Abstract
Objective
To identify risk factors for haemorrhagic transformation in Chinese patients with acute ischaemic stroke treated with recombinant tissue plasminogen activator.
Methods
We searched electronic databases including PubMed, EMBASE, CNKI and WanFang Data for studies reporting risk factors of haemorrhagic transformation after intravenous thrombolysis. Pooled OR, weighted mean difference (WMD) and 95% CI were estimated. Meta-analysis was performed by using Stata V.14.0 software.
Results
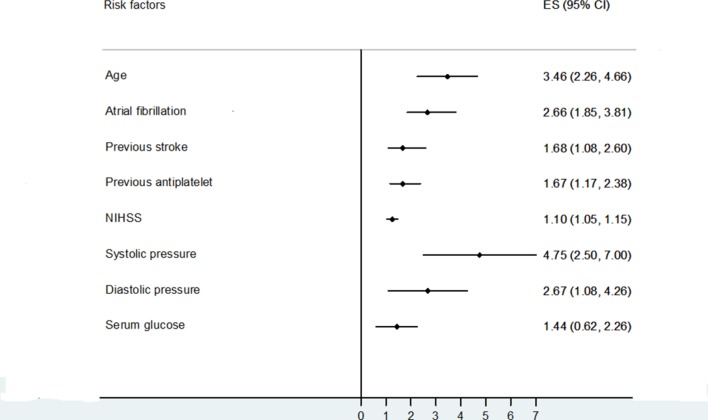
A total of 14 studies were included. The results indicated that older age (WMD=3.46, 95% CI 2.26 to 4.66, I2=47), atrial fibrillation (OR 2.66, 95% CI 1.85 to 3.81, I2=28), previous stroke (OR 1.68, 95% CI 1.08 to 2.60, I2=14), previous antiplatelet treatment (OR 1.67, 95% CI 1.17 to 2.38, I2=0), higher National Institute of Health stroke scale scores (OR 1.10, 95% CI 1. 05 to 1.15, I2=36), systolic (WMD=4.75, 95% CI 2.50 to 7.00, I2=42) or diastolic (WMD=2.67, 95% CI 1.08 to 4.26, I2=35) pressure, and serum glucose level (WMD=1.44, 95% CI 0.62 to 2.26, I2=66) were associated with increased risk of post-thrombolysis haemorrhagic transformation.
Conclusion
The current meta-analysis identified eight risk factors for post-thrombolysis haemorrhagic transformation in Chinese patients with acute ischaemic stroke. Given the risk of bias, these results should be explained with caution and do not justify withholding intravenous thrombolysis.
Keywords: acute ischemic stroke, recombinant tissue plasminogen activator, hemorrhagic transformation, risk factor, meta-analysis
Introduction
Intravenous recombinant tissue plasminogen activator (rt-PA) treatment is an effective therapy for acute ischaemic stroke.1 However, the data from the Chinese National Stroke Registry indicated that there were only 1.6% patients who received rt-PA treatment in China.2 One of the main reasons for withholding rt-PA therapy is fear of haemorrhagic transformation (HT), which may increase the risk of poor and fatal outcome.3 4According to the National Institute of Neurological Disorders and Stroke (NINDS) definition,5 the incidence rate of symptomatic intracranial haemorrhage is 2.2% to 8% across the world and 4.87% to 7.3% in China.6 Compared with patients from Western population, Asian patients may have a higher risk of intracranial haemorrhage,7–9 but the present evidence mostly comes from Japanese patients.7 8 In this study, we systematically reviewed the thrombolysis implementation in Chinese patients with acute ischaemic stroke and perform a meta-analysis to identify risk factors associated with HT.
Methods
Search strategy
The common evidence medicine framework PICO (Patient population, Intervention/Exposure, Control, Outcome) was used to specify our research question: Did Chinese patients with acute ischaemic stroke receiving intravenous thrombolysis (patient population) accompanied with any risk factors (exposure) have a greater risk of HT (outcome) than those patients without (control)? The systematic review and meta-analysis was prepared following the preferred reporting items for systematic reviews and meta-analyses (PRISMA).10 Because no prior review protocol specifically exists to address this question, a search of titles and abstracts of published journal articles in PubMed, EMBASE, CNKI and Wanfang Data database (from 1 February 2010 to 1 November 2017) was conducted without language restriction. Search terms included ‘ischaemic stroke or cerebral infarction or brain infarction’ and ‘thrombolysis or thrombolytic or tissue plasminogen activator or alteplase’ and ‘haemorrhage or haemorrhagic transformation or bleeding’ and ‘risk factor or relevant factor or correlative factor or predictive factor’ and ‘China or Chinese’.
Eligibility criteria
Included studies met the following criteria: (1) retrospective or prospective design, and cohort or case–control studies; (2) thrombolysis treatment within 4.5 hours of stroke onset conformed to Chinese acute ischaemic stroke diagnosis and treatment guideline and the study protocol specifies the dosage of 0.9 mg rt-PA per kilogram; (3) risk factors for haemorrhagic transformation in patients following rt-PA. Exclusion studies were (1) stroke onset to needle time >4.5 hours or unknown, (2) using urokinase thrombolysis, (3) measure outcome including extracranial haemorrhage events, (4) bridging endovascular therapy, (5) reviews and abstracts, and (6) data could not extracted from the studies.
Data extraction
A standardised data collection sheet was used to extract all data. Disagreements were solved by consensus. Two authors independently went through each eligible study and extracted the following information: first author, year of publication, study design, study location, sample size, patients’ baseline characteristics and risk factors. The definition of haemorrhagic transformation is according to the NINDS criteria.5 The risk of bias was assessed by the Newcastle-Ottawa scale (NOS).11
Statistical analysis
Risk factors of interest reported in at least five studies12 were extracted for meta-analysis. Pooled ORs for categorical data, weighted mean differences (WMDs) for continuous data and 95% CI were estimated. Heterogeneity among studies was assessed by I2 test. A fixed-effects model was applied when I2 <50%. When existing statistical heterogeneity measured by I2 >50%, a random-effects model was performed. Funnel plots and Begg’s linear regression test were used to evaluate publication bias. A prespecified sensitivity analysis was performed by omitting one single study in each turn. Meta-regression was used to estimate the impact of sample size on the statistical results. All analyses were conducted using the Stata software package (V.14.0; Stata, College Station, Texas, USA). Statistical significance was set as p value <0.05.
Results
Study selection and characteristic
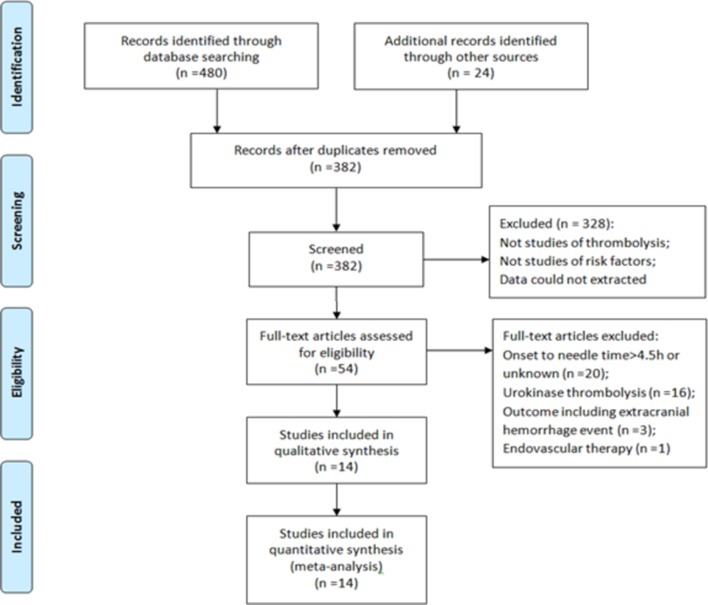
The literature search and screening process are shown in the flow diagrams (figure 1). A total of 504 citations were identified. Of these, 450 citations were eliminated by reviewing title or abstract, and the remaining 54 studies to be reviewed in full-text article. Of the 54 studies, 40 were excluded for not fulfilling the eligibility criteria. Finally, 14 studies6 13–25 including a total of 2548 participants were pooled into meta-analysis. Table 1 depicts the study characteristics and quality assessment.
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses diagram and study identification.
Table 1.
Characteristics of included studies and quality assessment in the meta-analysis
| Author | Publication year |
Study location | Sample size | Included risk factors | NOS scores |
| Liu et al 6 | 2017 | Multicentre | 1128 | (1), (2), (3), (4), (9), (10), (11), (12), (13), (14) | 8 |
| Xu et al 13 | 2017 | Shanghai | 162 | (1), (2), (3), (4), (6), (7), (8) (9), (10), (11), (14) | 7 |
| Shang et al 14 | 2017 | Beijing | 124 | (1), (2), (3), (4), (5), (6), (7), (8), (9), (10), (11), (12), (13), (14) | 6 |
| Wu et al 15 | 2017 | Hebei | 87 | (1), (2), (3), (4), (5), (6), (7), (8), (10), (11) | 6 |
| Li16 | 2017 | Hunan | 69 | (1), (2), (3), (4), (6), (7), (9), (10), (11), (12), (13), (14) | 6 |
| Wang et al 17 | 2016 | Jiangsu | 294 | (1), (2), (3), (4), (5), (6), (8), (9), (10), (11), (12), (13), (14) | 6 |
| Li18 | 2016 | Hebei | 176 | (1), (2), (3), (4), (6), (7), (8), (10), (11), (12), (14) | 8 |
| Chen et al 19 | 2016 | Zhejiang | 122 | (1), (2), (3), (4), (5), (6), (7), (8), (9), (10), (11), (12), (13), (14) | 8 |
| Li et al 20 | 2015 | Hubei | 60 | (1), (2), (3), (4), (5), (6), (7), (11), (12), (13), (14) | 6 |
| Xu et al 21 | 2015 | Jiangsu | 55 | (1), (2), (3), (4), (6), (7), (8), (10), (11), (12), (13), (14) | 7 |
| Zhao et al 22 | 2015 | Guangdong | 36 | (1), (2), (3), (4), (5), (6), (7), (8), (9), (11), (12), (13), (14) | 7 |
| Shen et al 23 | 2013 | Shanghai | 103 | (1), (2), (3), (4), (6), (8), (11), (12), (13) | 6 |
| You24 | 2013 | Chongqing | 65 | (1), (2), (3), (4), (6), (7), (9), (10), (11), (12), (13), (14) | 8 |
| Su et al 25 | 2013 | Zhejiang | 44 | (1), (2), (3), (4), (7), (9), (10), (11), (12), (13), (14) | 6 |
Included risk factors: (1) age, (2) gender, (3) hypertension, (4) diabetes, (5) hyperlipaemia, (6) atrial fibrillation, (7) previous stroke, (8) smoking, (9) previous antiplatelet treatment, (10) onset to needle time, (11) National Institute of Health stroke scale, (12) systolic pressure, (13) diastolic pressure, (14) serum glucose.
NOS, Newcastle-Ottawa scale.
Meta-analysis for risk factors
Demographic factors
Age and gender have been reported as potential risk factors for HT in included studies. A total of 14 studies evaluated age and gender as possible risk factors. The results of meta-analysis found older age (WMD=3.46, 95% CI 2.26 to 4.66, I2=47) was associated with an increased risk of HT, and gender (OR 0.95, 95% CI 0.76 to 1.18, I2=0) was not associated with HT.
Vascular risk factors
Six potential risk factors including hypertension, diabetes, hyperlipaemia, atrial fibrillation, previous stroke and smoking were evaluated in included studies. The meta-analysis demonstrated that atrial fibrillation (OR 2.66, 95% CI 1.85 to 3.81, I2=28) and previous stroke (OR 1.68, 95% CI 1.08 to 2.60, I2=14) were significantly associated with HT.
Previous antiplatelet treatment
A total of nine studies investigated the association between previous antiplatelet drugs and the risk of HT. Meta-analysis indicated that previous antiplatelet treatment (OR 1.67, 95% CI 1.17 to 2.38, I2=0) was associated with an increased risk of HT.
Stroke severity
A total of eight studies reported adjusted OR of initial National Institute of Health stroke scale (NIHSS). The result of meta-analysis suggesting higher NIHSS scores (OR 1.10, 95% CI 1. 05 to 1.15, I2=36) was associated with an increased risk of HT.
Blood pressure and serum glucose level on admission
Systolic pressure, diastolic pressure and serum glucose level were investigated in several included studies. Meta-analysis showed higher systolic pressure (WMD=4.75, 95% CI 2.50 to 7.00, I2=42), diastolic pressure (WMD=2.67, 95% CI 1.08 to 4.26, I2=35) and serum glucose level (WMD=1.11, 95% CI 0.07 to 2.16, I2=83) were significantly associated with HT.
Sensitivity analysis and meta-regression
We conducted a sensitivity analysis by excluding every single study to explore the stability of the combined results. The range of the combined ORs or WMDs for potential risk factors is shown in table 2. To explore the origin of heterogeneity between studies that investigated serum glucose, we pooled the effect size using random-effects model after excluding Li’s study,18 with a reduction of heterogeneity (I2=66%). The association between identified risk factors and HT is shown in figure 2. Meta-regression (table 3) was performed to detect the impact of sample size on combined ORs or WMDs, and the findings demonstrated no statistical significance (all p>0.05).
Table 2.
Heterogeneity and sensitivity analysis analysis of risk factors among included studies
| Risk factors | Number of studies |
HT | Non-HT | Statistic method | I2 | Pooled effect size | Sensitivity analysis | |
| 95% CI | Lower limit | Upper limit | ||||||
| Demographic factors | ||||||||
| Age | 14 | 248 | 2300 | I-V, fixed, WMD | 47 | 3.46 (2.26 to 4.66) | 2.86 (1.60 to 4.12) | 3.98 (2.68 to 5.28) |
| Male | 14 | 248 | 2300 | M-H, fixed, COR | 0 | 0.95 (0.76 to 1.18) | 0.78 (0.29 to 2.13) | 1.43 (0.45 to 5.88) |
| Vascular risk factors | ||||||||
| Hypertension | 14 | 248 | 2300 | M-H, fixed, COR | 0 | 1.05 (0.85 to 1.30) | 0.71 (0.22 to 2.30) | 1.57 (0.69 to 3.57) |
| Diabetes | 14 | 248 | 2300 | M-H, fixed, COR | 13 | 1.18 (0.87 to 1.61) | 0.59 (0.07 to 5.20) | 2.79 (1.08 to 7.22) |
| Hyperlipaemia | 6 | 96 | 650 | M-H, fixed, COR | 0 | 1.10 (0.63 to 1.90) | 1.03 (0.43 to 2.48) | 1.36 (0.29 to 6.42) |
| Atrial fibrillation | 12 | 176 | 1200 | M-H, fixed, MOR | 28 | 2.66 (1.85 to 3.81) | 2.39 (1.65 to 3.46) | 3.02 (2.05 to 4.45) |
| Previous stroke | 11 | 142 | 790 | M-H, fixed, COR | 14 | 1.68 (1.08 to 2.60) | 1.49 (0.92 to 2.41) | 1.97 (1.21 to 3.23) |
| Smoking | 9 | 142 | 1040 | M-H, fixed, COR | 0 | 1.09 (0.80 to 1.50) | 0.46 (0.05 to 4.21) | 1.43 (0.59 to 3.48) |
| Other risk factors | ||||||||
| Previous antiplatelet | 9 | 188 | 1879 | M-H, fixed, MOR | 0 | 1.67 (1.17 to 2.38) | 1.52 (1.04 to 2.22) | 1.91 (1.24 to 2.97) |
| NIHSS | 8 | 139 | 1040 | I-V, random, AOR | 36 | 1.10 (1.05 to 1.15) | 1.09 (1.04 to 1.14) | 1.12 (1.06 to 1.18) |
| Systolic pressure | 12 | 220 | 2079 | I-V, fixed, WMD | 42 | 4.75 (2.50 to 7.00) | 3.28 (0.77 to 5.78) | 6.10 (3.55 to 8.66) |
| Diastolic pressure | 11 | 207 | 1916 | I-V, fixed, WMD | 35 | 2.67 (1.08 to 4.26) | 2.17 (0.51 to 3.82) | 3.34 (1.43 to 5.26) |
| Serum glucose | 10 | 204 | 2058 | I-V, random, WMD | 83 | 1.11 (0.07 to 2.16) | 0.77(−0.19 to 1.73) | 1.43 (0.62 to 2.26) |
| Serum glucose* | 9 | 192 | 2001 | I-V, random, WMD | 66 | 1.44 (0.62 to 2.26) | 1.01 (0.38 to 1.61) | 1.66 (0.81 to 2.51) |
*Effect size was calculated by excluding one single study.
AOR, adjusted OR; COR, crude OR; HT, haemorrhagic transformation; I-V, inverse variance; M-H, Mantel-Haenszel; MOR, mixed OR; NIHSS, National Institute of Health stroke scale; WMD, weighted mean difference.
Figure 2.
Risk factors for haemorrhagic transformation in patients with acute ischaemic stroke receiving recombinant tissue plasminogen activator. ES, effect size; NIHSS, National Institute of Health stroke scale.
Table 3.
Meta-regression for the impact of sample size on pooled results
| Risk factors | Exp(b) | SE | t | p>t | 95% CI | Adjusted R2 (%) |
| Age | 1.07 | 0.21 | 0.36 | 0.723 | 0.71 to 1.61 | −28.75 |
| Atrial fibrillation | 1.22 | 0.59 | 0.41 | 0.691 | 0.42 to 3.56 | −53.25 |
| Previous stroke | 1.40 | 0.76 | 0.63 | 0.547 | 0.41 to 4.76 | −50.87 |
| Previous antiplatelet | 1.86 | 0.88 | 1.30 | 0.234 | 0.60 to 5.71 | 0 |
| NIHSS | 1.12 | 0.11 | 1.20 | 0.277 | 0.89 to 1.39 | 0 |
| Systolic pressure | 0.93 | 0.24 | −0.29 | 0.780 | 0.52 to 1.64 | −15.01 |
| Diastolic pressure | 0.99 | 0.25 | −0.05 | 0.959 | 0.56 to 1.75 | −25.21 |
| Serum glucose | 5.64 | 6.12 | 1.59 | 0.155 | 0.43 to 73.43 | 17.55 |
NIHSS, National Institute of Health stroke scale.
Publication bias
The funnel plot was performed to assess the publication bias for the gender that had been investigated in 14 studies. The visual inspection of the funnel plot and Begg’s test (p=0.155) indicated no evidence of publication bias.
Discussion
The systematic review and meta-analysis demonstrated that eight risk factors were significantly associated with HT in Chinese patients with acute ischaemic stroke treated with rt-PA. We used NOS for quality assessment of case–control or cohort studies in the current meta-analysis. As we could see in table 1, the scores of all included studies were no less than 6 in the quality assessment, which would help judging the reliability of the results.
HT following intravenous thrombolysis in patients with stroke is one of the complications that clinicians were reluctant to witness. For identifying patients with high risk of HT, several prognostic scores have been proposed to apply in clinical setting,26 including Multicenter Stroke Survey (MSS) score,27 Hemorrhage After Thrombolysis (HAT) score,28 baseline blood Sugar, Early infarct signs, (hyper) Dense cerebral artery sign, Age, NIH Stroke Scale (SEDAN) score,29 Glu, Race, Age, Sex, systolic blood Pressure, stroke Severity (GRASPS) score,9 Safe Implementation of Treatments in Stroke score30 and Stroke Prognostication using Age and NIH Stroke Scale (SPAN)-100.31 In these models developed based on Western population, age,9 27 29–31 NIHSS score,9 27–31 blood glucose or diabetes,9 27–30 demographic characteristics9 30 (race, gender, weight), hypertension or systolic blood pressure,9 30 platelet account,27 previous antiplatelet medication,30 32 onset to treatment time30 and early CT signs28 29 are identified items with favourable prediction for HT. In the present study based on Chinese population, the results of meta-analysis and included studies demonstrated risk factors for HT after rt-PA containing age,6 13 14 19 NIHSS score,6 13 15–17 21 22 systolic17 18 or diastolic pressure,16 19 serum glucose level14 21 24 25 and previous antiplatelet treatment. In addition, the present study also detected the risk factor of atrial fibrillation14 15 18 20 21 23 or previous stroke history was associated with increased risk of HT. The I2 test indicated that most pooled effect sizes were with favourable heterogeneity except serum glucose level. After excluding Li’s study,18 a moderate heterogeneity (I2=66%) was still found when estimating the association between HT and glucose level on admission. We speculated that the heterogeneity originated from the variability within studies. A systemic review33 reported that the prevalence of hyperglycaemia ranged from 8% to 63% in patients with acute stroke, and the measurement method used in individual patients contains random or fasting serum glucose, which was not specified in the original literature. The individual difference between patients and measurement bias within studies may explain the original of heterogeneity.
Prior study9 identified higher risk of intracranial haemorrhage in Asian patients with acute ischaemic stroke treated with intravenous tissue-type PA. Although the mechanism is not fully understood, racial difference in intracranial atherosclerotic diseases or blood coagulation–fibrinolysis factors8 34 may account for the observational result. However, due to the limited data extracted by included studies in this secondary analysis, we failed to explore the association between other risk factors and the risk for HT. Recently, a meta-analysis35 performed by Charidimou et al provided evidence between leukoaraiosis and increased risk of HT after intravenous thrombolysis, which may direct early CT or MRI signs and risk for HT for future researches.
Several limitations should be considered in our study. First, the present meta-analysis included 14 cohort or case–control studies. Despite all study protocols that stated the implementation of 0.9 mg rt-PA per kilogram recommended by Chinese guideline, selection bias within studies still exists due to the nature of observational design. Second, there were three different definitions of HT6 that have been proposed on the basis of established clinical trials in intravenous thrombolysis. To make a consistency in outcome measure of included studies, we used conservative NINDS criteria in the study. However, compared with other more strict criteria, the NINDS definition may overestimate the odds of HT and increase the risk of measurement bias. Third, we have to note that most studies included in the meta-analysis fail to distinguish the symptomatic intracranial haemorrhage and non-symptomatic intracranial haemorrhage in patients with HT, and a subgroup analysis for future study is needed to confirm these findings. Because of limitations mentioned above, the results of the current study should be explained with caution.
Conclusions
The systematic review and meta-analysis identified eight risk factors associated with a higher risk of HT, including age, atrial fibrillation, previous stroke, previous antiplatelet treatment, stroke severity, systolic or diastolic pressure, and serum glucose level. Given the risk of bias, these results should not justify withholding intravenous thrombolysis.
Acknowledgments
We thank the authors and participants of the included studies for their important contributions.
Footnotes
MZ and LH contributed equally.
Contributors: YG designed the study, collected and extracted data, and drafted the manuscript. YY collected and extracted data. MZ revised manuscript critically for important intellectual content. LH approved of the version to be published.
Funding: This work was supported by the National Natural Science Foundation of China (grant no. 81571153).
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. Wardlaw JM, Murray V, Berge E, et al. . Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev 2014:Cd000213 10.1002/14651858.CD000213.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Liu L, Wang D, Wong KS, et al. . Stroke and stroke care in China: huge burden, significant workload, and a national priority. Stroke 2011;42:3651–4. 10.1161/STROKEAHA.111.635755 [DOI] [PubMed] [Google Scholar]
- 3. Brown DL, Barsan WG, Lisabeth LD, et al. . Survey of emergency physicians about recombinant tissue plasminogen activator for acute ischemic stroke. Ann Emerg Med 2005;46:56–60. 10.1016/j.annemergmed.2004.12.025 [DOI] [PubMed] [Google Scholar]
- 4. Strbian D, Sairanen T, Meretoja A, et al. . Patient outcomes from symptomatic intracerebral hemorrhage after stroke thrombolysis. Neurology 2011;77:341–8. 10.1212/WNL.0b013e3182267b8c [DOI] [PubMed] [Google Scholar]
- 5. Kwiatkowski TG, Libman RB, Frankel M, et al. . Effects of tissue plasminogen activator for acute ischemic stroke at one year. N Engl J Med Overseas Ed 1999;340:1781–7. 10.1056/NEJM199906103402302 [DOI] [PubMed] [Google Scholar]
- 6. Liu M, Pan Y, Zhou L, et al. . Predictors of post-thrombolysis symptomatic intracranial hemorrhage in Chinese patients with acute ischemic stroke. PLoS One 2017;12:e0184646 10.1371/journal.pone.0184646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. van Asch CJ, Luitse MJ, Rinkel GJ, et al. . Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol 2010;9:167–76. 10.1016/S1474-4422(09)70340-0 [DOI] [PubMed] [Google Scholar]
- 8. Ueshima S, Matsuo O. The differences in thrombolytic effects of administrated recombinant t-PA between Japanese and Caucasians. Thromb Haemost 2002;87:544–6. 10.1055/s-0037-1613042 [DOI] [PubMed] [Google Scholar]
- 9. Menon BK, Saver JL, Prabhakaran S, et al. . Risk score for intracranial hemorrhage in patients with acute ischemic stroke treated with intravenous tissue-type plasminogen activator. Stroke 2012;43:2293–9. 10.1161/STROKEAHA.112.660415 [DOI] [PubMed] [Google Scholar]
- 10. Moher D, Liberati A, Tetzlaff J, et al. . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 12. Zhang J, Zhao T, Long S, et al. . Risk factors for postoperative infection in Chinese lung cancer patients: a meta-analysis. J Evid Based Med 2017;10:255–62. 10.1111/jebm.12276 [DOI] [PubMed] [Google Scholar]
- 13. Xu X, Li C, Wan T, et al. . Risk factors for hemorrhagic transformation after intravenous thrombolysis in acute cerebral infarction: a retrospective single-center study. World Neurosurg 2017;101:155–60. 10.1016/j.wneu.2017.01.091 [DOI] [PubMed] [Google Scholar]
- 14. Shang JY, Xf L, Zhao H, et al. . Analysis of related factors of hemorrhagic transformation after intravenous thrombolytic therapy with alteplase in patients with acute cerebral infarction. Journal of Guangxi Medical University 2017;34:1009–12. [Google Scholar]
- 15. Wu LJ, Li ZW, Kong YM, et al. . Clinical analysis of 89 cases of acute ischemic stroke who accepted rt-PA intravenous thrombolysis. Journal of Hebei Medical University 2017;38:386–94. [Google Scholar]
- 16. Li YP. Revelant factors analysis of intravenous thrombolysis in intracerebral hemorrhage transformation after acute cerebral infarction. Chin J of Clinical Rational Drug Use 2017;10:24–6. [Google Scholar]
- 17. Wang C, Chen GF, Liu WW, et al. . Analysis of related risk factors of hemorrhagic transformation in patients with cerebral infarction and thrombolysis. Chin J Clinicians 2016;10:3198–202. [Google Scholar]
- 18. Li H. Analysis of rt-PA intravenous thrombolysis for acute ischemic stroke clinical prognostic factors. Hebei: Master thesis, North China University of Science and Technology, 2016. [Google Scholar]
- 19. Chen S, Lu X, Zhang W, et al. . Does prior antiplatelet treatment increase the risk of hemorrhagic transformation and unfavorable outcome on day 90 after intravenous thrombolysis in acute ischemic stroke patients? J Stroke Cerebrovasc Dis 2016;25:1366–70. 10.1016/j.jstrokecerebrovasdis.2016.01.038 [DOI] [PubMed] [Google Scholar]
- 20. Li M, Hh L, Luo WJ, et al. . Risk factors and prognosis of the hemorrhagic transformation following thrombolysis in cerebral ischemia. Neural Injury And Functional Reconstruction 2015;10:484–7. [Google Scholar]
- 21. Xu YP, Sun YM, Liu CF. An analysis of factors related to hemorrhage transformation after intravenous alteplase thrombolysis in patients with acute cerebral infarction. Jiangsu Medical Journal 2015;41:2297–300. [Google Scholar]
- 22. Zhao YQ, Qiao LJ, Cai YF, et al. . Risk factors for hemorrhagic transformation in patients with acute ischemic stroke treated with intravenous thrombolysis: a nested case–control study. Guangdong Medical Journal 2015;36:398–401. [Google Scholar]
- 23. Shen J, Bai QK, Zhao ZG, et al. . Risk of intracerebral hemorrhage following multi-modality MRI-based intravenous thrombolytic therapy with rt-PA for acute cerebral infarction. Journal of Apoplexy and Nervous Diseases 2013;30:619–21. [Google Scholar]
- 24. You DX. Clinical analysis of outcome after rt-PA thrombolysis of acute ischemic stroke in 65 patients. Chongqing: Master thesis, Chong Qing Medical University, 2013. [Google Scholar]
- 25. Su LJ, Xu J, Xu HY. Clinical analysis of hemorrhagic transformation in ischemic stroke patients treated with intravenous thrombolysis. Prevention and Treatment of Cardio-Cerebral-Vascular Disease 2013;13:390–1. [Google Scholar]
- 26. Strbian D, Michel P, Seiffge DJ, et al. . Symptomatic intracranial hemorrhage after stroke thrombolysis: comparison of prediction scores. Stroke 2014;45:752–8. 10.1161/STROKEAHA.113.003806 [DOI] [PubMed] [Google Scholar]
- 27. Cucchiara B, Tanne D, Levine SR, et al. . A risk score to predict intracranial hemorrhage after recombinant tissue plasminogen activator for acute ischemic stroke. J Stroke Cerebrovasc Dis 2008;17:331–3. 10.1016/j.jstrokecerebrovasdis.2008.03.012 [DOI] [PubMed] [Google Scholar]
- 28. Lou M, Safdar A, Mehdiratta M, et al. . The HAT score: a simple grading scale for predicting hemorrhage after thrombolysis. Neurology 2008;71:1417–23. 10.1212/01.wnl.0000330297.58334.dd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Strbian D, Engelter S, Michel P, et al. . Symptomatic intracranial hemorrhage after stroke thrombolysis: the SEDAN score. Ann Neurol 2012;71:634–41. 10.1002/ana.23546 [DOI] [PubMed] [Google Scholar]
- 30. Mazya M, Egido JA, Ford GA, et al. . Predicting the risk of symptomatic intracerebral hemorrhage in ischemic stroke treated with intravenous alteplase: Safe Implementation of Treatments in Stroke (SITS) symptomatic intracerebral hemorrhage risk score. Stroke 2012;43:1524–31. 10.1161/STROKEAHA.111.644815 [DOI] [PubMed] [Google Scholar]
- 31. Saposnik G, Guzik AK, Reeves M, et al. . Stroke prognostication using age and NIH stroke scale: SPAN-100. Neurology 2013;80:21–8. 10.1212/WNL.0b013e31827b1ace [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Luo S, Zhuang M, Zeng W, et al. . Intravenous thrombolysis for acute ischemic stroke in patients receiving antiplatelet therapy: a systematic review and meta‐analysis of 19 studies. J Am Heart Assoc 2016;5:e003242 10.1161/JAHA.116.003242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Capes SE, Hunt D, Malmberg K, et al. . Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke 2001;32:2426–32. 10.1161/hs1001.096194 [DOI] [PubMed] [Google Scholar]
- 34. Wong LK. Global burden of intracranial atherosclerosis. Int J Stroke 2006;1:158–9. 10.1111/j.1747-4949.2006.00045.x [DOI] [PubMed] [Google Scholar]
- 35. Charidimou A, Pasi M, Fiorelli M, et al. . Leukoaraiosis, cerebral hemorrhage, and outcome after intravenous thrombolysis for acute ischemic stroke: a meta-analysis (v1). Stroke 2016;47:2364–72. 10.1161/STROKEAHA.116.014096 [DOI] [PMC free article] [PubMed] [Google Scholar]