Sir,
Listeriosis is an infection that generally affects pregnant women, neonates, and adults with weakened immune systems. We present a rare case of listeriosis that occurred in an immunocompetent adult.
A 34-year-old male, with no comorbidities, was admitted to wards with a history of fever, vomiting, and headache for 5 days. At presentation, he was disoriented and had a temperature of 101°F, but other vital signs and systemic examination were normal. Aspartate aminotransferase and alanine aminotransferase were 4943 and 4311, respectively. Serology was positive for hepatitis A. A history of having dined at a continental restaurant a fortnight back was elicited, following which his wife had also tested positive for hepatitis A.
Magnetic resonance imaging (MRI) brain and fundoscopy were normal. Cerebrospinal fluid (CSF) analysis was suggestive of partially treated bacterial meningitis [Table 1]. He was started on ceftriaxone, vancomycin, and dexamethasone. Both blood and CSF cultures grew Listeria monocytogenes [Figures 1 and 2]. Following this, antibiotics were changed to intravenous ampicillin 2 g stat and 4th hourly and intravenous gentamicin 300 mg stat and 8th hourly, both to be continued for a total of 2 weeks.
Table 1.
Cerebrospinal fluid findings
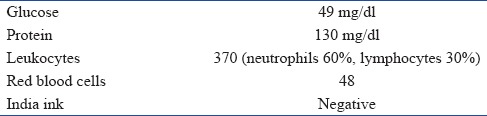
Figure 1.

Culture plate showing christie, atkins, and munch-peterson positive
Figure 2.
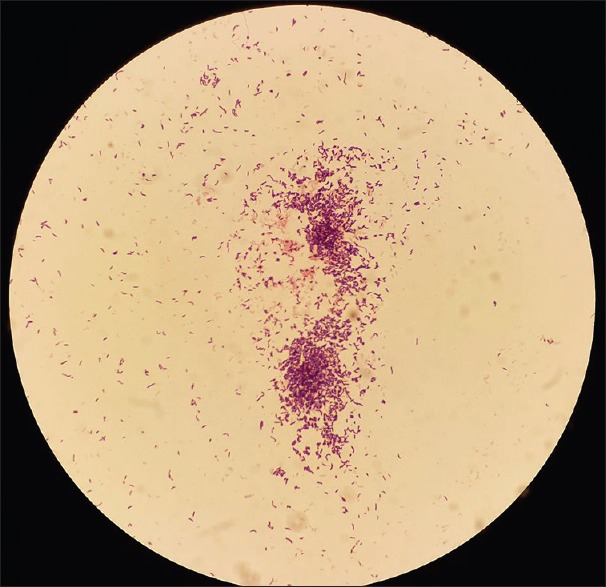
Gram-positive rods on gram staining
The patient was discharged 3 weeks later, after a slow neurological recovery, complicated by bilateral abducens nerve palsy and an episode of generalized tonic-clonic seizure. At discharge, cultures were sterile, but MRI brain remained suggestive of meningoencephalitis. Oral antibiotics were continued for another 3 weeks. On 1-month follow-up, he had recovered well except for mild headache and daytime somnolence.
L. monocytogenes, the Gram-positive bacteria causing listeriosis, spreads through food products such as milk, cheese, processed meat, and vegetables that have been refrigerated for a long period of time. The infection is usually asymptomatic or resembles a mild influenza-like disease. It may also cause meningitis, meningoencephalitis, cerebritis, rhombencephalitis, and intracranial abscess.[1,2] Unlike other causes of bacterial meningitis, listerial meningitis may not show typical meningeal signs such as nuchal rigidity[3] and is often complicated by encephalitis.
Listeriosis during pregnancy may lead to abortion, stillbirth, or delivery of an acutely ill infant. These diverse clinical manifestations reflect the bacteria's capacity to cross intestinal, blood–brain, and placental barriers. Its virulence is attributed to its capacity to multiply at low temperatures or in refrigerated products and form biofilms.[4]
Listeriosis usually affects pregnant women, neonates, the elderly and immunocompromised individuals. This predisposition is a consequence of suppressed T-cell-mediated immunity caused by the condition or its treatment. Concomitant infection with hepatitis A in the present case may have rendered a previously healthy individual susceptible to a more severe form of listeriosis, manifesting as meningitis and septicemia.[5]
L. monocytogenes meningitis should be considered in cases of community-acquired bacterial meningitis that fail to respond to routine antibiotics such as third-generation cephalosporins and vancomycin. The combination of ampicillin and a synergistic aminoglycoside is generally considered as optimal treatment of listerial meningitis. In patients allergic to beta-lactams, sulfamethoxazole-trimethoprim is the best alternative.
Duration of treatment in meningitis is 3 weeks and a minimum of 6 weeks in brain abscess. Antibiotics should be continued until brain imaging studies document resolving lesions.[3]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Zhang Y, Zang GQ, Tang ZH, Yu YS. Listeria monocytogenes meningitis in an immunocompetent adult: A case report. Rev Soc Bras Med Trop. 2012;45:410–1. doi: 10.1590/s0037-86822012000300028. [DOI] [PubMed] [Google Scholar]
- 2.DeJesus-Alvelo I, Merenda A. A case report of Listeria monocytogenes abscesses presenting as cortically predominant ring-enhancing lesions. Case Rep Neurol. 2015;7:105–9. doi: 10.1159/000430434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schuchat A, Deaver KA, Wenger JD, Plikaytis BD, Mascola L, Pinner RW, et al. Role of foods in sporadic listeriosis. I. Case-control study of dietary risk factors. The Listeria study group. JAMA. 1992;267:2041–5. [PubMed] [Google Scholar]
- 4.Brebenariu M, Hogea E, Gheorghiu E, Moldovan R, Bădiţoiu L, Crăciunescu M, et al. Listeria monocytogenes meningitis. Case report of a patient with occupational exposure. Rom Biotechnol Lett. 2016;21 [Google Scholar]
- 5.Koch RM, Kox M, de Jonge MI, Johanes G, van der Hoeven JG, Ferwerda G, et al. Patterns in bacterial and viral induced immunosuppression and secondary infections in the ICU. Shock. 2017;47:5–12. doi: 10.1097/SHK.0000000000000731. [DOI] [PubMed] [Google Scholar]


