Abstract
Mediastinal Mullerian cyst was first reported by Hattori in 2005. We report a case of a posterior mediastinal paravertebral cyst found incidentally by surveillance chest roentgenogram in a 44-year-old woman. She had a “no drain” uniportal thoracoscopic removal procedure, and histologic examination showed single layer of columnar epithelial lining that stained positive for estrogen receptors (ER), progesterone receptors (PR), paired box gene 8 (PAX8), and Wilms’ tumor protein 1 (WT-1), confirming the diagnosis of mediastinal Mullerian cyst.
Keywords: Mediastinal, Mullerian cyst, uniportal video-assisted thoracoscopic surgery (uniportal VATS)
Introduction
The first mediastinal Mullerian cyst was described by Hattori in 2005 (1). Since then several similar cases of mediastinal cyst with a feature characteristic of a Mullerian cyst have been reported in the literature (2-7). Radiographically it can be misdiagnosed as a bronchogenic cyst or a neurogenic tumor and pathologically it can be misclassified as bronchogenic or unspecified benign serous cysts. Now mediastinal Mullerian cyst is recognized as a type of mediastinal cyst with distinctive biological features. Here we present a case of posterior mediastinal paravertebral cyst in a 44-year-old woman with a history of hysterectomy. Complete resection was done using “no drain” uniportal video-assisted thoracoscopic surgery (VATS). The diagnosis of Mullerian cyst was confirmed with immunohistochemical stains, which showed positive results for estrogen receptor (ER), progesterone receptor (PR), paired box gene 8 (PAX8), and Wilms’ tumor protein 1 (WT-1).
Case presentation
A 44-year-old woman, with a past medical history of hysterectomy for uterine leiomyomas and adenomyosis, was incidentally found to have an intrathoracic lesion on a chest roentgenogram. Subsequent chest computed tomography (CT) confirmed a homogenous soft tissue lesion in the left paravertebral area, which was adjacent to the descending aorta (Figure 1A). Magnetic resonance imaging showed a 1.8 cm × 1.1 cm T1 low-signal and T2 high-signal cystic lesion in the left paravertebral region, with close contact to the descending aorta. The differential diagnosis included bronchogenic cyst and cystic neurogenic tumor. Left side uniportal VATS procedure was arranged to remove the lesion. A single 3-cm incision was made at the fifth intercostal space along the anterior axillary line and protected with a wound retractor (LapShield, Lagis, Taiwan). A cyst-like mass was found at paravertebral area, without invading the descending aorta. Hook electrocautery was used for complete resection. Since there was lung injury or bleeding during the whole procedure, we adopted a “no drain” policy and neither a chest tube or pigtail catheter was placed after the operation. The postoperative recovery was uneventful and there has been no recurrence at two-year follow-up after resection.
Figure 1.
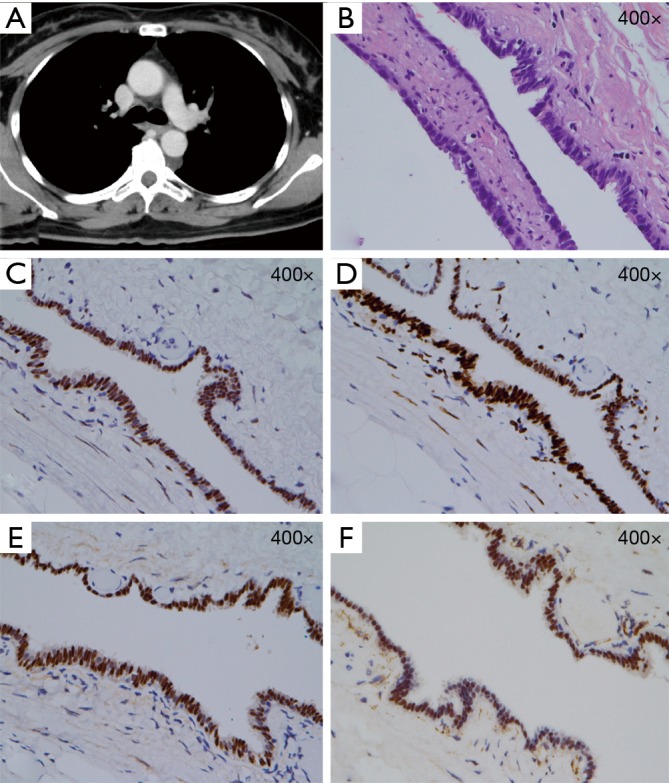
CT and histological results. (A) Chest CT scan revealed a homogenous soft tissue lesion in the left paravertebral area. (B) Hematoxylin-eosin stain. (C,D,E,F) Immunohistochemical stains for estrogen and progesterone receptors, paired box gene 8, and Wilms’ tumor protein 1.
Gross pathologic examination showed a 1.2 cm × 1.2 cm × 0.4 cm pink and yellowish colored soft cystic lesion. Histological examination revealed a single layer of columnar epithelial lining (Figure 1B), which had positive results on immunohistochemical stains for CK, CK7, ER, PR, PAX8, WT-1 (Figures 1C,D,E,F), and negative for CK20, TTF-1, and calretinin. The overall histologic and immunohistochemical findings were compatible with Mullerian cysts.
Discussion
Mediastinal Mullerian cysts may be initially misdiagnosed as bronchogenic cysts or neurogenic tumor radiographically, or misclassified as bronchogenic or unspecified benign serous cysts pathologically. The incidence could be as high as 5.5% in a series of 163 consecutive mediastinal non-neoplastic cysts (2). The patients are frequently with clinical characteristics of (I) women; (II) aged 40 to 60 years; (III) obese and with gynecologic history such as hormone replacement therapy, hysterectomy, and endometrioid carcinoma; (IV) asymptomatic or presenting with nonspecific symptoms such as cough and chest pain, and the locations are always in a posterior mediastinal paravertebral location, from third to eighth thoracic vertebrae levels (2-7). In pathological examination, a Mullerian cyst is lined with a single layer of non-mucinous columnar or cuboidal, and often ciliated, epithelial cells similar with uterine tubal epithelium. The lining epithelium of a Mullerian cyst is positive for CK7, epithelial membrane antigen, ER, PR, PAX8, WT-1, and negative for CK5/6, CK20, calretinin, CD10, and CEA immunohistochemically (2).
It is unknown about the origin of mediastinal Mullerian cyst. Batt described Hattori’s mediastinal cyst as Mullerianosis, which by histologic criteria are lesions containing “admixtures of endosalpingiosis, endometriosis, and endocervicosis” (7,8). Batt refined the clinicopathologic criteria defining Mullerianosis as a heterotopic organoid structure of embryonic origin, a choristoma composed of Mullerian rests: normal endosalpingeal, endometrial, or endocervical tissue mixed within other normal organs during organogenesis (7). Mullerian choristomas can be confidently diagnosed with an increasing number of predetermined tissue types (7). In addition, Batt preferred Ludwig’s theory which means misplaced endosalpingeal epithelium in thoracic location during developmental stages (9). Studying Mayer-Rokitansky-Kuster-Hauser syndrome, which is a malformation of the female genital organs related with interrupted development of the Mullerian ducts, Ludwig described the migration of the Mullerian duct from the third to fifth thoracic blastema into the pelvis and suggested that the Mullerian tissue could be shed during migration (9). This theory not only explains for a cystic structure lined with fallopian tubal epithelium, but also is compatible with the location in the thorax and at the paravertebral space.
Since there have been no reports of recurrence after resection, the clinical behavior of mediastinal Mullerian cysts seems to be benign; however, they should be considered in the differential diagnosis of lesions in posterior mediastinal paravertebral space, especially in middle-aged women with gynecologic history. Various types of surgical resection for mediastinal Mullerian cyst removal have been reported in the literature. Although minimally invasive surgery, such as thoracoscopic or robotic resection, has ever been used (5,6), the concepts of “uniportal VATS” and “no-drain policy” were applied in current case. The uniportal VATS is a modern surgical technique that has been widely accepted in many thoracic procedures and may contribute to an early recovery (10). The “no-drain policy” also has been shown to be safe in selected patients who predicted to be without postoperative air leak and much pleural effusion (11). Our method, uniportal VATS without a chest drain, is associated with the least surgical trauma and has the fastest postoperative recovery. Therefore, it could be recommended for mediastinal Mullerian cyst treatment.
Acknowledgements
None.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Hattori H. Ciliated cyst of probable mullerian origin arising in the posterior mediastinum. Virchows Arch 2005;446:82-4. 10.1007/s00428-004-1087-0 [DOI] [PubMed] [Google Scholar]
- 2.Thomas-de-Montpréville V, Dulmet E. Cysts of the posterior mediastinum showing müllerian differentiation (Hattori's cysts). Ann Diagn Pathol 2007;11:417-20 10.1016/j.anndiagpath.2006.12.011 [DOI] [PubMed] [Google Scholar]
- 3.Businger AP, Frick H, Sailer M, et al. A ciliated cyst in the posterior mediastinum compatible with a paravertebral Mullerian cyst. Eur J Cardiothorac Surg 2008;33:133-6. 10.1016/j.ejcts.2007.09.036 [DOI] [PubMed] [Google Scholar]
- 4.Karpathiou G, Da Cruz V, Patoir A, et al. Mediastinal cyst of müllerian origin: evidence for developmental endosalpingiosis. Pathology 2017;49:83-4. 10.1016/j.pathol.2016.08.017 [DOI] [PubMed] [Google Scholar]
- 5.Chon SH, Im UJ, Song DS. Paravertebral mediastinal Mullerian cyst resected by video assisted thoracoscopic surgery. J Thorac Dis 2015;7:E47-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simmons M, Duckworth LV, Scherer K, et al. Mullerian cysts of the posterior mediastinum: report of two cases and review of the literature. J Thorac Dis 2013;5:E8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Batt RE, Mhawech-Fauceglia P, Odunsi K, et al. Pathogenesis of mediastinal paravertebral müllerian cysts of Hattori: developmental endosalpingiosis-müllerianosis. Int J Gynecol Pathol 2010;29:546-51. 10.1097/PGP.0b013e3181e3640a [DOI] [PubMed] [Google Scholar]
- 8.Young RH, Clement PB. Müllerianosis of the urinary bladder. Mod Pathol 1996;9:731-7. [PubMed] [Google Scholar]
- 9.Ludwig KS. The Mayer-Rokitansky-Küster syndrome. An analysis of its morphology and embryology. Part II: Embryology. Arch Gynecol Obstet 1998;262:27-42. 10.1007/s004040050225 [DOI] [PubMed] [Google Scholar]
- 10.Mineo TC, Ambrogi V. A glance at the history of uniportal video-assisted thoracic surgery. J Vis Surg 2017;3:157. 10.21037/jovs.2017.10.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murakami J, Ueda K, Tanaka T, et al. The Validation of a No-Drain Policy After Thoracoscopic Major Lung Resection. Ann Thorac Surg 2017;104:1005-11. 10.1016/j.athoracsur.2017.03.030 [DOI] [PubMed] [Google Scholar]


