Among cigarette initiators, e-cigarette users and nonusers had similar patterns of transition to more frequent cigarette use; however, cigarette or dual product users rarely transitioned to exclusive e-cigarette use or nonuse.
Abstract
Video Abstract
BACKGROUND AND OBJECTIVES:
Electronic cigarette (e-cigarette) use is associated with cigarette initiation among adolescents. However, it is unclear whether e-cigarette use is associated with more frequent cigarette use after initiation. Also, the extent to which cigarette or dual cigarette and e-cigarette users transition to exclusive e-cigarette use or to the nonuse of either product is not yet known.
METHODS:
Data were pooled from 3 prospective cohort studies in California and Connecticut (baseline: 2013–2014; follow-up: 2014–2016; N = 6258). Polytomous regression models were used to evaluate the association of baseline e-cigarette use (never or ever) with cigarette use frequency at follow-up (experimental: initiation but no past-30-day use; infrequent: 1–2 of the past 30 days; frequent: 3–5 or more of the past 30 days). Polytomous regression models were also used to evaluate transitions between baseline ever or past-30-day single or dual product use and past-30-day single or dual product use at follow-up.
RESULTS:
Among baseline never smokers, e-cigarette users had greater odds of subsequent experimental (odds ratio [OR] = 4.58; 95% confidence interval [CI]: 3.56–5.88), infrequent (OR = 4.27; 95% CI: 2.75–6.62) or frequent (OR = 3.51; 95% CI: 1.97–6.24) cigarette use; the 3 OR estimates were not significantly different. Baseline past-30-day exclusive cigarette use was associated with higher odds at follow-up of exclusive cigarette or dual product use than of exclusive e-cigarette use.
CONCLUSIONS:
Tobacco control policy to reduce adolescent use of both e-cigarettes and cigarettes is needed to prevent progression to more frequent tobacco use patterns and reduce combustible cigarette use (with or without concurrent e-cigarette use) to lessen the adverse public health impact of e-cigarettes.
What’s Known on This Subject:
Electronic cigarette (e-cigarette) use is associated with cigarette initiation. However, it is unclear whether e-cigarette use is associated with more frequent cigarette use after initiation or whether adolescent cigarette or dual product users transition to exclusive e-cigarette use or nonuse.
What This Study Adds:
Adolescent e-cigarette users appear to follow similar trajectories of cigarette smoking frequency as nonusers. Exclusive cigarette or dual product users are more likely to continue using cigarettes than to transition away from smoking to exclusive e-cigarette use or to nonuse.
Recent studies of population trends in tobacco and alternative tobacco use prevalence among youth in the United States have revealed an indication that electronic cigarettes (e-cigarettes) are used by at least some youth who are unlikely to have started using tobacco products if e-cigarettes were unavailable.1,2 Moreover, we3–6 and others7–20 have demonstrated that youth and young adults who have used e-cigarettes are more likely than those who have not used e-cigarettes to subsequently initiate combustible cigarette use, with a meta-analytic estimate of more than a threefold increase in the risk of subsequent cigarette initiation.21
Based in part on this evidence, in a 2016 report “E-cigarette Use among Youth and Young Adults,” the Surgeon General concluded that e-cigarette use in this population is a public health concern.22 However, others have suggested that this conclusion may be premature if e-cigarette users are disproportionately more likely to be merely experimenting temporarily with cigarettes and are unlikely to progress to more frequent smoking.23 Because e-cigarettes have gained popularity only recently and the progression from cigarette initiation to regular use typically transpires over several years,24–28 it could be argued that researchers in studies to date showing a risk of subsequent cigarette experimentation among e-cigarette users may not have followed e-cigarette users long enough or in sample sizes large enough to assess the risk of progression to regular smoking.
Another key question regarding the public health impact of the high e-cigarette use prevalence among youth and young adults is whether e-cigarettes facilitate smoking cessation. Although there has been considerable study of the potential for e-cigarettes to be a cigarette smoking cessation aid in adults,29–31 there has been little study of transitions from cigarette or multiple tobacco product use to the exclusive use of e-cigarettes (or transition to the nonuse of cigarettes or e-cigarettes) among youth. We reported in an earlier publication that ever cigarette use was associated with a subsequent onset of e-cigarette use in adolescents.3 A separate study revealed that past-30-day cigarette use was not associated with subsequent past-30-day e-cigarette use across 3 annual waves of data in adolescents.16 Researchers in each of these studies have evaluated the use of cigarettes and e-cigarettes as separate variables, which cannot be used to distinguish whether the association of combustible cigarette use with subsequent e-cigarette use reflects youth who quit smoking and have completely transitioned to exclusive e-cigarette use or youth who are now dual product users of both cigarettes and e-cigarettes. Most youth do not use e-cigarettes to quit smoking; data from the National Youth Tobacco Survey (2016) revealed that only 7.8% (95% confidence interval [CI]: 6.5%–9.5%) of youth cited cessation as a reason for e-cigarette use.32 In 1 of our cohort studies (unpublished data), we also observed that few young adults (12.8%) cited cessation as a reason for using e-cigarettes.33 Although many youth (52.8%)34 and young adult (62.3%)35 smokers are interested in quitting using cigarettes, it is not clear that these populations are using e-cigarettes to do so or whether e-cigarettes are an effective aid in these populations. With no published evidence of the likelihood that adolescent and young adult smokers transition to the exclusive use of e-cigarettes or to complete abstention from both tobacco products, this possible positive public health impact of e-cigarettes in youth and young adults remain uninvestigated.
In the current study, we aimed to assess 2 critical questions that are central to the evaluation of the public health impact of e-cigarettes on youth. First, among baseline never smokers, we assessed the association of e-cigarette use with the frequency of smoking in the past 30 days at follow-up in a prospective study with a large pooled sample in which 3 cohorts of youth in California and Connecticut were combined. We aimed to evaluate whether e-cigarette users who initiate cigarette smoking are disproportionately represented by young people who are only temporarily experimenting, resulting in a reduced risk of progression to higher levels of smoking in contrast to nonusers of e-cigarettes, or whether the progression to more frequent cigarette use equals or exceeds the typical probability of transitioning observed among non–e-cigarette users, which would suggest that the e-cigarette–to–cigarette use transition is a significant public health concern. Second, we examined the rates of transition from cigarette use or the dual use of e-cigarettes and cigarettes to the exclusive use of e-cigarettes or no tobacco product use. Appreciable rates of transition away from cigarette use (to exclusive e-cigarette use or complete abstention) that are substantially lower than the likelihood of continued cigarette use, with or without concurrent e-cigarette use, may benefit the public health of the population of youth and young adult cigarette smokers.
Methods
Participants
Southern California Children’s Health Study
The Southern California Children’s Health Study (CHS) is a population-based prospective cohort study of youth in 12 communities across Southern California.36,37 The use of e-cigarettes was first assessed when participants were in 11th or 12th grade between January 2014 and June 2014 by using a paper-and-pencil questionnaire completed under study staff supervision in school classrooms.36,37 The present analyses are restricted to participants who completed an online follow-up questionnaire between February 2015 and July 2016 (N = 1553; response rate = 74.0%). All participants were ≥18 years of age at follow-up.
Happiness and Health Study
The Happiness and Health (H&H) Study is a population-based prospective cohort study of adolescents in 10 schools in the greater Los Angeles area.3 Students were initially enrolled in the study in ninth grade in the fall of 2013 at participating schools; data were collected every semester by using a paper-and-pencil questionnaire under study staff supervision in school classrooms. In the current analysis, we use data from participants who completed the spring 2014 data collection (baseline, ninth grade) and spring 2015 data collection (follow-up, 10th grade; N = 3190; response rate = 93.9%).
Yale Adolescent Survey Study
The Yale Adolescent Survey Study (YASS) is a cohort study of ninth- to 12th-grade students in southeastern Connecticut.38,39 An initial sample of students was recruited in the fall of 2013 from 3 high schools; data were collected by using a paper-and-pencil questionnaire under study staff supervision in school classrooms. Follow-up questionnaires were completed ∼6 months later (spring 2014) in the same high schools, and surveys were matched by using established procedures40,41 to maintain the confidentiality of participants. The matching procedure for this study is described in detail elsewhere.42 In the present analyses, we included participants who completed a follow-up questionnaire and were successfully matched with their baseline data at follow-up (N = 1404; match rate = 60.0%).
Ethics Statement
The study was approved by the University of Southern California Institutional Review Board and the Yale University Institutional Review Board. For the CHS and H&H Study, participants aged ≥18 years provided written informed consent; for participants <18 years of age at data collection, written or verbal parental informed consent was obtained, and students assented to participation. For the YASS, alternative consent procedures were used wherein investigators sent out an informational letter detailing the study to parents of eligible children who were enrolled in high schools at which data were collected; parents could opt their children out of the survey. Participants were informed before survey completion that participation was not mandatory; completion of the survey was considered to be assent by participants.
Measures
Tobacco and Alternative Tobacco Product Use
At each survey, participants were asked their age at first use of each product, which was used to classify participants as ever users. Participants who had “never tried” a product (“not even 1 or 2 puffs”) were classified as never users. Those reporting an age at first use of each tobacco product or who reported having ever used a product were classified as ever users of that product. Participants were additionally asked the number of days that each product was used in the past 30 days (0, 1–2, 3–5, 6–9, 10–19, 20–29, or all 30 days). Among ever users of a product, participants were categorized as “experimenters” (ever use but no use in the past 30 days), “infrequent users” (use on 1–2 of the past 30 days), or “frequent users” (use on 3–5 or more of the past 30 days). Participants who reported using e-cigarettes, but not cigarettes, in the past 30 days (at baseline or follow-up) were classified as exclusive e-cigarette users; participants who reported using cigarettes, but not e-cigarettes, in the past 30 days were classified as exclusive cigarette users; and participants who reported using both products in the past 30 days were considered dual product users.
Sociodemographic Characteristics
Questionnaires were also used to assess gender, race/ethnicity (Hispanic, non-Hispanic white, and other), baseline grade in high school (ninth, 10th, 11th, and 12th), and parental education (less than high school, high school graduate, some college, or college graduate; CHS and H&H Study only because this information was not available in the YASS).
Statistical Analysis
On the basis of prospectively collected data, we used polytomous logistic regression models to evaluate the association between e-cigarette use at baseline and patterns of tobacco use at follow-up. In analytic models that were restricted to never smokers at baseline, odds ratios (ORs) and 95% CIs were used to estimate the odds of smoking (experimentation, infrequent use, or frequent use relative to never use) associated with e-cigarette use. A second set of models were used to evaluate the association of baseline past-30-day tobacco use (no use, exclusive e-cigarette use, exclusive cigarette use, or dual product use) with past-30-day use at follow-up (no past-30-day use, exclusive e-cigarette use, exclusive cigarette use, or dual product use). Post hoc tests were used to evaluate the heterogeneity of effects. All models were adjusted for gender, race/ethnicity, grade, and cohort by using a missing indicator when appropriate with a random effect for school. We also assessed whether associations varied across cohorts (CHS, H&H Study, YASS) using appropriate interaction terms. Sensitivity analyses were additionally used to assess whether effect estimates differed after adjusting for parental education by using the CHS and H&H Study. All statistical analyses were based on 2-sided hypotheses tested at a .05 level of significance. Analyses were performed by using SAS 9.4 (SAS Institute, Inc, Cary, NC).
Results
Descriptive Results
Demographic data at baseline for each of the 3 cohort studies are presented in Table 1. Both the CHS and H&H Study had ∼50% Hispanic white participants (the CHS had ∼38% white participants; the H&H Study had ∼16% white participants); the YASS had ∼5% Hispanic white participants and ∼85% white participants. The prevalence of e-cigarette use at baseline was slightly higher in the H&H Study (29.2%) than in the CHS and YASS (22.7%–23.1%, respectively). The prevalence of cigarette use at baseline was similar across all 3 studies.
TABLE 1.
Demographic Characteristics of Subjects at Baseline
| CHS (CA) | H&H Study (CA) | YASS (CT) | |
|---|---|---|---|
| N = 1553 | N = 3190 | N = 1404 | |
| Sex | |||
| Male | 752 (48.4) | 1467 (46.0) | 637 (45.4) |
| Female | 801 (51.6) | 1723 (54.0) | 767 (54.6) |
| Race/Ethnicity | |||
| Non-Hispanic white | 592 (38.1) | 512 (16.0) | 1198 (85.3) |
| Hispanic white | 758 (48.8) | 1505 (47.2) | 66 (4.7) |
| Other | 203 (13.1) | 1173 (36.8) | 140 (10.0) |
| Baseline grade | |||
| Ninth | — | 3190 (100.0) | 417 (29.7) |
| 10th | 21 (1.3) | — | 363 (25.9) |
| 11th | 866 (55.8) | — | 340 (24.2) |
| 12th | 666 (42.9) | — | 283 (20.2) |
| Baseline e-cigarette use | |||
| No | 1197 (77.3) | 2211 (70.8) | 1078 (76.9) |
| Yes | 351 (22.7) | 911 (29.2) | 323 (23.1) |
| Baseline cigarette use | |||
| No | 1293 (83.5) | 2660 (85.2) | 1212 (86.3) |
| Yes | 255 (16.5) | 463 (14.8) | 192 (13.7) |
Data are presented as n (%). Totals may vary because of missing data. CA, California; CT, Connecticut; —, no participants.
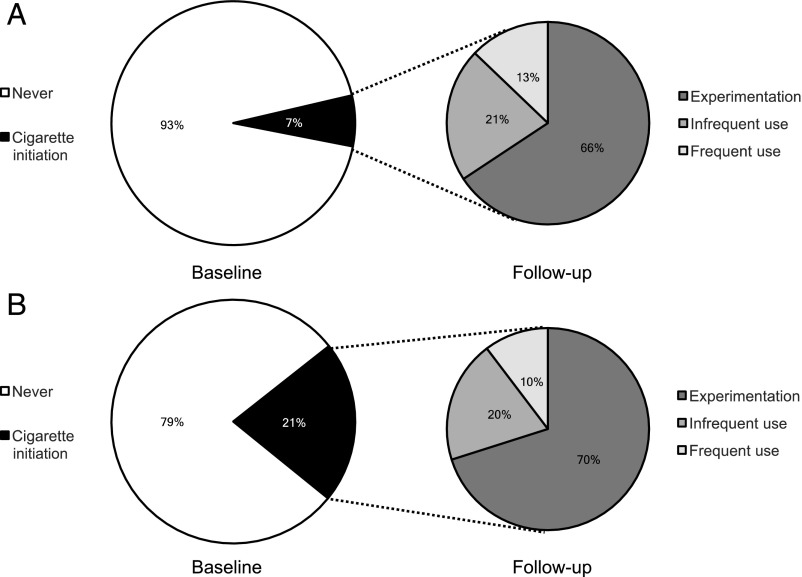
Frequency of Cigarette Use
In the combined sample at follow-up, 9.2% of never smoking youth at baseline had initiated the use of cigarettes; 6.2% were classified as experimenters, 1.9% were infrequent smokers, and 1.1% were frequent smokers (Table 2). Compared with baseline never e-cigarette users, a higher proportion of baseline e-cigarette users reported each category of cigarette use at follow-up (Fig 1): experimentation (15.1% vs 4.4%), infrequent smoking (4.2% vs 1.4%), and frequent smoking (2.2% vs 0.9%). Elevated ORs were observed for baseline e-cigarette use (versus no use) for cigarette experimentation at follow-up (OR = 4.57; 95% CI: 3.56–5.87), infrequent smoking (OR = 4.27; 95% CI: 2.75–6.62), and frequent smoking (OR = 3.51; 95% CI: 1.97–6.24) versus maintaining never use of cigarettes by follow-up. In the sample of adolescents who had initiated cigarette use between baseline and follow-up, the proportion who reported infrequent or frequent use was similar for e-cigarette users and nonusers (see the inset of Fig 1); those who used e-cigarettes at baseline had similar odds of reporting past-30-day infrequent (OR = 0.98; 95% CI: 0.60–1.60) or frequent (OR = 0.76; 95% CI: 0.41–1.42) versus experimental cigarette use at follow-up compared with those who had not used e-cigarettes at baseline. Results did not differ by study (interaction: P > .1; results not shown) or in sensitivity analyses after additional adjustment for parental education.
TABLE 2.
E-cigarette Use and Risk of Subsequent Smoking Among Baseline Never Smokers
| E-cigarette Use (Baseline) | Cigarette Use (Follow-up) | |||
|---|---|---|---|---|
| Never | Experimentationa | Infrequentb | Frequentc | |
| Total, N (%) | 4575 (90.8) | 315 (6.2) | 96 (1.9) | 55 (1.1) |
| Never | 3891 (93.3) | 184 (4.4) | 60 (1.4) | 36 (0.9) |
| Ever | 673 (78.5) | 129 (15.1) | 36 (4.2) | 19 (2.2) |
| Versus never use, adjusted OR (95% CI)d | Reference | 4.57 (3.56–5.87) | 4.27 (2.75–6.62) | 3.51 (1.97–6.24) |
| Versus previous use, adjusted OR (95% CI)e | — | Reference | 0.98 (0.60–1.60) | 0.76 (0.41–1.42) |
—, not applicable.
Experimentation is initiation between baseline and follow-up but no use in the past 30 days.
Infrequent use is initiation and use on 1–2 of the past 30 days.
Frequent use is initiation and use on 3–5 or more of the past 30 days.
Adjusted for sex, race and/or ethnicity, grade, and study; restricted to never cigarette users at baseline with a random effect for school.
Additionally restricted to ever cigarette initiators.
FIGURE 1.
Prevalence of cigarette initiation between baseline and follow-up and, among initiators, frequency of cigarette use at follow-up for never e-cigarette users and e-cigarette users at baseline. A, Never e-cigarette users. B, E-cigarette users.
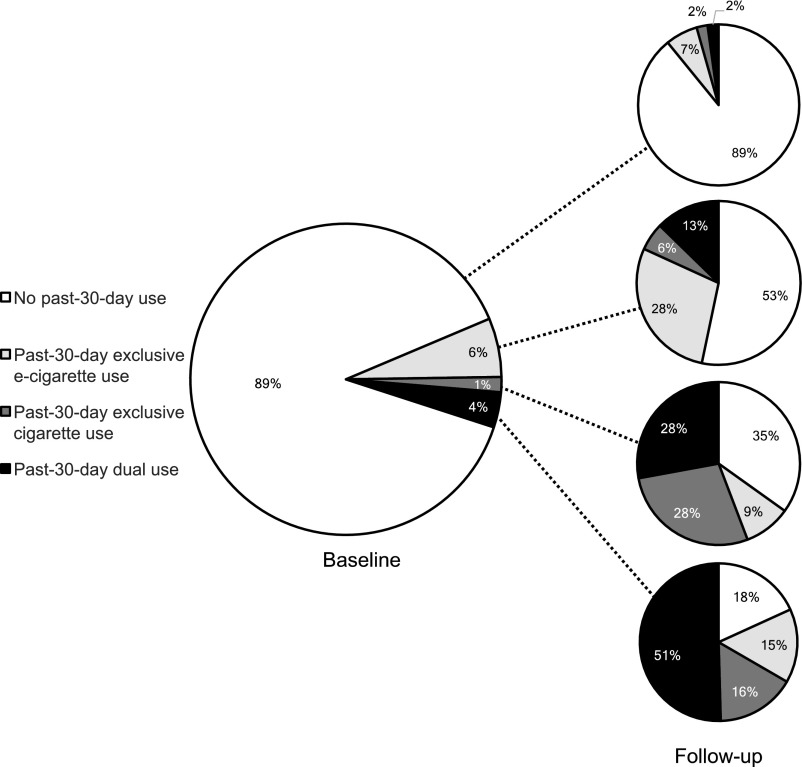
Transitions Between Past-30-Day Nonuse, Single Product Use, and Dual Product Use From Baseline to Follow-up
Among the 2 cohorts for which past-30-day product use data at baseline (N = 2705) were collected, participants who reported that they had not used either product in the past 30 days at baseline were highly likely to remain nonusers (89.2%; Fig 2). Among baseline past-30-day exclusive e-cigarette users, 53.3% were nonusers of either product at follow-up, 28.5% were exclusive e-cigarette users, 5.5% were exclusive cigarette users, and 12.7% were dual product users (see the right inset of Fig 2). Logistic regression models were used to estimate the relative odds of each tobacco use pattern in the past 30 days at follow-up (reference: nonuse of either product). Baseline exclusive e-cigarette users had higher odds of reporting exclusive e-cigarette use at follow-up (OR = 7.28; 95% CI: 4.86–10.9), exclusive cigarette use at follow-up (OR = 3.84; 95% CI: 1.80–8.19), or dual product use at follow-up (OR = 8.86; 95% CI: 5.08–15.4). No statistical differences in the magnitude of the ORs were observed (difference in e-cigarette versus dual product use: P = .53; difference in cigarette versus dual product use: P = .051; difference in e-cigarette versus cigarette use: P = .095).
FIGURE 2.
Prevalence of past-30-day tobacco product use at baseline and follow-up.
Baseline exclusive cigarette users were equally likely to be exclusive cigarette (27.9%) or dual (27.9%) users at follow-up, with 9.3% switching to exclusive e-cigarette use and 34.9% reporting no use of either product at follow-up. Relative to baseline nonusers of either product, baseline exclusive cigarette users had greater odds of reporting exclusive cigarette use (OR = 29.5; 95% CI: 12.3–70.8), dual product use (OR = 28.8; 95% CI: 12.6–66.1), or exclusive e-cigarette use (OR = 4.03; 95% CI: 1.30–12.6) versus nonuse of either product at follow-up; ORs were significantly greater for exclusive cigarette or dual product use relative to exclusive e-cigarette use at follow-up (difference in e-cigarette versus dual product use: P = .002; difference in e-cigarette versus cigarette use: P = .002), but no difference in the magnitude of ORs was observed for the likelihood of exclusive cigarette versus dual product use at follow-up (difference in cigarette versus dual product use: P = .96).
Participants who were dual past-30-day product users at baseline were likely to be using 1 or more products in the past 30 days at follow up (81.8%), with most remaining as dual product users (51%) and a smaller segment transitioning to exclusive cigarette use (16%). Few dual product users transitioned to exclusive e-cigarette use (15%) or no tobacco use (18%) at follow-up. Baseline dual product users were substantially more likely than those who were not using either product in the past 30 days at baseline to report dual product use (versus no use of either product) at follow-up (OR = 105; 95% CI: 56.6–194), with lower (but still elevated) odds of reporting exclusive cigarette use (OR = 44.3; 95% CI: 20.4–96.1) or exclusive e-cigarette use (OR = 11.3; 95% CI: 5.51–23.2) seen; all ORs were statistically different (difference for all contrasts: P < .01). Patterns were again similar by study, with generally higher ORs for the YASS (interaction: P = .024; results not shown), and did not differ in sensitivity analyses after additional adjustment for parental education.
Analyses in which we evaluated the transition from ever use of tobacco products at baseline to past-30-day use at follow-up are presented in the Supplemental Information (see also Supplemental Fig 3, Supplemental Table 4).
Discussion
Previous results from our research group have revealed that e-cigarette use is associated with subsequent cigarette initiation4,16 and that the frequency of e-cigarette use was associated with the frequency of smoking at a 6-month follow-up in a sample of 10th-grade students.6 Here, we provide new results in a pooled sample showing that the risk of past-30-day smoking and of more frequent smoking after initiation was higher in baseline e-cigarette ever versus never users. A smoking uptake pattern characterized by temporary experimentation without progression to more frequent smoking was not disproportionately represented in youth e-cigarette users versus nonusers who started smoking. Rather, among all smoking initiators, the smoking progression sequence was similar among those who used e-cigarettes at baseline and those who initiated cigarette use without a baseline history of e-cigarette use. Supplemental analyses revealed that the magnitude of associations did not significantly differ by cohort, suggesting that this is a generalizable phenomenon across age groups and locations.
Youth who initiate and quickly progress to more frequent smoking are at a high risk of becoming chronic smokers throughout adulthood,24,27,43–45 resulting in an increased risk of developing tobacco-related diseases. If smoking trajectories of youth who begin cigarette use with or without a previous use of e-cigarettes continue to be similar,44,45 the results from this study and others revealing a robust increase in the odds of smoking initiation due to e-cigarette use heighten concerns about recent trends in e-cigarette use. Because e-cigarettes are used by at least some youth who likely would not ever have begun smoking without having been exposed to e-cigarettes,1,2 the potential negative impact of e-cigarettes on the health of youth via the effect of e-cigarettes on smoking uptake is concerning.
In an evaluation of the likelihood of transitioning from exclusive cigarette or dual product use to exclusive e-cigarette use or abstention from both tobacco products, we found that baseline cigarette and dual product users were at an exceedingly high risk of past-30-day cigarette use or dual product use at follow-up, with a lower likelihood of transition away from smoking seen (Table 3). An appreciable proportion of baseline past-30-day exclusive cigarette and dual product users did transition to no past-30-day use of either product at follow-up (34.9% [exclusive cigarette users] and 18.2%, [dual product users]; Fig 2), and a smaller segment transitioned to exclusive e-cigarette use at follow-up (9.3% [exclusive cigarette users] and 15.2% [dual product users]; Fig 2). However, the likelihood of transitioning from smoking to less harmful tobacco product use patterns (exclusive e-cigarette use or use of neither product) was moderate. Although it is possible that dual product users may be using e-cigarettes with the intention of transitioning away from smoking to exclusive e-cigarette use or no use, the probability of this sequence within 6 months to 1 year was modest. Whether some of the dual product users at follow-up in our study may eventually transition to exclusive e-cigarette use or abstention from both products is unknown and will require further surveillance.
TABLE 3.
Use of E-cigarettes, Cigarettes, or Dual Product Use at Baseline and Odds of Past-30-Day Use at Follow-up
| Baseline Product Use | Past-30-d Use at Follow-up | ||
|---|---|---|---|
| Exclusively E-cigarettes Versus None, OR (95% CI) | Exclusively Cigarettes Versus None, OR (95% CI) | Dual Use Versus None, OR (95% CI) | |
| Past-30-d usea,b,c | |||
| Neither product | Reference | Reference | Reference |
| Exclusively e-cigarettes | 7.28 (4.86–10.9)d | 3.84 (1.80–8.19)d | 8.86 (5.08–15.4)d |
| Exclusively cigarettes | 4.03 (1.30–12.6)d | 29.5 (12.3–70.8)e | 28.8 (12.6–66.1)e |
| Dual product | 11.3 (5.51–23.2)d | 44.3 (20.4–96.1)e | 105 (56.6–194)f |
Superscript letters denote a test of independence of effect estimates by row; estimates sharing letters are not statistically significantly different from one another (P < .05).
Stability estimates of remaining in a use pattern (versus nonuse) on the diagonal.
Adjusted for gender, race and/or ethnicity, grade, and study with a random effect for school.
Restricted to the CHS and YASS.
It is possible that dual product use may be brief or rare for most who successfully transition from smoking to e-cigarette use, similar to those who successfully quit with Food and Drug Administration–approved nicotine replacement therapies, for whom the dual use of cigarettes and nicotine replacement therapy is limited. Therefore, some cases of successful cessation of smoking with e-cigarettes may not have been identified in this analysis. However, we found that most adolescent dual product users remain dual product users within 6 months to 1 year, suggesting that dual product use is most often not a temporary state of transition for youth. Regardless, additional types of analyses and study methodologies are needed to clarify whether e-cigarettes may function as an effective cessation aid in this population. Observational studies of adults to date have generally revealed that e-cigarette use among smokers is associated with a lower likelihood of cigarette smoking cessation.29,46,47 We are not aware of any studies in which researchers explicitly evaluate e-cigarettes as a cessation aid for youth, but studies to date have not found evidence for an association of e-cigarette use with a reduction in the frequency of smoking or for complete cessation.8,13,48
There were some limitations to the study. There were relatively few youth who reported levels of cigarette or e-cigarette use more often than 3 to 5 times in the previous month. Continued follow-up with these cohorts is needed to determine which youth progress to daily smoking in early adulthood. In addition, in the analysis evaluating dual product use, no data on past-30-day e-cigarette use were available at baseline for 1 of the cohorts. Although we adjusted for covariates that were hypothesized to confound the tested associations, we were unable to adjust for other factors that may be important but that were only collected in 1 of the 3 studies (for example, behavioral characteristics, including risk taking propensity or impulsivity or other factors, such as peer tobacco use or approval of use). Finally, the studies represent youth of varying ages in different geographical locations; all analyses were controlled for baseline grade, gender, race/ethnicity and study. Further research to examine factors that may influence regional differences in tobacco use transitions in youth could be useful for state and local tobacco control policy makers. Continued research to explore factors that may promote the transition to nicotine dependence (thus increasing the adverse public health impact of use) are warranted.
With our findings, we suggest that smoking uptake and progression is an adverse public health consequence of high rates of e-cigarette use among youth and young adults. The findings also did not reveal strong evidence of transitioning away from combustible cigarette use as a potential public health benefit of e-cigarette use in young people. Together, these findings reveal that adolescent e-cigarette use may result in an overall adverse impact on the public health of youth and young adults. Additional follow-up in large cohort studies along with data on factors that promote transitioning from e-cigarettes to cigarettes and that inhibit transitioning from cigarettes to e-cigarettes or nonuse are needed to develop targeted interventions to minimize the adverse public health impact of e-cigarettes in the adolescent population.
Glossary
- CHS
Children’s Health Study
- CI
confidence interval
- e-cigarette
electronic cigarette
- H&H
Happiness and Health
- OR
odds ratio
- YASS
Yale Adolescent Survey Study
Footnotes
Dr Barrington-Trimis formulated the research question, interpreted the results, wrote and edited the manuscript, and is the guarantor; Ms Liu and Ms Mayer contributed to formulating the research question, conducted the analyses, interpreted the results, and edited the manuscript; Drs Kong and Cruz contributed to formulating the research question, the interpretation of results, and the editing of the manuscript; Drs Leventhal, Krishnan-Sarin, and McConnell designed the study (each cohort), collected data, contributed to formulating the research question and the interpretation of the results, and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by grant P50CA180905 (Drs Barrington-Trimis, Leventhal, Cruz, and McConnell and Ms Liu) from the National Cancer Institute at the National Institutes of Health and the Food and Drug Administration Center for Tobacco Products and grants R01DA033296 (Dr Leventhal), P50DA036151 (Drs Kong and Krishnan-Sarin and Ms Mayer), and K01DA042950 (Dr Barrington-Trimis) from the National Institute on Drug Abuse at the National Institutes of Health. The funders had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the article. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Barrington-Trimis JL, Urman R, Leventhal AM, et al. E-cigarettes, cigarettes, and the prevalence of adolescent tobacco use. Pediatrics. 2016;138(2):e20153983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dutra LM, Glantz SA. E-cigarettes and national adolescent cigarette use: 2004-2014. Pediatrics. 2017;139(2):e20162450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leventhal AM, Strong DR, Kirkpatrick MG, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314(7):700–707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barrington-Trimis JL, Urman R, Berhane K, et al. E-cigarettes and future cigarette use. Pediatrics. 2016;138(1):e20160379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Unger JB, Soto DW, Leventhal A. E-cigarette use and subsequent cigarette and marijuana use among Hispanic young adults. Drug Alcohol Depend. 2016;163:261–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leventhal AM, Stone MD, Andrabi N, et al. Association of e-cigarette vaping and progression to heavier patterns of cigarette smoking. JAMA. 2016;316(18):1918–1920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Primack BA, Soneji S, Stoolmiller M, Fine MJ, Sargent JD. Progression to traditional cigarette smoking after electronic cigarette use among US adolescents and young adults. JAMA Pediatr. 2015;169(11):1018–1023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, Williams RJ. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tob Control. 2017;26(1):34–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miech R, Patrick ME, O’Malley PM, Johnston LD. E-cigarette use as a predictor of cigarette smoking: results from a 1-year follow-up of a national sample of 12th grade students. Tob Control. 2017;26(e2):e106–e111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spindle TR, Hiler MM, Cooke ME, Eissenberg T, Kendler KS, Dick DM. Electronic cigarette use and uptake of cigarette smoking: a longitudinal examination of U.S. college students. Addict Behav. 2017;67:66–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gmel G, Baggio S, Mohler-Kuo M, Daeppen JB, Studer J. E-cigarette use in young Swiss men: is vaping an effective way of reducing or quitting smoking? Swiss Med Wkly. 2016;146:w14271. [DOI] [PubMed] [Google Scholar]
- 12.Best C, Haseen F, Currie D, et al. Relationship between trying an electronic cigarette and subsequent cigarette experimentation in Scottish adolescents: a cohort study [published online ahead of print July 22, 2017]. Tob Control. doi: 10.1136/tobaccocontrol-2017-053691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Conner M, Grogan S, Simms-Ellis R, et al. Do electronic cigarettes increase cigarette smoking in UK adolescents? Evidence from a 12-month prospective study [published online ahead of print August 17, 2017]. Tob Control. doi: 10.1136/tobaccocontrol-2016-053539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loukas A, Marti CN, Cooper M, Pasch KE, Perry CL. Exclusive e-cigarette use predicts cigarette initiation among college students. Addict Behav. 2018;76:343–347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morgenstern M, Nies A, Goecke M, Hanewinkel R. E-cigarettes and the use of conventional cigarettes. Dtsch Arztebl Int. 2018;115(14):243–248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bold KW, Kong G, Camenga DR, et al. Trajectories of e-cigarette and conventional cigarette use among youth. Pediatrics. 2018;141(1):e20171832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aleyan S, Cole A, Qian W, Leatherdale ST. Risky business: a longitudinal study examining cigarette smoking initiation among susceptible and non-susceptible e-cigarette users in Canada. BMJ Open. 2018;8(5):e021080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hammond D, Reid JL, Cole AG, Leatherdale ST. Electronic cigarette use and smoking initiation among youth: a longitudinal cohort study. CMAJ. 2017;189(43):E1328–E1336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Treur JL, Rozema AD, Mathijssen JJP, van Oers H, Vink JM. E-cigarette and waterpipe use in two adolescent cohorts: cross-sectional and longitudinal associations with conventional cigarette smoking. Eur J Epidemiol. 2018;33(3):323–334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lozano P, Barrientos-Gutierrez I, Arillo-Santillan E, et al. A longitudinal study of electronic cigarette use and onset of conventional cigarette smoking and marijuana use among Mexican adolescents. Drug Alcohol Depend. 2017;180:427–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Soneji S, Barrington-Trimis JL, Wills TA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(8):788–797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.US Department of Health and Human Services; Centers for Disease Control and Prevention; National Center for Chronic Disease Prevention and Health Promotion; Office on Smoking and Health . E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2016 [Google Scholar]
- 23.Kozlowski LT, Warner KE. Adolescents and e-cigarettes: objects of concern may appear larger than they are. Drug Alcohol Depend. 2017;174:209–214 [DOI] [PubMed] [Google Scholar]
- 24.Colder CR, Mehta P, Balanda K, et al. Identifying trajectories of adolescent smoking: an application of latent growth mixture modeling. Health Psychol. 2001;20(2):127–135 [DOI] [PubMed] [Google Scholar]
- 25.Audrain-McGovern J, Rodriguez D, Tercyak KP, Epstein LH, Goldman P, Wileyto EP. Applying a behavioral economic framework to understanding adolescent smoking. Psychol Addict Behav. 2004;18(1):64–73 [DOI] [PubMed] [Google Scholar]
- 26.Robinson ML, Berlin I, Moolchan ET. Tobacco smoking trajectory and associated ethnic differences among adolescent smokers seeking cessation treatment. J Adolesc Health. 2004;35(3):217–224 [DOI] [PubMed] [Google Scholar]
- 27.Riggs NR, Chou CP, Li C, Pentz MA. Adolescent to emerging adulthood smoking trajectories: when do smoking trajectories diverge, and do they predict early adulthood nicotine dependence? Nicotine Tob Res. 2007;9(11):1147–1154 [DOI] [PubMed] [Google Scholar]
- 28.US Department of Health and Human Services; National Institutes of Health; National Cancer Institute . Phenotypes and Endophenotypes: Foundations for Genetic Studies of Nicotine Use and Dependence. NIH Publication No. 09-6366. Bethesda, MD: US Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2009 [Google Scholar]
- 29.Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med. 2016;4(2):116–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2016;9:CD010216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McRobbie H, Bullen C, Hartmann-Boyce J, Hajek P. Electronic cigarettes for smoking cessation and reduction. Cochrane Database Syst Rev. 2014;(12):CD010216. [DOI] [PubMed] [Google Scholar]
- 32.Tsai J, Walton K, Coleman BN, et al. Reasons for electronic cigarette use among middle and high school students - National Youth Tobacco Survey, United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(6):196–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hong H, Liu F, Urman R, McConnell R, Barrington-Trimis J. Reasons for electronic cigarette use among Southern California young adults. In: Proceedings of the American Thoracic Society International Conference; May 19–24, 2017; Washington, DC [Google Scholar]
- 34.Tworek C, Schauer GL, Wu CC, Malarcher AM, Jackson KJ, Hoffman AC. Youth tobacco cessation: quitting intentions and past-year quit attempts. Am J Prev Med. 2014;47(2,suppl 1):S15–S27 [DOI] [PubMed] [Google Scholar]
- 35.Babb S, Malarcher A, Schauer G, Asman K, Jamal A. Quitting smoking among adults - United States, 2000-2015. MMWR Morb Mortal Wkly Rep. 2017;65(52):1457–1464 [DOI] [PubMed] [Google Scholar]
- 36.Barrington-Trimis JL, Berhane K, Unger JB, et al. Psychosocial factors associated with adolescent electronic cigarette and cigarette use. Pediatrics. 2015;136(2):308–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McConnell R, Berhane K, Yao L, et al. Traffic, susceptibility, and childhood asthma. Environ Health Perspect. 2006;114(5):766–772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Krishnan-Sarin S, Morean ME, Camenga DR, Cavallo DA, Kong G. E-cigarette use among high school and middle school adolescents in Connecticut. Nicotine Tob Res. 2015;17(7):810–818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kong G, Morean ME, Cavallo DA, Camenga DR, Krishnan-Sarin S. Reasons for electronic cigarette experimentation and discontinuation among adolescents and young adults. Nicotine Tob Res. 2015;17(7):847–854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McGloin J, Holcomb S, Main DS. Matching anonymous pre-posttests using subject-generated information. Eval Rev. 1996;20(6):724–736 [DOI] [PubMed] [Google Scholar]
- 41.Yurek LA, Vasey J, Sullivan Havens D. The use of self-generated identification codes in longitudinal research. Eval Rev. 2008;32(5):435–452 [DOI] [PubMed] [Google Scholar]
- 42.Bold KW, Kong G, Cavallo DA, Camenga DR, Krishnan-Sarin S. E-cigarette susceptibility as a predictor of youth initiation of e-cigarettes. Nicotine Tob Res. 2018;20(4):527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chassin L, Presson CC, Sherman SJ, Edwards DA. The natural history of cigarette smoking: predicting young-adult smoking outcomes from adolescent smoking patterns. Health Psychol. 1990;9(6):701–716 [DOI] [PubMed] [Google Scholar]
- 44.US Department of Health and Human Services; Centers for Disease Control and Prevention; National Center for Chronic Disease Prevention and Health Promotion; Office on Smoking and Health . The Health Consequences of Smoking - 50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014 [Google Scholar]
- 45.US Department of Health and Human Services; Centers for Disease Control and Prevention; Office on Smoking and Health . Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health; 2012 [Google Scholar]
- 46.Glantz SA, Bareham DW. E-cigarettes: use, effects on smoking, risks, and policy implications. Annu Rev Public Health. 2018;39:215–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kulik MC, Lisha NE, Glantz SA. E-cigarettes associated with depressed smoking cessation: a cross-sectional study of 28 European Union countries. Am J Prev Med. 2018;54(4):603–609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Doran N, Brikmanis K, Petersen A, et al. Does e-cigarette use predict cigarette escalation? A longitudinal study of young adult non-daily smokers. Prev Med. 2017;100:279–284 [DOI] [PMC free article] [PubMed] [Google Scholar]