Abstract
Background:
US lung transplant registry data demonstrate differences in adult waitlist mortality by race/ethnicity. Whether these differences persist after risk-adjustment or occur secondary to disparities in disease severity at the time of listing is unknown.
Methods:
Adult lung transplant waitlist candidates between May 4, 2005 and March 5, 2015 were identified and compared by non-Hispanic white (NHW), non-Hispanic black (NHB), Hispanic, and Asian race/ethnicity. A competing risk proportional hazards model was used to assess the association of race/ethnicity with the unadjusted and adjusted risk of waitlist death or removal for too sick, transplant, or removal for other reason. Disease illness severity at transplant listing was compared by race/ethnicity.
Results:
There were 20,684 lung transplant candidates identified (82% NHW, 9% NHB, 6% Hispanic, 2% Asian, and 1% other). Non-white candidates had higher unadjusted waitlist mortality, which was fully mitigated by adjusting for other risk factors (NHB HR 1.05, 95%CI 0.93–1.18; Hispanic HR 1.02, 95%CI 0.99–1.18; Asian HR 0.90, 95%CI 0.70–1.16). Adjusted waitlist access to transplant was lower in non-white candidates (NHB HR 0.88, 95%CI 0.83–0.94; Hispanic HR 0.87, 95%CI 0.81–0.94; Asian HR 0.83, 95%CI 0.73–0.96). NHW candidates with obstructive lung disease and pulmonary fibrosis were older with less illness severity at listing than non-white candidates.
Conclusion:
Within the current lung allocation system, there is no difference in risk-adjusted waitlist mortality by race/ethnicity however non-white waitlist candidate have lower risk-adjusted access to lung transplant. Non-white candidates are generally younger with greater disease-specific illness severity at the time of lung transplant listing.
Introduction
The US lung transplant waitlist population continues to undergo racial and ethnic diversification. From 2006 to 2014, the proportion of non-Hispanic white candidates listed for lung transplant decreased, while non-Hispanic black, Hispanic, and Asian candidates increased1,2. As the number of lung transplant candidates continues to outnumber the supply of available donor lungs, an allocation system is required to prioritize scarce lungs and ensure equitable transplant access to all waitlist candidates. The previous lung allocation system that allocated based upon accrued waitlist time resulted in waitlist disparities for black and/or Hispanic patients with chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis (IPF).3–5 These disparities were attributed, particularly in IPF, to a delay in transplant listing, which resulted in less accrued waitlist time and lower allocation prioritization.
In May 2005, introduction of the lung allocation score (LAS) changed lung allocation within the US to a score based upon medical urgency and benefit.6 By allocating on medical urgency and not on the ability to be referred earlier, this change initially resolved differences in waitlist outcomes between black and white candidates.7 However, recent US lung transplant registry reports demonstrate significant variation in unadjusted waitlist mortality by race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and Asian).1,2,8,9 Whether these racial/ethnic disparities persist after adjusting for differences in diagnosis, geography, or illness severity is unknown.1,2,8,9 Accordingly, the aim of this paper is to assess whether race/ethnicity impacts risk adjusted mortality or transplant access among waitlisted candidates under the current US lung allocation system. We assess for pre-listing disparities by evaluating differences in disease severity by race/ethnicity at the time of transplant listing. Further insight into the relationship between race/ethnicity and lung transplant waitlist outcomes is critical for upholding equitable lung transplant access, both before and after listing, to the increasingly diverse US population with advanced lung disease.
Methods
Subjects
Using Scientific Registry of Transplant Recipients (SRTR) standard analysis files, we identified all adult lung transplant candidates on the waiting list between May 4, 2005 and March 5, 2015. The SRTR data system includes data on all donor, waitlist candidates, and transplant recipients in the United States, submitted by the members of the Organ Procurement and Transplantation Network (OPTN). The Health Resources and Services Administration (HRSA), U.S. Department of Health and Human Services provides oversight to the activities of the OPTN and SRTR contractors.
Candidates under the age of 18 years, those undergoing re-transplantation, and those with missing race/ethnicity, diagnosis, or a zero or missing LAS were excluded. Race/ethnicity was classified according to transplant center reported data fields as non-Hispanic white (NHW), non-Hispanic black (NHB), Hispanic, Asian, and other, which includes Native Americans, Native Alaskans, Pacific Islanders, and those of undefined or mixed race/ethnicity. Candidate lung diagnosis was grouped into 4 categories (Group A, Group B, Group C, and Group D) according to the LAS system. Group A consisted of candidates with obstructive lung diseases, Group B of candidates with pulmonary vascular diseases, Group C of candidates with cystic fibrosis or bronchiectasis lung diseases, and Group D of candidates with restrictive lung disease or pulmonary fibrosis. The candidates home zip code was used to obtain county-level median household income from the 2013 US Census Bureau, Small Area Income and Poverty Estimates.10 For candidates with zip codes in Puerto Rico, the territory-level median income was used. The US median household income was used for candidates with missing zip codes or whose county did not report median income. This study received an exemption from the Stanford University Institutional Review Board.
Outcomes
Three waitlist outcomes were analyzed: removal for transplant, removal for death or too sick, and removal for other (including too well, refusing transplant, error, loss of contact with center, medically unsuitable, inactive program, or unspecified). Candidates removed for too sick were combined with candidates removed for death to produce a composite waitlist death outcome, as removal for too sick often closely precedes death. Candidates alive on the waitlist at the time we received the data (March 5, 2015) were right-censored. For candidates listed at multiple centers, we defined their time at risk as the time from their earliest listing until their waitlist outcome or last status update. If there was a gap between listings, time at risk counted active waitlist time and did not include a candidate’s inactive time.
Statistical Analysis
Descriptive variables were generated from existing SRTR data fields and compared by race/ethnicity. Categorical variables were displayed using counts and percentages and continuous variables were summarized using median and interquartile range (IQR, 25th and 75th percentiles). A competing risk model was fit to assess how race/ethnicity was associated with the competing waitlist outcomes of lung transplant, death/too sick, and other removal.11–13 A proportional hazards model on the cause-specific hazards was fit with hazards stratified by waitlist outcome. The following variables were a priori included in the full risk-adjusted model: race/ethnicity, gender, age, United Network for Organ Sharing (UNOS) region, diagnosis group, median county household income, blood type, height, antibody cross-match requirement, LAS at listing, transplant type (any type, only single, only bilateral), and use of extracorporeal membrane oxygenation (ECMO) or mechanical ventilation. A partial risk-adjusted model that did not account for listing illness severity or geography was performed using the following variables: race/ethnicity, age, gender, diagnosis, and transplant type. For race, age, gender, region, diagnosis group, height, crossmatch requirement, and LAS we allowed different effects of the covariates for each outcome by using transition-specific coefficients. For example, we allowed the relationship between age and the hazard of death to differ from the relationship between age and the hazard of transplant. The proportional hazards assumption was assessed by visual examination of Schoenfeld residual plots and Kaplan-Meier plots. All eligible candidates were included in the primary analysis as all model covariates were available after imputing county-level median household income as described above. In a sensitivity analysis, we additionally adjusted for insurance type in our primary model using transition-specific coefficients on insurance type. Insurance type was classified as private, public, or other. 184 candidates missing the insurance type were excluded from the sensitivity analysis.
A Kruskal-Wallis rank sum test was used to compare age, forced expiratory volume in one second (FEV1), forced vital capacity (FVC), resting oxygen requirement, six minute walk distance, pulmonary artery systolic pressure, and listing LAS by race/ethnicity within obstructive lung disease (Group A) and pulmonary fibrosis (Group D) candidates. Fisher’s exact test was used to compare mechanical ventilation use across race/ethnicity. All statistical analyses were performed with R 3.1.0.14 The competing risk models were implemented using the R package ‘mstate’, version 0.2.7.11,15,16
Results
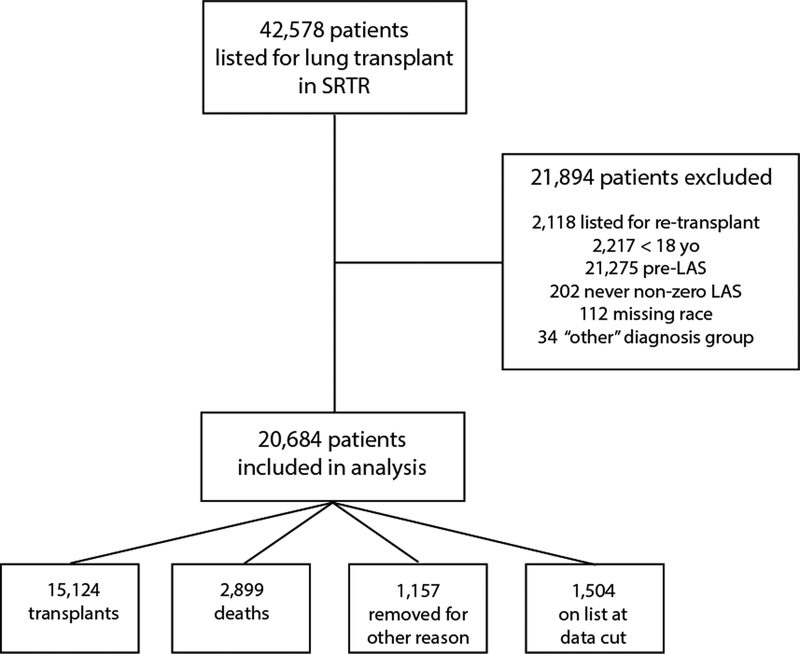
There were 20,684 lung transplant candidates identified from May 4, 2005 to March 5, 2015 who met all inclusion criteria (Figure 1). Of these candidates, 16,992 (82%) were NHW, 1,941 (9%) were NHB, 1,262 (6%) were Hispanic, 345 (2%) were Asian, and 144 (<1%) were other race/ethnicity. Candidate characteristics by race/ethnicity are shown in Table 1. Pulmonary fibrosis was the most common diagnosis across all race/ethnicities with a higher proportion seen in NHB (70%), Asian (79%), and Hispanic (75%) than in NHW (47%). Obstructive lung disease was more common in NHW (35%) than NHB (22%), Asian (11%), or Hispanic (9%) race/ethnicities. Asian and Hispanic candidates were of shorter stature and more likely to be hospitalized prior to transplant, particularly in the intensive care unit, than NHW candidates. Public insurance was more common in NHB (44%) and Hispanic (46%) candidates than in NHW (40%) or Asian (32%) candidates.
Figure 1.
Flow Diagram of Cohort
Table 1.
Candidate Characteristics by Race/Ethnicity
| White | Black | Asian | Hispanic | |
|---|---|---|---|---|
| n = 16,992 | n = 1,941 | n = 345 | n = 1,262 | |
| Age (years) | 59 (50, 64) | 53 (45, 60) | 59 (47, 65) | 56 (43, 63) |
| Male | 9688 (57) | 795 (41) | 194 (56) | 652 (52) |
| Height (cm) | 170 (163, 178) | 168 (163, 175) | 163 (157, 170) | 163 (158, 170) |
| Antibody Crossmatch Required | 925 (5) | 165 (9) | 31 (9) | 120 (10) |
| Transplant Type | ||||
| Bilateral only | 8734 (51) | 1273 (66) | 161 (47) | 696 (55) |
| Single lung only | 1736 (10) | 95 (5) | 38 (11) | 114 (9) |
| Left or Right (with or wo bilateral) | 6522 (38) | 573 (30) | 146 (42) | 452 (36) |
| Diagnosis Group | ||||
| Group A - Obstructive Lung Disease | 5926 (35) | 418 (22) | 38 (11) | 119 (9) |
| Group B - Pulmonary Hypertension | 704 (4) | 120 (6) | 32 (9) | 109 (9) |
| Group C - Cystic Fibrosis | 2341 (14) | 39 (2) | 2 (1) | 86 (7) |
| Group D - Pulmonary Fibrosis | 8021 (47) | 1364 (70) | 273 (79) | 948 (75) |
| Blood Type | ||||
| A | 7136 (42) | 491 (25) | 90 (26) | 381 (30) |
| AB | 627 (4) | 85 (4) | 30 (9) | 28 (2) |
| B | 1647 (10) | 383 (20) | 106 (31) | 109 (9) |
| O | 7582 (45) | 982 (51) | 119 (34) | 744 (59) |
| Medical Condition, Pre-Transplant | ||||
| Hospitalized, In ICU | 884 (6) | 104 (6) | 35 (11) | 110 (9) |
| Hospitalized, not in ICU | 840 (6) | 104 (6) | 24 (8) | 104 (9) |
| Not hospitalized | 13306 (89) | 1477 (88) | 258 (81) | 979 (82) |
| ECMO1 | 129 (1) | 19 (1) | 4 (1) | 7 (1) |
| Mechanical Ventilation | 471 (3) | 38 (2) | 15 (4) | 54 (4) |
| LAS at listing | 36.0 (32.9, 42.6) | 37.3 (33.8, 44.9) | 42.2 (35.9, 52.4) | 40.7 (35.1, 50.2) |
| Socioeconomic Factors | ||||
| County median income (in $1000s) | 52 (45, 61) | 52 (44, 59) | 62 (54, 76) | 54 (48, 59) |
| Non US Citizen | 141 (1) | 24 (1) | 6 (2) | 8 (1) |
| Highest Education Obtained | ||||
| Grade school | 312 (2) | 35 (2) | 2 (1) | 182 (16) |
| High school | 6261 (41) | 683 (40) | 59 (20) | 468 (42) |
| Attended college/Tech school | 4073 (27) | 496 (29) | 50 (17) | 248 (22) |
| Associate/Bachelor degree | 3067 (20) | 333 (20) | 106 (35) | 148 (13) |
| Graduate degree | 1420 (9) | 144 (9) | 85 (28) | 49 (4) |
| Primary insurance | ||||
| Private | 9923 (59) | 1056 (55) | 224 (66) | 661 (53) |
| Public | 6768 (40) | 841 (44) | 109 (32) | 571 (46) |
| Other | 156 (1) | 20 (1) | 6 (2) | 22 (2) |
ECMO, Extracorporeal Membrane Oxygenation
This table displays median (interquartile range) for continuous variables and N (%) for categorical variables.
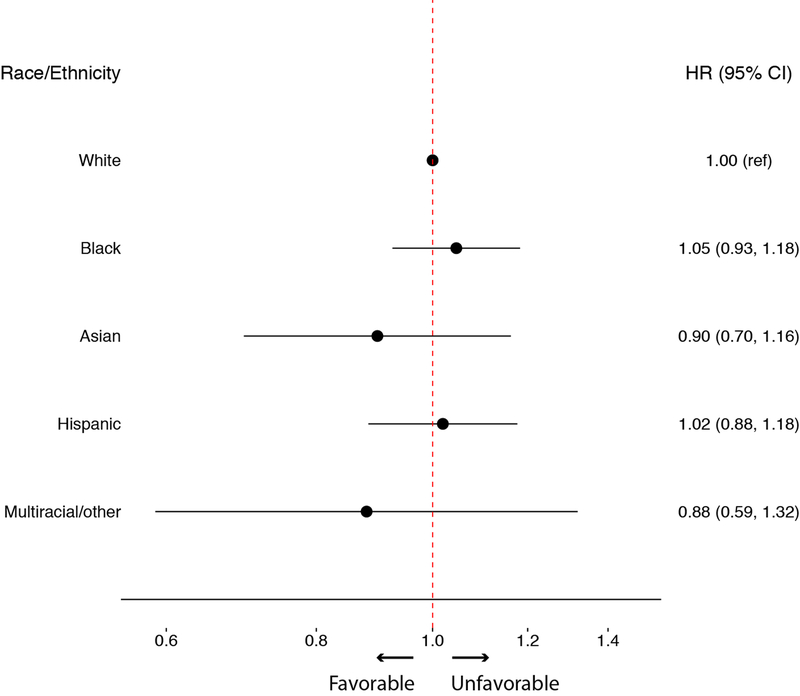
Non-white candidates had higher unadjusted waitlist mortality or removal for too sick (NHB hazard ratio [HR] 1.31, 95% confidence interval [CI] 1.17–1.47; Hispanic HR 1.61, 95%CI 1.41–1.83; Asian HR 1.54, 95%CI 1.20–1.98) compared to NHW candidates (Table 2). After partial adjustment for age, gender, diagnosis, and transplant type, there was no difference in waitlist mortality or removal for too sick in NHB (HR 1.07, 95%CI 0.94–1.20) or Asian (HR 1.20, 95%CI 0.93–1.54) candidates while the risk remained higher for Hispanic candidates (HR 1.24, 95%CI 1.08–1.41) compared to NHW candidates. After full risk adjustment, there was no difference by race/ethnicity in adjusted waitlist mortality (Figure 2).
Table 2.
Waitlist Mortality by Race/Ethnicity
| Non-Hispanic Black | Hispanic | Asian | |
|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Unadjusted Model | 1.31 (1.17–1.47) | 1.61 (1.41–1.83) | 1.54 (1.2–1.98) |
| Partially Adjusted Model** | 1.07 (0.94–1.20) | 1.24 (1.08–1.41) | 1.2 (0.93–1.54) |
| Fully Adjusted Model*** | 1.05 (0.93–1.18) | 1.02 (0.88–1.18) | 0.90 (0.70–1.16) |
Reference Group for all models is Non-Hispanic White
Partially adjusted model includes variables for race/ethnicity, age, gender, diagnosis group, and transplant type
Fully adjusted model includes variables for race/ethnicity, age, gender, diagnosis group, transplant type, United Network for Organ Sharing region, blood type, height, county median household income, antibody crossmatch requirement, mechanical ventilation or extracorporeal membrane oxygenation use, and lung allocation score at listing
Figure 2. Hazard Ratio of Waitlist Death by Race and Ethnicity.
The risk adjusted hazard ratio and 95% confidence interval of death by race/ethnicity for waitlisted lung transplant candidates.
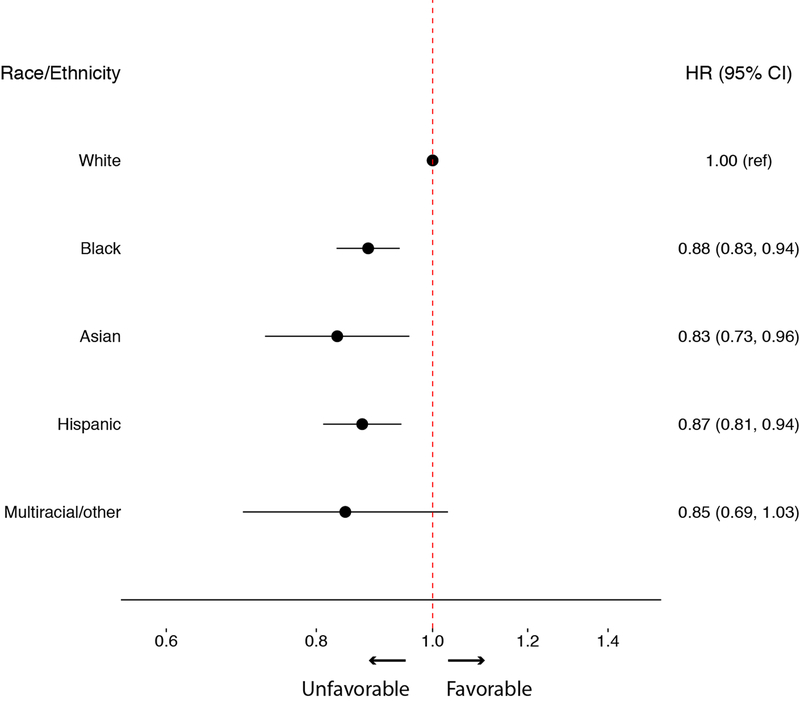
Adjusted waitlist access to transplant was lower in NHB (HR 0.88, 95%CI 0.83–0.94), Hispanic (HR 0.87, 95%CI 0.81–0.94), and Asian (HR 0.83, 95%CI 0.73–0.96) candidates compared to NHW candidates (Figure 3). NHB candidates were more likely to be removed for other reasons (HR 1.30, 95%CI 1.08–1.56) with no significant difference seen for other removal in Hispanic (HR 0.98, 95%CI 0.76–1.26) or Asian (HR 1.42, 95%CI 0.98–2.06) candidates compared to NHW candidates. A sensitivity analysis adjusting for candidate insurance type resulted in no significant change in these findings.
Figure 3. Hazard Ratio of Lung Transplant by Race and Ethnicity.
The risk adjusted hazard ratio and 95% confidence interval of lung transplant by race/ethnicity for waitlisted lung transplant candidates.
Demographic and clinical differences in obstructive lung disease (Group A) candidates at the time of lung transplant listing by race/ethnicity are shown in Table 3. NHW candidates were older (median 60 years) than NHB (58 years), Asian (55 years) and Hispanic (55 years) candidates (p<0.001). Twenty percent of NHW candidates with obstructive lung disease were ≥65 compared to 15.3% of Black candidates, 13.2% of Asian candidates, and 12.6% of Hispanic candidates. Among obstructive lung disease candidates, there was no significant difference in listing FEV1 (p=0.060) or resting oxygen requirement (p=0.063) by race/ethnicity. There were significant (p<0.001) differences in pulmonary artery pressure; non-white obstructive lung disease candidates had higher median pulmonary artery pressures (40 mmHg) than NHW candidates (35 mmHg). Functional capacity and mechanical ventilation differed by race/ethnicity (p=0.005 and p=0.021, respectively). NHB and Hispanic obstructive lung disease candidates had lower functional capacity as measured by six minute walk testing and were more likely to be mechanically ventilated at the time of listing than NHW or Asian candidates. NHW obstructive lung disease candidates had a lower listing LAS (32.7) than NHB (33.4), Asian (33.6), or Hispanic (33.9) candidates (p<0.001).
Table 3.
Obstructive Lung Disease (Group A) Illness Severity at Transplant Listing by Race/Ethnicity
| White | Black | Asian | Hispanic | p value | |
|---|---|---|---|---|---|
| n = 5926 | n = 418 | n = 38 | n = 119 | ||
| Age (years) | 59.9 (54.8, 64.1) | 58.4 (54.0, 62.5) | 55.0 (43.0, 61.2) | 55.3 (42.2 62.3) | < 0.001 |
| Forced Expiratory Volume (% predicted) | 20 (16, 25) | 20 (16, 26) | 23.5 (19, 30.3) | 21 (18, 26) | 0.060 |
| Resting Oxygen (liters per minute) | 3 (2, 4) | 3 (2, 4) | 2 (2, 4) | 3 (2, 4) | 0.063 |
| Six Minute Walk Distance (feet) | 780 (500, 1003.8) | 717.5 (420.8, 903.8) | 823.5 (442.8, 1093) | 762 (405.5, 948) | 0.005 |
| Pulmonary Artery Systolic Pressure (mmHg) | 35 (31, 42) | 40 (34, 48) | 40 (32, 46.3) | 40 (33, 47) | < 0.001 |
| Mechanical Ventilation (%) | 40 (0.7%) | 4 (1.0%) | 0 (0.0%) | 4 (3.4%) | 0.021 |
| Lung Allocation Score, at listing | 32.7 (31.7, 34.1) | 33.4 (32.2, 35.2) | 33.6 (32.7, 35.4) | 33.9 (32.1, 35.6) | < 0.001 |
This table displays median (interquartile range) for continuous variables and N (%) for categorical variables.
Demographic and illness severity measurements in pulmonary fibrosis (Group D) candidates at lung transplant listing by race/ethnicity are shown in Table 4. Age differed by race/ethnicity (p<0.001). NHW pulmonary fibrosis candidates were older (median 61 years) than black (52 years), Asian (60 years), and Hispanic (58 years) candidates. A higher proportion of NHW candidates with pulmonary fibrosis were ≥65 (30.8%) compared to 6.4% of Black candidates, 32.2% of Asian candidates, and 21.6% of Hispanic candidates. Similarly, 8.5% of NHW pulmonary fibrosis candidates were ≥70 compared to 1.0% of Black candidates, 8.4% of Asian candidates, and 4.0% of Hispanic candidates. Forced vital capacity (FVC) in pulmonary fibrosis candidates differed by race/ethnicity (p<0.001). FVC was higher in NHW (47% predicted) than NHB (43% predicted), Asian (40% predicted), and Hispanic (40% predicted) candidates. Functional capacity by six-minute walk test differed by race/ethnicity (p<0.001). Median distance walked was greater in NHW candidates (835 feet) than NHB (720 feet), Asian (690 feet), and Hispanic (650 feet) candidates. Mechanical ventilation use varied across race/ethnicity (p=0.028), with a higher proportion of Asian (4.8%) and Hispanic (4.5%) candidates compared to NHW (3.4%) and NHB (2.4%) candidates on mechanical ventilation at time of listing. Listing LAS was higher in Asian (43.9) and Hispanic (43.3) candidates than NHW (41.4) or NHB (39.8) candidates (p<0.001). A subgroup analysis of pulmonary fibrosis (Group D) candidates with a coded diagnosis of IPF revealed similar findings as shown in Table 5. NHW IPF candidates were older (62.4 years) than NHB (54.3 years) and Hispanic (59.8 years) candidates. NHW candidates also had higher FVC, greater functional capacity as measured in six-minute walk distance, and lower LAS than non-white candidates (Table 5).
Table 4.
Pulmonary Fibrosis (Group D) Illness Severity at Transplant Listing by Race/Ethnicity
| White | Black | Asian | Hispanic | p value | |
|---|---|---|---|---|---|
| n = 8021 | n =1364 | n = 273 | n = 948 | ||
| Age (years) | 61.4 (55.6, 65.9) | 51.6 (44.7, 58.2) | 60.1 (50.3, 65.8) | 57.9 (49.1, 63.9) | < 0.001 |
| Forced Vital Capacity (% predicted) | 47 (38, 59) | 43 (33, 56) | 40 (32, 50) | 40 (31, 50) | < 0.001 |
| Resting Oxygen (liters per minute) | 4 (2, 6) | 4 (2, 6) | 4 (2, 6) | 4 (2, 6) | 0.043 |
| Six Minute Walk Distance (feet) | 835 (400, 1157) | 720 (398, 1000) | 690 (295, 1044) | 650 (300, 964) | < 0.001 |
| Pulmonary Artery Systolic Pressure (mmHg) | 38 (31, 48) | 49 (38.3, 62) | 35 (29, 47.8) | 38 (30, 48) | < 0.001 |
| Mechanical Ventilation (%) | 274 (3.4%) | 32 (2.4%) | 13 (4.8%) | 43 (4.5%) | 0.028 |
| Lung Allocation Score, at listing | 41.4 (36.4, 50.5) | 39.8 (35.2, 48.5) | 43.9 (38.6, 57.3) | 43.3 (37.6, 54.5) | < 0.001 |
This table displays median (interquartile range) for continuous variables and N (%) for categorical variable
Table 5.
Idiopathic Pulmonary Fibrosis Illness Severity at Transplant Listing by Race/Ethnicity
| White | Black | Asian | Hispanic | p value | |
|---|---|---|---|---|---|
| n = 5732 | n =486 | n = 181 | n = 626 | ||
| Age (years) | 62.4 (57.3, 66.5) | 54.3 (46.0, 60.7) | 63.0 (55.7, 66.7) | 59.8 (53.1, 65.1) | < 0.001 |
| Forced Vital Capacity (% predicted) | 48 (39, 59) | 42 (33, 55) | 40 (33, 52) | 41 (32, 51) | < 0.001 |
| Resting Oxygen (liters per minute) | 4 (2, 6) | 4 (2, 6) | 4 (2, 6) | 4 (2, 6) | 0.04 |
| Six Minute Walk Distance (feet) | 834 (393, 1165) | 708 (288, 1001) | 740 (295, 1043) | 617 (265, 944) | < 0.001 |
| Pulmonary Artery Systolic Pressure (mmHg) | 38 (31, 47) | 45 (36, 57) | 35 (29, 46) | 38 (30, 47) | < 0.001 |
| Mechanical Ventilation (%) | 203 (3.5%) | 13 (2.7%) | 8 (4.4%) | 28 (4.5%) | 0.498 |
| Lung Allocation Score, at listing | 42.0 (37.0, 51.3) | 43.7 (37.2, 55.1) | 46.2 (39.5, 61.2) | 44.6 (38.6, 56.7) | < 0.001 |
This table displays median (interquartile range) for continuous variables and N (%) for categorical variable
Discussion
Non-white candidates have decreased waitlist access to lung transplant compared to NHW candidates. There is no difference in waitlist mortality by race/ethnicity after adjusting for known risk factors; however, unadjusted waitlist mortality was higher in non-white candidates likely related to differences in diagnosis and illness severity at listing. Additionally, non-white pulmonary fibrosis candidates were younger and have lower lung function, worse functional capacity, and higher mechanical ventilation use at the time of listing than NHW candidates. NHB and Hispanic obstructive lung disease candidates were younger and have worse functional capacity, higher pulmonary artery pressure, increased mechanical ventilation use, and higher LAS at listing than NHW candidates.
The absence of disparities in transplant access or death between waitlisted black and white candidates in the LAS era has been previously reported,7 however, this work adds to the prior study by examining these outcomes amongst waitlisted Hispanic and Asian candidates and by using competing risk methodology to better delineate waitlist outcomes. In contrast to the previous study of LAS era candidates,7 we found evidence of decreased lung transplant access in NHB, Hispanic, and Asian waitlist candidates. Given there is no difference in adjusted mortality by ethnicity/race, the reason for decreased transplant access within these waitlisted groups may include removal for another reason or incomplete adjustment for other confounders. Notably, NHB waitlist candidates have an increased risk of removal for other reasons (HR 1.30, 95% CI 1.08–1.56), which may explain the transplant access disparity within this group. The number of candidates removed for other reasons is small with heterogeneous reasons for removal, which limits the ability to make definitive conclusions and/or reliably measure its significance, particularly across the smaller Hispanic and Asian candidate populations. Nevertheless, there is a need to address differences in waitlist transplant access by race/ethnicity, which may entail regulatory monitoring and reporting of other reasons for waitlist removal to improve center accountability and/or exploration of other unmeasured or incompletely measured variables such as listing at multiple centers or local transplant rates.
Notably, waitlist mortality remained higher in Hispanic candidates after adjusting for differences in diagnosis, age, and gender, suggesting that mortality differences related to geography or listing illness severity are at least partially responsible for higher mortality in this group. This is important, as differences in listing illness severity may be modifiable through changes in transplant referral and listing practices. NHW pulmonary fibrosis candidates have greater lung function and NHW obstructive lung disease and pulmonary fibrosis candidates have lower pulmonary artery pressures and greater functional capacity at listing than non-white candidates. A similar finding was seen within the pre-LAS era in black and Hispanic pulmonary fibrosis candidates and black COPD candidates.3,5 Notably, NHW pulmonary fibrosis and obstructive lung disease candidates were older than non-white candidates perhaps reflecting a different listing age threshold for NHW candidates versus non-white candidates. This finding was true even when isolating candidates with a specific diagnosis of IPF. While biological and genetic differences by race/ethnicity could plausibly contribute to differences in listing age or illness severity, we hypothesize that disparities in disease management, referral, and transplant center evaluation produce this finding. For example, initial diagnosis of the underlying lung disease, the decision to refer a patient for transplant evaluation, or a center’s decision to list a candidate could occur at different age or illness thresholds by race/ethnicity and contribute to differences in illness severity and age at transplant listing. These differences in illness severity impact waitlist and post-transplant mortality, as higher lung allocation scores are associated with greater waitlist and post-transplant mortality.2,17–19 While disparities in lung transplant access have focused on the final transition from waitlist placement to transplant, the presence and significance of disparities in the earlier phases of referral and evaluation have not been well characterized and deserve future study. Pre-waitlist barriers may include timely referral to a lung transplant center, cultural acceptability of transplant, accessibility to a transplant center based upon geographic distance and insurance coverage, and medical and psychosocial suitability of a candidate for transplant listing. Understanding where and if disparities exist within these phases can allow for targeted education and policy interventions to improve the equality of lung transplant access.
Notably, our results differ from those previously reported in the LAS era.7 Study differences in exclusion criteria including prior exclusion of patients with missing data, those actively listed at time of data analysis, or those removed for other reasons may account for some of the differences. The current study is different methodologically by the use of a competing risks analysis to more accurately model waitlist outcomes of transplant or death. Competing risks analysis avoids bias due to informative censoring and more accurately differentiates waitlist transplant access and mortality risk between race/ethnicities.13 Furthermore, this study included a greater number of candidates than previous studies, which allowed for an adequate sample size to include multiple race/ethnicities in analysis.
Our analysis has several limitations. Potential for misclassification of race/ethnicity, diagnosis, and reason for waitlist removal exist, as these are registry reported data fields that are dependent on what is collected and reported by transplant centers. Candidate household income was ascertained from county level income estimates and therefore is not specific to each candidate. Additionally, while we adjusted for candidate region when assessing waitlist outcomes, the number of waitlist candidates was not sufficient to assess whether these outcomes varied by geographic region or center. Finally, although we characterized listing illness severity differences within disease groups by race/ethnicity, we could not distinguish the effect of race/ethnicity on earlier care patterns such as timing of transplant referral or delays in placement on the waitlist. Future studies of advanced lung disease patients are needed to study disparities that may arise during these critical earlier periods, including initial management, transplant referral, and transplant evaluation.
Conclusion:
Among advanced lung disease patients who are listed for lung transplant within the LAS era, there is no adjusted difference in waitlist mortality by race/ethnicity, however unadjusted mortality and adjusted waitlist transplant access is worse in non-white candidates. Non-white obstructive lung disease and pulmonary fibrosis patients are generally younger with greater illness severity at transplant listing suggesting possible disparities in the management of advanced lung disease patients prior to transplant listing. Further work is needed to examine lung transplant disparities that occur prior to transplant listing.
Acknowledgments:
This work was conducted with support from a KL2 Mentored Career Development Award of the Stanford Clinical and Translational Science Award to Spectrum NIH KL2 TR 001083 (J.J.M) and the Hearst Family Foundation. The data reported here have been supplied by the Minneapolis Medical Research Foundation (MMRF) as the contractor for the Scientific Registry of Transplant Recipients (SRTR). The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the SRTR or the U.S. Government.
Funding Information: NIH KL2 TR 001083 (J.J.M) and the Hearst Family Foundation
Abbreviation List:
- IPF
Idiopathic pulmonary fibrosis
- LAS
lung allocation score
- SRTR
Scientific Registry of Transplant Recipients
- OPTN
Organ Procurement and Transplantation Network
- HRSA
Health Resources and Services Administration
- NHW
non-Hispanic white
- NHB
non-Hispanic black
- UNOS
United Network for Organ Sharing
- ECMO
extracorporeal membrane oxygenation
- FEV1
forced expiratory volume in one second
- FVC
forced vital capacity
Footnotes
Conflict of Interest: The authors report no conflicts of interest.
Prior Abstract Presentation: This work was previously presented in abstract format at the Thomas L. Petty Aspen Lung Conference, June 8, 2016.
References:
- 1.Valapour M, Paulson K, Smith JM, et al. OPTN/SRTR 2011 Annual Data Report: lung. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2013;13 Suppl 1:149–177. [DOI] [PubMed] [Google Scholar]
- 2.Valapour M, Skeans MA, Smith JM, et al. Lung. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2016;16 Suppl 2:141–168. [DOI] [PubMed] [Google Scholar]
- 3.Lederer DJ, Arcasoy SM, Barr RG, et al. Racial and ethnic disparities in idiopathic pulmonary fibrosis: A UNOS/OPTN database analysis. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2006;6(10):2436–2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lederer DJ, Caplan-Shaw CE, O’Shea MK, et al. Racial and ethnic disparities in survival in lung transplant candidates with idiopathic pulmonary fibrosis. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2006;6(2):398–403. [DOI] [PubMed] [Google Scholar]
- 5.Lederer DJ, Benn EK, Barr RG, et al. Racial differences in waiting list outcomes in chronic obstructive pulmonary disease. American journal of respiratory and critical care medicine. 2008;177(4):450–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Egan TM, Murray S, Bustami RT, et al. Development of the new lung allocation system in the United States. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2006;6(5 Pt 2):1212–1227. [DOI] [PubMed] [Google Scholar]
- 7.Wille KM, Harrington KF, deAndrade JA, Vishin S, Oster RA, Kaslow RA. Disparities in lung transplantation before and after introduction of the lung allocation score. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 2013;32(7):684–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valapour M, Skeans MA, Heubner BM, et al. OPTN/SRTR 2012 Annual Data Report: lung. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2014;14 Suppl 1:139–165. [DOI] [PubMed] [Google Scholar]
- 9.Valapour M, Skeans MA, Heubner BM, et al. OPTN/SRTR 2013 Annual Data Report: lung. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2015;15 Suppl 2:1–28. [DOI] [PubMed] [Google Scholar]
- 10.United States Census Bureau. Small Area Income and Poverty Estimates (SAIPE). 2013; https://www.census.gov/did/www/saipe/data/. Accessed July 1, 2016.
- 11.Putter H, Fiocco M, Geskus RB. Tutorial in biostatistics: competing risks and multi-state models. Statistics in medicine. 2007;26(11):2389–2430. [DOI] [PubMed] [Google Scholar]
- 12.Kim WR, Therneau TM, Benson JT, et al. Deaths on the liver transplant waiting list: an analysis of competing risks. Hepatology. 2006;43(2):345–351. [DOI] [PubMed] [Google Scholar]
- 13.Sapir-Pichhadze R, Pintilie M, Tinckam KJ, et al. Survival Analysis in the Presence of Competing Risks: The Example of Waitlisted Kidney Transplant Candidates. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2016;16(7):1958–1966. [DOI] [PubMed] [Google Scholar]
- 14.R: A Language and Environment for Statistical Computing [computer program]. Vienna, Austria: 2013. [Google Scholar]
- 15.de Wreede L, Fiocco M, Putter H. mstate: An R Package for the Analysis of Competing Risks and Multi-State Models. Journal of Statistical Software. 2011;38(7):1–30. [Google Scholar]
- 16.de Wreede LC, Fiocco M, Putter H. The mstate package for estimation and prediction in non- and semi-parametric multi-state and competing risks models. Computer Methods and Programs in Biomedicine. 2010;99(3):261–274. [DOI] [PubMed] [Google Scholar]
- 17.Liu V, Zamora MR, Dhillon GS, Weill D. Increasing lung allocation scores predict worsened survival among lung transplant recipients. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2010;10(4):915–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merlo CA, Weiss ES, Orens JB, et al. Impact of U.S. Lung Allocation Score on survival after lung transplantation. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 2009;28(8):769–775. [DOI] [PubMed] [Google Scholar]
- 19.Weiss ES, Allen JG, Merlo CA, Conte JV, Shah AS. Lung allocation score predicts survival in lung transplantation patients with pulmonary fibrosis. The Annals of thoracic surgery. 2009;88(6):1757–1764. [DOI] [PubMed] [Google Scholar]