Abstract
Introduction:
Polysubstance abuse (PSA) is a significant problem affecting our society. In addition to negatively affecting the health and well-being of substance users, alcohol and/or drug abuse is also associated with heavy injury burden. The goal of this study was to determine if elevated serum alcohol (EtOH) levels on initial trauma evaluation correlate with the simultaneous presence of other substances of abuse (SOAs). We hypothesized that PSA would be more common among patients who present with EtOH levels in excess of the legal blood alcohol content (BAC) (≥0.10%).
Methods:
An audit of trauma registry records from January 2009 to June 2015 was performed. Abstracted data included patient demographics, BAC measurements, all available formal determinations of urine/serum “drug screening,” Glasgow Coma Scale (GCS) assessments, injury mechanism/severity, and 30-day mortality. Stratification of BAC was based on the 0.10% cutoff. Parametric and nonparametric statistical testing was performed, as appropriate, with significance set at α = 0.05.
Results:
We analyzed 1550 patients (71% males, mean age: 38.7 years) who had both EtOH and SOA screening. Median GCS was 15 (interquartile range [IQR]: 14–15). Median ISS was 9 (IQR: 5–17). Overall 30-day mortality was 4.25%, with no difference between elevated (≥0.10) and normal (<0.10) EtOH groups. For the overall study sample, the median BAC was 0.10% (IQR: 0–0.13). There were 1265 (81.6%) patients with BAC <0.10% and 285 (18.4%) patients with BAC ≥0.10%. The two groups were similar in terms of mechanism of injury (both, ∼95% blunt). Patients with BAC ≥0.10% on initial trauma evaluation were significantly more likely to have the findings consistent with PSA (e.g., EtOH + additional substance) than patients with BAC <0.10% (377/1265 [29.8%] vs. 141/285 [49.5%], respectively, P < 0.001). Among polysubstance users, BAC ≥0.10% was significantly associated with cocaine, marijuana, and opioid use.
Conclusions:
This study confirms that a significant proportion of trauma patients with admission BAC ≥0.10% present with the evidence of additional substance use. Cocaine and opioids were most strongly associated with acute alcohol intoxication. Our findings support the need for further research in this important area of public health concern. In addition, specific efforts should focus on primary identification, remediation of withdrawal symptoms, prevention of drug-drug interactions, and early PSA intervention.
Key Words: Alcohol abuse, drug abuse, injury, outcomes, polysubstance use, trauma
INTRODUCTION
Alcohol abuse is a major public health problem in the United States.[1] Alcohol is associated with motor vehicle collisions, industrial and recreational injuries, criminal activities, and various forms of drug abuse.[2,3,4] Identified as a “gateway drug,” alcohol use is thought to lead to experimentation and use of marijuana, cocaine, and other illicit substances.[5,6,7,8,9,10] This relationship is important to emphasize as the drug epidemic continues to escalate.[11,12] According to 2013 data from the National Institute on Drug Abuse, estimated 24.6 million Americans (9.4% of the population aged 12 years or older) had used an illicit drug “in the past month.”[13]
Both alcohol and drug use has been implicated as contributory to various types of trauma.[14,15] As many as 40%–60% of patients seen in trauma centers are under the influence of alcohol or other substances of abuse (SOAs) when admitted.[16,17] Following the initial standardized trauma evaluation – Airway, Breathing, Circulation, Disability, and Exposure,[18] one must quickly determine whether any alterations in mental status may represent acute intoxication. From definitional standpoint, patients who consume a combination of drugs are termed “polysubstance users.”[19,20] Polysubstance abuse (PSA) can be defined as the concurrent consumption of more than one SOA in a defined period, for nonmedical purposes.[20,21] In addition to the potential for the development of substance addiction, PSAs have elevated risk of associated toxicity and other adverse side effects.[21] Drug abuse, and particularly opiate abuse, resulted in more than 64,000 attributable deaths in the United States in 2016.[22,23] Moreover, vehicle drivers positive for alcohol and illicit drugs have greater odds of motor vehicle crash than drivers positive for either alcohol or illicit drugs in isolation.[24]
PSA is underrecognized secondary to unwillingness by patients to admit to substance abuse due to concerns about legal ramifications of possession, as well as health-care provider reticence regarding asking about potentially embarrassing personal information.[25,26,27,28,29] The assessment of polysubstance-induced delirium further complicates the evaluation and treatment of the injured victim with shock and/or brain injury in the chaotic environment of the trauma resuscitation unit.[30,31] Consequently, better, quicker, and more standardized means of assessment are needed to enable physicians to identify and treat (poly) substance users more promptly and effectively.[32,33]
State laws generally refer to alcohol intoxication using predetermined blood alcohol content (BAC) levels, expressed in grams per deciliter (g/dL).[34] When referring to “drunk driving,” BAC values in excess of 0.08%–0.10% g/dL are considered to be synonymous with “legal intoxication,” depending on local laws.[34,35] This study sought to determine whether the presence of elevated blood alcohol levels on initial trauma evaluation correlated with the concurrent presence of other illicit SOAs. We hypothesized that PSA will be more frequent among patients who present with alcohol levels in excess of the legal BAC.
METHODS
After obtaining an Institutional Review Board exemption, we retrospectively reviewed admission records (total, n = 14,057) from our Level I Trauma Center registry beginning January 1, 2009, and ending June 1, 2015. Abstracted data included patient demographics, BAC measurements, all available formal determinations of urine/serum drug screening (marijuana, cocaine, opioid, and benzodiazepines), injury mechanism and severity (injury severity score [ISS]) information, Glasgow Coma Scale (GCS) assessments, and 30-day mortality. Data abstraction was centralized using Research Electronic Data Capture (Vanderbilt University, Nashville, Tennessee, USA).
For the purposes of this study, stratification of BAC levels to determine “acute intoxication” was based on the 0.10% cutoff, which represents the higher end of legal BAC limits on vehicular driving (e.g., 0.08%–0.10% g/dL) across most localities in the United States.[35] This allows our data to be applicable across a larger number of geographic settings than the more restrictive BAC of 0.08% g/dL. Trauma physician discretion was used to determine whether trauma patients had qualitative and/or quantitative drug screens during the study period.
Statistical analyses were performed using SPSS 18 (PASW Statistics for Windows, SPSS Inc., Chicago, IL, USA). Data were tested for normality using Kolmogorov–Smirnov test, as appropriate. Intergroup comparisons utilized Chi-square and Fisher's exact tests (for categorical data) and Student's t-test (for normally distributed continuous data). Descriptive statistics using percentages, frequencies, and parameter-specific central tendencies (mean ± standard deviation) were utilized where appropriate. Statistical significance was set at α = 0.05. Due to the paucity of preliminary data (and thus lack of information regarding expected intergroup differences) in this area of clinical investigation, no formal power analysis was done.
RESULTS
During the study period, a total of 2099 trauma patients underwent drug screening and 2352 trauma patients had their serum BAC evaluated. Of these two combined subsets, 1550 patients had both drug and serum BAC testing performed [Figure 1]. Patient demographics included mean age of 38.7 ± 19.0 years, 71% male sex, median GCS of 15 (interquartile range [IQR]: 14–15), median ISS of 9 (IQR: 5–17), 94.6% blunt mechanism, and mortality of 4.25%. Specific mechanisms of injury included motor-vehicle crash (47.4%), fall (25.2%), pedestrian struck (2.8%), motorcycle crash (7.6%), gunshot wound (2.1%), stabbing (3.3%), and “other” modalities (11.6%). Average study patient spent 125 min in the emergency department during the trauma evaluation, and the average hospital length of stay (LOS) was 5.7 days. For the overall study sample, the median BAC was 0.10% (IQR: 0–0.13).
Figure 1.
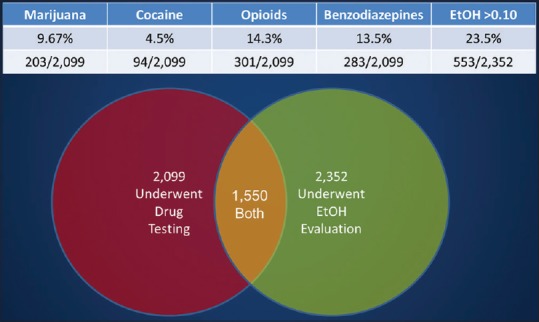
Descriptive characteristic drug (n = 2099) and alcohol (n = 2352) testing within the study sample, including the overlap between the two groups (n = 1550)
Among the 2099 patients who underwent screening for SOA, 14.3% tested positive for opioids, 13.5% for benzodiazepines, 9.67% for marijuana, and 4.5% tested positive for cocaine; the remainder of the group did not have any of the above SOA detected. Of the 2352 patients who had BAC levels drawn, 553 patients (23.5% of the group) had a serum BAC ≥ 0.10%. Detailed description of the above data is provided in Figure 1.
A total of 1550 patients had both SOA and BAC testing performed. This group was the primary study group for subsequent analyses. Of note, we did not detect significant differences between sample characteristics or outcomes between patients with elevated (≥0.10%) and those with nonelevated (<0.10%) BAC (results not shown). The overall study sample median BAC was 0.10% (IQR: 0–0.13). When stratified further, 1265 (81.6%) patients had a BAC <0.10% and 285 (18.4%) patients had a BAC ≥0.10%. These were our primary comparison subgroups in subsequent analyses regarding PSA.
Among patients presenting with BAC <0.10%, 70.2% (888/1265) were determined to have no other substances present, based on SOA screening [Table 1]. When looking at the remaining patients with BAC <0.10%, we noted that 16.8% tested positive for the presence of 1–2 SOAs, with 13.0% patients having >2 SOAs detected [Table 1]. Of the BAC <0.10% cohort with a positive SOA panel, 15.2% were positive for benzodiazepines, 13.3% for opioids, 9.6% for marijuana, and 3.8% for cocaine [Table 1].
Table 1.
Results of primary sample stratification into more granular subgroups, based on BAC <0.10 versus BAC ≥0.10
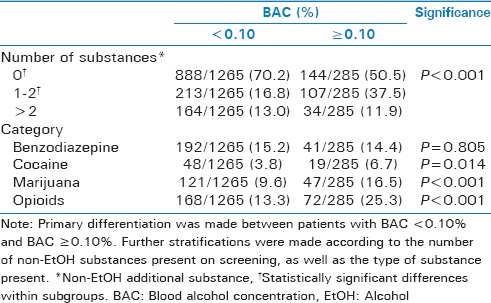
Of the 285 patients presenting with BAC ≥0.10%, approximately 51% were found to have isolated EtOH intoxication [Table 1]. When examining the remainder of the BAC ≥0.10% group, 37.5% patients were found to have 1–2 SOAs co-present, and 11.9% had >2 additional SOAs identified [Table 1; P < 0.001]. Further stratifying the group with BAC ≥0.10% according to the SOA co-present at the time of trauma evaluation, we found that 25.3% tested positive for opioids, 16.5% for marijuana, and 6.7% had evidence of cocaine use [all, P < 0.015 when compared to BAC <0.10%, Table 1]. Finally, while 14.4% tested positive for benzodiazepines in the BAC ≥0.10% group, this was not significantly different from the BAC <0.10% group (15.2% positive for benzodiazepines).
We further found that concurrent presence of 1–2 SOAs more than doubled in patients who presented with a BAC ≥0.10% when compared to the group with a BAC <0.10% (37.5% vs. 16.8%, P < 0.001). Overall, the co-presence of >2 drugs of abuse was similar between the BAC <0.10% and BAC ≥0.10% groups [13.0% vs. 11.9%; Table 1].
We noted important differences between the BAC <0.10% and BAC ≥0.10% groups in terms of distribution patterns of the most common SOA – benzodiazepines and opioids. Although benzodiazepine use was similar between the two groups, the proportion of patients using cocaine, marijuana, and opioids was universally greater in the BAC ≥0.10% group [Table 1].
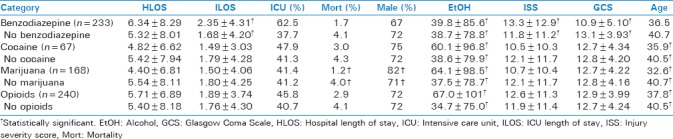
Our final set of comparisons examined patient outcomes in either the presence or absence of specific non-EtOH SOAs [Table 2]. Among key results of this analysis, we noted that benzodiazepine use was associated with longer hospital LOS of 6.34 ± 8.29, marijuana use was associated with the youngest average age (32.6 years), and all nonbenzodiazepine drugs were associated with approximately 1.5–2.0 times EtOH serum levels of the corresponding comparator groups [Table 2]. Finally, the finding of greater mortality for the non-SOA group, although not statistically significant, may be associated with demographic (age and sex) differences between SOA and non-SOA comparison samples.
Table 2.
Results of group comparisons according to the presence or absence of each nonalcohol substance of abuse examined in the current study
DISCUSSION
When comparing patients with initial BAC levels ≥0.10% to those with BAC levels <0.10%, we found important patterns regarding the co-ingestion of SOA and EtOH in our trauma population. Alcohol levels were higher across all group comparisons involving the co-presence of other SOAs [Table 2]. Cocaine, marijuana, and opioid use was significantly more likely among patients presenting with acute EtOH intoxication. However, this was not the case for concurrent benzodiazepine use [Table 1]. We found that opioids were the most commonly encountered illicit drug type in the setting of concurrent EtOH use and trauma, consistent with other published data.[36] This manuscript's findings differ from previously published data by Stoduto et al.,[37] who demonstrated that co-ingestions with illicit drugs were associated with 24% lower mean BAC concentrations. In combination with EtOH abuse, various mind-altering prescription and nonprescription SOAs predispose patients to a significant risk of injury and mortality – a phenomenon that seems to be escalating.[36,38,39,40] Because PSA puts the patient at risk for traumatic injury, standardized public health measures to identify intoxicated patients early in their trauma care should facilitate referral to alcohol and drug rehabilitation resources.[41,42,43,44,45]
In the early 1990s, a Canadian regional trauma unit reported that nearly 17% of patients with acute EtOH intoxication had other SOAs present in their bloodstream.[37] Within that subgroup, 5.3% were found to use cocaine, 12.4% used benzodiazepines, and 13.9% had detectable presence of cannabinoids.[37] These percentages are very similar to those reported in the current study, providing external validation of our results and highlighting that despite decades-long efforts, the “drug epidemic” persists. The magnitude of recent escalation of PSA in the trauma population is demonstrated by Soderstrom et al., who noted that among patients admitted to a regional Level I Trauma Center over a period of 16 years, documented cocaine use increased by 212% while opiate use increased by 543%.[31] In addition to corroborating the high incidence of SOA use in the current study, these statistics also demonstrate the problem's escalating nature. Of note, cocaine- and opiate-positive results were much higher in the setting of violent trauma when compared to nonviolent incidents.[31]
Not surprisingly, the average patient in our study was a male, approximately 30–40 years old, and involved in blunt trauma. We also noted that cocaine, marijuana, and opioid users were significantly younger (difference of 2.7–8.1 years) than patients in comparator groups [Table 2]. In terms of the above patient sample characteristics, our data are relatively similar to those reported previously,[37] with the exception of lower ISS in the current study. The importance of these demographic findings cannot be overstated, with major societal implications of the loss of contribution from young individuals in the midst of their most productive years.[46]
In terms of clinical outcomes, our data show mixed results. For example, we did not demonstrate any significant differences in hospital LOS when comparing patient groups with co-presence of EtOH and various SOA subsets. Except for slightly longer intensive care unit stays for the benzodiazepine and opioid cohorts, we did not note any additional significant differences across the remaining SOA groups [Table 2]. Others reported similar findings, with heterogeneous and somewhat scattered results pertaining to LOS.[37] In the current study, the only significant difference in mortality was noted between patients using marijuana versus those who did not (1.2% vs. 4.0% mortality). In this context, this represents a small degree of similarity to Stoduto et al.,[37] who also showed that patients with co-presence of EtOH and another SOA had lower mortality when compared to those using EtOH only. The clinical relevance of the above relationship is not clear, especially when considering demographic heterogeneity and the co-presence of different SOAs across specific study groups.
There is little doubt that EtOH and SOA screening in the setting of trauma is both worthwhile and “the right thing to do.”[37] However, due to associated costs, such screening programs must be implemented strategically, focusing on the application of evidence-based guidelines for optimal process efficiency. Furthermore, any screening procedures should be carefully integrated into the hospital's trauma diagnostic routine to avoid the potential for “singling out” or labeling individual patients. In addition to effectively identifying trauma patients who engage in PSA, it is critical for institutions to implement effective counseling and treatment programs.[47,48,49] It has been noted that posttrauma admission or observation period provides an excellent opportunity for brief intervention for at-risk and dependent drug and alcohol users, focusing on offering assistance for those interested in seeking help.[48,49] In such paradigm, the initial BAC/SOA testing could be incorporated within the Screening, Brief Intervention and Referral to Treatment model to help identify, reduce, and prevent problematic use, abuse, and dependence on EtOH and illicit drugs.[49]
The current study has important limitations. Due to its retrospective design, certain degree of unavoidable selection and temporal bias is present. In addition, our study group originated from a single institution, was a convenience sample, and its size was relatively small, although comparable to other similar endeavors.[37]
With the context of the above considerations, it is important to note that potential inconsistencies (e.g., provider-specific screening patterns) may have existed in our approach to patients suspected of acute EtOH intoxication or PSA. Moreover, there is no reliable way to determine whether any of the laboratory results for SOA testing may have been due to pharmacologic interventions in the prehospital setting or even in the trauma bay. Thus, some degree of inaccuracy regarding identifying the presence or absence of SOA may be present. For example, urine toxicology screens may not account for all illicit substances, and many popular designer drugs and synthetic drugs (e.g., fentanyl or K2) may not be reliably detected on such testing. Furthermore, lack of uniform timing of SOA testing, combined with varied half-life for different substances, may have resulted in additional diagnostic inaccuracies. This includes the inability to differentiate “immediate” versus “recent” drug use in some cases, making it difficult to accurately interpret opioid or benzodiazepine administration during routine trauma care in the context of SOA. As outlined earlier, SOA screening at our institution is typically done when the trauma provider suspects substance abuse or if the patient appears to be intoxicated. This approach, in turn, introduces selection bias. Finally, one must consider legality of certain drugs (e.g., marijuana in some states) in the context of public health impact and substance abuse epidemiology.[50] For example, simultaneous use of EtOH and marijuana may be much more widespread in Colorado (where marijuana is legal) compared to Pennsylvania (where it is currently not legal).
CONCLUSIONS
The current study determined that patients with BAC ≥0.10% on initial trauma evaluation were significantly more likely to have an additional SOA present on screening tests. Given the deleterious effects of SOA and alcohol, both at the individual and societal levels, it is imperative that dedicated efforts are made to better screen and identify trauma patients who are trapped in the self-destructive pattern of PSA. Once at-risk patients are identified, hospitals can institute and tailor more effective drug intervention strategies toward substance abuse remission programs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Room R, Babor T, Rehm J. Alcohol and public health. Lancet. 2005;365:519–30. doi: 10.1016/S0140-6736(05)17870-2. [DOI] [PubMed] [Google Scholar]
- 2.Smith GS, Kraus JF. Alcohol and residential, recreational, and occupational injuries: A review of the epidemiologic evidence. Annu Rev Public Health. 1988;9:99–121. doi: 10.1146/annurev.pu.09.050188.000531. [DOI] [PubMed] [Google Scholar]
- 3.Taylor B, Irving HM, Kanteres F, Room R, Borges G, Cherpitel C, et al. The more you drink, the harder you fall: A systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug Alcohol Depend. 2010;110:108–16. doi: 10.1016/j.drugalcdep.2010.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Research Council. Injury in America: A Continuing Public Health Problem. Washington, D.C.: National Academies Press; 1985. [PubMed] [Google Scholar]
- 5.Barry AE, King J, Sears C, Harville C, Bondoc I, Joseph K, et al. Prioritizing alcohol prevention: Establishing alcohol as the gateway drug and linking age of first drink with illicit drug use. J Sch Health. 2016;86:31–8. doi: 10.1111/josh.12351. [DOI] [PubMed] [Google Scholar]
- 6.Kirby T, Barry AE. Alcohol as a gateway drug: A study of US 12th graders. J Sch Health. 2012;82:371–9. doi: 10.1111/j.1746-1561.2012.00712.x. [DOI] [PubMed] [Google Scholar]
- 7.Golub A, Johnson BD. The shifting importance of alcohol and marijuana as gateway substances among serious drug abusers. J Stud Alcohol. 1994;55:607–14. doi: 10.15288/jsa.1994.55.607. [DOI] [PubMed] [Google Scholar]
- 8.Welte JW, Barnes GM. Alcohol: The gateway to other drug use among secondary-school students. J Youth Adolesc. 1985;14:487–98. doi: 10.1007/BF02139522. [DOI] [PubMed] [Google Scholar]
- 9.Bamba R, Madden JJ, Hoffman AN, Kim JS, Thayer WP, Nanney LB, et al. Flap reconstruction for pressure ulcers: An outcomes analysis. Plast Reconstr Surg Glob Open. 2017;5:e1187. doi: 10.1097/GOX.0000000000001187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shukla RK. Inside the gate: Insiders' perspectives on Marijuana as a gateway drug. Humboldt J Soc Relat. 2013;35:5, 17. [Google Scholar]
- 11.Scoggins WR. An Overview of Addiction and Addiction Treatment with a Special Focus on the Opioid Epidemic. 2018 [Google Scholar]
- 12.Hatchette K, Hatchette KE. Prevention: The Fight Against the Prescription. Opioid Epidemic. 2018 [Google Scholar]
- 13.National Institute on Drug Abuse – Drug Facts – Nationwide Trends; 2015. Nationwide Trends – Drug Facts. 2017. [Last accessed on 2017 Sep 24]. Available from: https://www.drugabuse.gov/publications/drugfacts/nationwide-trends .
- 14.Abdalla RR, Massaro L, de Queiroz Constantino Miguel A, Laranjeira R, Caetano R, Madruga CS, et al. Association between drug use and urban violence: Data from the II Brazilian National Alcohol and Drugs Survey (BNADS) Addict Behav Rep. 2018;7:8–13. doi: 10.1016/j.abrep.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cordovilla-Guardia S, Vilar-López R, Lardelli-Claret P, Guerrero-López F, Fernández-Mondéjar E. Alcohol or drug use and trauma recidivism. Nurs Res. 2017;66:399–404. doi: 10.1097/NNR.0000000000000231. [DOI] [PubMed] [Google Scholar]
- 16.Dinh-Zarr T, Goss C, Heitman E, Roberts I, DiGuiseppi C. Interventions for preventing injuries in problem drinkers. Cochrane Database Syst Rev. 2004;3:CD001857. doi: 10.1002/14651858.CD001857.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eriksen TR, Shumba L, Ekeberg Ø, Bogstrand ST. The association between hospital admission and substance use among trauma patients. J Subst Use. 2018;23:79–85. [Google Scholar]
- 18.Thim T, Krarup NH, Grove EL, Rohde CV, Løfgren B. Initial assessment and treatment with the airway, breathing, circulation, disability, exposure (ABCDE) approach. Int J Gen Med. 2012;5:117–21. doi: 10.2147/IJGM.S28478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sorsdahl K, Stein DJ, Naledi T, Breuer E, Myers B. Problematic alcohol and other substance use among patients presenting to emergency services in South Africa: Who is ready for change? S Afr Med J. 2017;107:352–3. doi: 10.7196/SAMJ.2017.v107i4.10791. [DOI] [PubMed] [Google Scholar]
- 20.Ogbu UC, Lotfipour S, Chakravarthy B. Polysubstance abuse: Alcohol, opioids and benzodiazepines require coordinated engagement by society, patients, and physicians. West J Emerg Med. 2015;16:76–9. doi: 10.5811/westjem.2014.11.24720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Addiction Centers. Polysubstance Use and Abuse: The Unique Treatment Needs of Polydrug Users. 2018. [Last accessed on 2018 Jun 10]. Available from: https://www.americanaddictioncenters.org/polysubstance-abuse/
- 22.CDC. Drugs Involved in U.S. Overdose Deaths, 2000 to 2016. 2017. [Last accessed on 2017 Sep 24]. Available from: https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates .
- 23.Scott R, Philip C. Statewide Drug Policy Advisory Council 2016 Annual Report. 2016 [Google Scholar]
- 24.Dubois S, Mullen N, Weaver B, Bédard M. The combined effects of alcohol and cannabis on driving: Impact on crash risk. Forensic Sci Int. 2015;248:94–100. doi: 10.1016/j.forsciint.2014.12.018. [DOI] [PubMed] [Google Scholar]
- 25.Woodcock J. A difficult balance – Pain management, drug safety, and the FDA. N Engl J Med. 2009;361:2105–7. doi: 10.1056/NEJMp0908913. [DOI] [PubMed] [Google Scholar]
- 26.Cantrill SV, Brown MD, Carlisle RJ, Delaney KA, Hays DP, Nelson LS, et al. Clinical policy: Critical issues in the prescribing of opioids for adult patients in the emergency department. Ann Emerg Med. 2012;60:499–525. doi: 10.1016/j.annemergmed.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 27.Rozenbroek K, Rothstein WG. Medical and nonmedical users of prescription drugs among college students. J Am Coll Health. 2011;59:358–63. doi: 10.1080/07448481.2010.512044. [DOI] [PubMed] [Google Scholar]
- 28.McCabe SE, West BT, Wechsler H. Trends and college-level characteristics associated with the non-medical use of prescription drugs among US college students from 1993 to 2001. Addiction. 2007;102:455–65. doi: 10.1111/j.1360-0443.2006.01733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McCarthy M. Prescription drug abuse up sharply in the USA. Lancet. 2007;369:1505–6. doi: 10.1016/S0140-6736(07)60690-4. [DOI] [PubMed] [Google Scholar]
- 30.Hoban C. Assessing for head injury in alcohol-intoxicated patients. Emerg Nurse. 2017;25:30–3. doi: 10.7748/en.2017.e1670. [DOI] [PubMed] [Google Scholar]
- 31.Soderstrom CA, Dischinger PC, Kerns TJ, Kufera JA, Mitchell KA, Scalea TM, et al. Epidemic increases in cocaine and opiate use by trauma center patients: Documentation with a large clinical toxicology database. J Trauma. 2001;51:557–64. doi: 10.1097/00005373-200109000-00024. [DOI] [PubMed] [Google Scholar]
- 32.Connors GJ, DiClemente CC, Velasquez MM, Donovan DM. Substance Abuse Treatment and the Stages of Change: Selecting and Planning Interventions. New York: Guilford Press; 2013. [Google Scholar]
- 33.Neale J, Tompkins C, Sheard L. Responding to Drugs Misuse: Research and Policy Priorities in Health and Social Care. London: Routledge; 2009. Barriers to the effective treatment of injecting drug users; pp. 86–98. [Google Scholar]
- 34.Alcohol Policy Information System. Blood Alcohol Concentration (BAC) Limits Adult Operators of Noncommercial Motor Vehicles – Policy Description. 2016. [Last accessed on 2017 Sep 24]. Available from: https://www.alcoholpolicy.niaaa.nih.gov/Blood_Alcohol_Concentration_Limits_Adult_Operators_of_Noncommercial_Motor_Vehicles.html .
- 35.U.S. Legal. Intoxication Law and Legal Definition. 2018. [Last accessed on 2018 Jun 10]. Available from: https://www.definitions.uslegal.com/i/intoxication/
- 36.Manchikanti L, Helm S, 2nd, Fellows B, Janata JW, Pampati V, Grider JS, et al. Opioid epidemic in the United States. Pain Physician. 2012;15:ES9–38. [PubMed] [Google Scholar]
- 37.Stoduto G, Vingilis E, Kapur BM, Sheu WJ, McLellan BA, Liban CB, et al. Alcohol and drug use among motor vehicle collision victims admitted to a regional trauma unit: Demographic, injury, and crash characteristics. Accid Anal Prev. 1993;25:411–20. doi: 10.1016/0001-4575(93)90070-d. [DOI] [PubMed] [Google Scholar]
- 38.Manchikanti L. Prescription drug abuse: What is being done to address this new drug epidemic? Testimony before the subcommittee on criminal justice, drug policy and human resources. Pain Physician. 2006;9:287–321. [PubMed] [Google Scholar]
- 39.Kanouse AB, Compton P. The epidemic of prescription opioid abuse, the subsequent rising prevalence of heroin use, and the federal response. J Pain Palliat Care Pharmacother. 2015;29:102–14. doi: 10.3109/15360288.2015.1037521. [DOI] [PubMed] [Google Scholar]
- 40.Schreiner MD. A deadly combination: The legal response to America's prescription drug epidemic. J Leg Med. 2012;33:529–39. doi: 10.1080/01947648.2012.739060. [DOI] [PubMed] [Google Scholar]
- 41.The National Child Traumatic Stress Network. Making the Connection: Trauma and Substance Abuse. 2008. [Last accessed on 2018 May 31]. Available from: https://www.nctsn.org/sites/default/files/resources//making_the_connection_trauma_substance_abuse.pdf .
- 42.National Institute on Drug Abuse. Drug Screening Tool – NIDA Modified ASSIST (NM ASSIST) [Last accessed on 2018 Dec 06]. Available from: https://www.drugabuse.gov/nmassist/
- 43.CRAFFT Screening Tool. [Last accessed on 2018 Jun 10]. Available from: http://www.ceasar-boston.org/CRAFFT/screenCRAFFT.php .
- 44.The World Health Organization's Alcohol, Smoking and Substance Involvement Screening Test. [Last accessed on 2018 Jun 10]. Available from: https://www.integration.samhsa.gov/clinical-practice/sbirt/ASSIST_Manual, 2.pdf .
- 45.CAGE-AID. [Last accessed on 2018 Dec 06]. Available from: https://www.drugabuse.gov/nidamed-medical-health-professionals/tool-resources-your-practice/screening-assessment-drug-testing-resources/chart-evidence-based-screening-tools-adults .
- 46.Singer M. Drugs and development: The global impact of drug use and trafficking on social and economic development. Int J Drug Policy. 2008;19:467–78. doi: 10.1016/j.drugpo.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 47.Tarter RE. Evaluation and treatment of adolescent substance abuse: A decision tree method. Am J Drug Alcohol Abuse. 1990;16:1–46. doi: 10.3109/00952999009001570. [DOI] [PubMed] [Google Scholar]
- 48.Resources for Optimal Care of the Injured Patient in Prevention. 6th ed. Chicago, Illinois: 2014. American College of Surgeons, Committee on Trauma; p. 141. [Google Scholar]
- 49.Screening, Brief Intervention, and Referral to Treatment. [Last accessed on 2018 Dec 06]. Available from: https://www.integration.samhsa.gov/clinical-practice/SBIRT .
- 50.Pacula RL, Kilmer B, Wagenaar AC, Chaloupka FJ, Caulkins JP. Developing public health regulations for marijuana: Lessons from alcohol and tobacco. Am J Public Health. 2014;104:1021–8. doi: 10.2105/AJPH.2013.301766. [DOI] [PMC free article] [PubMed] [Google Scholar]


