Abstract
Xanthogranulomatous pyelonephritis is a rare form of chronic pyelonephritis in which the involved areas of the kidneys are destroyed and replaced by foam cells. It usually occurs in immunocompromised middle-aged females with ureteral obstruction or chronic urinary tract infection induced by the formation of renal stones. We herein report the case of a 44-year-old woman, with a history of left kidney staghorn calculi and recurrent urinary tract infections. Abdominal computed tomography showed the ‘bear paw’ sign, typical appearance of XGP and patient underwent a nephrectomy with uneventful post-operative course.
Keywords: Xantogranulomatous, Pyelonephritis, Urinary stone, Complication, Computed Tomography
CASE REPORT
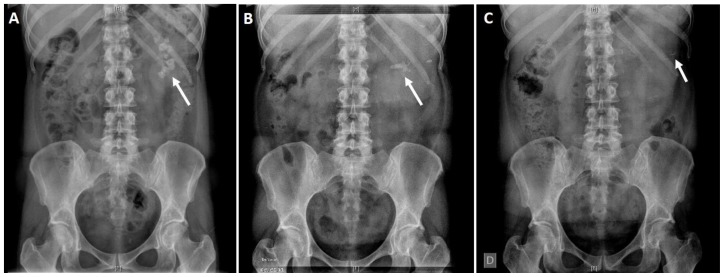
A 44-year-old woman, with a history of recurrent kidney stones and urinary tract infections, presented with left flank pain, fatigue and fever. She had previously undergone percutaneous nephrolithotomy and extracorporeal shock wave lithotripsy one year ago (Figure 1A–B) for left kidney staghorn calculi.
Figure 1.
A 44-year-old female with Xanthogranulomatous pyelonephritis.
Findings: Plain abdominal X-ray (KUB) shows: (A) Initial high burden left renal stone (September 2017). (B) Residual mid calyceal stone after percutaneous nephrolithotomy (October 2017). (C) Minimal residual fragments after extracorporeal shock wave lithotripsy (November 2017).
Technique: Abdominal Radiographs. Manufacturer: Siemens. Model name: Fluorospot Compact FD. 40 mAs, 75 kVp.
Physical examination revealed that the patient was uncomfortable on palpation of left flank. Laboratory tests revealed leukocytosis, with white blood cell count 18,200/mL (range: 3,600–10,500/ml), hemoglobin level 7.5 g/dL (range: 11.8–15.8 g/dL), creatinine level 1.19 mg/dL (range: 0.5–1.1 mg/dL), raised inflammatory markers as C-reactive protein 29.6 mg/L (range < 5 mg/L), normal liver function tests, and elevated Gamma-Glutamyl Transpeptidase 137 U/L (range: 0–55 U/L). Urinalysis revealed pyuria, with positive cultures for Escherichia Coli.
She had no previous history for autoimmune diseases, tuberculosis exposure or primary immunodeficiencies. Other pertinent medical history included obesity, hypertension, and hyperlipidemia.
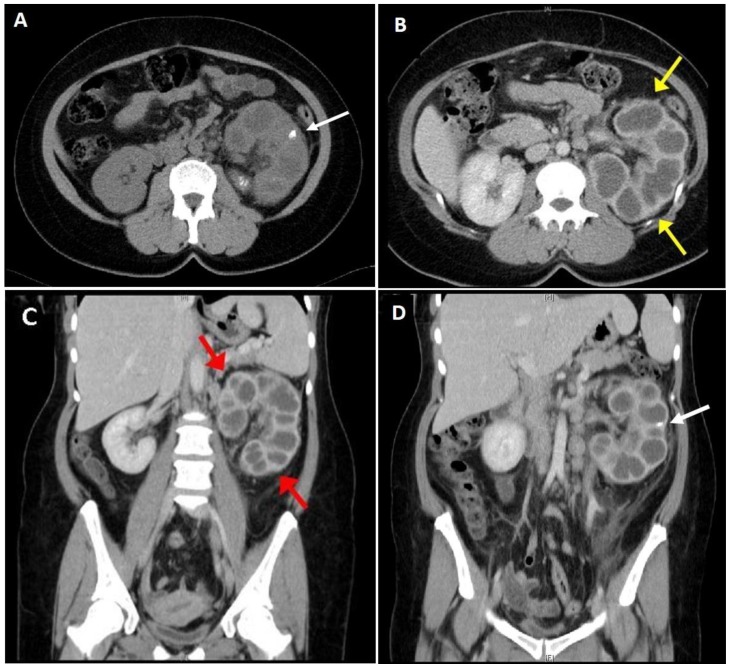
Plain X-ray of the abdomen (KUB) showed small residual fragments in mid and lower calyces (Figure 1C); meanwhile, abdominal ultrasound (US) showed renal enlargement with pelvicalyceal dilatation, parenchymal destruction and multiple anechoic areas with hyperechogenic septa (Figure 2). Abdominal computed tomography (CT) (Figure 3A–D) demonstrated residual renal calculi with dilated calyces and multiloculated appearance (low density [15–18 HU] rounded areas throughout the enlarged [12.2 cm × 9.1 cm] left kidney). It was similar to the paw print of a bear (bear’s paw sign), indicating the typical appearance of xanthogranulomatous pyelonephritis (XGP). No magnetic resonance imaging (MRI) or MAG-3 scan was performed.
Figure 2.
A 44-year-old female with Xanthogranulomatous pyelonephritis.
Findings: Abdominal ultrasound demonstrates renal enlargement with pelvicalyceal dilatation, parenchymal destruction and multiple anechoic areas with hyperechogenic septa.
Technique: (A) Abdominal ultrasound. Manufacturer: General Electric. Model name: GE Logiq 5. Transducer: GE 3.5C convex.
Figure 3.
A 44-year-old female with Xanthogranulomatous pyelonephritis.
Findings: (A) Axial non-contrast computed tomography scan of the abdomen and pelvis demonstrating dilated renal pelvis and calyces and a multiloculated appearance of the enlarged left kidney with mid calyx residual stone fragments (white arrow). (B) Contrast-enhanced computed tomography scan showing an enlarged (12.2 cm × 9.1 cm) left kidney (yellow arrows) and normal right kidney (9.4 cm × 5.5 cm) in axial section. (C) Coronal section of a contrast-enhanced computed tomography scan with low density [15–18 HU] rounded areas throughout the enlarged left kidney and bright enhancement of the rims of the collections (red arrows). (D) Coronal section of a contrast-enhanced computed tomography scan with residual stone fragments (white arrow).
Technique: (A) Axial CT. Body part examined: abdomen. Software version: syngo CT2006G. Manufacturer: Siemens. Model name: Sensation 16. DS slice thickness: 5 mm. mAs: 133. kV: 120.
(B) Axial CT. Body part examined: abdomen. Software version: syngo CT2006G. Manufacturer: Siemens. Model name: Sensation 16. DS slice thickness: 5 mm. mAs: 133. kV: 120. Contrast: 75 mL, Iohexol (Omnipaque®).
(C) Coronal CT. Body part examined: abdomen. Software version: syngo CT2006G. Manufacturer: Siemens. Model name: Sensation 16. DS slice thickness: 5 mm. mAs: 133. kV: 120. Contrast: 65 mL, Iohexol (Omnipaque®).
(D) Coronal CT. Body part examined: abdomen. Software version: syngo CT2006G. Manufacturer: Siemens. Model name: Sensation 16. DS slice thickness: 5 mm. mAs: 133. kV: 120. Contrast: 65 mL, Iohexol (Omnipaque®).
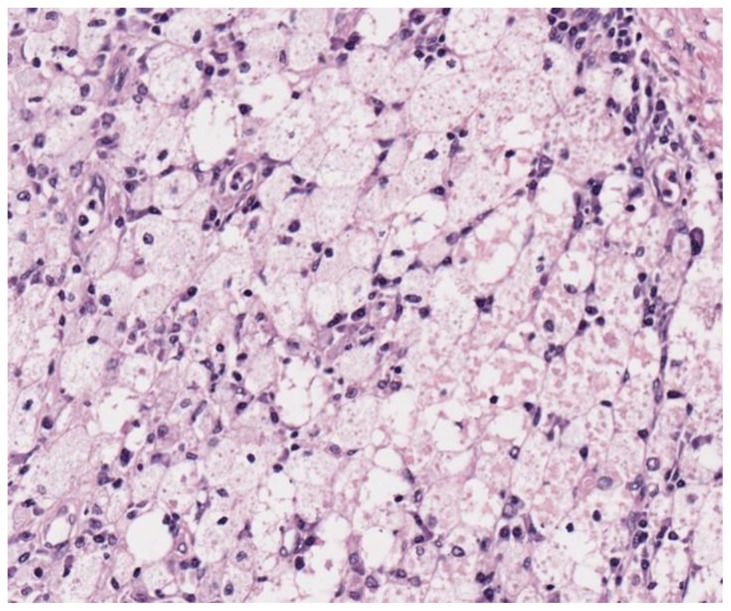
The patient was diagnosed with stage I XGP and completed a 7-days intravenous ceftriaxone antibiotic treatment and underwent an open left nephrectomy. The resected kidney was 14.1 × 8.3 × 4.9 cm in size. Histology showed large amounts of inflammatory cells, fibrosis and a large number of foamy histiocytes (Figure 4).
Figure 4.
A 44-year-old female with Xanthogranulomatous pyelonephritis.
Findings: Infiltration of inflammatory cells including foam cells, plasma cells, and lymphocytes.
Technique: Histopathology. (Stain: hematoxylin and eosin; Magnification: 400×).
The patient’s postoperative course was uneventful, and she was discharged on postoperative day 4 with a 7-day course of antibiotics. Contralateral urinary tract was evaluated closely during the follow-up, with emphasis on urinary tract infection (UTI) prevention maneuvers.
DISCUSSION
Etiology & Demographics
XGP is a rare chronic destructive granulomatous inflammation of renal parenchyma that was first described by Schlagenhaufer in 1916. It accounts for only 0.6% of all chronic pyelonephritis cases [1]. It is more prevalent in women than in men as indicated by the male-to-female ratio of 3:7 [2]. XGP has two morphological subtypes: focal form (confined to one segment with the greater part of the kidney intact) [1,3] and diffuse form (here, the whole kidney is affected, destroyed and replaced by granulomatous tissues containing lipid-laden macrophages or foam cells).
Several etiologies, including calculus or non-calculus urinary obstruction, urosepsis, chronic renal ischemia, lymphatic obstruction, alterations in lipid metabolism, and an altered immune response, are thought to be responsible for the pathogenesis of XGP [3]. It usually occurs in immunocompromised middle-aged females with ureteral obstruction or chronic urinary tract infection induced by the formation of renal stones [5]. However, some cases have also been reported in children and the elderly [6]. Urine cultures are usually positive for Proteus and E. coli [5] in 70% of cases, although other pathogens may also be found.
Clinical & Imaging findings
Its clinical presentation is non-specific and variable, with flank pain, fever, fatigue, weight loss, and anorexia being the most common physical findings [2].
The manifestations of XGP are classified into three stages: Stage 1 (localized disease confined to renal parenchyma), Stage 2 (inflammation involves the perirenal space [perinephric fat]), and Stage 3 (inflammation spread further to involve the paranephric spaces and/or abdominal wall) [4]. This aggressive process is not exclusive to the involved organ and can extend to the adjacent surrounding structures as well.
Laboratory studies often show leucocytosis, anemia, elevated C-reactive protein, and erythrocyte sedimentation rate. It should be noted that the diagnosis of XGP can be challenging as the clinical and radiological manifestations resemble other malignancies and infections. Radiological manifestations are variable and depend on the stage of the disease [7]. XGP typically appears as a hypoechoic lesion on US but is usually non-specific and require additional imaging with CT or MRI. On CT, XGP is associated with an enlarged kidney (or of a segment), poor or no excretion of contrast into the collecting system, and multiple focal low-attenuation (−10 to +30 HU) masses scattered throughout the involved kidney portions. The low attenuation collection represents dilated, debris-filled calyces, and xanthoma collections. The collection themselves do not enhance, and there is no excretion of contrast, but there is bright enhancement of the rims of the collections, because of inflammatory hypervascularity [8]. The dilated and enlarged renal pelvis and calyxes gives a multiloculated appearance, mimicking the toe pads of a bear’s paw. However, such a manifestation may not always be present. T1-weighted MRI images show a hyperintense appearance of included cavitary borders, with hypointense cavitary fluid and perirenal strands. In comparison, T2-weighted images are isointense in cavitary borders with hyperintensity in cavitary fluid and hypointensity in perirenal strands [9].
Differential Diagnoses
The differential diagnosis of XGP includes clear cell renal cell carcinoma (RCC), sarcomatoid RCC, renal abscess, tuberculosis and angiomyolipoma (Table 2). The clear cells of RCC may mimic the lipid-laden xanthomatous cells in XGP. RCC can be hypo-iso-hyperechoic on US and can be observed as heterogeneous, hypodense and hyperdense parenchymal mass with hemorrhage and necrosis on CT. On MRI, RCC are hypo to isointense on T1 and iso to hyperintense on T2 [10]. Sarcomatoid RCC is often described as solid hypodense mass on CT; meanwhile, on MRI, necrosis is evident as hypointense signal on T1 with corresponding T2 hyperintensity [10,11]. Renal tuberculosis presents as necrotic heterogeneous mass on US, mass with calcifications on CT, and hypoperfused areas on contrast-enhanced, fat-suppressed T1 with central hyperintense areas on T2 [12]. Angiomyolipoma develops as cortical heterogeneous lesions with fatty (low) attenuation and variable enhancement pattern on CT and with high intensity on non-enhanced T1 (fat) but isointense to perinephric fat on T2 MRI [13]. Renal abscess can appear as hypoechoic complex cystic mass on US, low-attenuation mass with peripheral enhancement and possible gas collections on CT. It can appear as peripherally enhancing mass and gas collections on MRI [14].
Table 2.
Differential diagnoses table for Xanthogranulomatous pyelonephritis (XGP).
| US | CT | MRI | |
|---|---|---|---|
| XGP | Renal enlargement with pelvicalyceal dilatation, parenchymal destruction and multiple anechoic areas with hyperechogenic septa. | Multiloculated appearance (low density rounded areas throughout the enlarged left kidney): bear’s paw sign. | T1-weighted:
|
| Clear cell RCC | Can be hypo-iso-hyperechoic and heterogeneous [10]. | Hypodense and hyperdense parenchymal mass with hemorrhage and necrosis [10]. |
|
| Sarcomatoid RCC | Large solid to cystic mass [10,11]. | Solid hypodense mass [10,11]. | Necrosis is evident as hypointense signal on T1 with corresponding T2 hyperintensity [10,11]. |
| Tuberculosis | Necrotic heterogeneous mass | Mass with calcifications and cortical scarring |
|
| Angiomyolipoma | Intense echogenicity Well-circumscribed [13]. |
|
|
| Renal Abscess | Anechoic/hypoechoic complex cystic mass [14]. | Low-attenuation mass with peripheral enhancement and possible gas collections [14]. | Peripherally enhancing mass and gas collections [14]. |
MRI fat suppression imaging has been reported to be useful, but angiomyolipoma, retroperitoneal liposarcoma, and some RCCs also contain fat lesions, making it difficult to make preoperative diagnosis of XGP [9]. Immunohistochemical study can play an essential role in the differential diagnosis. It should be noted that XGP is positive for CD68, whereas RCC is positive for CD10 and epithelial membrane antigen. Vimentin can stain positive for both XGP and RCC, and sarcomatoid RCC shows positivity for cytokeratin and epithelial membrane antigen [15].
Treatment & Prognosis
A high rate of complications, including hemorrhage, perforation with abscess formation, fistula tracts (renocutaneous, reno-colonic, reno-duodenal), hepatic dysfunction (reversible), secondary amyloidosis [16] and sepsis, is associated with XGP. The therapeutic approach to XGP is based on the extent of the disease [17]. Symptomatic management along with broad-spectrum antibiotics and initial nephrostomy (for decompression and evacuation as part of managing sepsis), before the surgical treatment and during postsurgical care have been associated with the successful management and better prognosis of the disease [1,18]. Conservative therapeutic management has been reported in experimented centers [19], but nephrectomy with resection of all other involved tissues is the treatment of choice in septic patients and treatment-resistant cases.
TEACHING POINT
Xanthogranulomatous Pyelonephritis (XGP) is a rare entity that usually occurs in immunocompromised middle-aged females with ureteral obstruction or chronic urinary tract infection induced by the formation of renal stones.
Imaging plays a significant role in assessing disease extension and associated complications. CT findings in XGP include multiloculated low-density rounded areas throughout the enlarged kidney (bear’s paw sign). XGP MRI features include hyperintense (or isointense) appearance of the solid component and hypointense cavity fluid on T1-weighted images. The administration of contrast material can reveal strong rim enhancement of the borders.
Without treatment, XGP can become a life-threatening disease. Thus, the usual management is nephrectomy.
Table 1.
Summary table of Xanthogranulomatous pyelonephritis (XGP).
| Etiology | Long-term renal obstruction and infection. Urolithiasis. |
| Clinical Presentation |
|
| Incidence | 0.6% of all chronic pyelonephritis cases. |
| Gender Ratio | Male to female ratio of 3:7 |
| Age Predilection | Middle-age: 40–50 years |
| Risk Factors | Urinary obstruction, urosepsis, chronic renal ischemia, lymphatic obstruction, alterations in lipid metabolism, and altered immune response. |
| Treatment |
|
| Prognosis | Surgical resection usually curative. |
| Imaging Findings |
|
ABBREVIATIONS
- CD10
Cluster of Differentiation 10
- CD68
Cluster of Differentiation 68
- CT
Computed tomography
- HU
Hounsfield Unit
- KUB
Kidney, ureter and bladder
- MAG-3
Mercaptuacetyltriglycine
- MRI
Magnetic resonance imaging
- RCC
Renal cell carcinoma
- US
Abdominal ultrasound
- UTI
Urinary tract infection
- XGP
Xanthogranulomatous pyelonephritis
REFERENCES
- 1.Ghoz HM, Williams M, Perepletchikov A, James N, Babeir AA. An unusual presentation of xanthogranulomatous pyelonephritis: psoas abscess with reno-colic fistula. Oxf Med Case Reports. 2016;2016(7):150–3. doi: 10.1093/omcr/omw063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zugor V, Scott GE, Labanaris AP. Xanthogranulomatous Pyelonephritis in Childhood: A critical analysis of 10 cases and of the literature. Urology. 2007;70(1):157–60. doi: 10.1016/j.urology.2007.02.068. [DOI] [PubMed] [Google Scholar]
- 3.Alan C, Ataus S, Tunç B. Xanthogranulamatous pyelonephritis with psoas abscess: 2 cases and review of the literature. Int Urol Nephrol. 2004;36(4):489–93. doi: 10.1007/s11255-004-0858-5. [DOI] [PubMed] [Google Scholar]
- 4.Malek RS, Elder JS. Xanthogranulomatous pyelonephritis: a critical analysis of 26 cases and of the literature. J Urol. 1978;119(5):589–93. doi: 10.1016/s0022-5347(17)57559-x. [DOI] [PubMed] [Google Scholar]
- 5.Chuang CK, Lai MK, Chang PL, et al. Xanthogranulomatous pyelonephritis: experience in 36 cases. J Urol. 1992;147(2):333–336. doi: 10.1016/s0022-5347(17)37229-4. [DOI] [PubMed] [Google Scholar]
- 6.Craig WD, Wagner BJ, Travis MD. Pyelonephritis: radiologic-pathologic review. Radiographics. 2008;28(1):255–77. doi: 10.1148/rg.281075171. [DOI] [PubMed] [Google Scholar]
- 7.Onn LV, Bickle I, Chua HB, Telisinghe PU, Chong CF, Chong VH. Xanthogranulomatous pyelonephritis with reno-colic fistula: A rare complication of urinary tract infection. Malays Fam Physician. 2017;12(3):33–36. [PMC free article] [PubMed] [Google Scholar]
- 8.Dani RD, Gandhi VS, Prajapati HJ, Shah P, Raval H, Rathod GD. Case report: Xanthogranulomatous pyelonephritis - an unusual variety. Indian J Radiol Imaging. 2005;15:195–8. [Google Scholar]
- 9.Verswijvel G, Oyen R, Van Poppel H, Roskams T. Xanthogranulomatous pyelonephritis: MRI findings in the diffuse and the focal type. Eur Radiol. 2000;10(4):586–9. doi: 10.1007/s003300050967. [DOI] [PubMed] [Google Scholar]
- 10.Reiter M, Schwope R, Clarkson A. Sarcomatoid renal cell carcinoma: a case report and literature review. J Radiol Case Rep. 2012;6(4):11–6. doi: 10.3941/jrcr.v6i4.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldsmith S, Harris M, Scherer K, Al-Quran S, Vorhis E. Sarcoidosis manifesting as a pseudotumorous renal mass. J Radiol Case Rep. 2013;7(5):23–34. doi: 10.3941/jrcr.v7i5.1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Merchant S, Bharati A, Merchant N. Tuberculosis of the genitourinary system-Urinary tract tuberculosis: Renal tuberculosis-Part II. Indian J Radiol Imaging. 2013;23(1):64–77. doi: 10.4103/0971-3026.113617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siegel CL, Middleton WD, Teefey SA, McClennan BL. Angiomyolipoma and renal cell carcinoma: US differentiation. Radiology. 1996;198(3):789–93. doi: 10.1148/radiology.198.3.8628873. [DOI] [PubMed] [Google Scholar]
- 14.Dedekam E, Graham J, Strenge K, Mosier AD. Primary renal lymphoma mimicking a subcapsular hematoma: a case report. J Radiol Case Rep. 2013;7(8):18–26. doi: 10.3941/jrcr.v7i8.1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ho CI, Wen YK, Chen ML. Xanthogranulomatous pyelonephritis successfully treated with antibiotics only. J Chin Med Assoc. 2008 Dec;71(12):643–5. doi: 10.1016/S1726-4901(09)70008-5. [DOI] [PubMed] [Google Scholar]
- 16.Hayashi Y, Kawahara T, Hattori Y, et al. Xanthogranulomatous Pyelonephritis with Incomplete Double Ureter. Case Rep Med. 2017;2017:2392670. doi: 10.1155/2017/2392670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bourm KS, Menias CO, Ali K, Alhalabi K, Elsayes KM. Spectrum of Xanthogranulomatous Processes in the Abdomen and Pelvis: A Pictorial Review of Infectious, Inflammatory, and Proliferative Responses. AJR Am J Roentgenol. 2017;208(3):475–484. doi: 10.2214/AJR.16.17075. [DOI] [PubMed] [Google Scholar]
- 18.Yang JH, Shin JY, Roh SG, Chang SC, Lee NH. Delayed diagnosis of xanthogranulomatous pyelonephritis in a quadriplegic patient with uncontrolled cutaneous fistula: A case report. Medicine (Baltimore) 2018;97(2):e9659. doi: 10.1097/MD.0000000000009659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Friedl A, Tuerk C, Schima W, Broessner C. Xanthogranulomatous Pyelonephritis with Staghorn Calculus, Acute Gangrenous Appendicitis and Enterocolitis: A Multidisciplinary Challenge of Kidney-Preserving Conservative Therapy. Curr Urol. 2015 Sep;8(3):162–5. doi: 10.1159/000365709. [DOI] [PMC free article] [PubMed] [Google Scholar]