Abstract
Background:
There are limited data on the use of healthy lifestyles among adults who are candidates for primary prevention of atherosclerotic cardiovascular disease (ASCVD) with statin therapy due to a 10-year predicted risk ≥7.5%. We determined the prevalence of healthy lifestyle factors and their association with incident ASCVD and all-cause mortality in the Reason for Geographic and Racial Differences in Stroke study participants (n=5,709).
Methods:
Lifestyle factors (non-obese waist circumference, physical activity ≥5 times-per-week, non-smoking, low saturated-fat-intake, highest Mediterranean diet score quartile) were assessed during an in-home examination and interviewer-administered questionnaires. Adjudicated incident ASCVD (nonfatal/fatal stroke, nonfatal myocardial infarction or coronary heart disease death) and all-cause mortality were identified through active participant follow-up.
Results:
Overall, 5.1%, 28.9%, 36.9%, 21.7% and 7.5% had 0, 1, 2, 3, and ≥4 of the 5 healthy lifestyle factors studied. There were 377 incident ASCVD events (203 CHD events and 174 strokes) and 471 deaths during 5.8 and 6.0 median years of follow-up, respectively. ASCVD incidence rates (95% CI) per 1,000-person-years associated with 0, 1, 2, 3 and ≥4 healthy lifestyles were 13.4 (7.3–19.5), 12.8 (10.4–15.2), 11.0 (9.0–12.9), 11.0 (8.3–13.7), and 8.7 (4.9–12.4), respectively. Mortality rates associated with 0, 1, 2, 3 and ≥4 healthy lifestyles were 20.6 (13.3–27.8), 15.9 (13.3–18.5), 13.1 (10.9–15.2), 12.6 (9.9–15.2) and 9.2 (5.3–13.2) per 1,000-person-years, respectively. The use of more healthy lifestyles were associated with lower risks for ASCVD and mortality after multivariable adjustment.
Conclusion:
Healthy lifestyles are underutilized among high-risk US adults and may substantially reduce their ASCVD risk.
Keywords: healthy lifestyle, statins, atherosclerotic cardiovascular disease, cholesterol treatment guidelines, atherosclerotic cardiovascular disease risk, mortality
1.1. Introduction
The 2013 American College of Cardiology/American Heart Association (ACC/AHA) Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults recommends consideration of statin therapy for primary prevention of atherosclerotic cardiovascular disease (ASCVD) for individuals aged 40–79 years without a history of diabetes, with low-density-lipoprotein-cholesterol levels between 70 and 189 mg/dL, and a 10-year predicted ASCVD risk ≥7.5%.(1) Prior analyses suggest that many more adults are eligible for statin therapy for the primary prevention of ASCVD using the 2013 ACC/AHA guidelines when compared to the 2001 Adults Treatment Panel III guidelines.(2, 3)
Observational studies and randomized controlled trials (RCTs) demonstrate that lifestyle modification reduces ASCVD risk.(4, 5) In the 2013 ACC/AHA cholesterol treatment guideline, lifestyle modification (i.e., maintaining a heart healthy diet and healthy weight, regular exercise, tobacco smoking avoidance) is emphasized both prior to and in conjunction with the use of lipid-lowering medications.(1) A New England Journal of Medicine survey found that most physicians favored lifestyle modification before initiating statins when presented with the case of a 52-year old male who jogs frequently but has a 10-year predicted risk of 10.9%.(6) Few studies have assessed the prevalence of healthy lifestyle factors among adults recommended statins for primary prevention of ASCVD by the 2013 ACC/AHA cholesterol treatment guidelines. If high-risk individuals practice few healthy lifestyle factors, then increasing the number of healthy lifestyles may provide a large ASCVD and mortality risk reduction, possibly eliminating the need for statins in some individuals. Based on data from the population-based REasons for Geographic And Racial Differences in Stroke (REGARDS) cohort study, we estimated the prevalence of healthy lifestyle factors among candidates for primary prevention of ASCVD with statin therapy due to having a 10-year predicted risk ≥7.5%.(1) Additionally, we determined the association of healthy lifestyles, individually and in combination, with incident ASCVD and all-cause mortality.
1.2. Methods
1.2.1. Study population
The REGARDS study has been described in detail previously.(7) Briefly, 30,239 adults aged ≥45 years were recruited between January 2003 and October 2007 from the 48 contiguous US states and District of Columbia. Residents of the “stroke buckle” (coastal North Carolina, South Carolina, and Georgia) and “stroke belt” (the remainder of North Carolina, South Carolina, and Georgia as well as Alabama, Mississippi, Tennessee, Arkansas and Louisiana) and blacks were oversampled by design. The inclusion criteria applied for the current analyses were chosen to identify candidates for primary prevention of ASCVD with statin therapy due to an estimated 10-year ASCVD risk ≥7.5%. Therefore, we excluded REGARDS participants aged ≥80 years, with a history of ASCVD (coronary heart disease [CHD], revascularization, or stroke ), heart failure, atrial fibrillation, diabetes, or end-stage renal disease (ESRD), Low-density-lipoprotein-cholesterol <70 or ≥190 mg/dL, or taking statins at baseline (Figure 1). Additionally, participants missing data on the Pooled Cohort risk equation components or with a 10-year predicted ASCVD risk <7.5% were excluded leaving 5,709 participants for our analyses.(8) At all participating centers, the Institutional Review Boards governing research in human subjects confirmed that the REGARDS study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. All participants provided written informed consent.
Figure 1.
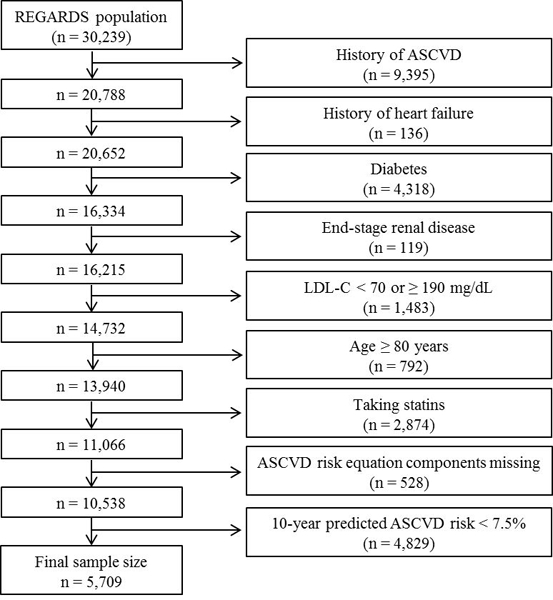
Exclusion cascade for the analysis of healthy lifestyle factors with atherosclerotic cardiovascular disease and all-cause mortality in the REGARDS study (n=5,709).
LDL-C: low-density lipoprotein cholesterol, ASCVD: atherosclerotic cardiovascular disease.
1.2.2. Data collection
Baseline data were collected through a computer-assisted-telephone-interview, self-administered questionnaires and an in-home examination. Information on age, race, sex, education, annual household income, co-morbid conditions [i.e., diabetes, atrial fibrillation, history of stroke, CHD or revascularization procedure, ESRD], antihypertensive medication use, cigarette smoking, and physical activity was self-reported during computer-assisted-telephone-interview administered by trained staff. Participants were asked to fast overnight prior to the in-home examination. During the examination, waist circumference and blood pressure were measured, blood and spot urine samples were collected, and an electrocardiogram was performed by trained technicians. Additionally, the names of all prescription and over-the-counter medications taken during the 2 weeks prior to the in-home visit were recorded based on pill bottle review. Following the in-home examination, participants were provided a Block 98 Food-Frequency Questionnaire to be completed and mailed to the REGARDS coordinating center.(9)
Low-density-lipoprotein-cholesterol was calculated using the Friedewald equation for participants who fasted (≥8 hours) prior to their in-home study visit.(10) Non-high-density-lipoprotein-cholesterol was calculated as total cholesterol minus high-density-lipoprotein-cholesterol for participants who did not fast (n=713). High-sensitivity C-reactive protein (hs-CRP) was measured by particle-enhanced immunonephelometry. Elevated hs-CRP was defined as >3.0 mg/L. The urinary albumin-to-creatinine ratio was calculated. Albuminuria was defined as an albumin-to-creatinine ratio ≥30 mg/g. Estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation.(11) Reduced eGFR was defined as <60 ml/min/1.73 m2. Diabetes was defined by self-report of a prior diagnosis while not pregnant and the use of insulin or oral hypoglycemic medications, a fasting serum glucose ≥126 mg/dL, or a non-fasting serum glucose ≥200 mg/dL. Atrial fibrillation was defined by self-report or electrocardiogram evidence. Participants taking digoxin were considered to have heart failure. Baseline history of CHD was defined by a self-reported history of myocardial infarction or coronary revascularization procedure, or electrocardiogram evidence of myocardial infarction.
1.2.3. Lifestyle factors
Five lifestyle factors were evaluated: waist circumference, physical activity, cigarette smoking, percentage of calories consumed from saturated fat, and adherence to a Mediterranean-style diet. Waist circumference was chosen due to (1) having a stronger association with ASCVD risk than body mass index and (2) evidence that achieving weight reduction goals can improve ASCVD risk factors.(12–15) Waist circumference was measured midway between the lowest rib and the iliac crest while participants were standing. Abdominal obesity was defined by a waist circumference >102 and >88 cm for men and women, respectively. Physical activity was assessed using the question “How many times-per-week do you engage in intense physical activity, enough to work up a sweat?” with responses grouped as “none,” “1-to-4,” or “≥5” times. Current smoking was defined as responding “yes” to both of the following two questions: “Have you smoked at least 100 cigarettes in your lifetime?” and “Do you smoke cigarettes now, even occasionally?” Non-smoking was defined by answering “no” to either question. Thus, former and never smokers were categorized as non-smoking. The Food-Frequency Questionnaire was processed with NutritionQuest software. The average amount of daily calories consumed and dietary nutrients intake were estimated for the year before participants’ in-home visits. The percentage of average daily calories consumed from saturated fat was calculated by multiplying the grams of daily saturated fat intake by 9 calories per gram and dividing this product by average daily calories consumed. Low saturated fat intake, <7%, was defined according to the AHA’s recommended daily intake level for this component of a heart healthy diet.(5) Similar to methods described by Trichopoulou et. al., a Mediterranean diet score was created from 14 all-inclusive food groups and nutrients using a monounsaturated-to-saturated-fats-ratio.(16) Quartiles were created using the distribution of Mediterranean diet scores in the entire REGARDS study population (scores for quartiles 1–4 [lowest-to-highest diet adherence]: <3, 3 to <4, 4 to <6, and ≥6). Healthy lifestyles were defined as non-obese waist circumference, physical activity ≥5 times-per-week, nonsmoking, low saturated fat intake and Mediterranean diet score in the highest quartile.
1.2.4. Outcomes
Two outcomes were studied: incident ASCVD and all-cause mortality. Following the in-home visit, participants or their proxies were contacted twice-annually via telephone to identify potential incident ASCVD events and vital status. Incident ASCVD was defined as a stroke (nonfatal or fatal and ischemic or hemorrhagic) or CHD (nonfatal myocardial infarction or CHD death) event. Medical records were retrieved for adjudication when stroke symptoms with a subsequent hospitalization, stroke, or heart-related hospitalization were reported. Experts adjudicated strokes according to the World Health Organization definition.(17) Strokes reported with symptoms lasting <24 hours and neuroimaging consistent with acute infarct or hemorrhage were categorized as a clinical stroke if the event did not meet the adjudication criteria. Trained clinicians adjudicated CHD events following published guidelines.(18–20) Additionally, stroke, CHD and all-cause deaths were detected and adjudicated using medical records in the last year of life, death certificates, autopsy reports, online sources (e.g., Social Security Death Index) and the National Death Index. Data were available on incident ASCVD events through December 31, 2011 and mortality through March 31, 2012.
1.2.5. Statistical Analysis
The prevalence of the individual and cumulative number of healthy lifestyle factors were calculated. Participant characteristics at baseline were calculated by number of healthy lifestyles (0, 1, 2, 3 or ≥4). Crude ASCVD incidence rates were calculated by levels of each individual lifestyle factor and by the number of healthy lifestyles. Hazard ratios (HRs) and 95% confidence intervals (95% CI) for ASCVD associated with each healthy lifestyle and the cumulative number of healthy lifestyles were estimated using Cox proportional hazard models with progressive adjustment. The initial model (Model 1) included adjustment for age, race, sex, education, income and region of residence. A second model (Model 2) was further adjusted for factors that may be intermediates in the causal pathway including high-density-lipoprotein-cholesterol, total cholesterol, hs-CRP >3 mg/L, systolic and diastolic blood pressure, antihypertensive medication use, albuminuria and eGFR <60 ml/min/1.73 m2. To determine whether the risk for ASCVD associated with healthy lifestyles differed by race and sex, multiplicative interaction was assessed in the full population including product terms between healthy lifestyles and race and, separately, sex (e.g., physical activity*sex). Identical analyses were repeated for all-cause mortality. Ten datasets were imputed using chained equations to account for missing data.(21) Data were missing for <4% of all variables except household income (11.6% missing), saturated fat intake (26.3% missing) and Mediterranean diet score (27.4% missing, Supplemental eTable 1). Analyses were repeated without multiple imputation (i.e., a complete case approach). The proportional hazards assumption was assessed by testing an interaction term between the exposures of interest (e.g., number of healthy lifestyles) and the log of follow-up time. This assumption was not violated. Two-sided p-values ≤0.05 were considered statistically significant. Analyses were conducted using Stata/IC 13.1 (Stata Corporation, College Station, Texas).
1.3. Results
1.3.1. Prevalence of healthy lifestyles
The prevalence of healthy lifestyle factors was 56.9% for non-obesity, 26.1% for physical activity, 80.7% for non-smoking, 7.3% for low saturated fat intake, and 27.7% for Mediterranean diet score in the highest quartile of the overall REGARDS sample population. The majority of participants had 1, 2 or 3 of the 5 healthy lifestyles studied (Figure 2). Overall, 7.5% of participants with a 10-year ASCVD risk ≥7.5% had 4 or 5 of the healthy lifestyles.
Figure 2.
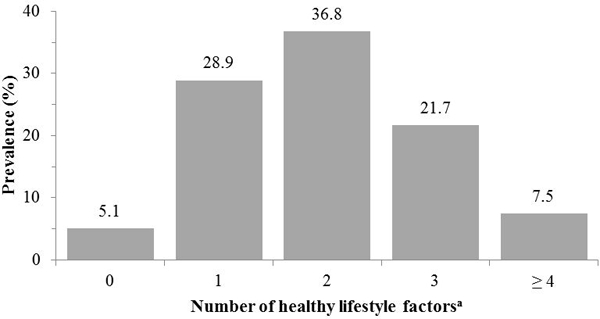
Number of healthy lifestyle factors among participants with a 10-year predicted atherosclerotic cardiovascular disease risk ≥7.5% (n=5,709).
aHealthy lifestyle factors include a non-obese waist circumference (men: <102 cm women: <88 cm), physical activity ≥5 times-per-week, nonsmoking, saturated fat intake <7.0% of daily calories and Mediterranean diet score ≥6.
1.3.2. Participant characteristics
Mean age and high-density-lipoprotein-cholesterol and the proportion of participants living outside of the stroke belt or buckle were higher among those with more healthy lifestyle factors (Table 1). The percentage of participants that were women, black, had less than a high school education, an annual household income <$20,000, elevated hs-CRP, taking antihypertensive medications, albuminuria and the mean levels of systolic and diastolic blood pressure and total cholesterol was lower with an increasing number of healthy lifestyle factors.
Table 1.
aBaseline Characteristics of Participants With a 10-year Predicted Atherosclerotic Cardiovascular Disease Risk ≥7.5% by Number of Healthy Lifestyle Factors (n=5,709).
| Number of healthy lifestyle factorsb | |||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ≥4 | |
| Participant characteristics | (n=289) | (n=1,649) | (n=2,104) | (n=1,238) | (n=429) |
| Age, years | 61.5 (0.4) | 66.0 (0.2) | 66.9 (0.2) | 67.5 (0.2) | 68.3 (0.3) |
| Men, % | 35.3 | 46.4 | 60.8 | 68.6 | 67.7 |
| Black, % | 53.5 | 46.4 | 39.6 | 37.5 | 39.1 |
| Less than a high school education, % | 17.4 | 14.1 | 10.7 | 7.8 | 3.6 |
| Annual household income < $20,000, % | 29.3 | 23.6 | 17.1 | 14.1 | 11.1 |
| Geographic Region, % | |||||
| Stroke belt | 37.1 | 35.4 | 35.8 | 36.3 | 33.1 |
| Stroke buckle | 17.9 | 18.2 | 19.0 | 16.7 | 15.6 |
| Non-belt and non-buckle | 45.0 | 46.4 | 45.2 | 47.0 | 51.3 |
| HDL cholesterol, mg/dL | 46.7 (0.7) | 49.7 (0.4) | 50.9 (0.4) | 52.3 (0.6) | 53.5 (0.9) |
| Total cholesterol, mg/dL | 207.0 (1.9) | 202.7 (0.8) | 202.9 (0.7) | 202.7 (1.0) | 200.7 (1.7) |
| hs-CRP > 3.0 mg/L, % | 64.6 | 53.6 | 36.5 | 28.3 | 20.8 |
| Systolic blood pressure, mm Hg | 133.6 (1.0) | 132.7 (0.4) | 130.3 (0.4) | 129.2 (0.5) | 129.4 (0.8) |
| Diastolic blood pressure, mm Hg | 81.3 (0.6) | 79.5 (0.3) | 77.9 (0.2) | 77.7 (0.3) | 77.1 (0.5) |
| Anti-hypertensive medication use, % | 51.2 | 55.7 | 48.1 | 42.8 | 41.5 |
| ACR ≥ 30 mg/g, % | 17.3 | 13.0 | 10.5 | 8.8 | 8.7 |
| eGFR < 60 ml/min/1.73 m2, % | 5.7 | 8.8 | 7.7 | 6.6 | 6.4 |
ACR: urinary albumin-to-creatinine ratio.
eGFR: estimated glomerular filtration rate.
HDL: high density lipoprotein.
hs-CRP: high sensitivity c-reactive protein.
Numbers in the table are percentages or mean (standard error).
Healthy lifestyle factors include a non-obese waist circumference (men: <102 cm women: <88 cm), physical activity ≥5 times-per-week, nonsmoking, saturated fat intake <7.0% of daily calories and Mediterranean diet score ≥6.
1.3.3. Healthy lifestyle and incident ASCVD
There were 377 incident ASCVD events (203 CHD events and 174 stroke events) over a median follow-up of 5.8 years (maximum: 8.9 years). Supplemental eTable 2 reports the CHD and stroke events for the level of each healthy lifestyle factors and the total number of healthy lifestyle factors among participants with a 10-year predicted ASCVD risk ≥7.5%. ASCVD incidence rates were lower for nonsmokers, those with saturated fat intake <7.0% and higher quartiles of Mediterranean diet adherence (Table 2, top panel). After adjustment for age, race, sex, and region of residence (Model 1), the HR for ASCVD was lower for nonsmokers versus current smokers (p≤0.05) and participants in the highest versus lowest quartile of Mediterranean diet adherence (p≤0.05). Nonsmoking remained associated with a lower HR for ASCVD after further adjustment (Model 2). The incidence of ASCVD was lower among individuals with a higher number of healthy lifestyle factors (Table 2, bottom panel). After multivariable adjustment, the HR (95% CI) for ASCVD associated with 1, 2, 3, and ≥ 4 healthy lifestyles was 0.80 (0.48 – 1.31), 0.66 (0.40 – 1.09), 0.67 (0.39 – 1.15), and 0.54 (0.28 – 1.03), respectively (p-trend≤0.05). The HRs for ASCVD associated with individual and cumulative number of healthy lifestyle factors did not differ by race or sex (all p-interaction>0.05). Results were markedly similar using a complete case analysis (Supplemental eTable 3).
Table 2.
Incidence Rates and Hazard Ratios of Incident Atherosclerotic Cardiovascular Diseasea Associated With Healthy Lifestyle Factors Among Participants With a 10-year Predicted Atherosclerotic Cardiovascular Disease Risk ≥7.5% (n=5,709).
| Events / n at risk |
Crude incidence rate per 1,000 person years (95% confidence interval) |
Hazard Ratio (95% confidence interval) |
||
|---|---|---|---|---|
| Model 1b | Model 2c | |||
| Individual healthy lifestyle factors | ||||
| Waist circumference | ||||
| Obese | 154 / 2,459 | 10.94 (9.21, 12.67) | 1 (ref) | 1 (ref) |
| Non-obese | 223 / 3,250 | 11.73 (10.19, 13.27) | 0.95 (0.77, 1.18) | 1.15 (0.92, 1.44) |
| Physical activity | ||||
| None | 114 / 1,720 | 11.72 (9.55, 13.89) | 1 (ref) | 1 (ref) |
| 1 – 4 times per week | 156 / 2,502 | 10.62 (8.94, 12.31) | 0.88 (0.69, 1.13) | 0.92 (0.72, 1.18) |
| ≥ 5 times per week | 107 / 1,488 | 12.34 (9.99, 14.68) | 0.97 (0.74, 1.27) | 1.05 (0.80, 1.37) |
| p-trend | 0.831 | 0.755 | ||
| Smoking status | ||||
| Current | 91 / 1,100 | 15.40 (12.24, 18.57) | 1 (ref) | 1 (ref) |
| Nonsmoker | 286 / 4,609 | 10.52 (9.30, 11.74) | 0.50 (0.39, 0.64) | 0.53 (0.41, 0.68) |
| Saturated fat intake | ||||
| ≥ 7.0% of daily calories | 355 / 5,292 | 11.61 (10.38, 12.84) | 1 (ref) | 1 (ref) |
| < 7.0% of daily calories | 22 / 417 | 8.78 (4.16, 13.40) | 0.74 (0.42, 1.31) | 0.80 (0.46, 1.40) |
| Mediterranean diet scored | ||||
| Quartile 1 (worse) | 129 / 1,792 | 12.84 (10.48, 15.21) | 1 (ref) | 1 (ref) |
| Quartile 2 | 78 / 1,143 | 11.86 (9.03, 14.70) | 0.92 (0.67, 1.25) | 0.95 (0.70, 1.30) |
| Quartile 3 | 82 / 1,190 | 11.68 (8.90, 14.46) | 0.90 (0.65, 1.23) | 0.96 (0.70, 1.32) |
| Quartile 4 (better) | 88 / 1,584 | 9.30 (7.29, 11.31) | 0.71 (0.53, 0.95) | 0.76 (0.57, 1.02) |
| p-trend | 0.032 | 0.103 | ||
| Number of healthy lifestyle factorse | ||||
| 0 | 21 / 289 | 13.38 (7.32, 19.45) | 1 (ref) | 1 (ref) |
| 1 | 118 / 1,649 | 12.75 (10.35, 15.15) | 0.72 (0.43, 1.18) | 0.80 (0.48, 1.31) |
| 2 | 134 / 2,104 | 10.95 (9.00, 12.90) | 0.54 (0.33, 0.89) | 0.66 (0.40, 1.09) |
| 3 | 81 / 1,238 | 10.99 (8.31, 13.66) | 0.51 (0.30, 0.88) | 0.67 (0.39, 1.15) |
| ≥ 4 | 23 / 429 | 8.66 (4.93, 12.39) | 0.40 (0.21, 0.76) | 0.54 (0.28, 1.03) |
| p-trend | 0.001 | 0.036 | ||
Incident atherosclerotic cardiovascular disease: a stroke (nonfatal or fatal and ischemic or hemorrhagic) or CHD (nonfatal myocardial infarction or CHD death) event.
Model 1: adjustment for age, race, sex, education, income and geographic region of residence.
Model 2: adjustment for Model 1 variables plus high-density lipoprotein and total cholesterol, c-reactive protein >3 mg/L, systolic and diastolic blood pressure, antihypertensive medication use, albumin-to-creatinine ratio ≥30 g/mg and estimated glomerular filtration rate <60 ml/min/1.73 m2.
Quartiles determined using all participants.
Mediterranean diet score cut-points: [quartile 1 (low) to quartile 4 (high)] <3, 3 to <4, 4 to <6, and ≥6.
Number of healthy lifestyle factors: the sum of a non-obese waist circumference (<102 cm for men and <88 cm for women), physical activity ≥ 5 times per week, nonsmoking, saturated fat intake < 7.0% of average daily calories and Mediterranean diet score in quartile 4.
1.3.4. Healthy lifestyle and all-cause mortality
There were 471 deaths over a median follow-up of 6.0 years (maximum: 9.1 years). All-cause mortality rates were lower for individuals participating in physical activity 1-to-4 and ≥5 versus 0 times-per-week, nonsmokers versus current smokers and participants with a higher adherence to the Mediterranean diet (Table 3, top panel). After adjustment for age, race, sex, and region of residence (Model 1), the HRs for mortality were lower for physical activity ≥5 versus no times per week (p<0.05), nonsmokers versus current smokers (p<0.05), and the highest versus lowest quartile of Mediterranean diet adherence (p<0.05). Nonsmoking and the highest versus lowest quartile of Mediterranean diet adherence remained associated with a lower HR for mortality after further multivariable adjustment (Model 2). All-cause mortality rates were lower among individuals with a higher number of healthy lifestyle factors (Table 3, bottom panel). After multivariable adjustment, the HR (95% CI) for all-cause mortality associated with 1, 2, 3, and ≥ 4 healthy lifestyles compared with none was 0.54 (0.37 – 0.80), 0.40 (0.26 – 0.60), 0.38 (0.25 – 0.59), and 0.28 (0.16 – 0.50), respectively (p-trend<0.001). The risk for death associated with individual and a higher number of healthy lifestyle factors did not differ by race or sex (all p-interaction>0.05). Results were markedly similar using a complete case analysis (Supplemental eTable 4).
Table 3.
Incidence Rates and Hazard Ratios of All-Cause Mortality Associated With Healthy Lifestyle Factors Among Participants With a 10-year Predicted Atherosclerotic Cardiovascular Disease Risk ≥7.5% (n=5,709).
| Events / n at risk |
Crude incidence rate per 1,000 person years (95% confidence interval) |
Hazard Ratio (95% confidence interval) |
||
|---|---|---|---|---|
| Model 1a | Model 2b | |||
| Individual healthy lifestyle factors | ||||
| Waist circumference | ||||
| Obese | 193 / 2,459 | 13.29 (11.42, 15.17) | 1 (ref) | 1 (ref) |
| Non-obese | 278 / 3,250 | 14.15 (12.49, 15.82) | 0.94 (0.78, 0.14) | 1.05 (0.86, 1.29) |
| Physical activity | ||||
| None | 167 / 1,720 | 16.65 (14.11, 19.19) | 1 (ref) | 1 (ref) |
| 1 – 4 times per week | 177 / 2,501 | 11.72 (9.98, 13.45) | 0.68 (0.55, 0.85) | 0.73 (0.59, 0.91) |
| ≥ 5 times per week | 127 / 1,488 | 14.09 (11.63, 16.56) | 0.77 (0.61, 0.98) | 0.83 (0.65, 1.06) |
| p-trend | 0.023 | 0.110 | ||
| Smoking status | ||||
| Current | 136 / 1,100 | 22.18 (18.45, 25.91) | 1 (ref) | 1 (ref) |
| Nonsmoker | 335 / 4,609 | 11.95 (10.67, 13.23) | 0.35 (0.29, 0.44) | 0.39 (0.32, 0.49) |
| Saturated fat intake | ||||
| ≥ 7.0% of daily calories | 437 / 5,294 | 13.84 (12.52, 15.15) | 1 (ref) | 1 (ref) |
| < 7.0% of daily calories | 34 / 415 | 13.21 (8.15, 18.27) | 0.89 (0.59, 1.35) | 0.93 (0.60, 1.42) |
| Mediterranean diet scorec | ||||
| Quartile 1 (worse) | 177 / 1,793 | 16.94 (14.31, 19.57) | 1 (ref) | 1 (ref) |
| Quartile 2 | 111 / 1,143 | 16.25 (12.91, 19.59) | 0.94 (0.72, 1.21) | 0.95 (0.73, 1.22) |
| Quartile 3 | 83 / 1,191 | 11.52 (8.81, 14.24) | 0.65 (0.49, 0.88) | 0.70 (0.52, 0.94) |
| Quartile 4 (better) | 100 / 1,582 | 10.34 (8.04, 12.65) | 0.57 (0.43, 0.77) | 0.61 (0.46, 0.82) |
| p-trend | <0.001 | <0.001 | ||
| Number of healthy lifestyle factorsd | ||||
| 0 | 21 / 289 | 20.55 (13.31, 27.79) | 1 (ref) | 1 (ref) |
| 1 | 118 / 1,649 | 15.89 (13.26, 18.51) | 0.51 (0.34, 0.75) | 0.54 (0.37, 0.80) |
| 2 | 134 / 2,104 | 13.07 (10.90, 15.24) | 0.35 (0.23, 0.53) | 0.40 (0.26, 0.60) |
| 3 | 81 / 1,238 | 12.56 (9.91, 15.21) | 0.32 (0.21, 0.48) | 0.38 (0.25, 0.59) |
| ≥ 4 | 23 / 429 | 9.21 (5.26, 13.16) | 0.23 (0.13, 0.40) | 0.28 (0.16, 0.50) |
| p-trend | <0.001 | <0.001 | ||
Model 1: adjustment for age, race, sex, education, income and geographic region of residence.
Model 2: adjustment for Model 1 variables plus high-density lipoprotein and total cholesterol, c-reactive protein >3 mg/L, systolic and diastolic blood pressure, antihypertensive medication use, albumin-to-creatinine ratio ≥30 g/mg and estimated glomerular filtration rate <60 ml/min/1.73 m2.
Quartiles determined using all participants.
Mediterranean diet score cut-points: [quartile 1 (low) to quartile 4 (high)] <3, 3 to <4, 4 to <6, and ≥6.
Number of healthy lifestyle factors: the sum of a non-obese waist circumference (<102 cm for men and <88 cm for women), physical activity ≥ 5 times per week, nonsmoking, saturated fat intake < 7.0% of average daily calories and Mediterranean diet score in quartile 4.
1.4. Discussion
In the current analysis of a nationwide sample of US adults who are candidates for primary prevention of ASCVD with statin therapy, only 21.7% and 7.5% had 3 and 4 or 5 of the healthy lifestyle factors studied, respectively. After full multivariable adjustment, nonsmoking was associated with a lower risk for incident ASCVD. Additionally, nonsmoking and the highest quartile of Mediterranean diet adherence were associated with a lower risk for all-cause mortality after full multivariable adjustment. Furthermore, there was a graded association between an increasing number of healthy lifestyle factors and a lower risk for ASCVD and all-cause mortality. These associations remained present after multivariable adjustment. Results from the current study contribute to knowledge of the benefit of healthy lifestyles for primary prevention among individuals with high ASCVD risk. Additionally, these results highlight the potential need to focus on healthy lifestyles as an approach for reducing ASCVD risk, as an adjunct or alternative to statins, among individuals at high ASCVD risk. These results should be considered beyond the US and are relevant in all settings where lifestyle modification is the first-line approach for primary prevention of ASCVD.
In many countries, healthy lifestyles are underutilized in adults with high ASCVD risk.(5, 22) National Health and Nutrition Survey (NHANES) 2009–2010 data indicate that less than 50% of US adults maintained lifestyle factors including body mass index <25 kg/m2, physical activity levels recommended by the AHA, low saturated fat intake (<7% of daily calories) and the AHA’s recommended diet (similar to the Mediterranean diet).(5) While avoidance of cigarette smoking has increased substantially over the past several decades, approximately 20% of US adults still smoke cigarettes.(5) Furthermore, the World Health Organization’s 2013–2020 Global Action Plan for Prevention and Control of Non-communicable Diseases targets decreases in the prevalence of non-healthy lifestyles including insufficient physical activity and tobacco use and mean sodium intake with the goal to achieve between 10% and 30% relative risk reduction in ASCVD mortality.(22) The current study extends prior research to a high-risk population of candidates for primary prevention of ASCVD with statins, and confirms that many healthy lifestyles are not being practiced. The low prevalence of healthy lifestyles in this high-risk population represents a missed opportunity for a safe and low-cost approach for ASCVD risk reduction. Additionally, the low utilization of healthy lifestyle factors in blacks and women identify these sub-groups to target for lifestyle modification.
Each healthy lifestyle studied herein has been reported to be associated with lipid-lowering benefits or reduced ASCVD and mortality risk.(5, 13–15, 23–29) Smoking cessation should be a priority for high-risk individuals since nonsmoking has been consistently associated with a substantially lower risk for ASCVD and mortality.(23) Observational studies and RCTs provide strong evidence that intentional central weight loss in overweight and obese individuals can improve cholesterol levels and ASCVD risk.(13–15) As reported in a meta-analysis that assessed exercise training trials, regularly participating in physical activity lowers low-density-lipoprotein-cholesterol levels an average of 5%.(24–26) Another meta-analysis of RCTs reported that for each 5% exchange of saturated with polyunsaturated fats there is a 10% reduction in CHD events (relative risk: 0.90, 95% CI: 0.83–0.97).(5, 27) Furthermore, observational studies and RCTs demonstrate that higher adherence to a Mediterranean-style diet consisting of fruits, vegetables, whole grains, ocean fish and low in saturated fats, largely achievable by following the AHA recommended diet, has been associated with a lower ASCVD risk.(28–30) While the lifestyle factors evaluated in the current study have been shown to be effective in lowering ASCVD risk in RCTs, their population-level effectiveness has not been demonstrated.(31, 32) Further, while we report not smoking has a large effect (i.e., HR: 0.58, 95% CI: 0.41 to 0.68) on ASCVD, smoking had a relatively low prevalence in the current study. Therefore, improving other non-healthy lifestyle factors that are more common, such as diet, may have a greater population-level effect. Importantly, although each healthy lifestyle studied was not associated with lower ASCVD and mortality risk in the current study, improvements in non-healthy lifestyles can substantially lower ASCVD morbidity and mortality risks as these effects accumulate over time.(33) Also, increasing the number of healthy lifestyles has a positive impact on overall health, well beyond maximizing the potential benefits of cardiovascular health, particularly if maintained over time.(34)
The importance of practicing a healthy lifestyle is emphasized in the current study by the graded association between a greater number of healthy lifestyle factors and lower ASCVD and mortality risk. Although studies of multifactorial interventions are heterogeneous in their chosen approaches and targeted lifestyle factors, evidence that combining healthy lifestyle factors to lower cholesterol levels and CHD mortality is provided by data from large RCTs.(35–37) For example, in 12,866 Multiple Risk Factor Intervention Trial (MRFIT) participants, there was a greater reduction in low-density-lipoprotein-cholesterol for the multifactorial intervention (stepped-care hypertension treatment, smoking-counseling, dietary advice) versus the usual care group, which in turn was associated with a 7.1% lower risk for CHD death.(35) Additionally, in PREMIER, compared with an advice-only control group, participants who received a lifestyle intervention or lifestyle intervention plus advice on consumption of a Dietary Approaches to Stop Hypertension (DASH) diet, lost more weight, had a greater increase in fitness, and a larger reduction in saturated fat intake.(36, 38) These lifestyle improvements translated into a statistically significant 12–14% reduction in predicted CHD risk for participants randomized to the intervention groups.(39) Participants in the current study who engaged in a healthier lifestyle had a lower risk for ASCVD and mortality outcomes confirming the benefit of a healthy lifestyle.(25)
The 2013 ACC/AHA cholesterol treatment guideline emphasizes lifestyle modification prior to and in conjunction with the use of lipid-lowering medications.(1) In the current study, most candidates for primary prevention with statin therapy utilized a limited number of healthy lifestyle factors. Following a healthier lifestyle may substantially lower the ASCVD and mortality risks. After multivariable adjustment, the risk for ASCVD and mortality were 46% and 72% lower, respectively, among participants with 4 or 5 compared with 0 healthy lifestyle factors in the current study. Among participants with a 10-year predicted ASCVD risk ≥7.5% and 4 or 5 healthy lifestyles, the incidence rate of ASCVD and mortality was 8.66 and 9.21 events per 1,000 person-years, respectively. These rates suggest that many individuals who do not utilize multiple healthy lifestyle factors may be able to achieve low ASCVD and mortality risk through lifestyle modification alone.(40)
1.4.1. Strengths and limitations
The current study has a number of strengths. These include a large nationwide population-based sample of black and white adults, the use of standardized methods to collect information on multiple lifestyle factors and the active follow-up of participants for incident ASCVD and all-cause mortality. Additionally, ASCVD events were adjudicated following methods applied in other large cohort studies. However, certain potential limitations of the current study should be considered. The observational study design limits the causal inferences that can be made between healthy lifestyles with ASCVD and all-cause mortality. Additionally, statin use was self-reported. Furthermore, each lifestyle factor was assessed at only one time and smoking status, physical activity, and dietary information, were self-reported. Although we used a validated dietary questionnaire, misclassification may have been present. Additionally, over 25% of our study sample was missing dietary data and we relied on multiple imputation to account for missing data. However, our results did not differ when conducting a complete case analysis. Finally, we only had data on a US sample and similar analyses should be conducted in other international settings.
1.5. Conclusion
The 2013 ACC/AHA cholesterol treatment guideline recommends lifestyle modification prior to and in conjunction with lipid-lowering medications. The current population-based study highlights the underutilization of healthy lifestyle factors among candidates for primary prevention of ASCVD with statin therapy based on having a 10-year predicted risk ≥ 7.5%. The use of a higher number of healthy lifestyle factors was associated with progressively lower ASCVD and all-cause mortality risk. These results highlight the important role of healthy lifestyle factors among individuals with high ASCVD risk.
Supplementary Material
Acknowledgements
Study conception and design: JNBIII, GH, MS, MC, PM; Acquisition, analysis or interpretation of data: JNBIII, LDC, GH, MS, MB, KR, MC, PM; Statistical analysis: JNBIII, LDC; Drafting of the manuscript: JNBIII; Critical revision of the manuscript: JNBIII, LDC, GH, MS, MB, KR, MC, PM; Critical revision of the manuscript for important intellectual content: LDC, GH, MS, MB, KR, MC, PM. JNBIII and PM had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding Sources: This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke and grants R01 HL080477 and K24 HL111154 from the National Heart, Lung and Blood Institute; National Institutes of Health, Department of Health and Human Service. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke; the National Heart, Lung and Blood Institute; or the National Institutes of Health. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data.2 The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Disclosures: JNBIII: None; LDC: receives research salary support from R01 HL080477; GH: receives research salary support from NIH grant U01 NS041588 and NINDS grants R01 HL080477 and K24 HL111154; MS: receives research salary support from NIH grant U01 NS041588, R01 HL080477, and K24 HL111154 and Amgen, Inc. MB: None; KR: None; MC: receives research salary support from NIH grant U01 NS041588; PM: receives research support from NIH grant R01 HL080477 and Amgen, Inc.
References
- 1.Stone NJ, Robinson J, Lichtenstein AH, Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013. [Google Scholar]
- 2.Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013;382(9907):1762–5. [DOI] [PubMed] [Google Scholar]
- 3.Pencina MJ, Navar-Boggan AM, D’Agostino RB Sr., Williams K, Neely B, Sniderman AD, et al. Application of new cholesterol guidelines to a population-based sample. The New England journal of medicine. 2014;370(15):1422–31. [DOI] [PubMed] [Google Scholar]
- 4.Kavey RE, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K, et al. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation. 2003;107(11):1562–6. [DOI] [PubMed] [Google Scholar]
- 5.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics−−2014 update: a report from the american heart association. Circulation. 2014;129(3):e28–e292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schulte JM, Rothaus CS, Adler JN. Clinical decisions. Starting statins--polling results. The New England journal of medicine. 2014;371(4):e6. [DOI] [PubMed] [Google Scholar]
- 7.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25(3):135–43. [DOI] [PubMed] [Google Scholar]
- 8.Goff DC Jr., Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB Sr., Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014;63(25 Pt B):2935–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. Journal of clinical epidemiology. 1990;43(12):1327–35. [DOI] [PubMed] [Google Scholar]
- 10.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical chemistry. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 11.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, Feldman HI 3rd, et al. A new equation to estimate glomerular filtration rate. Annals of internal medicine. 2009;150(9):604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Czernichow S, Kengne AP, Stamatakis E, Hamer M, Batty GD. Body mass index, waist circumference and waist-hip ratio: which is the better discriminator of cardiovascular disease mortality risk?: evidence from an individual-participant meta-analysis of 82 864 participants from nine cohort studies. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2011;12(9):680–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Despres JP, Arsenault BJ, Cote M, Cartier A, Lemieux I. Abdominal obesity: the cholesterol of the 21st century? The Canadian journal of cardiology. 2008;24 Suppl D:7D–12D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Milsom VA, Malcolm RJ, Johnson GC, Pechon SM, Gray KM, Miller-Kovach K, et al. Changes in cardiovascular risk factors with participation in a 12-week weight loss trial using a commercial format. Eating behaviors. 2014;15(1):68–71. [DOI] [PubMed] [Google Scholar]
- 15.Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129(25 Suppl 2):S102–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. The New England journal of medicine. 2003;348(26):2599–608. [DOI] [PubMed] [Google Scholar]
- 17.Stroke−−1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO Task Force on Stroke and other Cerebrovascular Disorders. Stroke. 1989;20(10):1407–31. [DOI] [PubMed] [Google Scholar]
- 18.Luepker RV, Apple FS, Christenson RH, Crow RS, Fortmann SP, Goff D, et al. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation. 2003;108(20):2543–9. [DOI] [PubMed] [Google Scholar]
- 19.Safford MM, Brown TM, Muntner PM, Durant RW, Glasser S, Halanych JH, et al. Association of race and sex with risk of incident acute coronary heart disease events. JAMA : the journal of the American Medical Association. 2012;308(17):1768–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prineas RJ, Crow RS, Zhang Z-M. The Minnesota code manual of electrocardiographic findings including measurement and comparison with the Novacode; standards and procedures for ECG measurement in epidemiologic and clinical trials. London; New York: Springer,; 2010. Available from: http://rave.ohiolink.edu/ebooks/ebc/9781848827783. [Google Scholar]
- 21.White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Statistics in medicine. 2011;30(4):377–99. [DOI] [PubMed] [Google Scholar]
- 22.Arena R, Guazzi M, Lianov L, Whitsel L, Berra K, Lavie CJ, et al. Healthy lifestyle interventions to combat noncommunicable disease-a novel nonhierarchical connectivity model for key stakeholders: a policy statement from the American Heart Association, European Society of Cardiology, European Association for Cardiovascular Prevention and Rehabilitation, and American College of Preventive Medicine. European heart journal. 2015;36(31):2097–109. [DOI] [PubMed] [Google Scholar]
- 23.Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, et al. 21st-century hazards of smoking and benefits of cessation in the United States. The New England journal of medicine. 2013;368(4):341–50. [DOI] [PubMed] [Google Scholar]
- 24.Thompson PD, Buchner D, Pina IL, Balady GJ, Williams MA, Marcus BH, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity). Circulation. 2003;107(24):3109–16. [DOI] [PubMed] [Google Scholar]
- 25.Ignarro LJ, Balestrieri ML, Napoli C. Nutrition, physical activity, and cardiovascular disease: an update. Cardiovascular research. 2007;73(2):326–40. [DOI] [PubMed] [Google Scholar]
- 26.Leon AS, Sanchez OA. Response of blood lipids to exercise training alone or combined with dietary intervention. Medicine and science in sports and exercise. 2001;33(6 Suppl):S502–15; discussion S28–9. [DOI] [PubMed] [Google Scholar]
- 27.Mozaffarian D, Micha R, Wallace S. Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS medicine. 2010;7(3):e1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Knoops KT, de Groot LC, Kromhout D, Perrin AE, Moreiras-Varela O, Menotti A, et al. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA : the journal of the American Medical Association. 2004;292(12):1433–9. [DOI] [PubMed] [Google Scholar]
- 29.Stathakos D, Pratsinis H, Zachos I, Vlahaki I, Gianakopoulou A, Zianni D, et al. Greek centenarians: assessment of functional health status and life-style characteristics. Experimental gerontology. 2005;40(6):512–8. [DOI] [PubMed] [Google Scholar]
- 30.Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. The New England journal of medicine. 2013;368(14):1279–90. [DOI] [PubMed] [Google Scholar]
- 31.Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, phase II. The Trials of Hypertension Prevention Collaborative Research Group. Archives of internal medicine. 1997;157(6):657–67. [PubMed] [Google Scholar]
- 32.Kumanyika SK, Cook NR, Cutler JA, Belden L, Brewer A, Cohen JD, et al. Sodium reduction for hypertension prevention in overweight adults: further results from the Trials of Hypertension Prevention Phase II. Journal of human hypertension. 2005;19(1):33–45. [DOI] [PubMed] [Google Scholar]
- 33.Artinian NT, Fletcher GF, Mozaffarian D, Kris-Etherton P, Van Horn L, Lichtenstein AH, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(4):406–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.King DE, Mainous AG, Geesey ME 3rd. Turning back the clock: adopting a healthy lifestyle in middle age. The American journal of medicine. 2007;120(7):598–603. [DOI] [PubMed] [Google Scholar]
- 35.Multiple risk factor intervention trial. Risk factor changes and mortality results. Multiple Risk Factor Intervention Trial Research Group. JAMA : the journal of the American Medical Association. 1982;248(12):1465–77. [PubMed] [Google Scholar]
- 36.Lien LF, Brown AJ, Ard JD, Loria C, Erlinger TP, Feldstein AC, et al. Effects of PREMIER lifestyle modifications on participants with and without the metabolic syndrome. Hypertension. 2007;50(4):609–16. [DOI] [PubMed] [Google Scholar]
- 37.Ebrahim S, Taylor F, Ward K, Beswick A, Burke M, Davey Smith G. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane database of systematic reviews. 2011(1):CD001561. [DOI] [PubMed] [Google Scholar]
- 38.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA : the journal of the American Medical Association. 2003;289(16):2083–93. [DOI] [PubMed] [Google Scholar]
- 39.Maruthur NM, Wang NY, Appel LJ. Lifestyle interventions reduce coronary heart disease risk: results from the PREMIER Trial. Circulation. 2009;119(15):2026–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Banach M, Malodobra-Mazur M, Gluba A, Katsiki N, Rysz J, Dobrzyn A. Statin therapy and new-onset diabetes: molecular mechanisms and clinical relevance. Current pharmaceutical design. 2013;19(27):4904–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


