Abstract
A 44‐year‐old man was referred to our hospital after an anterior mediastinal tumor was noted on computed tomography during follow‐up observation after left testicular seminoma resection. Chest computed tomography revealed an enhanced mass measuring 33 x 16 x 15 mm at the anterior mediastinum. Chest magnetic resonance imaging revealed high signal intensity on T2‐weighted imaging, and F18 fluorodeoxyglucose‐positron emission tomography showed a maximum standardized uptake of 12.45. Laboratory tests revealed no elevated tumor markers, except for mildly elevated interleukin‐2. Based on these results, complete resection was performed under suspicion of a malignant tumor, mediastinal metastasis of seminoma, or malignant lymphoma. An extended thymectomy with partial merger pericardial resection was performed using a subxiphoid approach. Small nodules and multiple thymic cysts were observed the thymus in addition to the main mass. Microscopic examination of the tumor revealed fibrosis, lymphocyte infiltration with lymphoid follicular hyperplasia, and hyperplasia of the thymus. Numerous immunoglobulin G4 (IgG4)‐positive plasma cells were found on immunohistochemical staining. The ratio of IgG4 to total IgG was approximately 60%. We ultimately diagnosed the patient with a thymic inflammatory pseudotumor with multilocular cyst caused by IgG4‐related disease.
Keywords: Anterior mediastinal tumor, immunoglobulin G4‐related (IgG4‐ related) disease, thymus
Introduction
Immunoglobulin G4 (IgG4)‐related disease can involve multiple organs, particularly exocrine organs such as the pancreas, salivary glands, and biliary tract.1, 2
When it affects the thorax, it commonly manifests as interstitial lung disease and fibrosing mediastinitis.3, 4, 5, 6, 7 IgG4‐related diseases occurring in the mediastinum are relatively rare, and a confirmed preoperative diagnosis is difficult with imaging modalities, even by a needle or open biopsy.8
Herein, we report a case of thymic inflammatory pseudotumor with multilocular thymic cyst caused by IgG4‐related disease.
Case presentation
A 44‐year‐old man was admitted to our hospital after incidental detection of an anterior mediastinal tumor on chest computed tomography (CT). He had no specific symptoms. He had undergone a left radical inguinal orchiectomy for seminoma and radiation therapy to the para‐aortic lymph nodes six years ago.
All of his basic preoperative laboratory data were normal, including tumor marker levels, except for an elevated level of interleukin‐2 (IL‐2) at 712 U/mL (normal: 145–519 U/mL). As we did not suspect IgG4‐related disease, we did not examine the serum IgG4 level preoperatively. Chest CT revealed a well‐defined homogeneous anterior mediastinal mass in wide contact with the pericardium (Fig 1a) that had not been noted on CT performed six months ago (Fig 1b). Magnetic resonance imaging (MRI) revealed a low signal intensity on T1‐weighted imaging (Fig 2a) and a high signal intensity on T2‐weighted imaging (Fig 2b). F18 fluorodeoxyglucose‐positron emission tomography (FDG‐PET) showed a maximum standardized uptake value of 12.45 (Fig 3). We suspected mediastinal metastasis of the seminoma, malignant lymphoma, thymoma, or thymic hyperplasia. We planned to perform extended thymectomy by video‐assisted thoracic surgery using the subxiphoid approach. The tumor was located in the upper left lobe of the thymus and was difficult to detach from the pericardium; therefore, the pericardium was partially resected. The left phrenic nerve was close to the tumor, but it was preserved. The tumor was macroscopically white‐yellowish with a smooth surface and combined with multilocular cysts (Fig 4a).
Figure 1.
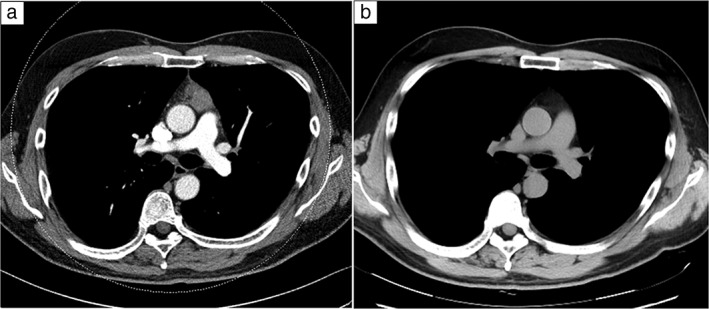
(a) Chest computed tomography (CT) revealed a well‐defined homogeneous anterior mediastinal mass in wide contact with the pericardium that had not been detected on (b) CT six months ago.
Figure 2.
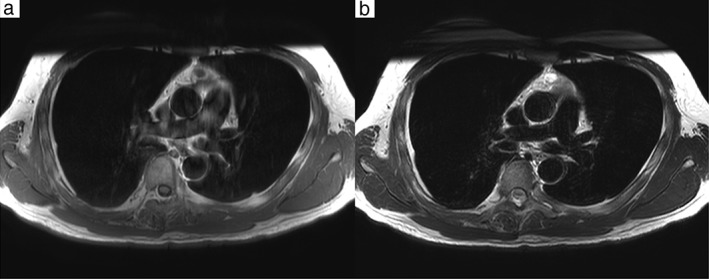
Chest magnetic resonance imaging revealed (a) low signal intensity on T1‐weighted imaging and (b) high signal intensity on T2‐weighted imaging.
Figure 3.

F18 fluorodeoxyglucose‐positron emission tomography showed a high maximum standardized uptake of 12.45 in the anterior mediastinal tumor.
Figure 4.
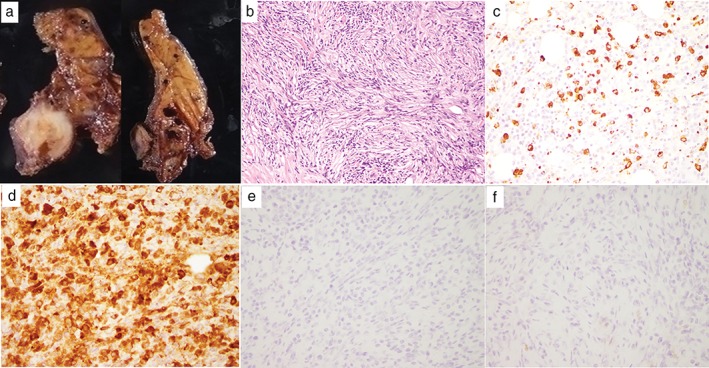
(a) A macroscopic view of the completely resected mass with a smooth surface, combined with multilocular cysts. (b) Lymphoplasmacytic infiltration and storiform fibrosis with lymphoid follicles on hematoxylin and eosin staining. Immunohistochemical staining for (c) immunoglobulin G4 (IgG4) and (d) IgG. The IgG4/IgG‐positive cell ratio was 60%. (e) Placental alkaline phosphatase and (f) c‐kit staining of the tumor were negative.
The final histopathological examination of the tumor revealed lymphoplasmacytic infiltration and storiform fibrosis with lymphoid follicles on hematoxylin and eosin staining (Fig 4b). Obliterative phlebitis was not observed. Numerous IgG4‐positive cells were found on immunostaining (Fig 4c) and the ratio of IgG4 staining to total IgG staining (Fig 4d) was approximately 60%.
Placental alkaline phosphatase and c‐kit staining of the tumor were negative (Fig 4e,f). We consulted doctors in internal medicine and connective tissue disorders to make a definitive diagnosis; diseases other than IgG4‐related disease were excluded. We ultimately diagnosed the patient with a thymic inflammatory pseudotumor with multilocular thymic cyst caused by IgG4‐related disease. The patient's serum IgG4 level two weeks after surgery was no longer elevated (44.9 mL/dL vs. normal: 4.5–117.0 mg/dL). We did not provide any additional treatment because preoperative PET showed no accumulation in any other organs or tumor lesions that could be completely resected. The patient was followed up for three years without recurrence, and his serum immunoglobulin levels were normal.
Discussion
Immunoglobulin G4‐related disease can involve virtually every organ; however, the most frequently involved sites are the pancreas, bile ducts, gallbladder, liver, salivary glands, and kidneys, with manifestations generally recognized as a mass at one or more sites mimicking a neoplasm.2, 5 In the thoracic region, IgG4‐related disease manifests as interstitial lung disease. In a Japanese study of 114 patients with IgG4‐related disease, 26 (22.8%) patients had pulmonary involvement and only 1 (0.9%) had mediastinal fibrosis.6 In a French study of 25 patients with IgG4‐related disease, 3 (12%) patients had pulmonary involvement, while none had mediastinal fibrosis.5 There have been only a few reports of occurrence in the anterior mediastinum.9, 10
Although no randomized trial has been performed, there is a consensus in favor of aggressive treatment when vital organs are involved with IgG4‐related tumors, usually with glucocorticoid agents as the first‐line therapy followed by azathioprine, mycophenolate mofetil, and methotrexate as glucocorticoid‐sparing agents for remission and maintenance purposes.11
It is difficult to obtain a correct diagnosis of mediastinal tumor before surgery. Of note, in cases involving the thymus, a preoperative diagnosis is not necessary, given the risk of dissemination by a needle biopsy. In this report, we failed to consider IgG4‐related disease as a differential diagnosis before surgery and required surgical resection to make the final correct diagnosis based on a histopathological examination. Some reports have described elevated levels of serum soluble IL‐2 receptor in cases of IgG4‐related disease.12 The mildly elevated levels of IL‐2 receptor in the present case may therefore have been suggestive of IgG4‐related disease. Previous studies have proposed that FDG‐PET is superior to other imaging modalities for the diagnosis of IgG4‐related disease.5, 6, 13, 14 In our case, FDG‐PET showed an abnormal uptake and the tumor manifested after only six months. Based on the PET findings and the rate of tumor growth, we should have considered inflammatory disease, especially IgG4‐related disease, as a differential diagnosis.
It is often difficult to diagnose inflammatory disease based on biopsy specimens, particularly for cases in which complete resection is impossible. When it is difficult to completely resect a tumor for which IgG4‐related disease is suspected, PET and MRI should be performed as diagnostic imaging modalities, and the serum IgG4 level should be measured in order to apply appropriate treatment as soon as possible. It is important to raise IgG4‐related disease to a differential disease when FDG‐PET shows an abnormally high uptake and MRI reveals low signal intensity on T1‐weighted imaging and high signal intensity on T2‐weighted imaging. In addition, if the rate of tumor growth is rapid, as in the present case, this finding can aid a diagnosis of IgG4‐related disease and lead to a definitive diagnosis with appropriate immunostaining.
Although IgG4‐related disease in the form of an anterior mediastinal tumor is rare, we should consider this disease when making a differential diagnosis in patients with anterior mediastinal tumors.
Disclosure
No authors report any conflict of interest.
References
- 1. Brito‐Zerón P, Ramos‐Casals M, Bosch X, Stone JH. The clinical spectrum of IgG4‐related disease. Autoimmun Rev 2014; 13: 1203–10. [DOI] [PubMed] [Google Scholar]
- 2. Islam AD, Selmi C, Datta‐Mitra A et al The changing faces of IgG4‐related disease: Clinical manifestations and pathogenesis. Autoimmun Rev 2015; 14: 914–22. [DOI] [PubMed] [Google Scholar]
- 3. Shigemitsu H, Koss MN. IgG4‐related interstitial lung disease: A new and evolving concept. Curr Opin Pulm Med 2009; 15: 513–6. [DOI] [PubMed] [Google Scholar]
- 4. Miyashita T, Yoshioka K, Nakamura T et al A case of lymphomatoid granulomatosis‐like lung lesions with abundant infiltrating IgG4‐positive plasma cells whose serum IgG4 levels became high following the start of corticosteroid therapy. Intern Med 2010; 49: 2007–11. [DOI] [PubMed] [Google Scholar]
- 5. Lin W, Lu S, Chen H et al Clinical characteristics of immunoglobulin G4‐related disease: A prospective study of 118 Chinese patients. Rheumatology (Oxford) 2015; 54: 1982–90. [DOI] [PubMed] [Google Scholar]
- 6. Zen Y, Nakamura Y. IgG4‐related disease: A cross‐sectional study of 114 cases. Am J Surg Pathol 2010; 34: 1812–9. [DOI] [PubMed] [Google Scholar]
- 7. Ebbo M, Daniel L, Pavic M et al IgG4‐related systemic disease: Features and treatment response in a French cohort: Results of a multicenter registry. Medicine 2012; 91: 49–56. [DOI] [PubMed] [Google Scholar]
- 8. Oka S, Uramoto H, Yamada S, Tanaka F. Sclerosing mediastinitis of unknown origin: Report of a case. Int J Surg Case Rep 2015; 10: 5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kang SR, Kim HR, Nam SJ, Hong S. Immunoglobulin G4‐related disease mimicking an anterior mediastinal tumor. Ann Thorac Surg 2018; 105: 75–7. [DOI] [PubMed] [Google Scholar]
- 10. Iguchi K, Ishibashi O, Takayashiki N, Satoh H. Mediastinal mass in a patient with IgG4‐related disease. Acta Med Int 2016; 3: 216–8. [Google Scholar]
- 11. Stone JH, Yoh Z, Vikram D. IgG4‐related disease. N Engl J Med 2012; 366: 539–51. [DOI] [PubMed] [Google Scholar]
- 12. Sato Y, Notohara K, Kojima M, Takata K, Masaki Y, Yoshino T. IgG4‐related disease: Historical overview and pathology of hematological disorders. Pathol Int 2010; 60: 247–58. [DOI] [PubMed] [Google Scholar]
- 13. Zhang J, Chen H, Ma Y et al Characterizing IgG4‐related disease with 18F‐FDG PET/CT: A prospective cohort study. Eur J Nucl Med Mol Imaging 2014; 41: 1624–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Takahashi H, Yamashita H, Morooka M et al The utility of FDG‐PET/CT and other imaging techniques in the evaluation of IgG4‐related disease. Joint Bone Spine 2014; 81: 331–6. [DOI] [PubMed] [Google Scholar]


