Abstract
Objective
Insomnia is a highly prevalent disorder among patients suffering from stroke. The association between insomnia and stroke mortality is less studied, particularly using the latest diagnostic criteria. The current study examined the relationship between insomnia and mortality among patients with first-evonal hazard models were used to calculate HRs for stroke er stroke in China.
Methods
Patients with acute cerebrovascular diseases (stroke) were recruited from 56 hospitals in mainland China. Insomnia was defined as difficulty falling asleep, or difficulty staying asleep or waking up early, for at least two consecutive visits. Demographic data, medical history and clinical data were collected. Four follow-up visits occurred within the first year after stroke, and the last follow-up call was conducted 6 years later. Cox proportional hazard models were used to calculate HRs for stroke mortality.
Results
Insomnia was reported by 38.4% (489/1273) of patients at baseline. During the 6 years of follow-up, after adjusting for all confounders, insomnia was found to be associated with increased mortality (HR=1.66, 95% CI 1.10 to 2.48). Old age (HR=1.08, 95% CI 1.06 to 1.10), stroke recurrence in the first year of follow-up (HR=2.53, 95% CI 1.48 to 4.31) and stroke survivors with hypertension (HR=1.62, 95% CI 1.04 to 2.53) had substantially higher risk of mortality.
Conclusions
Besides old age, stroke recurrence in the first year of follow-up and hypertension, insomnia is associated with increased risk of mortality in patients with first-ever stroke in China. More studies about prompt and efficient interventions for insomnia are expected in the future.
Trial registration number
rctn62169508.
Keywords: insomnia, risk factor, mortality, first-ever stroke
Introduction
Previous studies have reported that short sleep durations are associated with increased risks of mortality from stroke.1 2 In addition to short sleep duration, sleep quality may also play a role in disease aetiology.3 However, few studies have explored the effects of insomnia on stroke mortality.4
Insomnia, affecting approximately 12%–57% of stroke survivors, plays an essential role in the prognosis after stroke.5 6 Indeed, poststroke insomnia may have significant deleterious effects. Some studies have reported links between poststroke insomnia and more significant disabilities, including increased risk of subsequent stroke.7 8 Moreover, poststroke insomnia can worsen poststroke depression,9 which decreased outcomes of stroke.10 Although previous studies have reported detrimental effects of insomnia, the diagnositic criteria of insomnia in those studies were not unified.11
Recurrence of stroke is common among stroke survivors with cumulative disability. Furthermore, patients with recurrent stroke have a 43% higher risk of dying than survivors with the first-ever stroke.12 However, previous studies have failed to distinguish the effect of recurrence when studying the relationship between sleep and mortality.
The current study aimed to examine the association between insomnia and mortality in the first-ever stroke in the Chinese population.
Materials and methods
Patients and study settings
This was a 6-year follow-up study of patients with stroke. The baseline data were from a study titled ‘Prospective Cohort Study on the Incidence and Outcome of Patients with Post-stroke Depression in China (PRIOD)’.13 In this study, patients with stroke from 56 neurology departments were recruited between April 2008 and April 2010. Patients aged 18 years or older, whose conditions were confirmed by CT or MRI within 14 days of clinical presentation, were recruited based on the WHO criteria for stroke.14 The patients provided written informed consent and agreed to follow up.
Demographic data (age, gender, living condition, education, marital status and personal characteristics) were collected at intake time. Medical history, past psychiatric diagnosis, vascular risk factors (eg, history of hypertension, diabetes and smoking), clinical characteristics such as type of stroke and National Institute of Health Stroke Scale (NIHSS) score for the first time after admission, and other medical complications (eg, atrial fibrillation, urinary disease and tumours) were also collected at intake time. Exclusion criteria were patients who had a history of stroke; patients with obvious aphasia that impeded the patient from finishing psychological assessment; patients who withdrew from follow-up at any of the following time points; and patients with severe heart disease or nephropathy or tumour, or a history of psychiatric diagnosis, as the above conditions were shown to be associated with insomnia and mortality.15 16
The study was conducted in compliance with the Declaration of Helsinki guidelines for the protection of human subjects.
Measurement and evaluation
In this study, clinical physiologists who were responsible for the follow-up at each centre received systematic training on clinical assessment tools and diagnostic criteria.
Follow-up assessments included the diagnosis of depression based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV),17 and assessment of the Hamilton Rating Scale for Depression (17 items, HRSD-17) at day 14±2, 3 and 6 months, and day 360±7 poststroke.18 19 Stroke severity was assessed at baseline using the NIHSS.
Ascertainment of stroke mortality
All deaths were identified from the local Disease Surveillance Points system death registries. The causes of death were coded according to the 10th International Classification of Diseases. Duration of follow-up was calculated from the time of the baseline evaluation to the date of death.
Definition of insomnia
Insomnia was ascertained using three items from the HRSD-17, consisting of the core symptoms of insomnia in DSM-IV.17 These three questions are the following: (1)‘Have you experienced difficulty falling asleep?’ (2)‘Have you experienced difficulty staying asleep?’ and (3) ‘Have you experienced waking up early and not being able to sleep again?’ Participants were classified as having insomnia if they reported experiencing one or more sleep conditions for at least three nights a week. Patients were classified as having insomnia if they reported experiencing one or more of the above items at two consecutive visits. The two successive follow-up times were at least 3 months or 6 months.
Definition of baseline
Demographic characteristics, vascular risk factors and clinical characteristics were defined as the baseline in this study at intake time. Sleep factors of HRSD-17 in the four assessments during the first year were used to determine whether the patient had insomnia.
Statistical analysis
Statistical analyses were conducted using the Statistical Analysis System (SAS) V.9.2 software. Continuous data are expressed as median (IQR). Discrete data are expressed as frequencies and percentiles. The χ2 test or Fisher’s test was used for analysis. Group differences of continuous data and one-way orderly data were analysed using the Wilcoxon rank-sum test. Cox proportional hazard regressions were used to calculate HRs and their 95% CIs. For all analyses, a two-tailed probability value of P<0.05 was considered statistically significant.
Results
Comparison between patients enrolled and not enrolled
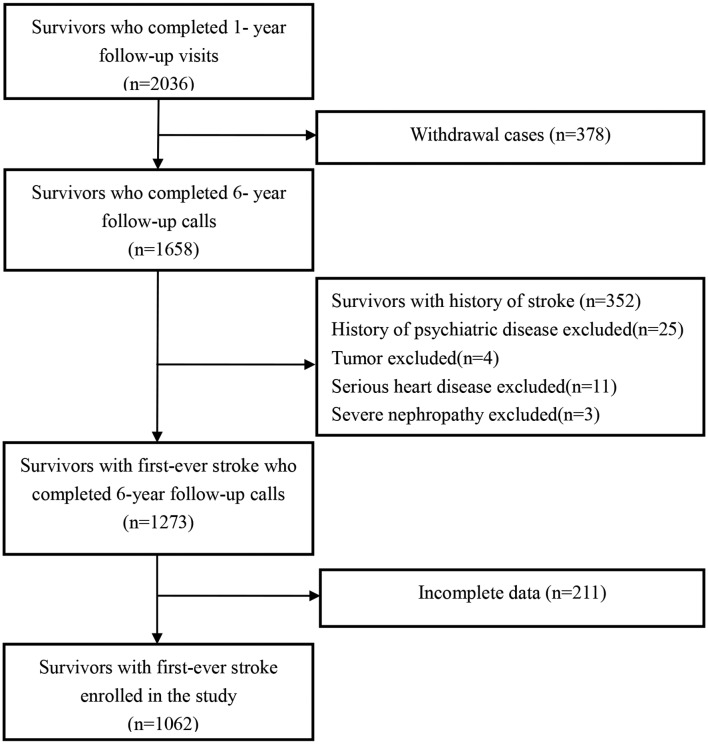
Among 1273 patients with first-ever stroke, 16.6% (211) were excluded from the analyses due to incomplete follow-up, and 1062 patients with first-ever stroke who met the inclusion criteria were enrolled in the study (figure 1). No significant differences were found between patients enrolled (n=1062) and those not enrolled (n=211) (table 1).
Figure 1.
Flow chart of the participant selection.
Table 1.
Comparison of characteristics between patients enrolled in the study and those who withdrew from the follow-up
| Variables | Enrolled (n=1062) | Withdrew (n=211) | P value |
| Demographic characteristics | |||
| Age, year, mean±SD | 60.47±11.57 | 60.60±12.90 | 0.88 |
| Female, n (%) | 364 (34.3) | 72 (34.1) | 0.97 |
| Education level | |||
| High school and above, n (%) | 762 (71.8) | 150 (71.1) | 0.85 |
| Married, n (%) | 992 (93.4) | 193 (91.9) | 0.43 |
| Living alone, n (%) | 1037 (97.6) | 204 (96.7) | 0.41 |
| Employed, n (%) | 502 (47.4) | 96 (45.5) | 0.60 |
| Family history of mental disease, n (%) | 187 (18.2) | 40 (19.9) | 0.56 |
| Vascular risk factors | |||
| Smoker, n (%) | 483 (45.7) | 97 (46.2) | 0.90 |
| Hypertension, n (%) | 708 (67.9) | 142 (69.6) | 0.77 |
| Diabetes, n (%) | 225 (21.6) | 39 (18.8) | 0.38 |
| Hyperlipidaemia, n (%) | 178 (19.1) | 40 (22.1) | 0.35 |
| Clinical characteristics | |||
| Diagnosis of ISH, n (%) | 863 (81.3) | 164 (77.7) | 0.24 |
| NIHSS score at 14±2 days, mean±SD | 4.62±4.03 | 4.62±4.03 | 0.07 |
| Stroke recurrence at 1-year follow-up, n (%) | 65 (7.1) | 11 (5.2) | 0.61 |
| Death at 6-year follow-up, n (%) | 130 (12.2) | 35 (16.6) | 0.40 |
Smoker, with or without a history of smoking.
ISH, ischaemic stroke; NIHSS score, the first National Institutes of Health Stroke Scale.
Demographic and clinical characteristics of patients with insomnia and without insomnia
Among 1062 patients included in the analyses, 489 (38.4%) met the diagnosis of insomnia in the first-year follow-up, 132 (15.5%) suffer from one kind of insomnia listed above, while 356 (33.9%) suffer from mixed features, and 130 (9.4%) patients died. The group of patients with insomnia had significantly higher NIHSS score (5.21±4.38 vs 4.12±3.65, P<0.001), more female patients (39.9% vs 29.5%, P<0.001) and higher rate of depression (54.8% vs 20.8%, P<0.001) at baseline assessment (table 2). Moreover, patients with insomnia had a significantly higher recurrence rate of stroke (8.2% vs 4.4%, P=0.02) during the first-year follow-up and had significantly higher mortality (15.1% vs 9.7%, P=0.008) at 6-year follow-up than those without insomnia. No other significant differences were found between the two groups.
Table 2.
Demographic and clinical characteristics of the study population at baseline
| Variables | All patients | Groups | ||
| (n=1062) | Insomnia (n=489) | Non-insomnia (n=573) | P value | |
| Demographic characteristics | ||||
| Age, year, mean±SD | 60.47±11.57 | 48.9±46.0 | 57.3±54.0 | 0.08 |
| Female, n (%) | 364 (34.3) | 195 (39.9) | 169 (29.5) | <0.001 |
| Education level, n (%) | ||||
| High school and above, n (%) | 762 (72.0) | 351 (71.8) | 411 (72.1) | 0.25 |
| Married, n (%) | 992 (93.5) | 456 (93.3) | 536 (93.5) | 0.90 |
| Living alone, n (%) | 25 (2.4) | 9 (1.84) | 16 (2.8) | 0.42 |
| Employed, n (%) | 502 (47.4) | 215 (44.1) | 287 (50.4) | 0.04 |
| Family history of mental disease, n (%) | 188 (18.3) | 87 (18.2) | 101 (18.3) | 1.0 |
| Vascular risk factors | ||||
| Smoker, n (%) | 483 (45.7) | 216 (44.3) | 267 (46.9) | 0.42 |
| Hypertension, n (%) | 708 (67.9) | 321 (66.7) | 387 (68.9) | 0.47 |
| Diabetes, n (%) | 224 (21.5) | 105 (21.9) | 119 (21.2) | 0.82 |
| Hyperlipidaemia, n (%) | 179 (19.0) | 80 (18.3) | 99 (19.8) | 0.62 |
| Clinical characteristics | ||||
| Diagnosis of ISH, n (%) | 863 (81.3) | 383 (78.3) | 480 (83.8) | 0.02 |
| NIHSS score at 14±2 day, mean±SD | 4.62±4.03 | 5.21±4.4 | 4.12±3.7 | <0.001 |
| Depression at 1-year follow-up, n (%) | 387 (36.4) | 268 (54.8) | 119 (20.8) | <0.001 |
| Stroke recurrence at 1-year follow-up, n (%) | 65 (6.1) | 40 (8.2) | 25 (4.4) | 0.02 |
| Death at 6-year follow-up, n (%) | 130 (12.2) | 74 (15.1) | 56 (9.7) | 0.008 |
Smoker, with or without a history of smoking.
ISH, ischaemic stroke; NIHSS score, the first National Institutes of Health Stroke Scale.
Univariate analysis and multivariate model of death and survivors
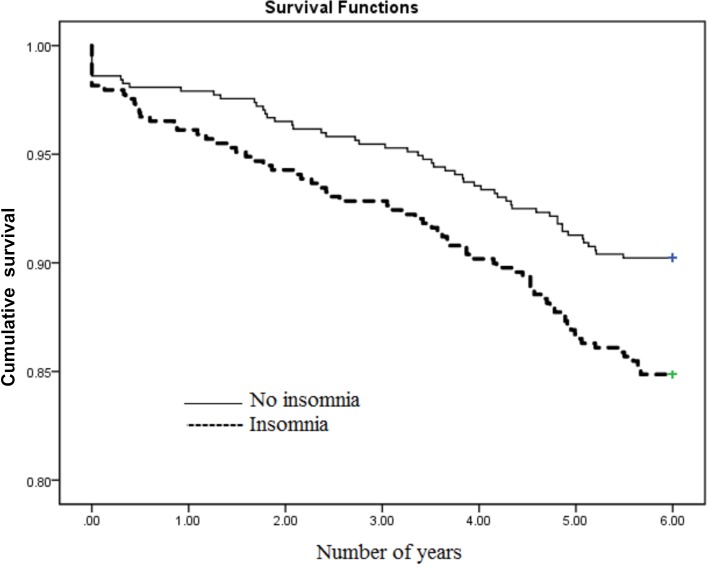
Death within 6 years was associated with old age (69.7±11.0 vs 59.2±11.0, P=0.000), higher rate of insomnia (56.9% vs 44.5%, P=0.01), higher recurrence rate of stroke (14.6% vs 5.0%, P=0.000) during the first year of follow-up, lower education (58.5% vs 73.6%, P=0.000), lower employment rate (21.5% vs 51.2%, P=0.000) and higher rate of hypertension (76.2% vs 66.7%, P=0.03) (table 3). The multivariate Cox regression analysis revealed that age (HR=1.08, 95% CI 1.06 to 1.10), stroke recurrence in the first-year follow-up (HR=2.53, 95% CI 1.48 to 4.31), insomnia (HR=1.66, 95% CI 1.10 to 2.48; figure 2) and hypertension (HR=1.62, 95% CI 1.04 to 2.53) were significantly associated with death at 6-year follow-up (table 4).
Table 3.
Demographic and clinical characteristics of the study population at baseline
| Variables | All patients | Groups | ||
| (n=1062) | Death (n=130) | Survivors (n=932) | P value | |
| Demographic characteristics | ||||
| Age, year, mean±SD | 60.47±11.57 | 69.7±11.0 | 59.2±11.0 | 0.00 |
| Female, n (%) | 364 (34.3) | 51 (39.2) | 313 (33.6) | 0.20 |
| Education level, n (%) | ||||
| High school and above, n (%) | 762 (71.8) | 76 (58.5) | 686 (73.6) | 0.00 |
| Married, n (%) | 992 (93.4) | 118 (90.8) | 874 (93.8) | 0.20 |
| Living alone, n (%) | 25 (2.4) | 6 (4.6) | 19 (2.0) | 0.07 |
| Employed, n (%) | 502 (47.5) | 28 (21.5) | 474 (51.2) | 0.00 |
| Family history of mental disease, n (%) | 188 (18.3) | 15 (12.3) | 173 (19.1) | 0.07 |
| Vascular risk factors | ||||
| Smoker, n (%) | 483 (45.7) | 45 (35.2) | 438 (47.2) | 0.01 |
| Hypertension, n (%) | 708 (67.9) | 99 (76.2) | 614 (66.7) | 0.03 |
| Hyperlipidaemia, n (%) | 179 (19.1) | 17 (14.8) | 162 (19.8) | 0.20 |
| Diabetes, n (%) | 224 (21.5) | 33 (26.2) | 191 (20.9) | 0.17 |
| Clinical characteristics | ||||
| Diagnosis of ISH, n (%) | 863 (81.3) | 111 (78.3) | 752 (85.4) | 0.21 |
| NIHSS score at 14±2 days, mean±SD | 4.62±4.03 | 5.23±4.0 | 4.54±4.0 | 0.07 |
| Depression at 1-year follow-up, n (%) | 387 (36.4) | 49 (37.7) | 338 (36.3) | 0.75 |
| Stroke recurrence at 1-year follow-up, n (%) | 65 (6.1) | 19 (14.6) | 47 (5.0) | 0.00 |
| Insomnia, n (%) | 489 (46.0) | 74 (56.9) | 415 (44.5) | 0.01 |
| Difficulty falling asleep, n (%) | 69 (6.5) | 14 (10.8) | 55 (5.9) | 0.04 |
| Difficulty staying asleep, n (%) | 19 (4.8) | 7 (5.4) | 12 (1.3) | 0.001 |
| Waking up early, n (%) | 44 (4.2) | 6 (4.6) | 38 (4.2) | 0.82 |
| Difficulty falling asleep and staying asleep, n (%) | 52 (4.9) | 7 (5.4) | 45 (4.8) | 0.78 |
| Difficulty falling asleep and waking up early, n (%) | 73 (6.9) | 10 (7.7) | 63 (6.8) | 0.69 |
| Difficulty staying asleep and waking up early, n (%) | 24 (2.3) | 3 (2.3) | 21 (2.3) | 0.97 |
| All of the three, n (%) | 208 (19.8) | 27 (21.5) | 181 (19.5) | 0.59 |
Smoker, with or without a history of smoking.
ISH, ischaemic stroke; NIHSS score, the first National Institutes of Health Stroke Scale.
Figure 2.
Kaplan-Meier survival curves by insomnia status at 6-year follow-up.
Table 4.
Risk factors associated with death in the Cox regression among the first-ever stroke survivors
| Factors | HR | 95% CI | P value |
| Age | 1.08 | 1.06 to 1.10 | 0.000 |
| Insomnia | 1.66 | 1.10 to 2.48 | 0.01 |
| Sex | 1.20 | 0.73 to 1.88 | 0.45 |
| Smoking | 0.97 | 0.63 to 1.51 | 0.90 |
| Marital status | 1.37 | 0.59 to 3.15 | 0.45 |
| Living arrangement | 0.63 | 0.21 to 1.90 | 0.42 |
| Depression | 0.89 | 0.59 to 1.35 | 0.58 |
| Illiteracy | 1.78 | 0.97 to 3.72 | 0.45 |
| Primary education | 0.83 | 0.51 to 1.36 | 0.62 |
| Hypertension | 1.62 | 1.04 to 2.53 | 0.04 |
| Hyperlipidaemia | 0.71 | 0.42 to 1.21 | 0.21 |
| Diabetes mellitus | 1.27 | 0.82 to 1.98 | 0.29 |
| Diagnoses | 0.94 | 0.55 to 1.61 | 0.82 |
| Stroke recurrence at 1-year follow-up | 2.53 | 1.48 to 4.31 | 0.001 |
| NHISS score | 1.03 | 0.98 to 1.08 | 0.21 |
Smoking status, with or without a history of smoking. Diagnoses include ischaemic stroke and haemorrhagic stroke.
NIHSS, the first National Institutes of Health Stroke Scale.
Discussion
So far as is known, this is the first prospective cohort study in China to investigate the relationship between insomnia and mortality in patients with first-ever stroke. The result demonstrated that insomnia was associated with a 1.66-fold increase in the risk of death at 6-year follow-up. The prevalence of insomnia was 38.4%, consistent with the range (12%–57%) reported by other Western researchers.5 6 20
This research adjusted many possible confounders, especially depression, as comorbidity, which was evaluated during the first-year follow-up. The association between insomnia and mortality was not essentially changed by depression.1 21 Also, the result concluded that old age and recurrent stroke within the first year were statistically the most important risk factors for mortality.22 23 The NIHSS scores were significantly more associated with insomnia, while these were not associated with mortality at 6-year follow-up. This result was consistent with another study by Luo et al 24, which exhibited that high NIHSS scores before treatment were associated with mortality at 90 days.
Linking insomnia to mortality had been extensively studied by other research groups25; however, no research has explored the relationship between insomnia and poststroke mortality. This finding showed that insomnia was significantly associated with the increase in mortality. Also, the definition of insomnia in this study stimulated to the diagnostic criteria of insomnia in the DSM-IV. Occurrence of sleep disturbance despite adequate opportunity and circumstances for sleep is required to diagnose insomnia,26 and the participants in this study were discharged from the hospital and met the standard. Furthermore, this study ruled out new tumours, severe heart failure and severe kidney disease, which may be linked to sleep deprivation and further impaired neuropsychological performance.27
This study found that stroke survivors with hypertension had a substantially higher risk of mortality (HR=1.61, 95% CI 1.04 to 2.53), and this result is consistent with previous investigations that showed that blood pressure and blood pressure variability were each associated with poor outcome.2 28 29 Some previous studies suggested that insomnia can lead to hypertension by activating the sympathetic system,30 31 impairing sleep quality, as well as decreasing insulin sensitivity and glucose tolerance.32 Hypertension and diabetes are thought to contribute to higher cardiovascular mortality risk. Extensive research has proved that insomnia increases the risk of mortality in patients with cardiovascular disease (CVD).3 25 33–35 Consequently, these two conditions might partly mediate the association between insomnia and death. Some studies found that patients with stroke who also had CVD or kidney dysfunction had a higher risk of death.15 36 In this study, subjects with severe physical illness were excluded, which might explain the weak statistical power of the result.
Strengths of this study are its large sample size, first-ever stroke and extended follow-up. There are several limitations to the present study that should be noted. First, the definition of insomnia in this study was similar to the diagnostic criteria of insomnia in the DSM-IV, and it qualified in every diagnostic criterion. Second, there are no statistics on the use of hypnotics in this study. Third, this study only included several potential confounding factors.
In summary, insomnia, old age, stroke recurrence in the first-year follow-up and hypertension were high-risk factors for mortality over 6 years of follow-up in the large sample of patients with first-ever stroke. Participants with insomnia suffered a higher recurrence of stroke during the first year of follow-up. Whether prompt and efficient interventions for insomnia can decrease mortality in patients with first-ever stroke is still ambiguous. More studies are expected in the future.
Acknowledgments
We thank all the clinicians, the patients and their families who had participated in this project.
Footnotes
Contributors: All the listed authors have participated actively in the study and approved the submitted manuscript. C-XW, NZ and Y-JW: responsible for conception or design of the work, and approved the final version of the manuscript to be published. YY, QC and A-XW: acquisition, analysis or interpretation of data for the work. C-XW and B-YG: revising the paper critically for important intellectual content. L-JL: conducted the experimental studies and drafted the manuscript.
Funding: This study was funded by National Key Research & Development Program of China (2016YFC1307200), Beijing excellent talents training Program, the Ministry of Science and Technology and the Ministry of Health of the People’s Republic of China. Individual grants include the National 11th & 12th Five-year S & T Major Project (2006BAI01A11, 2011BAI08B01, 2011BAI08B02, 2015BAI13B03), the National Key Technology Research and Development Program of the Ministry of Science and Technology of China (2013BAI09B03), the Ministry of Science and Technology of the People’s Republic of China Beijing Institute for Brain Disorders (BIBD-PXM2013_014226_07_000084), the Beijing Biobank of Cerebral Vascular Disease (D131100005313003), the Basic Clinical Research Cooperation Program of Capital Medical University (16JL(TTZX)03), Beijing Brain Research (Z161100000216131) and the Beijing Municipal Science & Technology Commission (Z151100004015127 and Z151100003915117).
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: The study was approved by the medical ethics committee (IRB) of Beijing Tiantan Hospital, which is affiliated with Capital Medical University.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. Ikehara S, Iso H, Date C, et al. . Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Sleep 2009;32:295–301. 10.1093/sleep/32.3.295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pan A, De Silva DA, Yuan JM, et al. . Sleep duration and risk of stroke mortality among Chinese adults: Singapore Chinese health study. Stroke 2014;45:1620–5. 10.1161/STROKEAHA.114.005181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rod NH, Vahtera J, Westerlund H, et al. . Sleep disturbances and cause-specific mortality: Results from the GAZEL cohort study. Am J Epidemiol 2011;173:300–9. 10.1093/aje/kwq371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chien KL, Chen PC, Hsu HC, et al. . Habitual sleep duration and insomnia and the risk of cardiovascular events and all-cause death: report from a community-based cohort. Sleep 2010;33:177–84. 10.1093/sleep/33.2.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Leppävuori A, Pohjasvaara T, Vataja R, et al. . Insomnia in ischemic stroke patients. Cerebrovasc Dis 2002;14:90–7. 10.1159/000064737 [DOI] [PubMed] [Google Scholar]
- 6. Tang WK, Grace Lau C, Mok V, et al. . Insomnia and health-related quality of life in stroke. Top Stroke Rehabil 2015;22:201–7. 10.1179/1074935714Z.0000000026 [DOI] [PubMed] [Google Scholar]
- 7. Hermann DM, Bassetti CL. Sleep-disordered breathing and stroke. Curr Opin Neurol 2003;16:87–90. 10.1097/00019052-200302000-00012 [DOI] [PubMed] [Google Scholar]
- 8. Cherkassky T, Oksenberg A, Froom P, et al. . Sleep-related breathing disorders and rehabilitation outcome of stroke patients: a prospective study. Am J Phys Med Rehabil 2003;82:452–5. 10.1097/01.PHM.0000069194.61078.6E [DOI] [PubMed] [Google Scholar]
- 9. Paffenbarger RS, Lee IM, Leung R. Physical activity and personal characteristics associated with depression and suicide in American college men. Acta Psychiatr Scand Suppl 1994;377:16–22. 10.1111/j.1600-0447.1994.tb05796.x [DOI] [PubMed] [Google Scholar]
- 10. Shi YZ, Xiang YT, Yang Y, et al. . Depression after minor stroke: the association with disability and quality of life--a 1-year follow-up study. Int J Geriatr Psychiatry 2016;31:421–7. 10.1002/gps.4353 [DOI] [PubMed] [Google Scholar]
- 11. Chen HC, Su TP, Chou P. A nine-year follow-up study of sleep patterns and mortality in community-dwelling older adults in Taiwan. Sleep 2013;36:1187–98. 10.5665/sleep.2884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lekoubou A, Nkoke C, Dzudie A, et al. . Recurrent Stroke and Early Mortality in an Urban Medical Unit in Cameroon. J Stroke Cerebrovasc Dis 2017;26:1689–94. 10.1016/j.jstrokecerebrovasdis.2017.03.031 [DOI] [PubMed] [Google Scholar]
- 13. Zhang N, Wang CX, Wang AX, et al. . Time course of depression and one-year prognosis of patients with stroke in mainland China. CNS Neurosci Ther 2012;18:475–81. 10.1111/j.1755-5949.2012.00312.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kunitz SC, Gross CR, Heyman A, et al. . The pilot Stroke Data Bank: definition, design, and data. Stroke 1984;15:740–6. 10.1161/01.STR.15.4.740 [DOI] [PubMed] [Google Scholar]
- 15. Synhaeve NE, van Alebeek ME, Arntz RM, et al. . Kidney Dysfunction Increases Mortality and Incident Events after Young Stroke: The FUTURE Study. Cerebrovasc Dis 2016;42:224–31. 10.1159/000444683 [DOI] [PubMed] [Google Scholar]
- 16. Stranges S, Dorn JM, Shipley MJ, et al. . Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. Am J Epidemiol 2008;168:1353–64. 10.1093/aje/kwn337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM). 4th edn Virginia, USA: American Psychiatric Association, 1994. [Google Scholar]
- 18. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:56–62. 10.1136/jnnp.23.1.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zheng YP, Zhao JP, Phillips M, et al. . Validity and reliability of the Chinese Hamilton Depression Rating Scale. Br J Psychiatry 1988;152:660–4. 10.1192/bjp.152.5.660 [DOI] [PubMed] [Google Scholar]
- 20. Chen YK, Lu JY, Mok VC, et al. . Clinical and radiologic correlates of insomnia symptoms in ischemic stroke patients. Int J Geriatr Psychiatry 2011;26:451–7. 10.1002/gps.2547 [DOI] [PubMed] [Google Scholar]
- 21. von Ruesten A, Weikert C, Fietze I, et al. . Association of sleep duration with chronic diseases in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam study. PLoS One 2012;7:e30972 10.1371/journal.pone.0030972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Aarnio K, Haapaniemi E, Melkas S, et al. . Long-term mortality after first-ever and recurrent stroke in young adults. Stroke 2014;45:2670–6. 10.1161/STROKEAHA.114.005648 [DOI] [PubMed] [Google Scholar]
- 23. Wang W, Wang D, Liu H, et al. . Trend of declining stroke mortality in China: reasons and analysis. Stroke Vasc Neurol 2017;2:132–9. 10.1136/svn-2017-000098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Luo G, Mo D, Tong X, et al. . Factors Associated with 90-Day Outcomes of Patients with Acute Posterior Circulation Stroke Treated By Mechanical Thrombectomy. World Neurosurg 2018;109:e318–28. 10.1016/j.wneu.2017.09.171 [DOI] [PubMed] [Google Scholar]
- 25. Condén E, Rosenblad A. Insomnia predicts long-term all-cause mortality after acute myocardial infarction: A prospective cohort study. Int J Cardiol 2016;215:217–22. 10.1016/j.ijcard.2016.04.080 [DOI] [PubMed] [Google Scholar]
- 26. Edinger JD, Bonnet MH, Bootzin RR, et al. . Derivation of research diagnostic criteria for insomnia: report of an American Academy of Sleep Medicine Work Group. Sleep 2004;27:1567–96. 10.1093/sleep/27.8.1567 [DOI] [PubMed] [Google Scholar]
- 27. Pilcher JJ, Huffcutt AI. Effects of sleep deprivation on performance: a meta-analysis. Sleep 1996;19:318–26. 10.1093/sleep/19.4.318 [DOI] [PubMed] [Google Scholar]
- 28. de Havenon A, Bennett A, Stoddard GJ, et al. . Determinants of the impact of blood pressure variability on neurological outcome after acute ischaemic stroke. Stroke Vasc Neurol 2017;2:1–6. 10.1136/svn-2016-000057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Appleton JP, Sprigg N, Bath PM. Blood pressure management in acute stroke. Stroke Vasc Neurol 2016;1:72–82. 10.1136/svn-2016-000020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vgontzas AN, Liao D, Bixler EO, et al. . Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep 2009;32:491–7. 10.1093/sleep/32.4.491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Roehrs T, Gumenyuk V, Drake C, et al. . Physiological correlates of insomnia. Curr Top Behav Neurosci 2014;21:277–90. 10.1007/7854_2014_324 [DOI] [PubMed] [Google Scholar]
- 32. Tasali E, Leproult R, Spiegel K. Reduced sleep duration or quality: relationships with insulin resistance and type 2 diabetes. Prog Cardiovasc Dis 2009;51:381–91. 10.1016/j.pcad.2008.10.002 [DOI] [PubMed] [Google Scholar]
- 33. Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. J Intern Med 2002;251:207–16. 10.1046/j.1365-2796.2002.00941.x [DOI] [PubMed] [Google Scholar]
- 34. Suzuki E, Yorifuji T, Ueshima K, et al. . Sleep duration, sleep quality and cardiovascular disease mortality among the elderly: a population-based cohort study. Prev Med 2009;49:135–41. 10.1016/j.ypmed.2009.06.016 [DOI] [PubMed] [Google Scholar]
- 35. Choi JW, Song JS, Lee YJ, et al. . Increased Mortality in Relation to Insomnia and Obstructive Sleep Apnea in Korean Patients Studied with Nocturnal Polysomnography. J Clin Sleep Med 2017;13:49–56. 10.5664/jcsm.6386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kakizaki M, Kuriyama S, Nakaya N, et al. . Long sleep duration and cause-specific mortality according to physical function and self-rated health: the Ohsaki Cohort Study. J Sleep Res 2013;22:209–16. 10.1111/j.1365-2869.2012.01053.x [DOI] [PubMed] [Google Scholar]