent variables, with each KOOS subscale as the dependent variable. Based on current literature regarding injury to the ACL and clinical assumption, the following variables were considered possible confounders and predictors for patient-reported outcome: sex, age (continuous variable), time from injury to surgery (continuous variable), concomitant meniscal injury, concomitant cartilage injury, concomitant neural/arterial/tendon injury, and type of PCL graft. These factors were included in the multiple linear regression analyses with the factors of interest as independent variables and with each KOOS subscale as the dependent variable.
Effects of injury activity and multiligament injury on KOOS values were considered statistically significant at P < .05. All crude mean KOOS scores and regression coefficient estimates (β) are presented with 95% CIs.
Results
Activity at Time of Injury
There were 137 (55%) patients injured in sports in our study population, 110 (43%) injured in activities other than sports, and 5 (2%) with unknown activity at the time of injury. Baseline characteristics of the groups injured in sports and other activity showed no significant differences except for a higher proportion of women in the sports group. Complete baseline data are shown in Table 2.
TABLE 2.
Baseline Characteristics of Patients Undergoing PCL Reconstruction by Activity at Time of Injurya
| Sports Injury (n1 = 137) | Other Activity (n2 = 110) | |
|---|---|---|
| Age at surgery, y, median (range) | 35 (14 to 67) | 33 (14 to 65) |
| Time from injury to surgery, mo, median (range) | 24 (0 to 228) | 24 (0 to 240) |
| Sex: female, percentage (95% CI) | 48 (40.8 to 55.2)b | 33 (26.1 to 39.9) |
| Concomitant, percentage (95% CI) | ||
| Ligament injuryc | ||
| Isolated PCL injury | 31 (24.3 to 37.7) | 35 (28.0 to 42.0) |
| Multiligament injury | 69 (62.3 to 75.6) | 65 (58.0 to 72.0) |
| Meniscal lesion | 22 (16.0 to 28.0) | 27 (20.5 to 33.5) |
| Cartilage lesion | 37 (30.0 to 44.0) | 37 (30.0 to 44.0) |
| Other injuryd | 3 (2.6 to 9.4) | 9 (4.8 to 13.2) |
| PCL graft, percentage (95% CI) | ||
| Hamstrings | 69 (62.3 to 75.6) | 68 (61.2 to 74.8) |
| Other | 25 (18.8 to 31.2) | 30 (23.3 to 36.7) |
| Unknown | 6 (2.6 to 9.4) | 2 (–0.1 to 4.1) |
| n3 | n4 | |
| KOOS, preoperative, mean (95% CI) | ||
| Pain (n3 = 129, n4 = 116) | 62.9 (59.2 to 66.6) | 60.4 (56.6 to 64.2) |
| Symptoms (n3 = 132, n4 = 117) | 67.2 (64.1 to 70.3) | 65.7 (62.5 to 68.9) |
| ADL (n3 = 129, n4 = 113) | 69.1 (65.1 to 73.1) | 66.1 (62.1 to 70.1) |
| Sport/Recreation (n3 = 130, n4 = 112) | 27.4 (22.8 to 32.0) | 26.2 (21.5 to 30.9) |
| QoL (n3 = 130, n4 = 115) | 29.4 (25.8 to 33.0) | 27.5 (24.1 to 30.9) |
aADL, Activities of Daily Living; KOOS, Knee injury and Osteoarthritis Outcome Score; PCL, posterior cruciate ligament; QoL, Quality of Life.
bStatistically significant higher number of females in the sport group, P < .05.
cAnterior cruciate ligament, medial collateral ligament, lateral collateral ligament, posterolateral corner.
dNeural injury, arterial injury, fracture, tendon rupture.
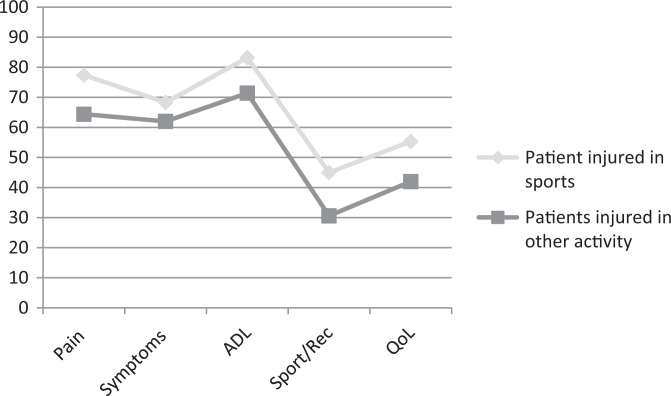
The crude mean KOOS scores at 2-year follow-up for those injured during sports and those injured during other activities are shown in Table 3. Patients injured during sports reported significantly better 2-year outcomes after PCLR than patients injured during other activities according to all KOOS subscales (P < .05 for all) (Figure 1).
TABLE 3.
Crude Mean KOOS at 2-Year Follow-up after PCL Reconstruction by Injury Activitya
| Patients Injured During Sports (n = 137) | Patients Injured During Activities Other Than Sports (n = 109 or 110)b | |||
|---|---|---|---|---|
| KOOS Subscale | Mean | 95% CI | Mean | 95% CI |
| Pain | 77.4 | 74.2-80.6 | 64.4 | 60.0-68.8 |
| Symptoms | 68.3 | 65.0-71.6 | 62.0 | 58.1-65.8 |
| ADL | 83.2 | 79.8-86.6 | 71.4 | 67.0-75.9 |
| Sport/Recreation | 45.0 | 40.1-49.9 | 30.6 | 25.6-30.5 |
| QoL | 55.3 | 51.2-59.4 | 42.0 | 37.3-46.7 |
aADL, Activities of Daily Living; KOOS, Knee injury and Osteoarthritis Outcome Score; PCL, posterior cruciate ligament; QoL, Quality of Life.
bSample sizes differ since valid data were not available for some of the subscales.
Figure 1.
KOOS scores by injury activity 2 years postoperatively. ADL, Activities of Daily Living; KOOS, Knee injury and Osteoarthritis Outcome Score; QoL, Quality of Life; Sport/Rec, Sport/Recreation.
In the unadjusted and adjusted linear regression analyses, injury during sports was associated with significantly better outcome than injury during other activities, per all KOOS subscales (P < .05 for all). The adjusted effects of injury during sports ranged from 7.0 points (95% CI, 1.9-12.2 points) in the KOOS Symptoms subscale to 15.3 points (95% CI, 8.0-22.5 points) in the Sport/Recreation subscale (Table 4).
TABLE 4.
Regression Analyses of the Effect of Activity at Time of Injury and Multiligament Injury on KOOS Scores at 2-Year Follow-upa
| Injury During Sportsb | Multiligament Injuryc | |||||||
|---|---|---|---|---|---|---|---|---|
| KOOS Subscale | n | β | 95% CI | P Value | n | β | 95% CI | P Value |
| Pain | ||||||||
| Unadjusted | 247 | 13.0 | 7.7 to 18.3 | <.001 | 252 | –2.1 | –7.9 to 3.8 | .484 |
| Adjusted | 234 | 13.4 | 8.0 to 18.9 | <.001 | 234 | 1.8 | –4.5 to 8.0 | .576 |
| Symptoms | ||||||||
| Unadjusted | 246 | 6.4 | 1.3 to 11.4 | .013 | 251 | –0.1 | –5.4 to 5.3 | .978 |
| Adjusted | 233 | 7.0 | 1.9 to 12.2 | .008 | 233 | 2.9 | –3.0 to 8.8 | .331 |
| ADL | ||||||||
| Unadjusted | 247 | 11.8 | 6.3 to 17.3 | <.001 | 252 | –4.9 | –10.8 to 1.0 | .105 |
| Adjusted | 234 | 12.6 | 7.1 to 18.1 | <.001 | 234 | 0.8 | –5.4 to 7.1 | .797 |
| Sport/Recreation | ||||||||
| Unadjusted | 246 | 14.4 | 7.4 to 21.5 | <.001 | 251 | –7.9 | –15.5 to –0.3 | .042 |
| Adjusted | 233 | 15.3 | 8.0 to 22.5 | <.001 | 233 | –3.7 | –12.1 to 4.7 | .385 |
| QoL | ||||||||
| Unadjusted | 247 | 13.3 | 7.1 to 19.5 | <.001 | 252 | –5.2 | –11.9 to 1.6 | .132 |
| Adjusted | 234 | 13.5 | 7.1 to 20.0 | <.001 | 234 | –2.6 | –10.0 to 4.8 | .495 |
aAdjusted for sex, age, time from injury to surgery, concomitant meniscal lesions, concomitant cartilage lesions, concomitant neural injury/arterial injury/fracture/tendon rupture, and type of PCL graft. ADL, Activities of Daily Living; KOOS, Knee injury and Osteoarthritis Outcome Score; PCL, posterior cruciate ligament; QoL, Quality of Life.
bOther activity than sports at time of injury used as reference.
cIsolated PCL injury used as reference.
Multiligament Injuries
The study population comprised 79 (31%) isolated PCL injuries and 173 (69%) multiligament injuries. Baseline characteristics of these 2 groups are shown in Table 5. Among female patients, there were more with isolated injuries than multiligament injuries: 46% (95% CI, 37.1%-54.8%) versus 31% (95% CI, 25.3%-36.7%). The delay to surgery was longer for isolated injuries than for multiligament injuries, at a mean of 3.1 years (95% CI, 2.5-3.8 years) versus 1.1 years (95% CI, 0.8-1.4 years). Injuries to the menisci were more frequent among the multiligament injuries than the isolated injuries, with a proportion of 30% (95% CI, 24.3%-35.7%) versus 14% (95% CI, 7.8%-20.1%). Apart from these areas, the isolated injuries and multiligament injuries were similar at baseline (Table 5).
TABLE 5.
Baseline Characteristics of Patients Undergoing PCL Reconstruction by Isolated or Multiligament Injurya
| Isolated PCL Injury (n1 = 122) | Multiligament Injuryb (n2 = 251) | |
|---|---|---|
| Age at surgery, y, median (range) | 29 (14 to 59) | 36 (15 to 67) |
| Time from injury to surgery, mo, median (range) | 36 (0 to 240) | 12 (0 to 228) |
| Sex: % female (95% CI) | 46 (37.1 to 54.8) | 31 (25.3 to 36.7) |
| Activity at time of injury, % of patients (95% CI) | ||
| Sports | 47 (38.1 to 55.9) | 51 (44.8 to 57.2) |
| Other than sports | 51 (42.1 to 59.9) | 47 (40.8 to 53.2) |
| Unknown | 2 (–0.5 to 4.5) | 2 (0.3 to 3.7) |
| Concomitant, % of patients (95% CI) | ||
| Meniscal lesion | 14 (7.8 to 20.1) | 30 (24.3 to 35.7) |
| Cartilage lesion | 35 (26.5 to 43.4) | 38 (32.0 to 44.0) |
| Other injuryc | 1 (–0.8 to 2.8) | 9 (5.5 to 12.5) |
| PCL graft, % of patients (95% CI) | ||
| Hamstrings | 76 (68.4 to 83.6) | 65 (59.1 to 70.9) |
| Other | 24 (16.4 to 31.6) | 30 (24.3 to 35.7) |
| Unknown | 0 | 5 (2.3 to 7.7) |
| n3 | n4 | |
| KOOS, preoperative, mean ± SD | ||
| Pain (n3 = 106, n4 = 146) | 58.4 ± 17.6 | 64.6 ± 23.0 |
| Symptoms (n3 = 107, n4 = 149) | 65.2 ± 16.7 | 67.3 ± 18.7 |
| ADL (n3 = 105, n4 = 144) | 68.1 ± 18.3 | 67.8 ± 25.1 |
| Sport/Recreation (n3 = 106, n4 = 143) | 27.2 ± 22.4 | 26.3 ± 28.0 |
| QoL (n3 = 106, n4 = 146) | 27.7 ± 14.0 | 29.4 ± 23.3 |
aADL, Activities of Daily Living; KOOS, Knee injury and Osteoarthritis Outcome Score; PCL, posterior cruciate ligament; QoL, Quality of Life.
bAnterior cruciate ligament, medial collateral ligament, lateral collateral ligament, posterolateral corner.
cNeural injury, arterial injury, fracture, tendon rupture.
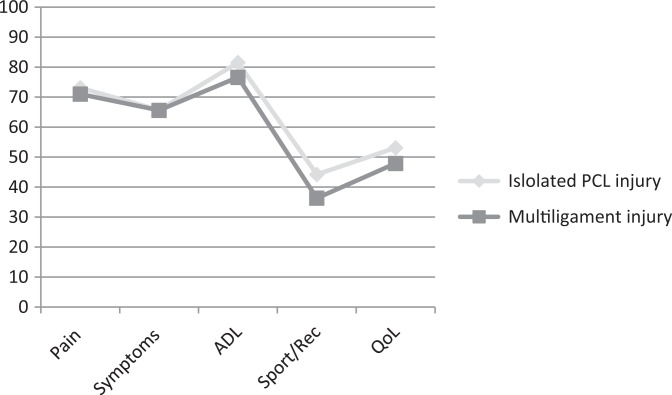
The crude mean KOOS values at 2-year follow-up for those with isolated PCL injury and those with multiligament injury are shown in Table 6. Patients with multiligament injuries had KOOS scores similar to those with isolated PCL injuries at 2-year follow-up (Figure 2).
TABLE 6.
Crude Mean KOOS at 2-Year Follow-up After PCL Reconstruction by Isolated PCL Injury and Multiligament Injurya
| Patients With Isolated PCL Injury (n = 79) | Patients With Multiligament Injury (n = 172 or 173)b | |||
|---|---|---|---|---|
| KOOS Subscale | Mean | 95% CI | Mean | 95% CI |
| Pain | 73.1 | 68.5-77.6 | 71.0 | 67.6-74.4 |
| Symptoms | 65.7 | 61.0-70.4 | 65.6 | 62.7-68.6 |
| ADL | 81.5 | 77.3-85.8 | 76.6 | 73.1-80.1 |
| Sport/Recreation | 44.2 | 37.8-50.6 | 36.3 | 32.0-40.5 |
| QoL | 53.1 | 47.7-58.5 | 47.9 | 44.1-51.8 |
aMultiligament injury: PCL injury combined with other ligament injury (anterior cruciate ligament, medial collateral ligament, lateral collateral ligament, and/or posterolateral corner). ADL, Activities of Daily Living; KOOS, Knee injury and Osteoarthritis Outcome Score; PCL, posterior cruciate ligament; QoL, Quality of Life.
bSample sizes differ since valid data were not available for some of the subscales.
Figure 2.
KOOS scores 2 years postoperatively. ADL, Activities of Daily Living; KOOS, Knee injury and Osteoarthritis Outcome Score; PCL, posterior cruciate ligament; QoL, Quality of Life; Sport/Rec, Sport/Recreation.
In the linear regression analyses, no significant associations were detected between multiligament injury and KOOS scores in any of the subscales, in neither the unadjusted nor the adjusted analyses, except for the Sport/Recreation subscale, where the patients with isolated PCL injury scored 7.9 points (95% CI, 0.3-15.5 points; P = .042) better in the unadjusted analysis (Table 4).
Discussion
The first important finding in this study is that sport injuries have a positive effect on patient-reported outcome following PCLR. This is new and clinically relevant information. In the adjusted analysis, patients injured in sports scored 7.0 to 15.3 points better than those injured in other activities. This was a clinically relevant and statistically significant finding for all KOOS subscales except the Symptom subscale. The most significant differences were in the Sport/Recreation and Quality of Life subscales, which are also the most relevant subscales when evaluating these types of injuries.
We can speculate why patients injured in sports have better outcomes. It possibly has something to do with better baseline fitness and health. Athletes may also have better access to rehabilitation and may be more compliant with their rehabilitation protocols. Athletes are accustomed to, and normally have time to do, their training every day. They are often in the care of physical therapists or athletic trainers with experience in treating sports-related injuries. We did not differentiate among types of sports in this study. As a consequence, there may be significant differences related to the amount of energy involved in the injury that our material did not detect. It could also be that there were a greater number of multiligament injuries among those injured in traffic- or work-related accidents, but this was not statistically significant for our material (Table 5). If there were such a difference, it should not influence the outcomes if we consider the second important finding in this study: patients treated for multiligament injuries had outcomes similar to those treated for an isolated PCL injury. What makes this finding more interesting is that injuries to the menisci were more frequent in multiligament-injured knees in our study than in existing literature.10,18 This is theoretically not in favor of those with multiligament injuries, as supported by 1 study showing a negative effect on patient-reported outcome from cartilage and meniscal injuries in multiligament injuries.10
As with our material, some previous studies have reported good or excellent outcomes following multiligament injuries.8,9,28 This finding is in part difficult to explain. Regarding the effect of cartilage and meniscal lesions, it has previously been shown that the patient-reported outcome for ACL injuries with concomitant meniscal lesions and superficial cartilage lesions is equal to that without such lesions.12,24,30 It might, of course, be that the outcome changes over a longer period of follow-up. One previous study showed that cartilage lesions had no significant effect on outcome at 5 and 9 years after ACL reconstruction.30 In the present study, the frequencies of cartilage injuries were equal between isolated and multiligament injuries (Table 5). It seems likely that the main problem is injury to the ligaments, with PCL injury predicting worse outcome than injury to the other ligaments.
Previous studies have also reported inferior outcomes after PCL versus ACL reconstruction.17,19,21 This indicates that injuries involving the PCL predict a worse outcome than do other ligament injuries. Even so, it is difficult to explain why patients with multiligament injuries report outcomes similar to those of patients with isolated PCL injuries. Time from injury to surgery is longer for the isolated PCL injuries, and this may be part of the explanation. Another important fact is a limitation to the KOOS score. The questionnaire contains no questions regarding change in physical requirements over time. One could speculate that patients with multiligament injuries changed their activities to something less demanding and, as such, had satisfactory scores in the Sport/Recreation and Quality of Life subscales because of lower demand. Better methods of reconstruction and perhaps careful selection of patients are needed to improve the outcome following PCLR and multiligament injuries involving the PCL.
Limitations to this study include the use of registry data. Only those injuries treated surgically are registered, however many isolated PCL injuries are treated nonoperatively. This probably means that only those with the most serious isolated PCL injuries are registered. There was also a 32% loss to follow-up at 2 years. However, those included and those lost to follow-up had similar characteristics, except for younger age and more men among those lost to follow-up. This was also found in other studies.1,18 Another possible weakness is the lack of objective measures, as the KOOS was the only available outcome measure and it was perhaps insufficient for a total evaluation of outcome. However, the KOOS is reliable and valid in evaluating knee injuries, including injuries to ligaments, according to previous studies.2,22 Additionally, in sports, an important outcome is the number of athletes who return to their preinjury activity levels. This is a main parameter that was not available in our material. Information about weight, body mass index, and smoking status is not available, and so far, we have few patients treated with double-bundle reconstruction with 2-year follow-up data. These are examples of variables that might affect outcome in either direction. Finally, in our material, there was a long time from injury to reconstruction. This may have led to a higher number of meniscal and full-thickness cartilage lesions, but it should be equal for both groups.
With the use of multiple regression analysis, there is a chance of more or less important confounders that were not included in the analysis. These can have effects on the result in either direction. Interesting confounders, such as body mass index and activity level, were not included, as these are not available from the Norwegian Knee Ligament Registry. The factors adjusted for in our analysis—age, sex, time from injury to surgery, concomitant meniscal lesions, concomitant cartilage lesions, concomitant neural injury/arterial injury/fracture/tendon rupture, and type of PCL graft—were chosen from what is important in such injuries from clinical experience and existing literature. The importance of activity level on patient-reported outcome is clear for all subscales, and it is less likely that other confounders will change the results significantly.
The clinical implication of this study is that we should have a lower threshold for PCLR regarding patients injured in sports and inform them that they can expect a better result compared with patients injured in other activities. Patients can be informed that the expected outcome of PCLR injury is not necessarily worse in the case of multiligament injuries but that it might reduce their chances for return to preinjury activity levels.
Conclusion
Patients injured in sports reported better outcomes after PCLR at 2 years as compared with patients injured in other activities. Multiligament injuries involving the PCL did not predict a worse outcome than isolated PCL injuries.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Norwegian Data Inspectorate.
References
- 1. Barenius B, Forssblad M, Engstrom B, Eriksson K. Functional recovery after anterior cruciate ligament reconstruction, a study of health-related quality of life based on the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):914–927. [DOI] [PubMed] [Google Scholar]
- 2. Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee injury and Osteoarthritis Outcome Score (KOOS), Knee injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken). 2011;63(suppl 11):S208–S228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Granan LP, Bahr R, Steindal K, Furnes O, Engebretsen L. Development of a national cruciate ligament surgery registry: the Norwegian National Knee Ligament Registry. Am J Sports Med. 2008;36(2):308–315. [DOI] [PubMed] [Google Scholar]
- 4. Granan LP, Forssblad M, Lind M, Engebretsen L. The Scandinavian ACL registries 2004-2007: baseline epidemiology. Acta Orthop. 2009;80(5):563–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Granan LP, Inacio MC, Maletis GB, Funahashi TT, Engebretsen L. Intraoperative findings and procedures in culturally and geographically different patient and surgeon populations: an anterior cruciate ligament reconstruction registry comparison between Norway and the USA. Acta Orthop. 2012;83(6):577–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jacobi M, Reischl N, Wahl P, Gautier E, Jakob RP. Acute isolated injury of the posterior cruciate ligament treated by a dynamic anterior drawer brace: a preliminary report. J Bone Joint Surg Br. 2010;92(10):1381–1384. [DOI] [PubMed] [Google Scholar]
- 7. Jain V, Goyal A, Mohindra M, Kumar R, Joshi D, Chaudhary D. A comparative analysis of arthroscopic double-bundle versus single-bundle posterior cruciate ligament reconstruction using hamstring tendon autograft. Arch Orthop Trauma Surg. 2016;136(11):1555–1561. [DOI] [PubMed] [Google Scholar]
- 8. King AH, Krych AJ, Prince MR, Pareek A, Stuart MJ, Levy BA. Surgical outcomes of medial versus lateral multiligament-injured, dislocated knees. Arthroscopy. 2016;32(9):1814–1819. [DOI] [PubMed] [Google Scholar]
- 9. King AH, Krych AJ, Prince MR, Sousa PL, Stuart MJ, Levy BA. Are meniscal tears and articular cartilage injury predictive of inferior patient outcome after surgical reconstruction for the dislocated knee? Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3008–3011. [DOI] [PubMed] [Google Scholar]
- 10. Krych AJ, Sousa PL, King AH, Engasser WM, Stuart MJ, Levy BA. Meniscal tears and articular cartilage damage in the dislocated knee. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3019–3025. [DOI] [PubMed] [Google Scholar]
- 11. LaPrade CM, Civitarese DM, Rasmussen MT, LaPrade RF. Emerging updates on the posterior cruciate ligament: a review of the current literature. Am J Sports Med. 2015;43(12):3077–3092. [DOI] [PubMed] [Google Scholar]
- 12. LaPrade CM, Dornan GJ, Granan LP, LaPrade RF, Engebretsen L. Outcomes after anterior cruciate ligament reconstruction using the Norwegian Knee Ligament Registry of 4691 patients: how does meniscal repair or resection affect short-term outcomes? Am J Sports Med. 2015;43(7):1591–1597. [DOI] [PubMed] [Google Scholar]
- 13. Levy BA, Dajani KA, Whelan DB, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25(4):430–438. [DOI] [PubMed] [Google Scholar]
- 14. Mair SD, Schlegel TF, Gill TJ, Hawkins RJ, Steadman JR. Incidence and location of bone bruises after acute posterior cruciate ligament injury. Am J Sports Med. 2004;32(7):1681–1687. [DOI] [PubMed] [Google Scholar]
- 15. Montgomery SR, Johnson JS, McAllister DR, Petrigliano FA. Surgical management of PCL injuries: indications, techniques, and outcomes. Curr Rev Musculoskelet Med. 2013;6(2):115–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Noh JH, Yoon KH, Kyung HS, Roh YH, Kang TS. Multiple looping technique for tibial fixation in posterior cruciate ligament reconstruction using free tendon Achilles allograft. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2640–2645. [DOI] [PubMed] [Google Scholar]
- 17. Ochiai S, Hagino T, Senga S, Yamashita T, Ando T, Haro H. Prospective analysis using a patient-based health-related scale shows lower functional scores after posterior cruciate ligament reconstructions as compared with anterior cruciate ligament reconstructions of the knee. Int Orthop. 2016;40(9):1891–1898. [DOI] [PubMed] [Google Scholar]
- 18. Owesen C, Sandven-Thrane S, Lind M, Forssblad M, Granan LP, Årøen A. Epidemiology of surgically treated posterior cruciate ligament injuries in Scandinavia. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2384–2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Owesen C, Sivertsen EA, Engebretsen L, Granan L-P, Årøen A. Patients with isolated PCL injuries improve from surgery as much as patients with ACL injuries after 2 years. Orthop J Sports Med. 2015;3(8):2325967115599539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Qi YS, Wang HJ, Wang SJ, Zhang ZZ, Huang AB, Yu JK. A systematic review of double-bundle versus single-bundle posterior cruciate ligament reconstruction. BMC Musculoskelet Disord. 2016;17:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rochecongar G, Plaweski S, Azar M, et al. Management of combined anterior or posterior cruciate ligament and posterolateral corner injuries: a systematic review. Orthop Traumatol Surg Res. 2014;100(8):S371–S378. [DOI] [PubMed] [Google Scholar]
- 22. Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. [DOI] [PubMed] [Google Scholar]
- 24. Rotterud JH, Sivertsen EA, Forssblad M, Engebretsen L, Aroen A. Effect of meniscal and focal cartilage lesions on patient-reported outcome after anterior cruciate ligament reconstruction: a nationwide cohort study from Norway and Sweden of 8476 patients with 2-year follow-up. Am J Sports Med. 2013;41(3):535–543. [DOI] [PubMed] [Google Scholar]
- 25. Shelbourne KD, Davis TJ, Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries: a prospective study. Am J Sports Med. 1999;27(3):276–283. [DOI] [PubMed] [Google Scholar]
- 26. Spiridonov SI, Slinkard NJ, LaPrade RF. Isolated and combined grade-III posterior cruciate ligament tears treated with double-bundle reconstruction with use of endoscopically placed femoral tunnels and grafts: operative technique and clinical outcomes. J Bone Joint Surg Am. 2011;93(19):1773–1780. [DOI] [PubMed] [Google Scholar]
- 27. Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among US high school athletes, 2005/2006-2010/2011. Med Sci Sports Exerc. 2013;45(3):462–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tardy N, Boisrenoult P, Teissier P, Steltzlen C, Beaufils P, Pujol N. Clinical outcomes after multiligament injured knees: medial versus lateral reconstructions. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):524–531. [DOI] [PubMed] [Google Scholar]
- 29. Tewes DP, Fritts HM, Fields RD, Quick DC, Buss DD. Chronically injured posterior cruciate ligament: magnetic resonance imaging. Clin Orthop Relat Res. 1997;335:224–232. [PubMed] [Google Scholar]
- 30. Ulstein S, Bredland K, Aroen A, Engebretsen L, Rotterud JH. No negative effect on patient-reported outcome of concomitant cartilage lesions 5-9 years after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1482–1488. [DOI] [PubMed] [Google Scholar]
- 31. Ytterstad K, Granan LP, Ytterstad B, et al. Registration rate in the Norwegian Cruciate Ligament Register: large-volume hospitals perform better. Acta Orthop. 2012;83(2):174–178. [DOI] [PMC free article] [PubMed] [Google Scholar]