Abstract
The term “conduct problems” refers to a pattern of repetitive rule-breaking behavior, aggression, and disregard for others. Such problems have received increased attention recently, owing to violent events perpetrated by youth and modifications in the Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria for conduct disorder, a syndrome involving recurrent conduct problems in children and adolescents. Youth conduct problems are predictive of an increased risk of substance abuse, criminal behavior, and educational disruption1; they also incur a considerable societal burden from interpersonal suffering and financial costs.2 This review summarizes current data on youth conduct problems and highlights promising avenues for research. Prior reviews have summarized either the clinical literature on outcome, treatment, and familial aggregation or the neurocognitive literature on mechanisms and pathophysiology.3–5 The current review differs by more tightly integrating clinical and neurocognitive perspectives.
PSYCHOPATHIC TRAITS
Current research on conduct problems focuses heavily on psychopathic traits, labeled as “callous–unemotional” when referring to such traits in youth, which include reduced guilt, callousness, uncaring behavior, and reduced empathy. On the basis of this research, callous–unemotional traits have been added to the fifth edition of the DSM (DSM-5) as a specifier for the diagnosis of conduct disorder. (Given concerns about the potentially stigmatizing nature of the term “callous–unemotional,” this entity is instead indicated by the phrase “with limited prosocial emotions” in DSM-5.)
The addition of this specifier reflects efforts to identify syndromes characterized by combinations of clinical and neurocognitive features. Callous–unemotional traits, which occur in fewer than half of young persons with conduct disorder, identify a subgroup with distinctive clinical features and neurocognitive perturbations. As compared with youth with conduct disorder who show remorse, empathy, and concern about school performance, those with callous–unemotional traits have a poorer prognosis and treatment response.3,6,7 The current review contrasts research on these two subgroups to illustrate how combining clinical and neurocognitive perspectives might facilitate outcome prediction and the development of new therapeutics.
DEVELOPMENT AND OUTCOME
Most longitudinal research on conduct problems charts clinical profiles without concomitant data on neurocognitive functions. This work shows considerable heterogeneity in course: children with similar clinical profiles often have distinct longitudinal outcomes. Although some studies have begun to combine clinical and neurocognitive data in an attempt to predict outcome,8–10 future prospective studies might do so more extensively, testing whether specific combinations of clinical and neurocognitive profiles identify subgroups with homogeneous outcomes.
For children with long-term behavioral problems, signs of conduct disorder often arise by early school age, but few children meet the full criteria for the disorder before 10 years of age. These early signs involve aggressive tendencies, impulsivity, and failure to comply with requests, which are features of attention deficit–hyperactivity disorder (ADHD) and oppositional-defiant disorder (see the Glossary). Prospective data show a trajectory of behavioral problems, with progression from ADHD in early school years to oppositional–defiant disorder in subsequent years, followed by conduct disorder as children approach adolescence.11 Although this developmental pattern is common, it is not typical in children who have early behavioral problems — that is, conduct disorder does not develop in most children with ADHD or oppositional–defiant disorder,12,13 and successful treatment of these two conditions may reduce the risk of progression. Like ADHD and oppositional–defiant disorder, callous–unemotional traits are expressed early. Such traits have been identified in children as young as 2 years of age,14 and among young children with conduct problems, they predict a particularly early onset of a severe,15 persistent variant of conduct problems.7
Once the diagnosis of conduct disorder is established, the prognosis is usually considered to be poor, though the outcome varies. Antisocial personality disorder, which has a particularly poor prognosis, develops in slightly less than 50% of patients with conduct disorder; however, youth with conduct disorder in whom antisocial personality disorder does not develop typically have other long-term problems. Thus, persistent psychopathology is the rule, though its nature can vary.16 Considerable stability is seen in callous–unemotional traits, with stability coefficients of 0.5 to 0.7 among children followed over a period of 4 to 9 years.4 The outcome may be particularly poor if the behavioral problems begin before 10 years of age.17 Some research suggests that such an early onset predicts stronger biologic correlates and greater persistence into adulthood than the later-onset variant.17 However, research has not consistently shown such distinctions for biologic features18 or outcome.19
NEUROCOGNITIVE DYSFUNCTIONS
Promising work on outcome prediction and new therapeutics uses a neuroscientific systems approach, linking individual differences in behavior to underlying mechanisms that shape brain function. This approach is used in the Research Domain Criteria project (www.nimh.nih.gov/research-priorities/rdoc/index.shtml). Fundamentally, the purpose of the project is to identify neurocognitive functions, for which the brain mechanisms are understood, that can predict outcome or treatment response. This approach requires research conducted at both a brain-systems level, focused on neural circuits, and a clinical level, focused on individual differences in behavior contributing to mental illness.
As described below, three neurocognitive dysfunctions have been linked to clinical aspects of conduct disorder, thereby bridging brain-systems and clinical data. This work has involved a range of clinical entities, which often overlap in patterns depicted in Figure 1. As discussed below, these dysfunctions are more clearly associated with callous–unemotional traits than the other entities shown in Figure 1. Thus, the first dysfunction, deficient empathy, occurs relatively selectively in youth with these traits, whereas the second dysfunction, heightened threat sensitivity, does not occur in this group. Rather, heightened threat sensitivity occurs in patients who have conduct disorder without callous–unemotional traits and in patients with anxiety disorders. The third dysfunction, deficient decision making, is expressed similarly in youth with conduct disorder who have callous–unemotional traits and those without such traits. Moreover, deficient decision making may represent the lowest common denominator for conduct problems — that is, the dysfunction is shared by multiple syndromes involving conduct problems. Few studies have examined correlations among these three neural dysfunctions, and none have directly compared patterns of dysfunction in children with the different clinical presentations depicted in Figure 1. Hence, it remains unclear how these dysfunctions interact to shape clinical profiles for individual children.
Figure 1. Overlap among Six Clinical Entities.
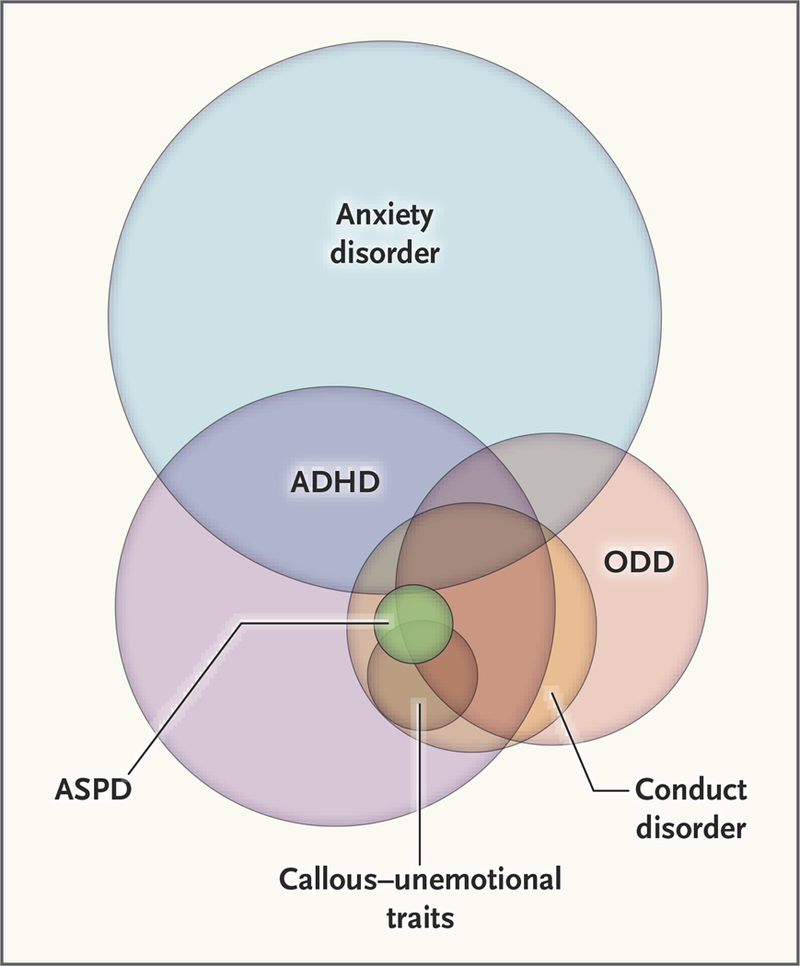
The size of each circle represents the relative prevalence of the clinical entity in the community. ADHD denotes attention deficit–hyperactivity disorder, ASPD antisocial personality disorder, and ODD oppositional–defiant disorder.
The hope is that further research on these three dysfunctions will generate biologically based diagnostic tests that are analogous to other diagnostic tests in medicine. That is, such tests would augment rather than replace current psychiatric-assessment techniques by differentiating among patients with similar clinical presentations on the basis of the ability of the tests to predict a specific course or treatment sensitivity.
DEFICIENT EMPATHY
Empathy influences behavior at many levels. Persons who have high levels of empathy for a victim, relative to those with low levels of empathy, may show lower levels of aggressive response and higher levels of altruism toward the victim.20–22 Developmentally, empathy is critical for socialization. Caregivers typically respond to transgressions that harm others by focusing on the victim’s distress.23 Children learn to refrain from harming others in order to prevent these associated aversive feelings.
Deficient empathy shows a particularly selective association with conduct disorder accompanied by callous–unemotional traits.3 This deficiency is manifested in patients’ reports of minimal emotional responses and an impaired ability to recognize distress in peers24,25 or respond physiologically to it.26,27 In youth with conduct disorder, the presence of callous–unemotional traits predicts a poor response to typical socialization practices.1
Deficient empathy is related to amygdala dysfunction.3 The amygdala plays a central role in aversive conditioning. Through this form of reinforcement learning, persons learn to respond with fear to a previously neutral action or object, after the action or object has been paired with the occurrence of an aversive event.28 Indeed, amygdala responses during prototypical forms of reinforcement learning are reduced in persons with psychopathic traits.29 Functional magnetic resonance imaging (fMRI) studies have shown that adolescents with callous–unemotional traits, as compared with adolescents without such traits, have reduced amygdala responses to images of faces with fearful expressions30–32; these weaker responses are presumably due to deficient empathy. Such studies require participants to view a series of faces that vary in their emotional features; faces with fearful expressions preferentially engage the amygdala relative to other expressions (Fig. 2).
Figure 2. Functional MRI Study of Face Processing.
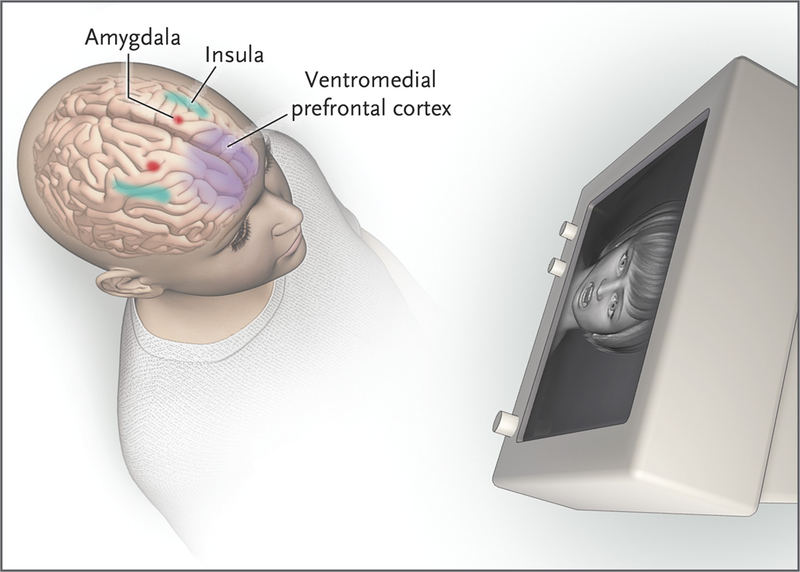
In the study, a child views a series of faces expressing various emotions. To ensure attention to each face, the child is asked to identify the sex of the person. In healthy children, faces with fearful expressions elicit greater amygdala activation than faces with neutral expressions. Faces with emotional expressions other than fear elicit activation in other structures, including the insula and prefrontal cortex. Amygdala activation in response to fearful faces is reduced in youth with conduct disorder and callous–unemotional traits, as compared with either healthy youth or those who have conduct disorder without callous–unemotional traits.
HEIGHTENED THREAT SENSITIVITY
The amygdala functions in multiple circuits to support diverse psychological abilities. Beyond its role in empathy, the amygdala functions in a circuit encompassing the brain stem, the prefrontal cortex, and the association cortex in the temporal lobe. Heightened responsiveness of this circuit may be associated with general difficulties in the processing of emotional expression and certain peripheral hemodynamic changes in various forms of developmental psychopathology.33–35 Moreover, the amygdala is part of a circuit, encompassing the hypothalamus and periaqueductal gray matter, that mediates graded responses to threats36: from freezing to flight to reactive aggression with increasing proximity of the threat.37 Increased activity in this circuit, after exposure to threat, increases the probability of reactive aggression. Figure 3 depicts the functioning of this circuit, illustrating how threat proximity modulates activity and behavior.
Figure 3. Relationships among the Proximity of a Threat, the Activity in a Particular Neural Circuit, and the Behavioral Response to the Threat.
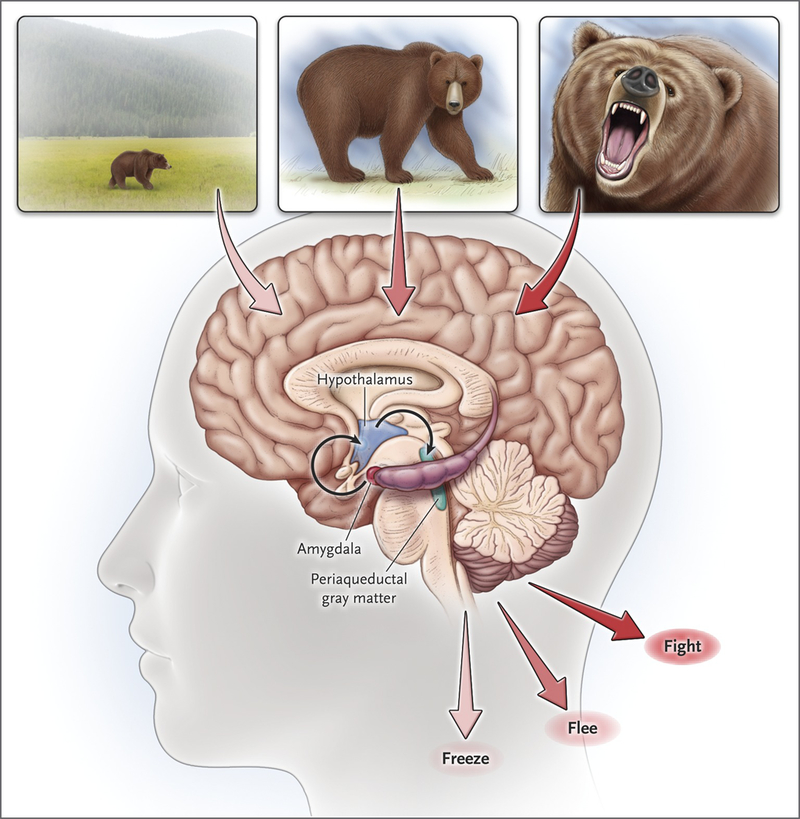
The neural circuit that is activated in response to a threat connects the amygdala, hypothalamus, and periaqueductal gray matter. The figure depicts a threat of increasing proximity, in the form of a bear that appears in the distance, somewhat closer, or very close and about to attack. The brain circuitry activity increases as the threat draws closer. Also shown are the different behaviors that are elicited as the proximity of the threat increases: from freezing to flight to fight.
Functioning in this circuit may differentiate subgroups of youth with conduct disorder. One subgroup has callous–unemotional traits and shows reduced amygdala function when performing tasks that engage either empathic responding or threat assessment. The subgroup without callous–unemotional traits exhibits a different pattern, with atypically elevated threat-circuitry responsiveness,38 a hostile attributional bias,39 and increased risks of anxiety and aggression in reaction to frustration or threat.1 Indeed, patients with conduct problems who do not have callous–unemotional traits, much like patients with anxiety disorders,40 show elevated amygdala responses to threat, as compared with responses in youth free of psychopathology.32 The risk of reactive aggression may be highest when such heightened responses occur in tandem with impulsivity or other features of ADHD. This combination is a feature of many disorders, including intermittent explosive disorder, borderline personality disorder, and disruptive mood dysregulation disorder.41–43 In short, youth with elevated amygdala responsiveness to threat might have different problems over time and different responses to treatment than youth with normal or reduced amygdala responsiveness.
DEFICIENT DECISION MAKING
Persons who fail to learn how to make choices that lead to rewards rather than punishments are at high risk for impulsivity, frustration, and reactive aggression. Patients with conduct disorder exhibit such difficulties when performing tasks that require flexible responses to changing task contingencies.44–46
Neuroscientific systems research shows that the striatum and ventromedial prefrontal cortex represent the value of an action and influence prediction-error signaling (Fig. 4), functions that are critical for decision making.47 This research requires the participant to learn to differentiate rewarding from punishing stimuli by pressing a button after exposure to one type of stimulus and not pressing the button after exposure to the other type of stimulus. In such research, the participant is said to appropriately represent value when the participant has learned the corresponding rewarding and punishing consequences that follow from either pressing or not pressing the button after exposure to each stimulus. Before learning these stimulus–response contingencies, the participant cannot represent value and hence cannot predict the occurrence of rewards and punishments. In this context, receipt of an unexpected reward elicits a brain response known as a positive prediction error, indicating that an event is more rewarding than expected. Conversely, failure to receive an expected reward elicits a response known as a negative prediction error, indicating that an event is less rewarding than expected. In such research, youth with conduct problems show deficits in negative-prediction-error signaling, manifested by deficient recruitment of the striatum and ventromedial prefrontal cortex.44–46 Thus, deficient brain functioning may be associated with deficient decision making.
Figure 4. Format of a Functional MRI Study of Decision Making and Brain-Activation Data as They Relate to Prediction-Error Signals in the Basal Ganglia.
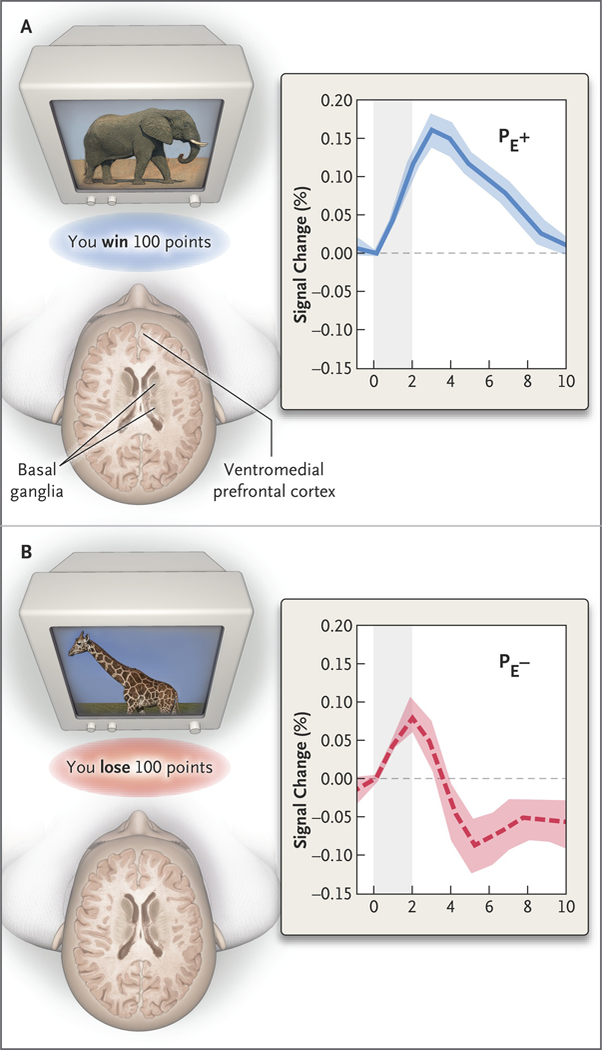
In this type of study, a research participant must learn to select one set of stimuli (e.g., the elephant) by pressing a button and to avoid another set of stimuli (e.g., the giraffe) by not pressing the button. Receipt of an unexpected reward elicits a positive prediction error (PE+), whereas failure to receive an expected reward, or a loss that is greater than expected, elicits a negative prediction error (PE−). The plots show responses to feedback in the basal ganglia during blood oxygen level–dependent functional MRI; the ventromedial prefrontal cortex is also shown. The timing of feedback is represented by the shaded column beginning at time zero. A PE+ occurs when the participant wins more than expected after pushing a button at the sight of the elephant. A PE− occurs when the participant loses more than expected after pushing a button at the sight of the giraffe. These positive and negative prediction errors generate the depicted reaction in the basal ganglia.
Perturbed decision making occurs more broadly than perturbed empathy or threat sensitivity. Decision-making impairments occur in youth who have conduct disorder with or without callous–unemotional traits,44 in youth with ADHD or oppositional–defiant disorder,48–50 and even in unaffected children of parents with conduct problems or drug addiction.51 Thus, impaired decision making may be a substrate for various types of conduct problems that frequently coexist, including DSM diagnoses of conduct disorder, ADHD, oppositional–defiant disorder, and substance-use disorders.
GENETIC AND ENVIRONMENTAL RISKS
Genetic and environmental risks interact through their effects on brain function. These interactions are seen in behavioral research involving twins, adoptees, and families in natural experiments as well as in molecular research on genetic and epigenetic factors.
GENETIC RISK
Considerable data from genetic epidemiologic studies have shown moderate-to-high heritability for clinical aspects of conduct problems, including aggression52 and callous–unemotional traits.53 Other work in this area has suggested that performance on neurocognitive tasks related to empathy and decision making is also heritable.54 These findings point to an avenue for future research that integrates a neuroscientific systems approach with genetic studies to elucidate how genetic factors shape clinical profiles through effects on neurocognitive function. However, because research in this area is only beginning, a consensus has not emerged on the most productive directions for investigation. Some work has linked specific genetic polymorphisms with individual differences in the circuitry mediating empathy and threat sensitivity.55 However, much of this research has relied on candidate-gene approaches in relatively small samples, raising concern about type I errors.55
ENVIRONMENTAL RISK
Different aspects of the environment relate to conduct problems at distinct developmental phases. Some factors, such as maternal diet or smoking, represent prenatal risks, which affect the development of neural structures (e.g., the amygdala, striatum, and ventromedial prefrontal cortex) that are linked to conduct disorder and perturbed neurocognitive functions.56–58 Like research on genetic factors, this work suggests that environmental risks confer a predisposition to conduct problems through effects on neurocognitive function. Risk factors with a postnatal effect include low levels of parental monitoring, exposure to violence, and harsh and inconsistent discipline, as well as circumstances, such as poverty, in which the other risk factors tend to coalesce. As with prenatal risks, the later-occurring risks are also related to perturbed neurocognitive function.
Environmental factors may interact with characteristics of the child. For example, parenting variables have less effect on the conduct problems of children with callous–unemotional traits than on those of children without these traits.59 In addition, the low degree of stress reactivity seen in youth with callous–unemotional traits may reduce the negative effects of exposure to adversities that predict heightened amygdala responses to threat,60,61 anxiety,62 and reactive aggression.39
TREATMENT
Various treatments reduce conduct problems. When delivered early, they can be effective63,64 and may prevent developmental progression.65 However, there is a need for better treatments. Currently available treatments target symptoms rather than underlying mechanisms, since the latter are, as yet, unknown. Most important, currently available treatments are only moderately effective.
The hope is that pathophysiological research will yield more effective treatments. From this perspective, unique subgroups may exhibit unique dysfunctions in neural circuits that respond to specific treatments targeting these dysfunctions. Modest effectiveness in treating a heterogeneous construct such as conduct disorder may reflect the failure to tailor treatments to specific pathogenic mechanisms.
Two types of psychosocial intervention are effective in reducing conduct problems. One targets diverse behaviors with the use of multiple treatment components, including components that rely on principles from cognitive behavioral therapy to address anxiety and related emotional problems. Such problems can be viewed as clinical manifestations of threat-circuit hypersensitivity that occur in conduct disorder accompanied by anxiety and a hostile attributional bias. For example, Multidimensional Treatment Foster Care66 and Multisystemic Therapy67 treat diverse aspects of conduct problems by applying social and emotional learning techniques. In the treatment of anxiety, this involves the use of techniques from cognitive behavioral therapy. The therapist begins by having the child hierarchically rank the scenarios that elicit fear and by teaching the child strategies to minimize such fear. Next, the child works with the therapist to confront these scenarios and extinguish the associated fear, working gradually over time to confront increasingly frightening scenarios in each therapy session. These techniques may reduce reactive aggression by decreasing clinical anxiety, threat hypersensitivity, and associated cognitive perturbations, such as a hostile attributional bias.
The other form of effective psychosocial intervention facilitates proper child-rearing practices. This involves teaching parents to reduce stress in the home, use supportive rather than harsh limit-setting practices, monitor the child’s activities, and obtain services as needed. Most research on these two types of intervention shows that children with callous–unemotional traits have a less robust response than children without such traits,68,69 possibly because the interventions fail to target relevant mechanisms in the former group.
Two pharmacologic interventions also show promise, but concerns about adverse effects should lead to judicious use.70 First, antipsychotic medications reduce irritability and aggression in children.70–72 The Food and Drug Administration (FDA) has approved two medications, risperidone and aripiprazole, for the treatment of irritability and aggression in autism. Although autism is not strongly associated with conduct problems, data leading to FDA approval for these indications broadly inform clinicians regarding the use of these agents in children. Other data show efficacy in youth conduct problems occurring in other contexts, but the usefulness of the drugs is limited by short-term adverse effects, such as sedation, and long-term adverse effects from disrupted metabolic and neurologic functions.
Second, data also show benefits of psychostimulant medications. For example, methylphenidate reduces aggression in youth with ADHD or with conduct disorder, even in the absence of ADHD.73 In general, psychostimulants are preferable to antipsychotic agents owing to fewer adverse effects. Nevertheless, stimulants can exacerbate anxiety and cause agitation. Moreover, as with antipsychotic agents, evidence of a benefit comes from short-term efficacy studies.
Although there has been minimal research on the long-term stability of brain dysfunction in conduct disorder, biologic markers assessed at one point in time have been shown to predict the long-term outcome.8–10 This suggests that brain dysfunction associated with conduct disorder exhibits some degree of stability. Thus, although clinical experience suggests that signs and symptoms can wax and wane in children with behavioral problems, it is unusual for these problems to remit spontaneously in children with conduct disorder, necessitating long-term treatment. Clinical experience suggests that psychostimulants can be prescribed safely for relatively long periods of time with careful monitoring. However, even though no long-term risks of psychostimulants have been unequivocally documented, concerns remain about growth disruption, adverse cardiovascular effects, and adverse effects on behavior, such as substance abuse; more research is needed on these possible effects.
FUTURE DIRECTIONS AND CONCLUSIONS
Current research seeks to identify new treatment approaches that are based on knowledge of pathophysiology and to use this knowledge to tailor treatments to individual patients. There is relatively good evidence of dysfunctional mechanisms, at least at the neuroscientific systems level, that are linked to conduct disorder. The critical test will be whether this information can be used to predict the course of the disorder and identify treatment for individual patients. Given the state of the research, this will require many years. Nevertheless, preliminary findings suggest that measures reflecting the integrity of threat-related or decision-making circuitry might predict risk.8–10 Currently, there are virtually no data on biomarkers that might be used to predict the response to treatment, and there are only limited data on the ways in which current treatments alter pathophysiology.
In conclusion, the diagnosis of conduct disorder encompasses at least two subgroups: one group exhibits callous–unemotional traits, which are associated with an increased risk of persistent antisocial behavior; the other group shows heightened threat sensitivity and reactive aggression. Both groups have perturbations in neural systems that are critical for decision making. Conduct disorder with callous–unemotional traits appears to be more difficult to treat, and advances in our understanding of the pathophysiology of this type of conduct disorder may aid in the search for new treatments.
Supplementary Material
Glossary
- Antisocial personality disorder (ASPD)
Like other personality disorders, ASPD refers to a long-standing pattern of behavior, typically manifesting in adults, which broadly interferes with functioning. ASPD differs from other personality disorders on the basis of its associated high levels of persistent aggression and rule-violating behavior. Nearly all persons with ASPD will have had conduct disorder in childhood, and many of them will also have exhibited callous–unemotional traits. A minority of children with conduct disorder go on to have ASPD as adults, and those who do are more likely to have had callous–unemotional features than those who do not
- Anxiety disorder
The term refers to a family of mental disorders that involve excessive fear and anxiety. Although fear and anxiety are features of normal development, in anxiety disorders excessive fear and anxiety usually impair functioning through the avoidance of feared objects or scenarios. Anxiety disorders are extremely common during childhood. Typically, in clinical settings, approximately half of all children with an anxiety disorder have a behavioral disorder, such as conduct disorder, oppositional–defiant disorder, or attention deficit–hyperactivity disorder, and approximately half of all children seen for one of these behavioral disorders have an anxiety disorder
- Attention deficit–hyperactivity disorder (ADHD)
ADHD is one of the most common reasons why families seek mental health services for their children. This mental disorder is characterized by high levels of inattention, hyperactivity, and excessive impulsivity. The condition typically arises by school age and predicts a high risk of other behavioral problems, such as oppositional–defiant disorder and conduct disorder. In clinical settings, about half of children with ADHD have an anxiety disorder, and an even greater proportion have one of two behavioral disorders: conduct disorder and oppositional–defiant disorder. Conversely, most children for whom treatment for these behavioral disorders is sought have ADHD
- Callous–unemotional traits
This term refers to patterns of callousness, uncaring behavior, reduced guilt, and reduced empathy. When such traits accompany mental disorders, they typically occur in children with conduct disorder. Nevertheless, fewer than half of all patients with conduct disorder manifest callous–unemotional traits, though this relatively small group of children has a particularly high risk of ASPD and other adverse outcomes
- Conduct disorder
Conduct disorder is a mental disorder arising in childhood that is less common than anxiety disorders or ADHD. The syndrome involves high levels of aggression and rule-violating behavior. In clinical settings, conduct disorder usually occurs in children with a history of ADHD and oppositional–defiant disorder. Particularly when it is accompanied by callous–unemotional traits, conduct disorder predicts a high risk of chronic behavioral problems, which can be expressed as ASPD in adulthood; however, fewer than half of patients with conduct disorder will go on to have ASPD
- Oppositional–defiant disorder (ODD)
This mental disorder arises in childhood and is characterized by persistent angry, irritable, and argumentative behaviors. Although such behaviors are common in children, in ODD the behaviors occur at particularly high levels in ways that interfere with functioning. In clinical settings, ODD usually occurs in children with a history of ADHD, and over time a substantial minority of such children will have conduct disorder
Footnotes
No potential conflict of interest relevant to this article was reported.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
REFERENCES
- 1.Frick PJ, Ray JV, Thornton LC, Kahn RE. Can callous-unemotional traits enhance the understanding, diagnosis, and treatment of serious conduct problems in children and adolescents? A comprehensive review. Psychol Bull 2014;140:1–57. [DOI] [PubMed] [Google Scholar]
- 2.Scott S, Knapp M, Henderson J, Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. BMJ 2001;323:191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blair RJ. The neurobiology of psychopathic traits in youths. Nat Rev Neurosci 2013;14:786–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frick PJ, Ray JV, Thornton LC, Kahn RE. Annual research review: a developmental psychopathology approach to understanding callous-unemotional traits in children and adolescents with serious conduct problems. J Child Psychol Psychiatry 2014;55:532–48. [DOI] [PubMed] [Google Scholar]
- 5.Waller R, Gardner F, Hyde LW. What are the associations between parenting, callous-unemotional traits, and antisocial behavior in youth? A systematic review of evidence. Clin Psychol Rev 2013;33:593–608. [DOI] [PubMed] [Google Scholar]
- 6.Pardini DA, Frick PJ, Moffitt TE. Building an evidence base for DSM-5 conceptualizations of oppositional defiant disorder and conduct disorder: introduction to the special section. J Abnorm Psychol 2010;119:683–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rowe R, Maughan B, Moran P, Ford T, Briskman J, Goodman R. The role of callous and unemotional traits in the diagnosis of conduct disorder. J Child Psychol Psychiatry 2010;51:688–95. [DOI] [PubMed] [Google Scholar]
- 8.Gao Y, Raine A, Venables PH, Dawson ME, Mednick SA. Association of poor childhood fear conditioning and adult crime. Am J Psychiatry 2010;167:56–60. [DOI] [PubMed] [Google Scholar]
- 9.Aharoni E, Vincent GM, Harenski CL, et al. Neuroprediction of future rearrest. Proc Natl Acad Sci U S A 2013;110:6223–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pardini DA, Raine A, Erickson K, Loeber R. Lower amygdala volume in men is associated with childhood aggression, early psychopathic traits, and future violence. Biol Psychiatry 2014;75:73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. J Child Psychol Psychiatry 2005;46:1200–10. [DOI] [PubMed] [Google Scholar]
- 12.Rowe R, Costello EJ, Angold A, Copeland WE, Maughan B. Developmental pathways in oppositional defiant disorder and conduct disorder. J Abnorm Psychol 2010;119:726–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mannuzza S, Klein RG, Bonagura N, Malloy P, Giampino TL, Addalli KA. Hyperactive boys almost grown up. V. Replication of psychiatric status. Arch Gen Psychiatry 1991;48:77–83. [DOI] [PubMed] [Google Scholar]
- 14.Waller R, Gardner F, Hyde LW, Shaw DS, Dishion TJ, Wilson MN. Do harsh and positive parenting predict parent reports of deceitful-callous behavior in early childhood? J Child Psychol Psychiatry 2012;53:946–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dandreaux DM, Frick PJ. Developmental pathways to conduct problems: a further test of the childhood and adolescent-onset distinction. J Abnorm Child Psychol 2009;37:375–85. [DOI] [PubMed] [Google Scholar]
- 16.Robins LN, Price RK. Adult disorders predicted by childhood conduct problems: results from the NIMH Epidemiologic Catchment Area project. Psychiatry 1991;54:116–32. [DOI] [PubMed] [Google Scholar]
- 17.Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychol Rev 1993;100:674–701. [PubMed] [Google Scholar]
- 18.Passamonti L, Fairchild G, Goodyer IM, et al. Neural abnormalities in early-onset and adolescence-onset conduct disorder. Arch Gen Psychiatry 2010;67:729–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Odgers CL, Moffitt TE, Broadbent JM, et al. Female and male antisocial trajectories: from childhood origins to adult outcomes. Dev Psychopathol 2008;20:673–716. [DOI] [PubMed] [Google Scholar]
- 20.Batson CD. Altruism in humans. New York: Oxford University Press, 2011. [Google Scholar]
- 21.Lozier LM, Cardinale EM, VanMeter JW, Marsh AA. Mediation of the relationship between callous-unemotional traits and proactive aggression by amygdala response to fear among children with conduct problems. JAMA Psychiatry 2014; 71:627–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blair RJR. A cognitive developmental approach to mortality: investigating the psychopath. Cognition 1995;57:1–29. [DOI] [PubMed] [Google Scholar]
- 23.Nucci LP, Nucci M. Children’s social interactions in the context of moral and conventional transgressions. Child Dev 1982;53:403–12. [Google Scholar]
- 24.Marsh AA, Blair RJ. Deficits in facial affect recognition among antisocial populations: a meta-analysis. Neurosci Biobehav Rev 2008;32:454–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dawel A, O’Kearney R, McKone E, Palermo R. Not just fear and sadness: meta-analytic evidence of pervasive emotion recognition deficits for facial and vocal expressions in psychopathy. Neurosci Biobehav Rev 2012;36:2288–304. [DOI] [PubMed] [Google Scholar]
- 26.Blair RJR. Responsiveness to distress cues in the child with psychopathic tendencies. Pers Individ Dif 1999;27:135–45. [Google Scholar]
- 27.de Wied M, van Boxtel A, Matthys W, Meeus W. Verbal, facial and autonomic responses to empathy-eliciting film clips by disruptive male adolescents with high versus low callous-unemotional traits. J Abnorm Child Psychol 2012;40:211–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jeon D, Kim S, Chetana M, et al. Observational fear learning involves affective pain system and Cav1.2 Ca2+ channels in ACC. Nat Neurosci 2010;13:482–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Birbaumer N, Veit R, Lotze M, et al. Deficient fear conditioning in psychopathy: a functional magnetic resonance imaging study. Arch Gen Psychiatry 2005;62:799–805. [DOI] [PubMed] [Google Scholar]
- 30.Marsh AA, Finger EC, Mitchell DG, et al. Reduced amygdala response to fearful expressions in children and adolescents with callous-unemotional traits and disruptive behavior disorders. Am J Psychiatry 2008;165:712–20. [Errata, Am J Psychiatry 2008;165:652, 920.] [DOI] [PubMed] [Google Scholar]
- 31.White SF, Marsh AA, Fowler KA, et al. Reduced amygdala responding in youth with disruptive behavior disorder and psychopathic traits reflects a reduced emotional response not increased top- down attention to non-emotional features. Am J Psychiatry 2012;169:750–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Viding E, Sebastian CL, Dadds MR, et al. Amygdala response to preattentive masked fear in children with conduct problems: the role of callous-unemotional traits. Am J Psychiatry 2012;169:1109–16. [DOI] [PubMed] [Google Scholar]
- 33.Park G, Van Bavel JJ, Vasey MW, Thayer JF. Cardiac vagal tone predicts attentional engagement to and disengagement from fearful faces. Emotion 2013;13:645–56. [DOI] [PubMed] [Google Scholar]
- 34.Guyer AE, McClure EB, Adler AD, et al. Specificity of facial expression labeling deficits in childhood psychopathology. J Child Psychol Psychiatry 2007;48:863–71. [DOI] [PubMed] [Google Scholar]
- 35.McCubbin JA, Merritt MM, Sollers JJ III, et al. Cardiovascular-emotional dampening: the relationship between blood pressure and recognition of emotion. Psychosom Med 2011;73:743–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gregg TR, Siegel A. Brain structures and neurotransmitters regulating aggression in cats: implications for human aggression. Prog Neuropsychopharmacol Biol Psychiatry 2001;25:91–140. [DOI] [PubMed] [Google Scholar]
- 37.Blanchard RJ, Blanchard DC, Takahashi T, Kelley MJ. Attack and defensive behaviour in the albino rat. Anim Behav 1977;25:622–34. [DOI] [PubMed] [Google Scholar]
- 38.Crowe SL, Blair RJR. The development of antisocial behavior: what can we learn from functional neuroimaging studies? Dev Psychopathol 2008;20:1145–59. [DOI] [PubMed] [Google Scholar]
- 39.Dodge KA, Pettit GS, Bates JE, Valente E. Social information-processing patterns partially mediate the effect of early physical abuse on later conduct problems. J Abnorm Psychol 1995;104:632–43. [DOI] [PubMed] [Google Scholar]
- 40.Blackford JU, Pine DS. Neural substrates of childhood anxiety disorders: a review of neuroimaging findings. Child Adolesc Psychiatr Clin N Am 2012;21:501–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Coccaro EF, McCloskey MS, Fitzgerald DA, Phan KL. Amygdala and orbitofrontal reactivity to social threat in individuals with impulsive aggression. Biol Psychiatry 2007;62:168–78. [DOI] [PubMed] [Google Scholar]
- 42.New AS, Hazlett EA, Newmark RE, et al. Laboratory induced aggression: a positron emission tomography study of aggressive individuals with borderline personality disorder. Biol Psychiatry 2009; 66:1107–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Leibenluft E Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. Am J Psychiatry 2011;168:129–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.White SF, Pope K, Sinclair S, et al. Disrupted expected value and prediction error signaling in youths with disruptive behavior disorders during a passive avoidance task. Am J Psychiatry 2013;170:315–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Finger EC, Marsh AA, Mitchell DG, et al. Abnormal ventromedial prefrontal cortex function in children with psychopathic traits during reversal learning. Arch Gen Psychiatry 2008;65:586–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Crowley TJ, Dalwani MS, Mikulich-Gilbertson SK, et al. Risky decisions and their consequences: neural processing by boys with antisocial substance disorder. PLoS One 2010;5(9):e12835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.O’Doherty JP. Beyond simple reinforcement learning: the computational neurobiology of reward-learning and valuation. Eur J Neurosci 2012;35:987–90. [DOI] [PubMed] [Google Scholar]
- 48.Ströhle A, Stoy M, Wrase J, et al. Reward anticipation and outcomes in adult males with attention-deficit/hyperactivity disorder. Neuroimage 2008;39:966–72. [DOI] [PubMed] [Google Scholar]
- 49.Plichta MM, Vasic N, Wolf RC, et al. Neural hyporesponsiveness and hyperresponsiveness during immediate and delayed reward processing in adult attention-deficit/hyperactivity disorder. Biol Psychiatry 2009;65:7–14. [DOI] [PubMed] [Google Scholar]
- 50.Scheres A, Milham MP, Knutson B, Castellanos FX. Ventral striatal hyporesponsiveness during reward anticipation in attention-deficit/hyperactivity disorder. Biol Psychiatry 2007;61:720–4. [DOI] [PubMed] [Google Scholar]
- 51.Yau WY, Zubieta JK, Weiland BJ, Samudra PG, Zucker RA, Heitzeg MM. Nucleus accumbens response to incentive stimuli anticipation in children of alcoholics: relationships with precursive behavioral risk and lifetime alcohol use. J Neurosci 2012;32:2544–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rhee SH, Waldman ID. Genetic and environmental influences on antisocial behavior: a meta-analysis of twin and adoption studies. Psychol Bull 2002; 128:490–529. [PubMed] [Google Scholar]
- 53.Viding E, Blair RJ, Moffitt TE, Plomin R. Evidence for substantial genetic risk for psychopathy in 7-year-olds. J Child Psychol Psychiatry 2005;46:592–7. [DOI] [PubMed] [Google Scholar]
- 54.Lau JY, Hilbert K, Goodman R, et al. Investigating the genetic and environmental bases of biases in threat recognition and avoidance in children with anxiety problems. Biol Mood Anxiety Disord 2012;2:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Heinz AJ, Beck A, Meyer-Lindenberg A, Sterzer P, Heinz A. Cognitive and neurobiological mechanisms of alcohol-related aggression. Nat Rev Neurosci 2011; 12:400–13. [DOI] [PubMed] [Google Scholar]
- 56.Workman JL, Fonken LK, Gusfa J, Kassouf KM, Nelson RJ. Post-weaning environmental enrichment alters affective responses and interacts with behavioral testing to alter nNOS immunoreactivity. Pharmacol Biochem Behav 2011;100:25–32. [DOI] [PubMed] [Google Scholar]
- 57.Isaacs EB, Gadian DG, Sabatini S, et al. The effect of early human diet on caudate volumes and IQ. Pediatr Res 2008; 63:308–14. [DOI] [PubMed] [Google Scholar]
- 58.Seidel K, Poeggel G, Holetschka R, Helmeke C, Braun K. Paternal deprivation affects the development of corticotrophin-releasing factor-expressing neurones in prefrontal cortex, amygdala and hippocampus of the biparental Octodon degus. J Neuroendocrinol 2011;23:1166–76. [DOI] [PubMed] [Google Scholar]
- 59.Wootton JM, Frick PJ, Shelton KK, Silverthorn P. Ineffective parenting and childhood conduct problems: the moderating role of callous-unemotional traits. J Consult Clin Psychol 1997;65:301–8. [DOI] [PubMed] [Google Scholar]
- 60.McCrory EJ, De Brito SA, Sebastian CL, et al. Heightened neural reactivity to threat in child victims of family violence. Curr Biol 2011;21:R947–R498. [DOI] [PubMed] [Google Scholar]
- 61.Tottenham N, Hare TA, Millner A, Gilhooly T, Zevin JD, Casey BJ. Elevated amygdala response to faces following early deprivation. Dev Sci 2011;14:190–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McLaughlin KA, Greif Green J, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Arch Gen Psychiatry 2012;69:1151–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brotman LM, Gouley KK, Huang KY, Kamboukos D, Fratto C, Pine DS. Effects of a psychosocial family-based preventive intervention on cortisol response to a social challenge in preschoolers at high risk for antisocial behavior. Arch Gen Psychiatry 2007;64:1172–9. [DOI] [PubMed] [Google Scholar]
- 64.Scott S, Briskman J, O’Connor TG. Early prevention of antisocial personality: long-term follow-up of two randomized controlled trials comparing indicated and selective approaches. Am J Psychiatry 2014;171:649–57. [DOI] [PubMed] [Google Scholar]
- 65.Webster-Stratton C, Reid MJ, Hammond M. Preventing conduct problems, promoting social competence: a parent and teacher training partnership in head start. J Clin Child Psychol 2001;30:283–302. [DOI] [PubMed] [Google Scholar]
- 66.Chamberlain P, Smith DK. Antisocial behavior in children and adolescents: the Oregon Multidimensional Treatment Foster Care model — evidence-based psychotherapies for children and adolescents. New York: Guilford Press, 2003. [Google Scholar]
- 67.Eyberg SM, Nelson MM, Boggs SR. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. J Clin Child Adolesc Psychol 2008;37:215–37. [DOI] [PubMed] [Google Scholar]
- 68.Waschbusch DA, Carrey NJ, Willoughby MT, King S, Andrade BF. Effects of methylphenidate and behavior modification on the social and academic behavior of children with disruptive behavior disorders: the moderating role of callous/ unemotional traits. J Clin Child Adolesc Psychol 2007;36:629–44. [DOI] [PubMed] [Google Scholar]
- 69.Hawes DJ, Dadds MR. The treatment of conduct problems in children with callous-unemotional traits. J Consult Clin Psychol 2005;73:737–41. [DOI] [PubMed] [Google Scholar]
- 70.Findling RL. Atypical antipsychotic treatment of disruptive behavior disorders in children and adolescents. J Clin Psychiatry 2008;69:Suppl 4:9–14. [PubMed] [Google Scholar]
- 71.Burris KD, Molski TF, Xu C, et al. Aripiprazole, a novel antipsychotic, is a high-affinity partial agonist at human dopamine D2 receptors. J Pharmacol Exp Ther 2002;302:381–9. [DOI] [PubMed] [Google Scholar]
- 72.Taylor DM. Aripiprazole: a review of its pharmacology and clinical use. Int J Clin Pract 2003;57:49–54. [PubMed] [Google Scholar]
- 73.Connor DF, Glatt SJ, Lopez ID, Jackson D, Melloni RH Jr. Psychopharmacology and aggression. I: a meta-analysis of stimulant effects on overt/covert aggression-related behaviors in ADHD. J Am Acad Child Adolesc Psychiatry 2002;41: 253–61. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


