Abstract
Background:
Unrelieved pain is associated with adverse outcomes among older adults. While previous studies found a high prevalence of pain among community dwelling older adults, the occurrence of pain among older patients in the hospital is not well understood. The objective of this study was to investigate the prevalence, characteristics and management of pain in older hospitalized medical patients.
Methods:
To determine the prevalence of moderate to severe pain (i.e., pain of ≥ 4 on the 0 to 10 Numeric Pain Rating Scale), medical record aggregate review was conducted on patients ≥ 65 years of age admitted to the medicine service at a tertiary hospital between 11/28/2014 – 5/28/2015. Demographic characteristics, comorbidity burden, pain characteristics, and analgesics during the index hospitalization were assessed on moderate to severe pain patients only.
Results:
Of 1267 patients admitted to the medicine service, 248 (20%) had moderate to severe pain on admission. Mean age was 75 ± 8 years, 57% were female, and 50% were white. During hospitalization, most patients received opioids (80%) and acetaminophen (74%), and few received nonsteroidal anti-inflammatory drugs (9%). Compared to those without a history of chronic pain, patients with chronic pain experienced a lower reduction in pain intensity score from admission to discharge (mean change score 3.7 vs. 4.9, p=0.002) and were more likely to receive opioids, adjuvant analgesics, and other analgesics (all p<0.05).
Conclusions:
Moderate to severe pain is present in one of five older adults admitted to the general medicine service. Further research about optimal pain management among hospitalized older adults, particularly those with chronic pain, is necessary to improve care in this population.
Keywords: pain, pain management, older adult, hospital, opioids
Introduction
Pain is a common and disabling condition in the older population. Approximately 24–72% of community-dwelling older adults and 60–80% of long-term care facility older residents report or have been observed to have pain.1–4 Unrelieved pain is associated with adverse outcomes among older adults, including decreased physical functioning, sleep disturbance, and falls.5–7 However, across different care settings, studies found that pain is often inadequately treated among older adults.8–10 Pain management for older adults is complicated by multimorbidity, as 65% of older adults have ≥2 chronic conditions and 24% have ≥4 chronic conditions.11 Furthermore, high rates of polypharmacy among older adults increase the risk of drug-drug interactions and adverse effects.12, 13
Despite comprising 13% of the United States population in 2008, patients ≥65 years of age represented over 40% of all hospitalized adults.14 However, limited research exists about the occurrence and management of pain among older adults in the hospital setting. Studies to date have focused on overall admission pain prevalence, pain in the emergency department and hip fracture pain.15–18 The prevalence and management of pain in older patients on general medicine services remains unknown.
Therefore, the objectives of this study were to (1) determine the prevalence of pain in older adults admitted to a medicine service, (2) examine the pain characteristics and management of moderate to severe pain in these patients, and (3) investigate differences in pain and pain management among different subgroups of patients.
Methods
Study Population
This retrospective cohort study included patients aged ≥65 years of age who were admitted with moderate to severe pain to the medicine service of a tertiary medical center in San Francisco between 11/28/2014 and 05/28/2015. Moderate to severe pain was defined as the first documented pain intensity score within 24 hours of admission as assessed by the 0 to 10 Numerical Pain Rating Scale (NPRS) of ≥4 or the Checklist of Nonverbal Pain Indicators (CNPI) of ≥ 1.19, 20 The NPRS is a reliable and commonly used tool to assess pain in older adults, while the CNPI is frequently used to assess pain in cognitively impaired elders.21 For patients with multiple admissions during the 6 months of enrollment, the most recent admission was considered. Ethics approval was obtained from the local institutional review board.
Study Measures
Structured medical record reviews were conducted by trained clinical and research personnel. Demographic data such as age at hospitalization, sex, race, ethnicity, marital status, insurance type, and language preference were abstracted electronically. Abstracted index admission information included length of hospital stay and admission and discharge locations. Collected pain characteristics included pain sites and relevant pain related diagnoses from the electronic health record problem list (e.g., chronic pain, dementia and depression).
On admission, the first documented NPRS or CNPI score was recorded. At discharge, the last documented NPRS, CNPI, or the Verbal Descriptor Scale (VDS) score was recorded. A subset of patients completed pain assessments at discharge using VDS, which is a valid and reliable tool that elicits a verbal description of pain intensity (i.e., none, mild, moderate, severe, or very severe).22 Patients who did not have documented pain scores within 24 hours of admission or within 48 hours of discharge were excluded. To harmonize the three pain scales, CNPI scores were converted to NPRS scores using the following algorithm: “1–2” → “5”, “3–4” → “8”. VDS scores were converted to equivalent NPRS scores with the following algorithm: “None” → “0”, “mild” → “2”, “moderate” → “5”, “severe” → “8”, and “very severe” → “10”.23
We recorded data about analgesics at three time points: medications prescribed before the time of hospitalization, during hospitalization, and at discharge. We categorized analgesics into four types: non-opioids (acetaminophen and nonsteroidal anti-inflammatory drug [NSAID] combined), opioids, co-analgesics (e.g., antidepressants, anticonvulsants), and “other” analgesics (e.g., lidocaine, baclofen).24 We noted non-pharmacologic methods of pain treatment (e.g. repositioning, hot or cold application, emotional support). Morphine Equivalent Daily Dose (MEDD) was calculated for opioid intake on the first and last day of admission. A high MEDD was defined as ≥50 mg based on dosing recommended by the 2016 Centers for Disease Control guidelines.25 To verify the accuracy of chart abstraction, an independent abstractor re-evaluated and adjudicated the data for 10% of the sample.
We assessed comorbidity burden using the Cumulative Illness Rating Scale for Geriatrics (CIRS-G).26,27 The CIRS-G is a validated tool in older adults and comprises 14 organ systems assigned ratings from 0–4 based on severity. Total score ranges from 0–56, with higher scores indicating greater burden of disease. While the 1991 CIRS-G manual was the main reference for score calculation,28 the 2008 CIRS-G manual29 was used to clarify ambiguous scoring scenarios. Trained clinical personnel completed the CIRS-G scoring. To check inter-rater reliability, a trained research team member scored a subset of the first 100 charts. All discrepancies were resolved with the consultation of the senior author (CSR).
Statistical Analysis
We calculated descriptive summary statistics related to pain prevalence and treatment characteristics using Chi-square test for categorical variables and Student’s t-test for continuous variables. Pain prevalence, characteristics, and management were examined among different subgroups of patients. These variables were determined a priori based on previously identified factors associated with pain and included age, sex, race, history of chronic pain, depression, and dementia.2, 17, 30 We examined outpatient treatment characteristics before hospitalization and at discharge using McNemar’s test or Wilcoxon’s rank sum test and paired t-test as appropriate. To adjust for significant factors based on previous research, multivariate logistic regression analysis was used to determine variables independently associated with a history of chronic pain.31–33 All analyses were conducted using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
Results
Patient Sample
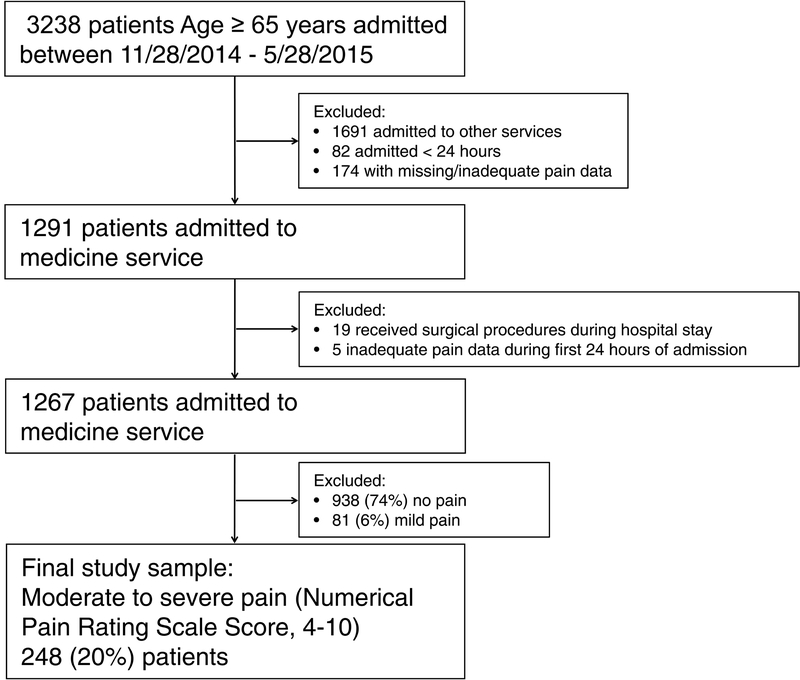
Of the 1267 patients admitted to the medicine service for non-elective procedures, 938 (74.0%) had no pain, 81 (6.4%) had mild pain, and 248 (19.6%) had moderate to severe pain. The current analysis is restricted to the 248 patients whose admission records reported moderate to severe pain (Figure 1). The mean age of moderate to severe pain group was 75.0±8.3 years, 56.5% were female, 50.4% were White and 89.5% were non-Hispanic. Most patients (71.4%) reported English as their primary language, 82.7% had Medicare insurance coverage, and 45.2% had Medicaid coverage. The mean length of hospitalization was 5.7±6.4 days and the mean CIRS-G total score was 17.3±5.6 (Table 1).
Figure 1:
Flow chart of study participants
Table 1.
Demographic and Clinical Characteristics of Older Adults Admitted to Medicine Service with Moderate to Severe Pain, Overall and According to Age
| Characteristic | Overall, N=248 | < 80, n=179 | ≥ 80, n=69 | P-Value |
|---|---|---|---|---|
| Age, mean±SD | 75.0±8.3 | 70.7±4.4 | 86.2±4.9 | <.001 |
| Female, n (%) | 140 (56.5) | 102 (57.0) | 38 (55.1) | .79 |
| White, n (%) | 125 (50.4) | 100 (55.9) | 25 (36.2) | .01 |
| Married, n (%) | 110 (44.4) | 79 (44.1) | 31 (44.9) | .92 |
| Preferred language English, n (%) | 177 (71.4) | 137 (76.5) | 40 (58.0) | .004 |
| Admission source community, n (%) | 224 (90.3) | 165 (92.2) | 59 (85.5) | .11 |
| Discharge location community, n (%) | 148 (59.7) | 115 (64.2) | 33 (47.8) | .02 |
| Hospital length of stay, mean±SD | 5.7±6.4 | 5.9±7.1 | 5.2±4.3 | .37 |
| Comorbid conditions, n (%) | ||||
| Anxiety | 56 (22.6) | 47 (26.3) | 9 (13.0) | .03 |
| Cancer | 91 (36.7) | 74 (41.3) | 17 (24.6) | .01 |
| Cerebrovascular disease | 38 (15.3) | 22 (12.3) | 16 (23.2) | .03 |
| Congestive heart failure | 55 (22.2) | 30 (16.8) | 25 (36.2) | <.001 |
| Dementia | 25 (10.1) | 14 (7.8) | 11 (15.9) | .06 |
| Depression | 63 (25.4) | 50 (27.9) | 13 (18.8) | .14 |
| Liver disease | 26 (10.5) | 23 (12.8) | 3 (4.3) | .05 |
| History of falls, n (%) | 59 (23.8) | 33 (18.4) | 26 (37.7) | .001 |
| Charlson Comorbidity Index, mean±SD | 3.1±2.3 | 3.2±2.4 | 2.6±2.1 | .06 |
| Cumulative Illness Rating Scale for Geriatrics score, mean±SD | 17.3±5.6 | 16.9±5.6 | 18.2±5.5 | .10 |
| Body mass index, kg/m2, mean±SD1 | 26.1±7.0 | 26.8±7.4 | 24.3±5.2 | .005 |
| Creatinine clearance on admission, mean±SD1 | 60.4±34.4 | 67.6±36.2 | 41.4±19.0 | <.001 |
| Admission pain score | ||||
| Mean±SD (range) | 6.3±1.8 (4–10) | 6.4±1.9 (4–10) | 6.2±1.7 (4–10) | .45 |
| Median (IQR) | 6 (5–8) | 6 (5–8) | 6 (5–8) | .45 |
| Discharge pain score | ||||
| Mean±SD (range) | 1.9±2.7 (0–10) | 2.2±2.7 (0–10) | 1.3±2.4 (0–10) | .02 |
| Median (IQR) | 0 (0–4) | 0 (0–4) | 0 (0–2) | .02 |
| History of chronic pain, n (%) | 99 (39.9) | 73 (40.8) | 26 (37.7) | .66 |
| Sites of pain on admission, n (%) | ||||
| Abdomen | 58 (23.4) | 47 (26.3) | 11 (15.9) | .09 |
| Chest | 40 (16.1) | 32 (17.9) | 8 (11.6) | .23 |
| Back, knee, hip, shoulder | 66 (26.6) | 45 (25.1) | 21 (30.4) | .40 |
| Arm, hand, wrist, leg, foot | 54 (21.8) | 40 (22.3) | 14 (20.3) | .73 |
| Generalized | 17 (6.9) | 15 (8.4) | 2 (2.9) | .13 |
1Data missing as follows: body mass index (n=16), creatinine clearance at admission (n=14).
SD=standard deviation; IQR=interquartile range.
Pain Characteristics and Management
At the time of admission, the mean NPRS score was 6.3±1.8; 55.2% reported moderate pain (NPRS: 4–6) and 44.8% reported severe pain (NPRS: 7–10). A total of 39.9% had a documented history of chronic pain. The most common sites of pain upon admission were back/knee/hip/shoulder (26.6%), abdomen (23.4%), and arm/hand/wrist/leg/foot (21.8%) (Table 1). A significant reduction in mean NPRS score occurred from admission to discharge (4.4±2.9, p<0.001).
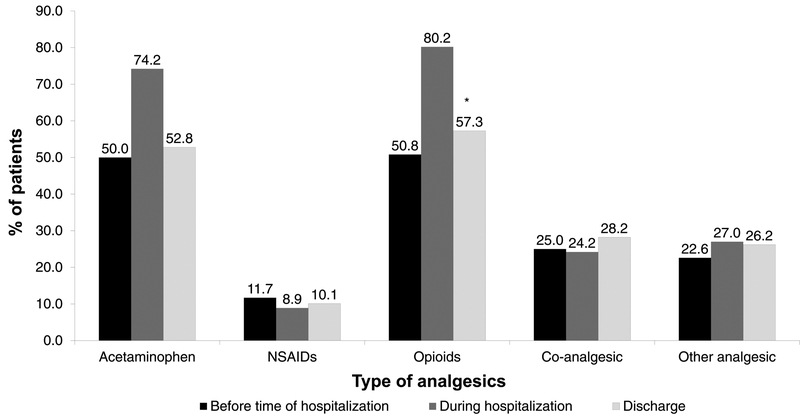
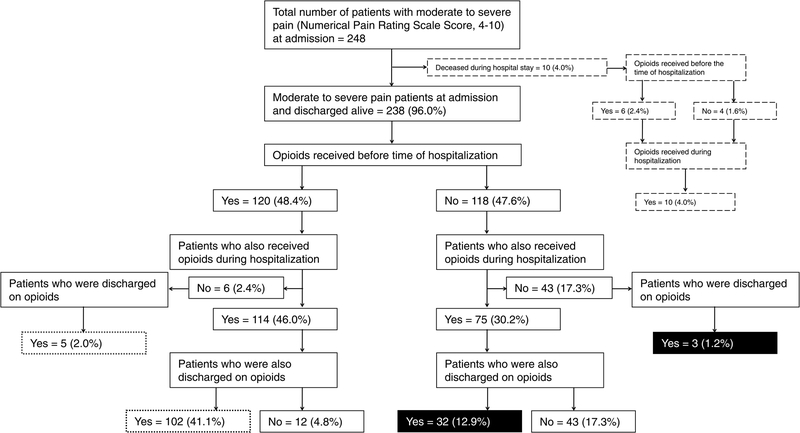
During hospitalization, most patients received opioids (80.2%) and acetaminophen (74.2%, Figure 2); 60.5% received both acetaminophen and opioids. Few patients (8.9%) received NSAIDs. Intravenous patient-controlled analgesia was prescribed for 3.6% of patients. Approximately half (49.6%) received non-pharmacologic pain interventions. Of those prescribed opioids during admission, 23.6% received a high MEDD (≥50 mg). Overall, significantly more patients were prescribed opioids at discharge than before hospitalization (57.3% vs. 50.8%, p=0.04, Figures 2, 3). In addition, 14.1% patients received new opioid prescriptions at discharge and 43.1% patients received opioid prescriptions both before hospitalization and at discharge (Figure 3). No differences were observed in other outpatient analgesic prescriptions from before hospitalization to discharge (Figure 2). Patients who were prescribed opioids before admission had longer hospital stays compared to those who did not (mean 6.8 vs. 4.6 days, p=0.005).
Figure 2:
Types of analgesics prescribed before the time of hospitalization, during hospitalization, and at discharge. NSAID = Nonsteroidal anti-inflammatory drug. Co-analgesics = antidepressants, anticonvulsants, and antiarrhythmic. *p = 0.04. P-value represents comparison between frequency of opioid analgesics prescribed before the time of hospitalization and at discharge.
Figure 3:
Flow chart of opioid prescription before the time of hospitalization, during hospitalization, and at discharge. Percentages are calculated based on total study sample (N=248).  Received new prescription at discharge, inception cohort,
Received new prescription at discharge, inception cohort,  Received prescription before the time of hospitalization and at the discharge, prevalent cohort,
Received prescription before the time of hospitalization and at the discharge, prevalent cohort,  Deceased during hospital stay.
Deceased during hospital stay.
Association of Patient Characteristics with Pain and Pain Management
Age
Patients aged 65–79 years old reported higher pain scores on discharge (2.2 ± 2.7 vs. 1.3 ± 2.4, p=0.024 and NPRS ≥1, 49.2% vs. 31.9%, p=0.014) compared to those ≥80 years. No differences were found in pharmacologic or non-pharmacologic pain management by age (all p>0.05).
Gender
No differences were observed in admission and discharge pain scores by gender (all p>0.25). Compared to males, females were more likely to be prescribed non-opioids before hospitalization, during hospitalization, and at discharge (all p<0.05). Females were also more likely to be prescribed other analgesics during hospitalization and at discharge (all p<0.05). There was no difference in non-pharmacologic pain management by gender (p=0.15).
Race
Admission and discharge pain scores between white and non-white patients were not significantly different (all p>0.25). However, white patients were more likely to be prescribed opioids before and during hospitalization (all p<0.05). White patients were less likely to be prescribed acetaminophen at discharge compared to non-white patients (p=0.022). No differences were observed in non-pharmacologic interventions by race (p=0.80).
Chronic Pain
Patients with a history of chronic pain were more likely to live alone (63.6% vs. 43.6%, p=0.002), have a history of depression (33.3% vs. 20.1%, p=0.019), and a history of sleep apnea (18.2% vs. 8.1%, p=0.017). In an a priori logistic regression model, depression was the only factor associated with a history of chronic pain (odds ratio, 1.94; 95% confidence interval, 1.05–3.59; p=0.035) after adjusting for age, sex and body mass index.
No differences were found between admission pain scores for patients with and without a history of chronic pain (p=0.83). However, at discharge, patients with chronic pain reported a lower numeric reduction in pain compared to patients without chronic pain (mean change score 3.7±2.9 vs. 4.9±2.8, p=0.002). Across the inpatient hospitalization, before hospitalization, and discharge settings, patients with a history of chronic pain were significantly more likely to receive opioids, co-analgesics, and other analgesics (all p<0.05). While no differences were found in non-pharmacologic interventions (50% in each group) and non-opioids prescriptions during hospitalization, patients with chronic pain were more likely to receive non-opioids before hospitalization and at discharge (all p<0.05, Table 2). A total of 38.9% of patients without chronic pain received opioid prescriptions prior to admission, of which 51.7% had a history of a cancer diagnosis.
Table 2.
Analgesics Prescribed to Participants with and Without a History of Chronic Pain
| Drug Category | No History of Chronic Pain (n=149) | History of Chronic Pain (n=99) | ||||
|---|---|---|---|---|---|---|
| Before Hospitalization | During Hospitalization | At Discharge | Before Hospitalization | During Hospitalization | At Discharge | |
| Nonopioid | 69 (46.3)1 | 110 (73.8) | 77 (51.7)2 | 67 (67.7)1 | 78 (78.8) | 65 (65.7)2 |
| Acetaminophen | 64 (43.0)2 | 108 (72.5) | 70 (47.0)2 | 60 (60.6)2 | 76 (76.8) | 61 (61.6)2 |
| Nonsteroidal antiinflammatory drug | 13 (8.7) | 15 (10.1) | 13 (8.7) | 16 (16.2) | 7 (7.1) | 12 (12.1) |
| Opioid | 58 (38.9)1 | 112 (75.2)2 | 72 (48.3)1 | 68 (68.7)1 | 87 (87.9)2 | 70 (70.7)1 |
| Co-analgesic3 | 24 (16.1)1 | 23 (15.4)1 | 28 (18.8)1 | 38 (38.4)1 | 37 (37.4)1 | 42 (42.4)1 |
| Other analgesic | 24 (16.1)2 | 26 (17.4)1 | 26 (17.4)1 | 32 (32.3)2 | 41 (41.4)1 | 39 (39.4)1 |
P-values represent comparison of analgesic prescription before the time of hospitalization, during hospitalization, and at discharge among patients with and without a history of chronic pain.
P <1.001, 2.05
3Antidepressant, anticonvulsant, antiarrhythmic.
Dementia
In this sample, 10.1% of patients had a documented history of dementia. Patients with dementia were more likely to be older (79.5±10.8 vs. 74.5±7.8 years, p=0.034) and have a higher CIRS-G score (19.8±5.7 vs. 17.0±5.5, p=0.016). Compared to patients without dementia, those with dementia had similar pain scores on admission (p=0.45), but reported lower pain scores on discharge (0.5±1.4 vs. 2.1±2.7, p<0.001) and achieved higher reduction in pain from admission to discharge (mean change score 5.6±2.2 vs. 4.3±3.0, p=0.035). Patients with dementia were less likely to be prescribed opioids prior to hospitalization (32.0% vs. 52.9%, p=0.047) and during admission (64.0% vs. 82.1%, p=0.032). Non-pharmacologic interventions during hospitalization and prescription of non-opioids, co-analgesics, and other analgesics before hospitalization, during hospitalization and at discharge did not differ between patients with and without dementia.
Depression
A total of 63 (25.4%) patients had a documented history of depression. No differences were found in pain scores at admission (p=0.45) or numeric reduction of pain from admission to discharge (p=0.23) between patients with and without depression. Patients with depression were more likely to receive opioid prescriptions prior to admission (63.5% vs. 46.5%, p=0.02) and during hospitalization (93.7% vs. 75.7%, p=0.002), but not at discharge (65.1% vs. 54.6%, p=0.15). Patients with depression were more likely to receive co-analgesics (34.9% vs. 21.6%, p=0.035) before hospitalization and more likely to be discharged with other analgesics (39.7% vs. 21.6%, p=0.005). There were no differences in non-pharmacologic interventions among patients with and without depression (p=0.42).
Because CNPI scores were converted to NPRS scores, we conducted a sensitivity analysis where patients with CNPI scores on admission (8.5%) were excluded. The overall results were essentially unchanged. The magnitude of the effect remained similar; however, age group differences in discharge pain scores and CIRS-G score differences by dementia group were no longer statistically significant. VDS scores at discharge (13.7% of sample) were converted to equivalent NPRS scores.
Discussion
This study expands our understanding of pain characteristics and current pain management practices in older adults admitted to a medicine service. We found that one in five older medical patients reported moderate to severe pain. The majority of these patients received opioid therapy for pain management. Finally, while patients with chronic pain commonly reported pain in the hospital, their pain was often not as responsive to multiple pharmacologic agents.
Our study offers a unique focus on the pain management of moderate to severe pain among older medical patients. Other samples of hospitalized patients have been either smaller, investigated specific analgesics (i.e., opioids), or included more heterogeneous groups (e.g., mixed age groups or combined medical and surgical patients).34–37 Although the prevalence identified in our study (20%) is lower than estimates of pain among community dwelling adults (24–72%),2–4 this difference is likely because we specifically focused on moderate to severe pain, whereas other studies reported any level of pain. If patients with mild pain were included, the total prevalence would be 26%, similar to previous estimates. In addition, because pain was identified through chart abstraction, pain prevalence may be underestimated relative to self-report.
The most common analgesics in our sample were acetaminophen and opioids, whereas NSAIDs were rarely used. Opioid use has grown substantially in the general population, including among older adults.38 One study showed that between 1999–2010, outpatient opioid prescriptions among older adults were almost doubled from 4 to 9%,38 and another study reported a 2% annual increase in opioid prescriptions for older patients without cancer between 2004 and 2013.39 In our study of hospitalized patients, 51% received opioids prior to admission, and their use increased to 80% during the hospital stay, which was higher than a recent study of opioid prescription in the emergency department (35%).40 Our study also reported a higher use of opioids at discharge compared to admission. Among 536,767 opioid-naïve patients who filled an opioid prescription in Oregon, 5% continued with long-term use.41, 42 While not evaluated in our study, it is possible that increased prescription of opioids in the hospital may contribute to persistent use in these older adults.42
Almost one-third of patients in our study received high doses of opioids (MEDD ≥50 mg) during admission. While often needed to adequately control pain, higher doses of opioids are associated with more adverse outcomes. The 2016 Centers for Disease Control guidelines and other national and state-based initiatives to curb opioid use have highlighted concerns related to higher doses of opioids and have led to an overall plateauing of opioid use nationally.25, 43 How these new initiatives to restrict opioid use affect older adults’ pain and pain management remains to be determined.
Opioid therapy is one of the most frequently implicated medications in adverse drug reactions in the hospital.44 A recent study showed that hospitalized older adults who received opioids had longer hospital stays and were more likely to be readmitted.37 In our study, patients who received outpatient opioids before hospitalization experienced longer lengths of hospital stay compared to those who did not. Further research is necessary to clarify the impact of opioid use in this population and to identify non-opioid strategies for pain management in the hospital setting.
More than one-third of patients in our study had a documented history of chronic pain. Overall, these patients received more analgesics during their hospitalization and yet reported a lower reduction in pain. Chronic pain is prevalent among older adults and often challenging to manage.45 Factors that contribute to chronic pain include older age, Hispanic ethnicity, female gender, depression, anxiety, and obesity.31–33 In our study, depression was the only factor associated with chronic pain in multivariate analysis. Depression is well studied in chronic pain and thought to represent a dyad in which the two conditions coexist and may exacerbate each other.46 Although the American Geriatrics Society guidelines recommend utilizing non-pharmacologic methods for management of persistent pain, patients with chronic pain in our study did not receive more non-pharmacologic interventions compared to their counterparts.47 Our findings underscore the need for improved comprehensive management of older adults with chronic pain and attention to psychiatric components of the pain experience in the inpatient setting.
Our study has important implications for clinical practice. As the population ages, an increasing number of older adults will be hospitalized with moderate to severe pain. Health care providers should adopt evidence-based approaches to manage their pain. While our study indicates that opioids are the current mainstay of hospital pain management, opioids have significant risks and there are limited prospective trials examining treatment outcomes among older adults. Furthermore, the impact of opioid administration in patients with chronic pain in the hospital is unknown. Thus, health care providers should exert caution when prescribing opioids to older hospitalized patients.
Several limitations warrant consideration. Our study findings may be limited in generalizability as the sample is from a single medical center with a higher proportion of non-white patients compared to the general population. Data were abstracted from medical records, which may not reflect actual pain management practices and may underestimate pain prevalence due to missing or incomplete pain documentation. Furthermore, reliability of pain assessments may be limited among patients with cognitive impairment.48, 49 There is currently no validated conversion of CNPI to NPRS scores; however, our sensitivity analysis indicates that overall results were essentially unchanged when CNPI scores were excluded. Dosing information for other analgesics were not collected except for opioids. Due to the heterogeneity of admission diagnoses and the lack of clarity regarding the rationale for pain management decisions both in inpatient and outpatient settings, we could not determine with certainty the indications for analgesic prescription based on chart review. As with any retrospective study, it is difficult to determine temporal relationship among variables. Nevertheless, this study offers important new insights on pain characteristics and management among hospitalized older adults with moderate to severe pain.
Conclusions
Moderate to severe pain was present in one of five older adults admitted to the general medicine service. Opioid therapy was commonly utilized for pain management. Patients with chronic pain were often less responsive to multiple pharmacologic agents. Future research is needed to clarify factors that contribute to the pain experience of hospitalized older adults and to identify optimal pain management strategies in this population.
Impact Statement.
We certify that this work is novel or confirmatory of recent novel clinical research.
- The potential impact of this research on clinical care or health policy includes the following:
- A dearth of studies have examined pain in hospitalized older adults. The findings from this study provide new information on the prevalence of pain in hospitalized older adults, characteristics of these patients, and how their pain was managed in the inpatient setting. This information can be used to develop interventions to improve pain management in hospitalized older adults.
Acknowledgements
This study was supported by Tideswell at UCSF, which seeks to advance the care of older adults living in the community with multiple chronic conditions and functional limitations, and the Medical Student Training in Aging Research Program, sponsored by the National Institute on Aging and American Federation for Aging Research. There were no conflicts of interest.
Sponsor’s Role
The sponsors had no role in development of the study, data acquisition, data interpretation, writing, or editing of manuscript.
Footnotes
The research reported in this paper was presented as a poster at the Journal of the American Geriatrics Society 2016 Annual Scientific Meeting.
References:
- [1].Crook J, Rideout E, Browne G. The prevalence of pain complaints in a general population. Pain. 1984;18: 299–314. [DOI] [PubMed] [Google Scholar]
- [2].Patel KV, Guralnik JM, Dansie EJ, et al. Prevalence and impact of pain among older adults in the United States: findings from the 2011 National Health and Aging Trends Study. Pain. 2013;154: 2649–2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Ferrell BA, Ferrell BR, Osterweil D. Pain in the nursing home. J Am Geriatr Soc. 1990;38: 409–414. [DOI] [PubMed] [Google Scholar]
- [4].Sengstaken EA, King SA. The problems of pain and its detection among geriatric nursing home residents. J Am Geriatr Soc. 1993;41: 541–544. [DOI] [PubMed] [Google Scholar]
- [5].Weiner DK, Rudy TE, Morrow L, et al. The relationship between pain, neuropsychological performance, and physical function in community-dwelling older adults with chronic low back pain. Pain Med. 2006;7: 60–70. [DOI] [PubMed] [Google Scholar]
- [6].Foley D, Ancoli-Israel S, Britz P, et al. Sleep disturbances and chronic disease in older adults: results of the 2003 National Sleep Foundation Sleep in America Survey. J Psychosom Res. 2004;56: 497–502. [DOI] [PubMed] [Google Scholar]
- [7].Patel KV, Phelan EA, Leveille SG, et al. High prevalence of falls, fear of falling, and impaired balance in older adults with pain in the United States: findings from the 2011 National Health and Aging Trends Study. J Am Geriatr Soc. 2014;62: 1844–1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Won AB, Lapane KL, Vallow S, et al. Persistent nonmalignant pain and analgesic prescribing patterns in elderly nursing home residents. J Am Geriatr Soc. 2004;52: 867–874. [DOI] [PubMed] [Google Scholar]
- [9].Morrison RS, Magaziner J, McLaughlin MA, et al. The impact of post-operative pain on outcomes following hip fracture. Pain. 2003;103: 303–311. [DOI] [PubMed] [Google Scholar]
- [10].Herr K, Titler M. Acute pain assessment and pharmacological management practices for the older adult with a hip fracture: review of ED trends. J Emerg Nurs. 2009;35: 312–320. [DOI] [PubMed] [Google Scholar]
- [11].Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162: 2269–2276. [DOI] [PubMed] [Google Scholar]
- [12].Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5: 345–351. [DOI] [PubMed] [Google Scholar]
- [13].Routledge PA, O’Mahony MS, Woodhouse KW. Adverse drug reactions in elderly patients. Br J Clin Pharmacol. 2004;57: 121–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].HCUP Facts and Figures: Statistics on Hospital-based Care in the United States, 2008. Rockville (MD: ), 2010. [PubMed] [Google Scholar]
- [15].Hwang U, Richardson LD, Harris B, et al. The quality of emergency department pain care for older adult patients. J Am Geriatr Soc. 2010;58: 2122–2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Titler MG, Herr K, Schilling ML, et al. Acute pain treatment for older adults hospitalized with hip fracture: current nursing practices and perceived barriers. Appl Nurs Res. 2003;16: 211–227. [DOI] [PubMed] [Google Scholar]
- [17].Morrison RS, Siu AL. A comparison of pain and its treatment in advanced dementia and cognitively intact patients with hip fracture. J Pain Symptom Manage. 2000;19: 240–248. [DOI] [PubMed] [Google Scholar]
- [18].Desbiens NA, Mueller-Rizner N, Connors AF, et al. Pain in the oldest-old during hospitalization and up to one year later. HELP Investigators. Hospitalized Elderly Longitudinal Project. J Am Geriatr Soc. 1997;45: 1167–1172. [DOI] [PubMed] [Google Scholar]
- [19].Jensen MP, Karoly P, McCaffery M. Self-report scales and procedures for assessing pain in adults In: Turk DC, Melzack R, editors. Handbook of pain assessment. New York: Guilford Press; 2001. p. 15–34. [Google Scholar]
- [20].Feldt KS. The checklist of nonverbal pain indicators (CNPI). Pain Manag Nurs. 2000;1: 13–21. [DOI] [PubMed] [Google Scholar]
- [21].Hjermstad MJ, Fayers PM, Haugen DF, et al. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41: 1073–1093. [DOI] [PubMed] [Google Scholar]
- [22].Gracely RH, Dubner R. Reliability and validity of verbal descriptor scales of painfulness. Pain. 1987;29: 175–185. [DOI] [PubMed] [Google Scholar]
- [23].Edelen MO, Saliba D. Correspondence of verbal descriptor and numeric rating scales for pain intensity: an item response theory calibration. J Gerontol A Biol Sci Med Sci. 2010;65: 778–785. [DOI] [PubMed] [Google Scholar]
- [24].American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older P. Pharmacological management of persistent pain in older persons. Pain Med. 2009;10: 1062–1083. [DOI] [PubMed] [Google Scholar]
- [25].Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016. MMWR Recomm Rep. 2016;65: 1–49. [DOI] [PubMed] [Google Scholar]
- [26].de Groot V, Beckerman H, Lankhorst GJ, et al. How to measure comorbidity. a critical review of available methods. J Clin Epidemiol. 2003;56: 221–229. [DOI] [PubMed] [Google Scholar]
- [27].Miller MD, Paradis CF, Houck PR, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992;41: 237–248. [DOI] [PubMed] [Google Scholar]
- [28].Miller MD, Towers A. A Manual of Guidelines for Scoring the Cumulative Illness Rating Scale for Geriatrics (CIRS-G). Pittsburgh, PA: University of Pittsburgh, 1991. [Google Scholar]
- [29].Salvi F, Miller MD, Grilli A, et al. A manual of guidelines to score the modified cumulative illness rating scale and its validation in acute hospitalized elderly patients. J Am Geriatr Soc. 2008;56: 1926–1931. [DOI] [PubMed] [Google Scholar]
- [30].Green CR, Anderson KO, Baker TA, et al. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med. 2003;4: 277–294. [DOI] [PubMed] [Google Scholar]
- [31].McCarthy LH, Bigal ME, Katz M, et al. Chronic pain and obesity in elderly people: results from the Einstein aging study. J Am Geriatr Soc. 2009;57: 115–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Gold DT, Roberto KA. Correlates and consequences of chronic pain in older adults. Geriatr Nurs. 2000;21: 270–273. [DOI] [PubMed] [Google Scholar]
- [33].Reyes-Gibby CC, Aday LA, Todd KH, et al. Pain in aging community-dwelling adults in the United States: non-Hispanic whites, non-Hispanic blacks, and Hispanics. J Pain. 2007;8: 75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Rockett MP, Simpson G, Crossley R, et al. Characteristics of pain in hospitalized medical patients, surgical patients, and outpatients attending a pain management centre. Br J Anaesth. 2013;110: 1017–1023. [DOI] [PubMed] [Google Scholar]
- [35].Simmons SF, Schnelle JF, Saraf AA, et al. Pain and Satisfaction With Pain Management Among Older Patients During the Transition From Acute to Skilled Nursing Care. Gerontologist. 2016;56: 1138–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Lin RJ, Reid MC, Chused AE, et al. Quality Assessment of Acute Inpatient Pain Management in an Academic Health Center. Am J Hosp Palliat Care. 2016;33: 16–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Maiti S, Sinvani L, Pisano M, et al. Opiate Prescribing in Hospitalized Older Adults: Patterns and Outcomes. J Am Geriatr Soc. 2018;66: 70–75. [DOI] [PubMed] [Google Scholar]
- [38].Steinman MA, Komaiko KD, Fung KZ, et al. Use of opioids and other analgesics by older adults in the United States, 1999–2010. Pain Med. 2015;16: 319–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Barbera L, Sutradhar R, Chu A, et al. Opioid Prescribing Among Cancer and Non-cancer Patients: Time Trend Analysis in the Elderly Using Administrative Data. J Pain Symptom Manage. 2017;54: 484–492 e481. [DOI] [PubMed] [Google Scholar]
- [40].Platts-Mills TF, Esserman DA, Brown DL, et al. Older US emergency department patients are less likely to receive pain medication than younger patients: results from a national survey. Ann Emerg Med. 2012;60: 199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Deyo RA, Hallvik SE, Hildebran C, et al. Association Between Initial Opioid Prescribing Patterns and Subsequent Long-Term Use Among Opioid-Naive Patients: A Statewide Retrospective Cohort Study. J Gen Intern Med. 2017;32: 21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Calcaterra SL, Yamashita TE, Min SJ, et al. Opioid Prescribing at Hospital Discharge Contributes to Chronic Opioid Use. J Gen Intern Med. 2016;31: 478–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Dart RC, Surratt HL, Cicero TJ, et al. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372: 241–248. [DOI] [PubMed] [Google Scholar]
- [44].Davies EC, Green CF, Taylor S, et al. Adverse drug reactions in hospital in-patients: a prospective analysis of 3695 patient-episodes. PLoS One. 2009;4: e4439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Herr K Chronic pain: challenges and assessment strategies. J Gerontol Nurs. 2002;28: 20–27; quiz 54–25. [DOI] [PubMed] [Google Scholar]
- [46].Lindsay PG, Wyckoff M. The depression-pain syndrome and its response to antidepressants. Psychosomatics. 1981;22: 571–573, 576–577. [DOI] [PubMed] [Google Scholar]
- [47].AGS Panel on Persistent Pain in Older Persons. The management of persistent pain in older persons. J Am Geriatr Soc. 2002;50: S205–224. [DOI] [PubMed] [Google Scholar]
- [48].Taylor LJ, Harris J, Epps CD, et al. Psychometric evaluation of selected pain intensity scales for use with cognitively impaired and cognitively intact older adults. Rehabil Nurs. 2005;30: 55–61. [DOI] [PubMed] [Google Scholar]
- [49].Ersek M, Herr K, Neradilek MB, et al. Comparing the psychometric properties of the Checklist of Nonverbal Pain Behaviors (CNPI) and the Pain Assessment in Advanced Dementia (PAIN-AD) instruments. Pain Med. 2010;11: 395–404. [DOI] [PMC free article] [PubMed] [Google Scholar]