Abstract
Introduction:
Excess sodium intake can increase the risk of high blood pressure and cardiovascular disease, common comorbidities for those with type 2 diabetes mellitus (T2DM). The purpose of this study is to describe sodium intake and high sodium food sources among Korean Americans (KAs) with T2DM.
Method:
This study, a descriptive, secondary analysis of baseline data from a clinical trial for diabetes, recruited KAs with T2DM (n = 232) from the community.
Results:
Average dietary sodium intake was 3,433 mg. Major sources of dietary sodium were from bicultural diets: noodles and dumplings, Korean-style soups, kimchi, breads and snacks, and boiled or seasoned vegetables. Participants who consumed excessive sodium were more likely to consume more calories and be male, married, and more recently diagnosed with T2DM.
Discussion:
High consumption of sodium among KAs with T2DM supports the need to develop effective, tailored interventions addressing dietary sodium that incorporates the individual’s culture.
Keywords: food sources, sodium and calorie intake, Korean Americans, type 2 diabetes
Diet modification is a critical component in the prevention of cardiovascular disease (CVD), the leading cause of U.S. deaths (Lichtenstein et al., 2006; Roger et al., 2012). It is well documented that excess sodium intake can lead to high blood pressure (HBP), the primary risk factor for CVD (Jackson, King, Zhao, & Cogswell, 2016). People with type 2 diabetes mellitus (T2DM) are at high risk of developing CVD, and CVD risks are even higher in those with concurrent HBP (Leon & Maddox, 2015; Martín-Timón, Sevillano-Collantes, Segura-Galindo, & Del Cañizo-Gómez, 2014).
High sodium intake is associated with an increased risk of obesity through high energy intake (He & MacGregor, 2010), and high energy intake is related to increased excessive consumption of processed food that is high in both calories and sodium (National Institute for Health and Clinical Excellence, 2015). Although people with diabetes may be concerned about calorie intake, few are likely to recognize the risk of high sodium intake and its consequences, including HBP, hyperinsulinemia (Sharma, Ruland, Spies, & Distler, 1991) and insulin resistance (Poch et al., 2001) in T2DM.
People with diabetes tend to focus on restricting their diet, including low intake of total calories and carbohydrates, in order to manage weight and blood glucose levels. Many immigrants, including Korean Americans (KAs), originate from countries where the prevalence of obesity is lower than it is in the United States (Gordon-Larson, Harris, Ward, & Popkin, 2003), and they are found to be in better health than their U.S.-born counterparts (Frisbie, Cho, & Hummer, 2001). However, compared with Koreans in Korea, KAs have a higher prevalence of overweight and obesity (Cho & Juon, 2006) and report more overweight- and obesity-related illnesses such as HBP, T2DM, and heart disease (S. K. Lee, Sobal, & Frongillo, 2000; Y. J. Song et al., 2004). Yet, KAs often perceive that they are less obese than the majority of the U.S. population (S. K. Lee et al., 2000). The main reason for weight gain in KAs is their high calorie intake from fatty foods and processed foods that also contain high amounts of sodium after immigrating to the United States (S. K. Lee et al., 2000).
There are limited studies about the sodium intake of Asian Americans even though the number of Asian Americans, including KAs, is increasing rapidly in the United States. One noteworthy risk factor among KAs is related to changes in dietary patterns after immigration. Many KAs undergoing acculturation increase their consumption of animal protein, fats, and refined sugar. At the same time, they continue to eat traditional Korean foods, which are high in sodium (e.g., pickled vegetables, soy, and other high-sodium sauces). This bicultural diet combination can be detrimental for people with or at risk for HBP and CVD (Ye, Rust, Baltrus, & Daniels, 2009).
The reported patterns for the major sources of sodium among those in Korea and KAs are similar. Previous studies have repeatedly identified several traditional dishes as the main sources of dietary sodium including kimchi, bean paste soup, salty stews, and spicy noodles (Cross, Kim, Yu, Chen, & Kim, 2002; Park, Murphy, Sharma, & Kolonel, 2005). Although these studies are valuable, there are several gaps in the literature regarding our understanding of the major sources of sodium and calories in the diet for KAs with T2DM and its impact on their clinical outcomes. First, the available data are outdated and KAs’ diets have become more diverse and rapidly change after immigration. Moreover, people with diabetes are more likely to be conscious about their calorie intake and may yield a different pattern of their dietary sodium and calorie intake.
To address this gap in the literature, the amount of dietary sodium and calorie intake for KAs with T2DM, along with the major dietary sources of sodium, need to be assessed. Thus, the purposes of this study were (a) to determine the distribution of daily sodium intake of KAs with T2DM, (b) to identify major sources of dietary sodium in the diets of KAs with T2DM, and (c) to examine the ratio of sodium to calories using the major sources of dietary sodium.
Method
Study Design
This secondary analysis was part of an open-label, randomized controlled trial to assess the effectiveness of a self-help intervention for diabetes management among KAs. The details concerning recruitment, enrollment, and retention have been previously reported (M. T. Kim et al., 2015).
Sample
Eligible participants were self–identified KAs with uncontrolled type 2 diabetes, as verified by HbA1C values of 7.0% (53 mmol/mol) or higher, were between 35 and 80 years of age and were able to speak and read Korean or English. One additional inclusion criterion was added for the present study—participants must have completed a 24-hour dietary recall at the baseline data collection time. A total of 250 KAs were enrolled in the program and randomized into the intervention group (n = 120) or the control group (n = 130) and 232 KAs, who had complete 24-hour dietary recall data, at baseline were used in this analysis. A power analysis was undertaken to determine whether the sample size was enough to detect meaningful changes in the randomized control trial using a conservative effect size of 0.5% reduction in A1C with type 1 error of 0.05 and 90% power. The sample size was 210 subjects (105 subjects per group) (M. T. Kim et al., 2015).
Setting
Participants were recruited in a natural community setting through media campaigns, outreach to places (e.g., ethnic churches, supermarkets, festivals), and referrals by Korean health care providers. Most research activities took place at a community site, the Korean Resource Center, where the community–academic team members worked together to enroll participants, provide interventions, and collect data for a year-long follow-up period (M. T. Kim et al., 2015).
The data were collected at baseline and at 3, 6, 9, and 12 months. For the present study, only the data collected at baseline were used in the analysis. The study proposal was approved by the institutional review board of the primary author’s educational institution.
Measurement
Demographic data included age, gender, education attainment, financially stable, marital status, length of U.S. residency, duration of diagnosed DM, level of health literacy, and health insurance. Anthropometric data encompassed height and body weight, from which the body mass index (BMI) was calculated. The cutoff points for obesity (BMI ⩾ 25 kg/m2) used were those defined by the International Obesity Task Force for adults in the Asian and Pacific regions (World Health Organization, 2000); that is, normal (BMI < 23 kg/m2), overweight (BMI ⩾ 23 and < 25 kg/m2), and obese (BMI ⩾ 25 kg/m2) based on the BMI.
Dietary Data.
A single 24-hour dietary recall was collected from each participant through the in-person interview. Each participant was asked to report all the food, beverages, and supplements that the participant had consumed during the past 24 hours. To enhance data accuracy, each participant was shown three-dimensional food models depicting foods and serving sizes to assist in reporting portion sizes of food intake. The accuracy of data collection was also improved by using contemporary Korean food samples and containers to measure participants’ portion sizes.
Ingredients and nutrients were calculated using a software (Can Pro 4.0) that the Korean Dietetic Association developed and validated (The Korean Nutrition Society, 2012). The 24-hour dietary recall has been reported as a valid and sensitive measure to compare with both urinary excretion of sodium and total energy expenditure of energy intake (calories) (Espeland et al., 2001; De Keyzer et al., 2015; Hagfors, Westerterp, Sköldstam, & Johansson, 2005).
Selected Food Items.
Food groups for this study were based on the system used by Can Pro 4.0, which is similar to the Nutrition Data System Research that analyzes dietary composition. To address the food sources of sodium, foods were grouped into categories based on Korean National Nutrition and Health Examination Survey dietary intake file using Can Pro 4.0. The comparison for sodium amount was based on serving size as determined by the Can Pro 4.0. These food groups were developed by categorizing 1,821 kinds of commonly used Korean foods into 23 food groups described in Table 1.
Table 1.
Food Groups and Food Items by Korean Nutrient Database Can Pro 4.0
| Food group | Food items |
|---|---|
| Rice | Boiled rice, multigrain rice, bibimbap, fried rice, bowl of rice with toppings, sushi |
| Bread and snacks | Breads, donut, muffin, bagel, cake, chips, sandwich, hamburger, pizza, toast, hotdog, taco, cereal |
| Noodles and dumplings | Noodle soup, ramen, vermicelli, Chinese noodle, dumpling, rice-cake soup, pasta |
| Soups and gruel | Cream-soup, mushroom-soup, gruel with pumpkin, red bean, and vegetable |
| Korean-style soups | Clear soup, bean paste soup, beef bone soup, cold soup |
| Stews | Fish and shellfish stew, bean paste stew, vegetable/Kimchi stew, hot pot |
| Roasted meat and fish | Roasted fishes and shellfish, meat, seaweed, tofu and vegetable |
| Korean-style pancake | Korean style pancake with vegetable, fish, meat, and tofu |
| Stir-fried food | Stir-fried with vegetables, fishes, and meats, stir-fried rice cake |
| Food boiled down in soy sauce/other seasonings | Boiled down fishes, meats, vegetables, or tofu in soy sauce or other seasonings |
| Fried food | Fried fishes, meats, or vegetables |
| Boiled or seasoned vegetable | Boiled and seasoned vegetable, seasoned raw vegetable, salad |
| Kimchi | Kimchi (napa cabbage kimchi), kkakduki (cubed radish kimchi)/small radish kimchi, nabak kimchi (watery kimchi with sliced vegetable), other kimchi |
| Sashimi | Sashimi |
| Fermented fish | Salt-fermented fish |
| Pickled vegetable | Pickled vegetables |
| Salt-containing seasoning | Soy sauce, soybean paste, red pepper paste, salty seasonings used during cooking |
| Milk and dairy products | Milk, low-fat milk, cheese, ice cream, yogurt |
| Beverage and alcohol | Beverage, soda, alcohol, tea, coffee |
| Fruits | Fresh fruit, canned fruit, fruit juice |
| Rice cake | Rice cake |
| Single foods | Grain, nuts, fresh vegetable, seaweeds |
| Processed food and other foods | Bacon, ham, beef jerky, canned tuna, canned ham, fish cake |
The contribution of each food group to daily sodium intake was calculated using the following formula: % of sodium from food group = (sum of sodium from food group [mg]/total sum of sodium from all foods [mg]) × 100. The researchers also calculated the contribution of each food group to calorie intake using the same formula: % of calories from food group = (sum of calories from food group [kcal]/total sum of calories from all foods [kcal]) × 100. The dietary sodium to calorie ratio was determined for each food group using the following formula: % of sodium / % of calorie for each food group.
Data Analysis
Data were analyzed using SPSS Windows release 21.0 (IBM Corp, 2013). Descriptive statistics were used to characterize the sample and histograms were generated and used to examine outliers. Five outliers were found with extremely high-sodium intakes and were removed because the values between mean and 5% trimmed mean were relatively large (3600.49 and 3405.34). Independent sample t tests and chi-square tests were conducted to identify statistical differences in demographic characteristics by dietary sodium intake (optimal vs. excessive sodium intake). The differences in food group intake patterns were also analyzed by age group (30-49, 50-64, 65 years and older), gender, and meal type.
Results
Sample Characteristics
The distribution of the sample demographic information is presented in Table 2. There were 135 males (58.2%) and 97 females (41.8%), with an average age of 58.7 years (standard deviation [SD] = 8.4) (range: 35-76 years). The sample had a relatively low level of education (47.7% not having graduated from high school) and the majority of them were married (88.8%). Only one third of the sample reported being financially stable, and all of them were first-generation immigrants who had been in the United States for an average of 24.1 years (SD = 11.2) (range: 1.3-53 years). On average, they were aware of having diabetes for 7.9 years (SD = 7.2), with a range of 0 to 35 years. The majority of participants exhibited limited health literacy (83.7%) and did not have health insurance (47.8%).
Table 2.
Comparison of the Optimal and Excessive Sodium Group in Korean Americans With Type 2 Diabetes (N = 227).
| Indicators | n (%)/M (SD) | Range | Optimal group (I)(n = 74) | Excessive group (2) (n = 153) | Difference (1 – 2) | p value |
|---|---|---|---|---|---|---|
| Demographic information | ||||||
| Age, years | 58.7 (8.4) | 35-76 | 59.2 (8.1) | 58.6 (8.7) | 0.6 (1.2) | .600 |
| Male | 135 (58.2) | 35 (26.7%) | 96 (73.3%) | −46.6% | .027 | |
| Education level | ||||||
| Less than high school | 110 (47.7) | 39 (36.1%) | 69 (63.9%) | −27.8% | .282 | |
| High school or greater | 122 (52.3) | 35 (29.4%) | 84 (70.6%) | −41.2% | ||
| Financially stable | 82 (36.3) | 24 (29.3%) | 58 (70.7%) | −41.4% | .401 | |
| Married | 206 (88.8) | 60 (29.9%) | 141 (70.1%) | −40.2% | .014 | |
| The length of stay in the United States, years | 24.1 (11.2) | 1.3-53 | 25.5 (10.3) | 23.5 (1 1.7) | 2.0 (1.6) | .207 |
| Duration of diagnosed DM, years | 7.9 (7.2) | 0-35 | 9.4 (8.0) | 7.1 (6.6) | 2.3 (1.0) | .026 |
| Limited health literacy | 190 (83.7) | 0-6 | 61 (32.1) | 129 (67.9) | −35.8% | .719 |
| No health insurance | 108 (47.6) | 36 (33.3%) | 72 (66.7%) | −33.4% | .822 | |
| BMI, kg/m2 | 25.4 (0.2) | 17.7-35.7 | 25.6 (3.2) | 25.4 (3.1) | 0.18 (0.4) | .692 |
| Dietary intake | n(%)/M (SD) | Median (IQR) | Optimal Group (I)(n = 74) | Excessive Group (2) (n = 153) | Difference (1 – 2) | p value |
| Calorie status and level (kcal/day) | ||||||
| Malesa | 1933.0 (697.4) | 1823.9 (974.6) | 1471.9 (541.9) | 2069.2 (673.9) | −597.3 (126.7) | <.001 |
| Femalesb | 1510.1 (566.2) | 1481.5 (742.5) | 1239.0 (496.9) | 1690.3 (544.1) | −451.3 (107.4) | <.001 |
Note. BMI = body mass index; DM, diabetes mellitus; M = mean; SD = standard deviation; IQR = interquartile range. Optimal group: sodium ⩽2,300 mg/day; Excessive group: >2,300 mg/day. Values in boldface indicate statistical significance (p < .05).
n (Optimal) = 35, n (Excessive) = 96.
n (Optimal) = 39, n (Excessive) = 57.
Characteristics of Dietary Sodium and Calorie Intake
The average daily sodium intake of 227 KAs with T2DM was 3433.4 mg (SD = 1963.9; range: 492.5-9400.2). The majority (67.4%) of the KAs with T2DM in this sample consumed more dietary sodium than the recommended sodium intake of 2,300 mg per day (American Diabetes Association, 2017; American Heart Association, 2015). The average daily energy intake (calories) was 1933.0 kcal (SD = 697.4; Mdn = 1823.9; interquartile range = 974.6) for males and 1510.1 kcal (SD = 566.2; Mdn = 1481.5; interquartile range = 742.5) for females (Table 2).
For the comparison of the optimal and excessive sodium group, there were significant differences by gender (χ2 = 4.88, p < .05); marital status (χ2 = 6.03, p < .05); duration of diagnosed T2DM, t(225) = 2.25, p < .05. There were also significant differences in calorie intake for both males and females, t(129) = −522, p < .001; t(94) = −4.20, p < .001.
Major Sources of Dietary Sodium and Calorie Intake
Table 1 demonstrates the ranked food group contributing high sodium and calorie intake and how different foods contributed as a percentage of the total sodium intake to the overall dietary sodium to KAs with T2DM.
The top five food sources of sodium are noodles and dumplings, Korean-style soups, kimchi, breads and snacks, and boiled or seasoned vegetable, which accounted for 57.7% of the total sodium intake of the KAs with T2DM in this study. Across all age groups and gender, the greatest contributor to sodium intake was noodles and dumplings, which accounted for 15.14% of the sample’s intake. Other major sources, which contributed to more than 10% of intake, were Korean-style soups (12.75%), kimchi (12.14%), and breads and snacks (10.28%). Among the top-ranked food groups, noodles and dumplings, noodle soup and ramen contained the highest amounts of sodium (56912.52 mg; 50467.44 mg). The combination of Korean traditional diet (noodles and dumplings, Korean-style soups, and kimchi) and Western diet (breads and snacks) represent a bicultural diet contributing to high sodium intake of KAs with T2DM.
There were significant differences based on gender for the amount of noodles and dumplings (t = 2.40, p < .05) and breads and snacks (t = 2.06, p < .05) consumed. Males consumed significantly higher amounts of sodium from noodles and dumplings and breads and snacks. Sodium intake from consuming breads and snacks was significantly lower in older age groups (F = 2.85, p < .05). There were expected differences in sodium intake of food groups by meal type. For example, the top sodium food groups (i.e., noodles and dumplings and Korean-style soups) were not significantly different during the main meals of breakfast, lunch, or dinner. On the other hand, the breads and snacks food group was the top-ranked sodium food group in both morning snack and evening snacks (F = 3.53, p < .01).
The amount of calories that the top five sodium foods contributed to total calorie intake included: noodles and dumplings (14.17%), Korean-style soups (3.51%), kimchi (0.26%), breads and snacks (13.57%), and boiled or seasoned vegetable (1.43%;) (see Table 3). Other major food sources that contributed the greatest to total calorie intake were rice (9.03%; third ranked), soups and gruel (8.1%; fourth ranked), and fried food (6.89%; fifth ranked).
Table 3.
Ranked Food Group and Subfood Group Contributing to Sodium and Calorie Intake in KAs With T2DM.
| Rank | Food Group (Total amount of sodium, contribution to sodium intake) | Subfood Group (Amount of sodium, mg) | Total amount of calories (kcal) | Contribution to calorie intake (%) | Sodium/Calorie ratio |
|---|---|---|---|---|---|
| 1 | Noodles and dumplings (133069.40 mg, 15.14%) | • Noodle soup (56912.52) • Ramen (50467.44) • Chinese noodle (9621.14) • Dumpling (9160.41) • Buckwheat vermicelli (5287.94) • Pasta (1619.90) |
46843.87 | 14.17 | 1.1 |
| 2 | Korean-style soups (112041.34 mg, 12.75%) | • Clear soup (52117.49) • Bean paste soup (29432.88) • Beef bone soup (19896.36) • Cold soup (10594.62) |
18625.05 | 3.51 | 3.6 |
| 3 | Kimchi (106687.38 mg, 12.14%) | 2497.28 | 0.26 | 49.0 | |
| 4 | Bread and snacks (90371.76 mg, 10.28%) | • Sandwich, hamburger (31427.28) • Bread, donut, muffin, bagel, cake (19744.57) • Pizza (13970.35) • Cereal (9657.76) • Toast, hotdog, burrito and taco (8917.98) • Chips (6626.83) |
56501.08 | 13.57 | 0.8 |
| 5 | Boiled or seasoned vegetable (64741.34 mg, 7.37%) | • Seasoned boiled vegetable (31786.25) • Seasoned raw vegetable (20176.94) • Salad with dressing (7865.46) |
10446.68 | 1.43 | 5.2 |
Note. KAs = Korean Americans; T2DM = type 2 diabetes mellitus.
Dietary Sodium-Calorie Ratio
The order of contribution of sodium and calorie was not consistent (Figure 1). Among the top five ranked sodium source food groups, noodles and dumplings (14.17%) had the highest contribution to daily calorie intake as well. On the other hand, kimchi had only 0.26% contribution to daily calorie intake, moreover, the ratio of sodium and calorie was 49.0, which means kimchi contains much higher sodium compared with calories. There were two food groups, noodles and dumplings (sodium/calorie 1.1) and breads and snacks (sodium/calorie 0.8), which had similar contribution ratio between sodium and calorie intake.
Figure 1.
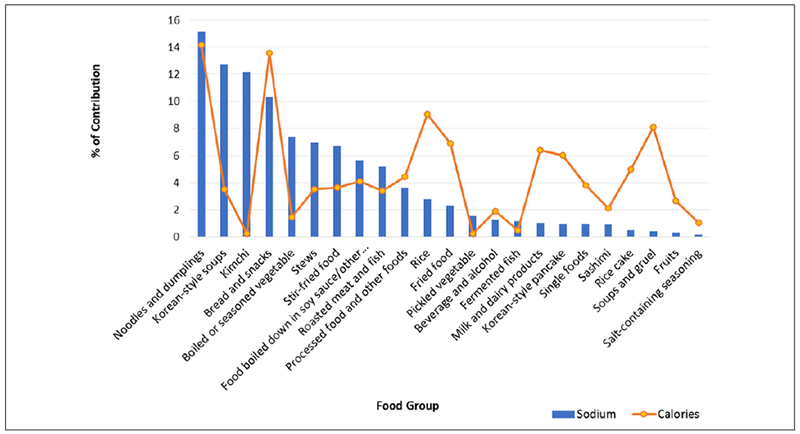
Contribution to daily sodium and calorie intake by food group in Korean Americans with type 2 diabetes mellitus.
Discussion
Excessive dietary sodium intake is a major health risk in KAs, especially those diagnosed with diabetes, in terms of having a higher prevalence of high blood pressure, cardiovascular disease, and chronic kidney disease (Provenzano, Stark, Steenkiste, Piraino, & Sevick, 2014). The present study supports and extends the concern over high sodium intake. The mean daily sodium intake of KAs with T2DM was 3,433.4 mg. The majority of the sample (67.4%) exceeded the recommendation of the American Diabetes Association (e.g., 2,300 mg per day). Recent studies that reported sodium intake showed that mean sodium intake in individuals with T2DM ranged from 3,214 to 3,910 mg per day, similar to the findings of this study, but still higher than recommended, which is 2,300 mg per day (Ekinci et al., 2010; Provenzano et al., 2014).
The daily sodium intake reported in this study was lower than the daily sodium intake reported for the Korean general population (Park et al., 2005; Yon et al., 2011). Yon et al. (2011) found that the daily sodium intake for Koreans aged 12 to 65 years was 4,600 mg. Park et al. (2005) reported that Korea-born KA females’ sodium intake was 3,378 mg, which is slightly greater amount than of KA females (2989.1 mg) in the current study. In comparison with the sodium intake of other ethnic groups, African Americans had the lowest average daily sodium intake (3,475 mg) while Whites had the highest average daily sodium intake (3,702 mg) (U.S. Department of Health and Human Services, 2010). In summary, the average daily sodium intake of KAs with T2DM for this study was relatively lower than the general population in various ethnic groups (except African Americans) but still exceeded the recommendations.
The guidelines for individual calorie intake vary depending on body size and physical activity level. Based on the 2015-2020 U.S. Dietary Guidelines, the general estimates of recommended calorie intake for males are 2,200 kcal and 1,600 kcal for females (U.S. Department of Agriculture, 2015). In this study, the average daily energy intake (calories) for males was 1933.03 kcal (SD = 697.44) and for females was 1510.09 kcal (SD = 566.15). Among males, 32.6% of participants consumed more calories than recommended (2,200 kcal). The total calorie intake in KAs for this study was higher than a previous study for KA elderly (1756.2 ± 677.6 kcal vs. 1520.5 ± 36.0 kcal) (Y. H. Lee, Lee, Kim, & Han, 2009).
Across all age groups, gender, BMI, and acculturation, the top five major contributors to sodium intake were noodles and dumplings (15.14%), Korean-style soups (12.75%), kimchi (12.14%), breads and snacks (10.28%), and boiled or seasoned vegetable (7.37%). The combination of Korean traditional diet (noodles and dumplings, Korean-style soups, and kimchi) and Western diet (breads and snacks) represents a bicultural diet contributing to high sodium intake of KAs with T2DM. KAs with T2DM showed not only similarities but also differences in sodium food sources from native Koreans. Compared with a previous study which evaluated trends and identified sodium sources for Koreans using Korean National Nutrition and Health Examination Survey data from 1998 to 2010 (D. Y. Song, Park, Shim, & Lee, 2013), the major food groups contributing to dietary sodium intake were kimchi (22.8%-31.7%), noodles and dumplings (10.5%-13.8%), soups (10.2%-13.8%), and stews (8.5%-11.2%). KAs still eat Korean traditional foods as their top three major sodium sources but the contribution of each food group was a little lower than Koreans in Korea. Additionally, KAs consumed breads and snacks (e.g., sandwiches, hamburgers) as a fourth major sodium source, and breads and snacks were often eaten as morning or evening snacks and breakfast among younger KAs. The researchers found statistically significant differences in sources of sodium intake among demographic subgroups. Most notable is that although a great amount of sodium is consumed through major dishes, there were differences among gender and age groups. Whether there are significant differences according to taste preference and meal frequency warrants further investigation.
Until now, Korean traditional foods have been considered as high sodium containing foods, and KAs’ tendency to maintain their traditional diet after immigration has been noted as the main reason for the high sodium intake in their diet (Cross et al., 2002; Kwon, Shim, Park, & Paik, 2009). However, a bicultural diet that includes both Korean and Western foods more accurately explains KAs’ high sodium intake. It is of note that this bicultural diet was found in KAs, who were first-generation and middle-aged adults in this study. A common assumption is that acculturation and, accordingly, diet change would occur with greater length of U.S. residence after immigration. A longitudinal study provided evidence that acculturation increases with the length of U.S. residence and is accompanied by dietary changes (Tseng, Wright, & Fang, 2015). However, the same study showed that these changes were not large enough to have a clear health impact. Therefore, factors besides acculturation or length of U.S. residence as a proxy of acculturation that affect dietary changes and health in first generation KA immigrants warrant further investigation. In addition, it will be beneficial to provide nutritional education focusing on healthier bicultural dietary practices for more acculturated first generation KAs with T2DM.
Interestingly, the contributions to the total daily calorie intake for each top sodium food group are not always high. Similarly, the ratios of sodium to calorie intake among top-five ranked sodium source food groups in this study provided valuable information regarding diet patterns of high sodium and calorie intake among KAs. Among the top-five ranked sodium source food groups, noodles and dumplings (14.17%), which represents the main dish containing a high portion of carbohydrates, and breads and snacks, which represents the Western diet (13.57%), had the top two contributions to daily calorie intake. On the other hand, kimchi had only 0.26% contribution to daily calorie intake, moreover, the ratio of sodium to calories was 49.0, which means kimchi contains much higher sodium compared with calories. Among the top-five ranked food groups, the total contribution of sodium and calorie intake in Korean traditional foods versus Western foods provided meaningful information. For sodium intake, Korean traditional foods (noodles and dumplings, Korean-style soups, kimchi, and boiled or seasoned vegetable) totaled 47.40% of the contribution, while Western foods (breads and snacks including sandwiches, hamburgers, bread, pizza, cereal, toast, hotdogs, burritos, and chips) had 10.28% of contribution. In calorie intake, Korean traditional foods had only 19.37% of the contribution, but Western foods, breads and snacks alone had 13.57% of contribution. Based on these findings, KAs may consume the same amount of high sodium by eating fewer calories from high-sodium items (e.g., kimchi, Korean-style soups, and boiled/seasoned vegetable) or by eating moderate to large amounts of calories from medium or low sodium items simultaneously.
Another notable finding was that there were two kinds of food groups that are noteworthy for this population that had highest contributions of both sodium and calories and also represent bicultural diet: noodles and dumplings (15.14% of sodium and 14.17% of calories) and breads and snacks (10.28% of sodium and 13.57% of calories). These food groups may influence not only the sodium level but also the level of blood glucose in people with diabetes due to having a high portion of carbohydrates. KAs with T2DM, who may recognize that Korean traditional foods contain relatively lower levels of calories, might be surprised at their high sodium levels (Kim, Lee, Ahn, Bowen, & Lee, 2007). In reality, the ratio of sodium to calories in Korean traditional foods ranked as the top-five major sodium sources and were considerably higher than other food groups: Korean-style soups (3.6), kimchi (49.0), and boiled or seasoned vegetable (5.2; Table 3). These foods seem like healthy foods and contain relatively lower calories when compared with Western foods, but they can boost sodium consumption. Alderman, Cohen, and Madhavan (1998) reported with National Nutrition and Health Examination Survey data that not only sodium intake but also the sodium to calorie ratio were directly associated with CVD mortality and all-cause mortality. Because there was a strong correlation of sodium with energy intake, both sodium alone and the sodium concentration in the diet may be needed to explain variations in health outcomes in KAs with chronic disease.
Limitations
A limitation of this study was the use of a single 24-hour dietary recall to assess the level of sodium and calorie intake, which may result in underestimation of food intake. It is hard to identify the variations between foods eaten on weekends versus weekdays with only one day of intake. Also, measures based on self-report can be affected by the inaccurate recall of past events (Gibson, 1990). However, despite these limitations, the data provides an important snapshot into the dietary intake of this population which has been understudied. Second, the generalizability of the study findings is limited to KAs with T2D in this sample due to the lack of probability sampling. This sample may not represent the population of KAs with T2DM across the United States. Thus, generalizing the findings of this study should be done with caution.
Implications
This study has several implications for nursing practice. Nurses need to be aware that patients with T2DM may be consuming high amounts of sodium in their diet. Current patient education on the diet for T2DM self-management emphasizes restriction of calories and carbohydrates. However, reduction in the high consumption of sodium may also need to be emphasized in dietary education to reduce the risk of high blood pressure, especially in KAs with T2DM whose bicultural diet is likely contributing to high sodium consumption.
Furthermore, nurses may play a pivotal role in developing culturally sensitive dietary self-management programs and facilitating patients self-management of dietary intake skills in multiple heath care settings. For nurses caring for patients with T2DM who come from diverse backgrounds, it is essential to avoid stereotyping and thinking that a “one size fits all” approach will work for all members of any ethnic or minority group. Every component of dietary self-management should be patient centered, modified and designed with patients to reflect their cutural values. In addition, nurses can help people with T2DM to understand how sodium intake can affect potential health complications such as HBP and kidney disease along with guidance on how to implement their personalized dietary recommendations.
Examples of practical strategies that nurses can use with the KA population may include recommending modifications of Korean contemporary food recipes to reduce salt content that subsequently reduces sodium intake. Many KAs consider soups and stews comfort food, and they drink the broth, which increases sodium intake. To help reduce the sodium in the soup, one can make their own soup with low amounts of salt or use no-salt added or reduced-sodium broths. People can also reduce the volume of broth consumed by using a smaller bowl, and they can adjust the ingredients in the soup, adding more vegetables and tofu for flavor and less room for high sodium broth.
Conclusion
In conclusion, this secondary descriptive study on assessing dietary sodium intake and major food sources of sodium consumption in KAs with T2DM showed that excessive sodium intake was problematic in this sample and that bicultural diets contributed to their high consumption of sodium. In addition, two major types of foods (i.e., noodles and dumplings, breads and snacks) containing high amounts of sodium also contained high amounts of calories, which may affect glucose control in people with diabetes. Despite years of clinical trials and scientific evidence to reduce the burden of CVD, many people having diabetes still do not comply with their dietary recommendations. Moreover, immigrants remain more likely than the U.S.-born populations to be unaware of their risk factors for CVD (Langellier et al., 2012). An approach reflecting their own culture has been not used for dietary self-management to deal with high-risk dietary habits and foods. This study contributes to our understanding about the sodium consumption and its food sources for the KA population with T2DM. This knowledge is necessary to develop interventions that can be culturally tailored. Future study developing culturally sensitive, efficient, and effective dietary programs for immigrant populations are warranted.
Acknowledgments
This study used a secondary data analysis from a randomized clinical trial with community-dwelling Korean American immigrants diagnosed with type 2 diabetes (NCT01264796).
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was partially supported by the Technology Innovation Program (or Industrial Strategic Technology Development Program (10053704, Development of Smart Healthcare System and Pilot Project for Military Personnel and Global Healthcare) funded By the Ministry of Trade, Industry & Energy (MOTIE, Korea).
Footnotes
The research protocol was approved by the Johns Hopkins Medical Institutions Institutional Review Board and written consent was obtained from all study participants.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- American Diabetes Association. (2017). Standards of Medical Care in Diabetes-2017. Retrieved from http://care.diabetesjournals.org/content/diacare/suppl/2016/12/15/40.Supplement_1.DC1/DC_40_S1_final.pdf
- American Heart Association. (2015). The American Heart Association’s diet and lifestyle recommendations. Retrieved from http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/HealthyDietGoals/Dictionary-of-Nutrition_UCM_305855_Article.jsp
- Alderman MH, Cohen H, & Madhavan S (1998). Dietary sodium intake and mortality: The National Health and Nutrition Examination Survey (NHANES 1). Lancet, 351, 781–785. [DOI] [PubMed] [Google Scholar]
- Cho J, & Juon HS (2006). Assessing overweight and obesity risk among Korean Americans in California using World Health Organization body mass index criteria for Asians. Preventing Chronic Disease, 3, A79. [PMC free article] [PubMed] [Google Scholar]
- Cross NA, Kim KK, Yu ESH, Chen EH, & Kim J (2002). Assessment of the diet quality of middle-aged and older adult Korean Americans living in Chicago. Journal of the American Dietetic Association, 102, 552–554. [DOI] [PubMed] [Google Scholar]
- De Keyzer W, Dofková M, Lillegaard IT, De Maeyer M, Andersen LF, Ruprich J, … Huybrechts I (2015). Reporting accuracy of population dietary sodium intake using duplicate 24 h dietary recalls and a salt questionnaire. British Journal of Nutrition, 113, 488–497. [DOI] [PubMed] [Google Scholar]
- Ekinci EI, Cheong KY, Dobson M, Premaratne E, Finch S, MacIsaac RJ, & Jerums G (2010). High sodium and low potassium intake in patients with type 2 diabetes. Diabetic Medicine, 19, 1401–1408. [DOI] [PubMed] [Google Scholar]
- Espeland MA, Kumanyika S, Wilson AC, Reboussin DM, Easter L, Self M, … McFarlane M (2001). Statistical issues in analyzing 24-hour dietary recall and 24-hour urine collection data for sodium and potassium intakes. American Journal of Epidemiology, 153, 996–1006. [DOI] [PubMed] [Google Scholar]
- Frisbie WP, Cho Y, & Hummer RA (2001). Immigration and the health of Asian and Pacific Islander adults in the United States. American Journal of Epidemiology, 153, 372–380. doi: 10.1093/aje/153.4.372 [DOI] [PubMed] [Google Scholar]
- Gibson RS (1990). Principles of nutritional assessment. New York, NY: Oxford University Press. [Google Scholar]
- Gordon-Larson P, Harris KM, Ward DS, & Popkin BM (2003). Acculturation and overweight-related behaviors among Hispanic immigrants to the US: The National Longitudinal Study of Adolescent Health. Social Science & Medicine, 57, 2023–2034. [DOI] [PubMed] [Google Scholar]
- Hagfors L, Westerterp K, Sköldstam L, & Johansson G (2005). Validity of reported energy expenditure and reported intake of energy, protein, sodium and potassium in rheumatoid arthritis patients in a dietary intervention study. European Journal of Clinical Nutrition, 59, 238–245. [DOI] [PubMed] [Google Scholar]
- He FJ, & MacGregor GA (2010). Reducing population salt intake worldwide: From evidence to implementation. Progress in Cardiovascular Diseases, 52, 363–382. [DOI] [PubMed] [Google Scholar]
- IBM Corp. (2013). IBM SPSS Statistics for Windows, Version 22.0 [Computer software]. Armonk, NY: Author. [Google Scholar]
- Jackson SL, King SM, Zhao L, & Cogswell ME (2016). Prevalence of excess sodium intake in the United States—NHANES, 2009-2012. MMWR Morbidity and Mortality Weekly Report, 64, 1393–1397. [DOI] [PubMed] [Google Scholar]
- Kim MJ, Lee SJ, Ahn YH, Bowen P, & Lee HK (2007). Dietary acculturation and diet quality of hypertensive Korean Americans. Journal of Advanced Nursing, 58, 436–445. [DOI] [PubMed] [Google Scholar]
- Kim MT, Kim KB, Huh B, Nguyen T, Han HR, Bone LR, & Levine D (2015). The effect of a community-based self-help intervention: Korean Americans with type 2 diabetes. American Journal of Preventive Medicine, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Korean Nutrition Society. (2012). Computer Aided Nutritional Analysis Program version 4.0. Seoul, South Korea: Author. [Google Scholar]
- Kwon JH, Shim JE, Park MK, & Paik HY (2009). Evaluation of fruits and vegetables intake for prevention of chronic disease in Korean adults aged 30 years and over: Using the third Korea National Health and Nutrition Examination Survey (KNHANES III), 2005. Korean Journal of Nutrition, 42, 146–157. [Google Scholar]
- Langellier BA, Garza JR, Glik D, Prelip ML, Brookmeyer R, Roberts CK, … Ortega AN (2012). Immigration disparities in cardiovascular disease risk factor awareness. Journal of Immigrant and Minority Health, 14, 918–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SK, Sobal J, & Frongillo EA (2000). Acculturation and health in Korean Americans. Social Science & Medicine, 51, 159–173. [DOI] [PubMed] [Google Scholar]
- Lee YH, Lee J, Kim MT, & Han H-R (2009). In-depth assessment of the nutritional status of Korean American elderly. Geriatric Nursing, 30, 304–311. doi: 10.1016/j.gerinurse.2009.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon BM, & Maddox TM (2015). Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World Journal of Diabetes, 6, 1246–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, … Wylie-Rosett J (2006). Summary of American Heart Association diet and lifestyle recommendations revision 2006. Arteriosclerosis, Thrombosis, and Vascular Biology, 26, 2186–2191. [DOI] [PubMed] [Google Scholar]
- Martín-Timón I, Sevillano-Collantes C, Segura-Galindo A, & Del Cañizo-Gómez FJ (2014). Type 2 diabetes and cardiovascular disease: Have all risk factors the same strength? World Journal of Diabetes, 5, 440–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence. (2015). Obesity: The prevention, identification, assessment and management of overweight and obesity in adults and children. Retrieved from http://www.nice.org.uk/guidance/cg189/resources/guidanceobesity-identificationassessment-and-management-of-overweight-and-obesity-in-children-young-people-andadults-pdf [PubMed]
- Park SY, Murphy SP, Sharma S, & Kolonel LN (2005). Dietary intakes and health-related behaviors of Korean American women born in the USA and Korea: The Multiethnic Cohort Study. Public Health Nutrition, 8, 904–911. doi: 10.1079/PHN2005740 [DOI] [PubMed] [Google Scholar]
- Poch E, González D, Giner V, Bragulat E, Coca A, & de la Sierra A (2001). Molecular basis of salt sensitivity in human hypertension evaluation of renin-angiotensin-aldosterone system gene polymorphisms. Hypertension, 38, 1204–1209. doi: 10.1161/hy1101.099479 [DOI] [PubMed] [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, … Turner MB (2012). Heart disease and stroke statistics—2012 update: A report from the American Heart Association. Circulation, 125(1), e2–e220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Provenzano LF, Stark S, Steenkiste A, Piraino B, & Sevick MA (2014). Dietary sodium intake in type 2 diabetes. Clinical Diabetes, 32, 106–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma AM, Ruland K, Spies K-P, & Distler A (1991). Salt sensitivity in young normotensive subjects is associated with a hyperinsulinemic response to oral glucose. Journal of Hypertension, 9, 329–335. [DOI] [PubMed] [Google Scholar]
- Song DY, Park JE, Shim JE, & Lee JE (2013). Trends in the major dish groups and food groups contributing to sodium intake in the Korea National Health and Nutrition Examination Survey 1998—2010. Korean Journal of Nutrition, 46(1), 72–85. [Google Scholar]
- Song YJ, Hofstetter CR, Hovell MF, Paik HY, Park HR, Lee J, & Irvin V (2004). Acculturation and health risk behaviors among Californians of Korean descent. Preventive Medicine, 39(1), 147–156. [DOI] [PubMed] [Google Scholar]
- Tseng M, Wright DJ, & Fang CY (2015). Acculturation and dietary change among Chinese immigrant women in the United States. Journal of Immigrant and Minority Health, 17, 400–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Agriculture. (2015). 2015-2020 Dietary guidelines for Americans. Retrieved from https://health.gov/dietaryguidelines/2015/
- U.S. Department of Health and Human Services. (2010). Healthy people 2020. Retrieved from http://www.healthypeople.gov/2020/
- World Health Organization. (2000). The Asia-Pacific perspective: Redefining obesity and its treatment. Brisbane, Queensland, Australia: International Obesity Task Force, Health Communications Australia. [Google Scholar]
- Ye J, Rust G, Baltrus P, & Daniels E (2009). Cardiovascular risk factors among Asian Americans: Results from a national health survey. Annals of Epidemiology, 19, 718–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yon M, Lee Y, Kim D, Lee J, Koh E, Nam E, … Kim C (2011). Major sources of sodium intake of the Korean population at prepared dish level—based on the KNHANES 2008–2009. Korean Journal of Community Nutrition, 16, 473–487. [Google Scholar]


